Abstract
Background
Peptide receptor radionuclide therapy (PRRT) serves as a novel and effective treatment option for somatostatin receptor-positive unresectable liver metastases of pancreatic neuroendocrine tumors (PNETs). However, there are few reported cases of surgical resection for initially unresectable liver metastases of PNET that were converted to resectable after PRRT. Here we report a case where PRRT and somatostatin analogs (SSAs) led to a pathological complete response of initially unresectable multiple liver metastases following PNET resection.
Case presentation
A 52-year-old man underwent pylorus-preserving pancreaticoduodenectomy for PNET at age 40 and subsequent hepatectomies for resectable liver metastases at 44 and 47 years of age. At age 48, a follow-up examination revealed unresectable multiple liver metastases, and PRRT with 177Lu-DOTATATE therapy was initiated. After four cycles of PRRT, most liver metastases diminished according to imaging studies, and the remaining two hepatic lesions continued to shrink with additional lanreotide. Conversion surgery for liver metastases was successfully performed, revealing no viable tumor cells in tissue specimens. Seventeen months after surgery, imaging showed no detectable residual tumor or recurrence. We present a review of the relevant literature that highlights the significance of our findings.
Conclusions
This rare case highlights the pathological complete response of initially unresectable multiple liver metastases achieved by PRRT and SSAs following PNET resection, suggesting their potential as a multimodality treatment option for unresectable PNET.
Similar content being viewed by others
Introduction
Pancreatic neuroendocrine tumors (PNETs) are rare, accounting for approximately 1–2% of pancreatic tumors [1]. Patients diagnosed with PNET experience 5-year survival rates ranging from 23% to 95% [2] that are significantly longer than those for pancreatic ductal adenocarcinoma. Despite the relatively indolent clinical courses of the disease, PNETs frequently manifest with distant metastases, with liver metastases the most common, affecting approximately 30%–85% of patients who are faced with a grim prognosis [3, 4]. Liver resection achieves significant survival benefits by reducing tumor burden and slowing disease progression, resulting in favorable 5-year survival rates ranging from 60% to 80% [3, 5]. Consequently, global practice recommends liver resection for such patients; however, for most cases, liver resection is often considered inappropriate, particularly in the presence of extrahepatic lesions and a high tumor burden across both liver lobes [6, 7]. In such cases, the cornerstone of treatment involves multimodal therapy, including systemic chemotherapy, transcatheter arterial chemoembolization, and ablation.
Peptide receptor radionuclide therapy (PRRT) selectively attacks tumor cells by binding to peptides expressed on their surface [8]. NETs frequently express membrane-localized somatostatin receptors (SSTRs), making these receptors suitable targets for PRRT using somatostatin analogs (SSAs). PRRT has been predominantly employed in Europe since the late 1990s to stabilize unresectable advanced or end-stage NETs. Previous studies report high response rates and favorable long-term outcomes with PRRT in patients with NET [9,10,11,12]. Consequently, PRRT is unequivocally recognized in multiple guidelines as a novel and effective treatment option for SSTR-positive and progressive NETs [13,14,15,16]. A similar favorable morphological response occurs in liver metastases of PNET, suggesting potential improvement in overall survival (OS) and progression-free survival (PFS) [17, 18]. However, the cases [19,20,21] in which initially unresectable liver metastases of PNET are converted to resectable after PRRT, followed by successful resection (conversion surgery), are limited given the high tumor burden and remnant liver function.
Here we report a case of conversion surgery for a patient who developed multiple unresectable liver metastases after PNET resection and underwent liver resection after PRRT with an SSA, leading to a remarkable reduction of tumor burden. We describe the pathological findings for the resected liver specimens and present a review of the relevant literature regarding patients who underwent conversion surgery after PRRT.
