Abstract
Background
An esophageal anastomotic stricture (EAS) after an esophageal atresia surgery occurs in approximately 4–60% of the cases, and its first-line therapy includes balloon dilatation. Oral balloon dilatation cannot be performed in some EAS cases; conversely, even if dilatation is possible, these strictures recur in some cases, necessitating a surgical procedure for repairing the stenosis. However, these procedures are invasive and have short- and long-term complications. If an EAS recurs repeatedly after multiple balloon dilations, gastroesophageal reflux disease (GERD) may be the underlying cause. A fundoplication procedure may be effective for treating a refractory EAS, as in the present case.
Case presentation
A neonatal patient with type D esophageal atresia underwent thoracoscopic esophago-esophageal anastomosis at the age of 1 day, and her postoperative course was uneventful. Thereafter, the patient underwent gastrostomy for poor oral intake at the age of 3 months. After gastrostomy, the patient presented with a complete obstructive EAS. Balloon dilatation via the oral route was attempted; however, a guidewire could not be inserted into the EAS site. Hence, retrograde balloon dilatation via gastrostomy was performed successfully. However, the EAS recurred easily thereafter, and laparoscopic anti-reflux surgery was performed to prevent GERD. The anti-reflux surgery cured the otherwise refractory EAS and prevented its recurrence.
Conclusions
Retrograde balloon dilatation is another treatment option for an EAS. When an EAS recurs soon after dilatation, the patient must be evaluated for GERD; if severe GERD is observed, an appropriate anti-reflux surgery is required before dilating the EAS.
Similar content being viewed by others
Background
An esophageal anastomotic stricture (EAS) after an esophageal atresia (EA) surgery occurs in approximately 4–60% of the cases [1,2,3], and its first-line therapy includes balloon dilatation [4]. When balloon dilatation is impossible to perform or when patients are refractory despite multiple balloon dilatations, surgery is essential; the surgical procedures for treatment include EAS site resection with esophago-esophageal anastomosis, gastric pull-up, and interpositioning of the colon and jejunum. However, these procedures are invasive and have short- and long-term complications. Herein, we report a case of a refractory, complete obstructive EAS that occurred after a type D EA surgery involving gastrostomy and balloon dilatation. To preserve the native esophagus, the patient was treated with retrograde balloon dilatation via gastrostomy followed by laparoscopic fundoplication.
Case presentation
The patient was a second-born, monochorionic, diamniotic twin with a gestational age of 36 weeks and 2 days. The patient weighed 2054 g and had Apgar scores of 1 and 4 at 1 and 5 min, respectively. The prenatal course was uneventful, with no apparent prenatal diagnosis. However, the patient was referred to our hospital with suspected EA. We routinely perform contrast examinations [5], and a contrast examination on the day of admission revealed a tracheoesophageal fistula at the proximal esophagus. Intraoperative findings confirmed the diagnosis of type D EA. Thoracoscopic esophago-esophageal anastomosis with ligation of two parts of the tracheoesophageal fistula was performed at the age of 1 day (Fig. 1). The postoperative course was uneventful except for tracheomalacia and dysphagia, and enteral nutrition was started via a nasogastric tube at the age of 6 days. A contrast study on postoperative day 21 revealed an EAS and gastroesophageal reflux with sliding hernia. Mosapride citrate, rikkunshito, and famotidine were administered to prevent gastroesophageal reflux. Tracheomalacia was well-controlled with continuous positive airway pressure. The cause of dysphagia was unknown. Soon after the operation, left recurrent laryngeal nerve palsy was noted; however, it improved at 3 weeks postoperatively. Dysphagia persisted despite this; hence, nutrition was continued via a nasogastric tube. The patient was transferred to a local hospital at the age of 56 days.
Preoperative and operative findings. PA view (a) and lateral view (b) during contrast examination suggest the presence of a TEF in the proximal esophagus (white arrowhead). Intraoperative findings show two TEFs at the proximal and distal esophagus (arrowhead), resulting in type D esophageal atresia (c). PA: posterior anterior; TEF: tracheoesophageal fistula
At the local hospital, the patient developed aspiration pneumonia and underwent tracheal intubation at the age of 65 days. In addition, the patient had poor oral intake and was fed using a nasogastric feeding tube. The feeding tube was accidentally removed, and re-insertion was difficult due to the EAS; hence, gastrostomy was performed for enteral feeding at the age of 3 months. However, severe gastroesophageal reflux disease (GERD) remained unresolved after the procedure, and the EAS progressed and became almost obstructive. The patient’s condition could not be controlled at the local hospital; therefore, she was re-transferred to our institution.