Case report
Initial diagnosis and pancreaticoduodenectomy
A 40-year-old male with jaundice was referred to our hospital for further evaluation. During the initial visit, contrast-enhanced computed tomography (CECT) demonstrated a 35-mm hypo-attenuated mass in the pancreatic head (Fig. 1a). No obvious regional lymph node metastasis or distant metastasis was detected. Although there was no histological confirmation due to the absence of a tumor biopsy, the radiological findings strongly indicated the presence of invasive pancreatic ductal adenocarcinoma. Subsequently, the patient underwent pylorus-preserving pancreaticoduodenectomy (PPPD) with lymph node dissection, which achieved R0 resection (Fig. 1b). Histopathological diagnosis revealed that the tumor was a PNET G2 (3.5 cm; mitotic count 6 per 10 high-power fields; Ki67 proliferative index, 10%) (Fig. 1c–f). According to the UICC TNM classification of malignant tumors 8th edition [22], the PNET was classified as pT3N0M0 Stage II with invasion into the common bile duct’s epithelium and the duodenum’s submucosa.
Primary pancreatic neuroendocrine tumor. a Contrast-enhanced computed tomography demonstrated a hypo-attenuated mass in the pancreatic head (arrowheads). b Gross appearance of the specimen obtained by pancreatoduodenectomy. c On the cut section, a whitish-yellow nodular tumor (arrowheads) appeared in the pancreatic parenchyma and invaded the duodenal wall. d–f Histology (d) and immunohistochemistry (e, f) of the resected specimen in medium-power views. Atypical polygonal proliferating tumor cells arranged in trabecular or nested patterns (hematoxylin and eosin staining) (d). Most tumor cells expressed chromogranin A (e), and their Ki67 labeling index was approximately 10% (f)
Resectable liver metastasis and hepatectomy
The patient underwent regular postoperative follow-up imaging examinations. Six liver lesions were detected in segments (S) 5, 7, and 8 (Fig. 2a–c) after 45 months, raising suspicion of multiple metastases of PNET. Evaluating the resectability of the lesions and considering the patient’s liver function assessed through indocyanine green clearance (R15: 3.3%, K: 0.22709, Child–Pugh classification A), we performed three partial hepatectomies. Histopathological analysis confirmed the diagnosis of PNET metastases for all lesions, classified as G2 (Ki67 index, 12%) (Fig. 2d–f). Approximately one year after liver resection, magnetic resonance imaging (MRI) revealed multiple liver metastases and enlarged mesenteric lymph nodes. Due to the small size of the liver metastases, observation was planned without immediate resection. After careful monitoring, the lesions exhibited slight growth over 17 months, making them amenable to resection (Fig. 3a–c). Somatostatin receptor scintigraphy (SRS) with 111In-pentetreotide and single photon emission computed tomography (SPECT) showed multiple liver metastases with substantial SRS detection of accumulation (scores 3–4) in the early phase [23]. Furthermore, in the delayed phase, SRS detected accumulation in the lymph node near the superior mesenteric vein as well as in the liver lesions (Fig. 3d). Subsequently, 13 partial liver resections and mesenteric lymphadenectomies were performed, yielding 18 liver metastases and one mesenteric lymph node metastasis.
Initial recurrence. a–c Magnetic resonance imaging revealed multiple liver metastases (arrow). d A fresh cut specimen of the well-demarcated whitish-yellow nodular tumor in liver segment 5, showing a solid tumor without necrosis. e, f Histology (e) and immunohistochemistry of Ki67 (f) of the resected specimen in medium power views. Histological features of proliferating tumor cells arranged in trabecular and nested patterns were similar to those of the primary tumor (e). Ki-67 labeling index of the metastatic liver tumor was 12% (f)
Second recurrence. Contrast-enhanced computed tomography revealed multiple liver metastases (arrows) (a and b) and lymph node metastasis near the superior mesenteric vein (arrowheads) (c). Somatostatin receptor scintigraphy revealed receptor accumulation in the liver and the lymph node (arrowheads) (d)
PRRT and SSAs for unresectable liver metastases
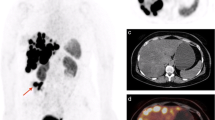
Eleven months after the second hepatectomy, CT revealed 16 multiple liver metastases and bone metastasis in the first lumbar vertebra (L1). SRS detected multiple nodules with score 3 as well as the accumulation in the liver and L1 vertebral body, indicating liver and bone metastases (Fig. 4a, b). The liver metastases were judged unresectable due to the presence of extrahepatic lesions. The patient was administered the SSA lanreotide, but the sizes of the lesions increased (Fig. 4c, d). Subsequently, the patient expressed interest in PRRT and was referred to another hospital. To initiate PRRT therapy, the patient provided informed consent to participate in the F-1515 phase I/II clinical trial [24]. The patient had no adverse events during PRRT. Following the administration of four cycles of PRRT with 177Lu-DOTATATE, most liver metastases diminished on imaging, and the remaining two hepatic lesions continued to shrink. While the liver metastases remained under control for a prolonged period, a new intrahepatic lesion was suspected 20 months after the completion of PRRT. After reintroducing lanreotide, the new intrahepatic lesion disappeared, and we could visualize only previously detected two lesions. Bone metastasis was well controlled with no remarkable change (Fig. 5). In the referral hospital, continued lanreotide therapy was proposed because there was no long-term progression of both liver and bone metastases. However, the patient wished to undergo tumor resection if possible, and further evaluation was performed in the referral hospital. A gadolinium-ethoxybenzyl-diethylene-triamine-pentaacetic acid-enhanced MRI showed no apparent liver metastasis other than the two lesions. In addition, MRI showed no change in the size of bone metastasis and no other extrahepatic lesions except for the bone metastasis (Fig. 6). Based on these findings, the disease was considered stable, and we thought the surgical resection of the remaining liver metastases was appropriate.
Post-PRRT to conversion surgery (contrast-enhanced computed tomography images). Most liver metastases diminished on imaging during peptide receptor radionuclide therapy, and only two reduced lesions with blurred contrast enhancement were detected in segments 2 (white arrow) and 8 (yellow arrow). A new intrahepatic lesion was identified 20 months after completion of PRRT (yellow dotted circle), however it disappeared after lanreotide administration. The bone metastasis remained stable during the treatment (white dotted circle)
Conversion surgery for liver metastases
After being referred again to our hospital, the patient underwent a partial hepatectomy (S2 and S8). This marked the third liver resection, and severe intraperitoneal adhesions were noted during the procedure. Intraoperative ultrasound findings indicated the absence of tumors, except for the two lesions, which were difficult to distinguish between scars or tumors. Therefore, two partial hepatectomies were performed. Because the tumors were difficult to detect in the resected specimens from both S2 and S8, additional liver resections were conducted to fully include the tumor area respectively. Operative time was 557 min, and blood loss was 1892 mL. There were no postoperative complications, and the patient was discharged on postoperative day 10. The resected specimens were S2 (2.5 × 1.5 × 1.5 cm, 5.0 × 2.5 × 0.5 cm) and S8 (3.5 × 3.0 × 1.0 cm, 3.0 × 2.5 × 0.6 cm). Gross examination revealed the presence of a grayish-white lesion resembling scar tissue on the surface of the liver S8 specimen; however, no apparent tumor was identified (Fig. 7a, b). Histopathological analysis did not detect viable tumor cells in both specimens (Fig. 7c, d). Seventeen months after surgery, the bone metastasis remained stable, and no other recurrence was identified via imaging modalities, including CECT and SRS, without administering drug therapy. The patient’s clinical course is summarized in Additional file 1: Figure S1.