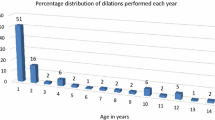
Contrast examination at the local hospital revealed a complete obstruction at the anastomosis site (Fig. 2). Upper endoscopy was performed to evaluate the EAS site, which revealed a complete obstruction that looked like a membrane. We unsuccessfully attempted to insert a 0.025-inch Jagwire™ Plus (Boston Scientific, Tokyo, Japan) via the oral route blindly under fluoroscopic view. Retrograde balloon dilatation for the EAS was performed through the gastrostomy site at the age of 4 months (Fig. 2). Briefly, by advancing a 2.8 mm bronchoscope and a guidewire through the gastrostomy site, a 0.025-inch Jagwire™ was easily inserted through the EAS site under fluoroscopic and bronchoscopic guidance. CRE™ wire-guided balloon dilatation catheters (Boston Scientific, Tokyo, Japan) were then inserted through the Jagwire™ via the gastrostomy site, and the EAS site was dilated until 7 mm. After retrograde balloon dilatation, balloon dilatation via the oral route became possible. Oral balloon dilatation with proton pump inhibitor treatment was performed four times, twice at the age of 5 months and once at the ages of 6 and 7 months each; however, the EAS recurred easily after these procedures. In addition, after improvement in the EAS by retrograde balloon dilatation, the patient began vomiting frequently. GERD was considered the cause of the repeated re-strictures; hence, laparoscopic Toupet fundoplication was performed at the age of 7 months. The esophagus was gently separated from the diaphragmatic crus to avoid causing esophageal dysmotility after surgery. The intra-abdominal esophagus was mobilized for at least 3 cm without strong traction. The diaphragmatic hiatus was sutured to prevent hiatal hernia. Because the patient had undergone gastrostomy and the stomach volume was relatively small, a wrap was difficult to make; however, a tension-free wrap was possible due to Toupet fundoplication. The first balloon dilatation after fundoplication was performed at the age of 8 months, yielding an almost complete improvement in the anastomotic stricture. The second balloon dilatation after fundoplication was performed during the final check at the age of 9 months, and contrast examination revealed no anastomotic strictures. The anastomotic stricture did not recur for 3 years and 7 months after the last dilatation (Fig. 3). However, dysphagia persisted after fundoplication. Laryngoscopy revealed no apparent recurrent laryngeal nerve palsy and laryngeal movement; however, the patient drank a little and refused to eat. Rehabilitation for dysphagia was continued, and the patient drank a cup of tea without aspiration at the age of 1 year and 5 months and started to eat solids at the age of 1 year and 10 months. The patient started eating baby food at the age of 3 years. Dysphagia has improved gradually; we believe its etiology is an unexplained developmental delay in the patient. To better depict the timeline of the case, a flow chart of the treatments provided has been given in Fig. 4.
Contrast examination at retrograde balloon dilatation. Contrast examination at the previous hospital shows complete obstruction at the anastomosis site (a; black arrowhead). A guidewire is inserted via the gastrostomy site under bronchoscopic guidance (b). Retrograde balloon dilatation is performed until 7 mm dilatation and a severe anastomotic stricture is noted as white arrow (c)
Discussion
The risk factors for an EAS include long-gap EA, postoperative anastomotic leakage [2, 6], trans-anastomotic tube placement [7], and GERD [2]. Balloon dilatation is the first-line treatment for an EAS [4]. To avoid a dilator tip directly perforating the esophagus, a guidewire is inserted, and its passage and position are evaluated using endoscopy or fluoroscopy. However, in case of a severe EAS (i.e., a complete obstructive EAS), it is impossible to insert a guidewire orally. In our case, the patient had a complete obstructive EAS at the time of transfer. Gastrostomy feeding blinded the EAS-related impaired esophageal clearance, while the complete obstructive EAS blinded the GERD symptoms; these were assumed to result in delayed recognition of the complete obstruction in the former hospital. Retrograde balloon dilatation (i.e., insertion of a guidewire via a gastrostomy site) is another option for EAS treatment [8] in patients with gastrostomy, in whom insertion of a guidewire via the oral route is difficult. In our case, the EAS was successfully dilated by retrograde balloon dilatation, and subsequent balloon dilatations were performed orally. Macher et al. assumed that retrograde guidewire insertion is easier than oral guidewire insertion because of the progressive narrowing of the EAS [9]. In addition, we assumed that the difficulty of oral guidewire insertion is attributed to anatomical changes. The esophageal lumen on the oral side is dilatated by saliva, and it is difficult to identify the stenotic hole. Because the esophageal lumen on the anal side of the EAS narrows progressively, the guidewire easily follows the narrowing esophagus and immediately enters the stenotic hole: the convex dome shape of the anal side of the EAS possibly allows this easy insertion.