Cut surface of formalin-fixed specimens (a, b). The specimens resected by partial hepatectomies of segment 2 (a) and segment 8 (b) were cut into serial slices 5-mm thick. All sections underwent histological examination after staining with hematoxylin and eosin (c, d). No viable or degenerated/necrotic tumor cells were found. A whitish fibrotic nodule in a section (arrow) of segment 8 was a histologically fibrotic scar (b)
Discussion
We present here the case of a patient who underwent PRRT for multiple unresectable liver metastatic recurrences after PNET resection. Following PRRT and SSA treatment, 16 liver metastases exhibited marked reduction, and partial hepatectomy was performed on the remaining two lesions. Notably, pathological examination of the resected liver specimens revealed no residual viable tumor cells. This case is noteworthy for the reasons as follows. First, it is uncommon for unresectable lesions, whether locally advanced or distant metastatic NET, to be resected after a favorable response to PRRT, i.e. conversion surgery. Second, the histological diagnosis of pathological complete response (pCR) makes this case highly rare; and to our knowledge, no reports exist regarding pCR for initially unresectable liver metastases in patients with PNETs. Third, to date, no tumor regrowth or new metastatic lesions have been identified 17 months after the final surgery.
As a consequence of recent advances in enhancing the efficacies of chemotherapy and radiotherapy, an increasing number of conversion surgeries have been applied to patients with colorectal liver metastases, pancreatic cancer, and gastric cancer, thus becoming a common treatment strategy [25, 26]. In PNETs, conversion surgery following chemotherapy, such as with sunitinib, streptozocin, or capecitabine/temozolomide, offer an improved prognosis [27, 28]. PRRT with 90Y- or 177Lu-DOTATATE achieve better response rates and longer PFS for patients with unresectable NETs than the aforementioned chemotherapies [11, 29, 30]. Thus, conversion of unresectable to resectable disease after PRRT is occasionally observed for some patients [19,20,21, 31,32,33].
A literature search for conversion surgery after PRRT revealed 9 cases, including that of our patient [19,20,21, 31,32,33]. Furthermore, Staszczak et al. presented a case in which tumor size reduction enabled surgical intervention [34]. However, surgery had not been performed at the time of the report and was under follow-up. As shown in Table 1, six of the nine patients showed a CR or partial response after PRRT for primary and distant metastatic disease, and one patient was diagnosed with progressive disease due to the emergence of a new liver lesion. Seven patients achieved R0 resection, and none experienced tumor recurrence during follow-up. Including our case, there were six patients with liver metastases; five patients who underwent liver resection, and four patients who achieved R0 resection. In one patient without R0 liver resection, three residual tumors continued to exhibit excellent responses after surgery. However, tumor regrowth was observed after 57 months. Subsequently, PRRT was repeated, and all tumors regressed. One patient did not undergo liver resection because a radiological CR was obtained after PRRT. There was no evidence of liver metastasis 22 months after surgery. Our case confirmed a pCR was achieved by PRRT and SSA treatment, contrary to other cases that show residual tumor cells in the resected specimen [19,20,21]. In summary, multiple patients with unresectable liver metastases of PNETs achieved significant responses to PRRT, highlighting the crucial role of PRRT as a multimodal treatment option in PNETs with liver metastases. Furthermore, it is noteworthy that conversion surgery can provide the advantage of liberation from long-term drug treatment, as demonstrated here.
However, it is essential to recognize that the effectiveness of PRRT is not uniform among all NETs [9, 10, 17] due to their diverse and heterogeneous nature. Moreover, PRRT alone is relatively ineffective in patients with NET with a Ki67 proliferative index > 10%, a high tumor burden, and functioning tumors [9, 10, 17]. As a result, multidisciplinary treatment incorporating other therapies has been contemplated. In a retrospective analysis by Yordanova et al., the coadministration of an SSA with PRRT, or its use as a maintenance therapy, demonstrates significant improvement in PFS (48 months vs 27 months) and OS (91 months vs 47 months) when compared with PRRT alone [35]. Another multicenter study reported that the addition of lanreotide following PRRT elevated the objective response rate from 27.3% to 36.8% [36]. The combination of PRRT with other chemotherapies, as well as with SSAs, enhances the disease control rate [37, 38]. Initially, controlling unresectable liver and bone metastases with lanreotide therapy alone was challenging in our case. However, subsequent PRRT successfully suppressed tumor growth, and additional lanreotide therapy markedly reduced tumor size, consistent with the findings of previous studies [37, 38]. When reviewing cases of conversion surgery in PNETs with unresectable liver metastases, all previously reported patients received PRRT alone. However, in our patient, it was evident that additional SSA therapy radiologically suppressed disease progression and contributed to the histological disappearance of the tumor (pCR).
The present case involved metachronous liver metastasis after primary NET resection, indicating the application of drug therapy combined with PRRT. However, in cases of simultaneous unresectable liver metastases, primary NET resection may serve as a therapeutic option to enhance the efficacy of PRRT. Evidence indicates that reducing tumor volume through primary NET resection leads to a favorable response to PRRT of metastatic tumors, thus improving prognosis [17]. Once the disease is exclusively confined to the liver, subsequent PRRT combined with chemotherapy is expected to be effective.
The present case report has several limitations. First, it reports a single case. However, NETs are rare, and it is even more challenging to collect resection cases after PRRT. Previous studies of conversion surgery employed few patients [19,20,21, 31,32,33]. Although conducting a randomized controlled trial will be difficult, an increase in successful conversion surgery after PRRT may result in more opportunities to obtain a pCR in the future. With the accumulation of patients undergoing conversion surgery, it may be possible to establish resection criteria and optimal timing for conversion surgery after PRRT. Second, while our patient could safely complete PRRT, adverse events should always be taken into consideration. In phase III NETTER-1 study [12], 85% of patients experienced adverse events during PRRT with 177Lu-DOTATATE, including grade 3 or higher neutropenia, thrombocytopenia, and lymphopenia, and only 77% of patients completed the planned four cycles of PRRT. Myelodysplastic syndromes were also observed in 0.9% of patients. Therefore, prompt diagnosis and treatment of adverse events are essential during PRRT. Third, this patient is currently undergoing follow-up 17 months after conversion surgery. In general, PNET progresses slowly, and cases of progression from residual tumors occur four years postoperatively in the conversion case series [20]. Therefore, in our case, long-term follow-up is necessary to ensure the absence of recurrences or re-emergence of disappearing disease. Fourth, in our patient, we assessed the therapeutic effects of PRRT and SSAs through CT/MRI and confirmed that liver and bone metastases were both well controlled before conversion surgery. Although tumor viability was not assessed by SRS before surgery, postoperative follow-up SRS showed no evidence of metastases except that the bone metastasis showed mild accumulation of octreotide without apparent progression. We believe that this finding suggests conversion surgery was adequately performed. The application of 111In-pentetreotide and 68Ga-DOTATOC-PET as well as conventional CT, MRI, and SRS for detecting distant metastases and assessing the efficacy of preoperative treatment will be particularly important in more complex treatment protocols.
Conclusion
We report a rare case of conversion surgery for initially unresectable multiple liver metastases after PNET resection. PRRT and SSAs significantly reduced the tumor burden, and a pCR was detected in resected liver specimens. Our case indicates the promising potential of PRRT and SSA therapy as a multimodal treatment option for unresectable liver metastases of PNET.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- PNET:
-
Pancreatic neuroendocrine tumor
- PRRT:
-
Peptide receptor radionuclide therapy
- SSTR:
-
Somatostatin receptor
- SSA:
-
Somatostatin analog
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- CECT:
-
Contrast-enhanced computed tomography
- PPPD:
-
Pylorus-preserving pancreaticoduodenectomy
- MRI:
-
Magnetic resonance imaging
- SRS:
-
Somatostatin receptor scintigraphy
- SPECT:
-
Single photon emission computed tomography
- CR:
-
Complete response
- pCR:
-
Pathological complete response
References
Oberg K, Eriksson B. Endocrine tumours of the pancreas. Best Pract Res Clin Gastroenterol. 2005;19(5):753–81.
Neuroendocrine Tumor of the Pancreas: Statistics [Internet]. Cancer.net. [cited 2023 Nov 25]. Available from: https://www.cancer.net/cancer-types/neuroendocrine-tumor-pancreas/statistics.
Chamberlain RS, Canes D, Brown KT, Saltz L, Jarnagin W, Fong Y, et al. Hepatic neuroendocrine metastases: does intervention alter outcomes? J Am Coll Surg. 2000;190(4):432–45.
Panzuto F, Boninsegna L, Fazio N, Campana D, Pia Brizzi M, Capurso G, et al. Metastatic and locally advanced pancreatic endocrine carcinomas: analysis of factors associated with disease progression. J Clin Oncol. 2011;29(17):2372–7.
Fendrich V, Langer P, Celik I, Bartsch DK, Zielke A, Ramaswamy A, et al. An aggressive surgical approach leads to long-term survival in patients with pancreatic endocrine tumors. Ann Surg. 2006;244(6):845–51.
Evans DB, Skibber JM, Lee JE, Cleary KR, Ajani JA, Gagel RF, Sellin RV, Fenoglio CJ, Merrell RC, Hickey RC. Nonfunctioning islet cell carcinoma of the pancreas. Surgery. 1993;114(6):1175–81.
Solorzano CC, Lee JE, Pisters PW, Vauthey JN, Ayers GD, Jean ME, et al. Nonfunctioning islet cell carcinoma of the pancreas: survival results in a contemporary series of 163 patients. Surgery. 2001;130(6):1078–85.
Merola E, Grana CM. Peptide receptor radionuclide therapy (PRRT): innovations and improvements. Cancers. 2023. https://doi.org/10.3390/cancers15112975.
Kwekkeboom DJ, de Herder WW, Kam BL, van Eijck CH, van Essen M, Kooij PP, et al. Treatment with the radiolabeled somatostatin analog [177 Lu-DOTA 0, Tyr3]octreotate: toxicity, efficacy, and survival. J Clin Oncol. 2008;26(13):2124–30.
Ezziddin S, Attassi M, Yong-Hing CJ, Ahmadzadehfar H, Willinek W, Grünwald F, et al. Predictors of long-term outcome in patients with well-differentiated gastroenteropancreatic neuroendocrine tumors after peptide receptor radionuclide therapy with 177Lu-octreotate. J Nucl Med. 2014;55(2):183–90.
Brabander T, van der Zwan WA, Teunissen JJM, Kam BLR, Feelders RA, de Herder WW, et al. Long-term efficacy, survival, and safety of [177Lu-DOTA0, Tyr3]octreotate in patients with gastroenteropancreatic and bronchial neuroendocrine tumors. Clin Cancer Res. 2017;23(16):4617–24.
Strosberg J, El-Haddad G, Wolin E, Hendifar A, Yao J, Chasen B, et al. Phase 3 Trial of 177Lu-dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376(2):125–35.
Falconi M, Eriksson B, Kaltsas G, Bartsch DK, Capdevila J, Caplin M, et al. ENETS Consensus Guidelines Update for the Management of patients with functional pancreatic neuroendocrine tumors and non-functional pancreatic neuroendocrine tumors. Neuroendocrinology. 2016;103(2):153–71.
Pavel M, Öberg K, Falconi M, Krenning EP, Sundin A, Perren A, Berruti A. Gastroenteropancreatic neuroendocrine neoplasms: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31(7):844–60.
Hope TA, Bodei L, Chan JA, El-Haddad G, Fidelman N, Kunz PL, et al. NANETS/SNMMI consensus statement on patient selection and appropriate use of 177Lu-DOTATATE peptide receptor radionuclide therapy. J Nucl Med. 2020;61(2):222–7.
Shah MH, Goldner WS, Benson AB, Bergsland E, Blaszkowsky LS, Brock P, et al. Neuroendocrine and adrenal tumors, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2021;19(7):839–68.
Bertani E, Fazio N, Radice D, Zardini C, Grana C, Bodei L, et al. Resection of the primary tumor followed by peptide receptor radionuclide therapy as upfront strategy for the treatment of G1–G2 pancreatic neuroendocrine tumors with unresectable liver metastases. Ann Surg Oncol. 2016;23(Suppl 5):981–9.
Partelli S, Bertani E, Bartolomei M, Perali C, Muffatti F, Grana CM, et al. Peptide receptor radionuclide therapy as neoadjuvant therapy for resectable or potentially resectable pancreatic neuroendocrine neoplasms. Surgery. 2018;163(4):761–7.
Stoeltzing O, Loss M, Huber E, Gross V, Eilles C, Mueller-Brand J, et al. Staged surgery with neoadjuvant 90Y-DOTATOC therapy for down-sizing synchronous bilobular hepatic metastases from a neuroendocrine pancreatic tumor. Langenbecks Arch Surg. 2010;395:185.
Chiapponi C, Lürssen N, Cremer B, Wahba R, Drebber U, Faust M, et al. Peptide receptor radionuclide therapy as a two-step strategy for initially unresectable liver disease from neuroendocrine tumors: a single-center experience. Endocrine. 2020;70(1):187–93.
Opalińska M, Sowa-Staszczak A, Grochowska A, Olearska H, Hubalewska-Dydejczyk A. Value of Peptide receptor radionuclide therapy as neoadjuvant treatment in the management of primary inoperable neuroendocrine tumors. Front Oncol. 2021;12(11): 687925.
Brierley JD, Gospodarowicz MK, Wittekind C, editors. TNM classification of malignant tumours. 8th ed. Oxford: Wiley-Blackwell; 2016.
Krenning EP, Valkema R, Kooij PP, Breeman WA, Bakker WH, de Herder WW, van Eijck CH, Kwekkeboom DJ, de Jong M, Pauwels S. Scintigraphy and radionuclide therapy with [indium-111-labelled-diethyl triamine penta-acetic acid-D-Phe1]-octreotide. Ital J Gastroenterol Hepatol. 1999;2:219–23.
A phase I/II clinical study of F-1515 in combination with F-1520 in patients with somatostatin receptor positive, progressive midgut carcinoids and other neuroendocrine tumors [Internet]. Available from: https://jrct.niph.go.jp/latest-detail/jRCT2080223813.
Kim SW. The result of conversion surgery in gastric cancer patients with peritoneal seeding. J Gastric Cancer. 2014;14(4):266–70.
Satoi S, Yamamoto T, Yamaki S, Sakaguchi T, Sekimoto M. Surgical indication for and desirable outcomes of conversion surgery in patients with initially unresectable pancreatic ductal adenocarcinoma. Ann Gastroenterol Surg. 2020;4(1):6–13.
Squires MH, Worth PJ, Konda B, Shah MH, Dillhoff ME, Abdel-Misih S, et al. Neoadjuvant capecitabine/temozolomide for locally advanced or metastatic pancreatic neuroendocrine tumors. Pancreas. 2020;49(3):355–60.
Murase Y, Kudo A, Akahoshi K, Maekawa A, Ishikawa Y, Ueda H, et al. Surgery after sunitinib administration to improve survival of patients with advanced pancreatic neuroendocrine neoplasms. Ann Gastroenterol Surg. 2021;5(5):692–700.
Yao JC, Shah MH, Ito T, Bohas CL, Wolin EM, Cutsem EV, Hobday TJ, Okusaka T, Capdevila J, de Vries EGE, Tomassetti P, Pavel ME, Hoosen S, Haas T, Lincy J, Lebwohl MS, Öberg K. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med. 2011;364(6):514–23.
Raymond E, Dahan L, Raoul J-L, Bang Y-J, Borbath I, Lombard-Bohas C, et al. Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N Engl J Med. 2011;364(6):501–13.
Kaemmerer D, Prasad V, Daffner W, Hörsch D, Klöppel G, Hommann M, et al. Neoadjuvant peptide receptor radionuclide therapy for an inoperable neuroendocrine pancreatic tumor. World J Gastroenterol. 2009;15(46):5867–70.
Ezziddin S. Neoadjuvant downsizing by internal radiation a case for preoperative peptide receptor radionuclide therapy in patients with pancreatic neuroendocrine tumors. Clin Nucl Med. 2012;37:102.
Barber TW, Hofman MS, Thomson BNJ, Hicks RJ. The potential for induction peptide receptor chemoradionuclide therapy to render inoperable pancreatic and duodenal neuroendocrine tumours resectable. Eur J Surg Oncol. 2012;38(1):64–71.
Sowa-Staszczak A, Pach D, Chrzan R, Trofimiuk M, Stefańska A, Tomaszuk M, et al. Peptide receptor radionuclide therapy as a potential tool for neoadjuvant therapy in patients with inoperable neuroendocrine tumours (NETs). Eur J Nucl Med Mol Imaging. 2011;38(9):1669–74.
Yordanova A, Wicharz MM, Mayer K, Brossart P, Gonzalez-Carmona MA, Strassburg CP, et al. The role of adding somatostatin analogues to peptide receptor radionuclide therapy as a combination and maintenance therapy. Clin Cancer Res. 2018;24(19):4672–9.
Prasad V, Srirajaskanthan R, Toumpanakis C, Grana CM, Baldari S, Shah T, et al. Lessons from a multicentre retrospective study of peptide receptor radionuclide therapy combined with lanreotide for neuroendocrine tumours: a need for standardised practice. Eur J Nucl Med Mol Imaging. 2020;47(10):2358–71.
Kesavan M, Claringbold PG, Turner JH. Hematological toxicity of combined 177Lu-octreotate radiopeptide chemotherapy of gastroenteropancreatic neuroendocrine tumors in long-term follow-up. Neuroendocrinology. 2014;99(2):108–17.
Yordanova A, Ahrens H, Feldmann G, Brossart P, Gaertner FC, Fottner C, et al. Peptide receptor radionuclide therapy combined with chemotherapy in patients with neuroendocrine tumors. Clin Nucl Med. 2019;44(5):e329-335.
Acknowledgements
We thank Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Funding
There was no funding supporting this study.
Author information
Authors and Affiliations
Contributions
All authors attest that they met the current ICMJE criteria for authorship. RU and SN drafted the manuscript. RU, SN, and NK contributed to the patient’s care. RU performed literature searches. RU, SN, NK, TM, TT, DB, ME, and KS participated in the critical revision of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from the patient to publish this case report and any accompanying images. The National Cancer Center Hospital’s Institutional Review Board reviewed and approved the study protocol (approval number: 2018-299).
Consent for publication
The patient provided informed consent for publishing this case report.
Competing interests
Noritoshi Kobayashi received a research grant from Novartis Pharma and lecture fees from Novartis Pharma, Teijin Pharma, Teijin Healthcare, EA Pharma, Ono Pharmaceutical, Taiho Pharmaceutical, Yakult Honsha, MSD, and PDRadiopharma. All the remaining authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Fig. S1.
A schema shows the treatment course and the tumor location.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Umino, R., Nara, S., Kobayashi, N. et al. Pathological complete response of initially unresectable multiple liver metastases achieved using combined peptide receptor radionuclide therapy and somatostatin analogs following pancreatic neuroendocrine tumor resection: a case report. surg case rep 10, 40 (2024). https://doi.org/10.1186/s40792-024-01839-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-024-01839-4