When balloon dilatation cannot be performed, surgical procedures (such as resection of the stenotic site with or without interpositioning) are needed for EAS treatment. However, considering that these surgeries are invasive and associated with a high EAS recurrence rate, they should be considered the last treatment option (especially interposition grafting, which plays an extremely limited role in EAS treatment) [1].
In cases of EAS recurrence after dilatation, patients should be evaluated for GERD. Whether an anti-reflux surgery contributes to EAS prevention is controversial; however, some studies have shown that gastric acid contributes to EAS formation [10], whereas fundoplication for GERD prevents EAS formation [10]. However, the fundoplication method (either total or partial) that prevents EAS formation most efficiently remains unknown. In our case, partial fundoplication was performed to prevent gas bloat and dysphagia. Thus, our case indicates that partial fundoplication for GERD can cure and prevent refractory EAS.
Anti-reflux medications are another treatment option; however, the patient had already received an anti-reflux medication (i.e., proton pump inhibitors). Histamine H2 antagonists are generally considered first, but high-dose proton pump inhibitors are recommended for severe GERD [11]. Conversely, a previous report suggested that prophylactic antacid medications for patients with postoperative EA do not always prevent an EAS [12, 13]; therefore, anti-reflux surgery should be considered for treating refractory EAS with severe GERD [10]. However, the efficacy of fundoplication for EAS treatment remains unproven. One possibility is that anti-reflux medications cannot control reflux and cannot neutralize gastric acid completely. Another possibility is that non-acid reflux can contribute to EAS exacerbation. Non-acid reflux is associated with extra-esophageal symptoms such as cough at 25–50% [14] and is more correlated with a cough episode than acid reflux [15]. Non-acid reflux repeatedly stimulates the anastomotic site, resulting in an EAS. The successful treatment of an EAS with balloon dilatation may be attributed to the fact that fundoplication controls physical reflux.
The patient in our case was successfully treated with anti-reflux medication and fundoplication; however, patients in some cases may remain refractory even when GERD is corrected by fundoplication. Yasuda et al. performed a univariate regression analysis on 177 cases of EA and reported that fundoplication is a significant predictor of the need for EAS resection [16]; however, this predictor did not retain its significance in a subsequent multivariate analysis. If an EAS remains refractory after fundoplication, other treatment plans must be considered [17], including mitomycin C treatment [4, 18], endoscopic incisional therapy [19,20,21], and EAS resection with esophageal anastomosis [22]. Researchers have also recommended considering eosinophilic esophagitis in cases of a refractory EAS. Eosinophilic esophagitis does not respond well to dilatation unless the underlying immune mechanism is treated [23]. Kassabian et al. suggested that eosinophilic esophagitis is a frequently concomitant condition in patients with a history of esophageal deformities and that such patients may benefit from an endoscopic evaluation with biopsies [23]. Eosinophilic esophagitis should be kept in mind particularly when a patient has a history of atopy and presents with peripheral eosinophilia [24]. Our patient had no history of atopy and did not present with peripheral eosinophilia; however, we will consider this disease as a differential diagnosis in later cases. Although recurrent EASs seriously decrease the quality of life, the decline in our patient’s quality of life did not appear severe, because she could not intake food orally due to other unexplained developmental delays.
Conclusions
From this case, we deduced that if the esophageal anastomosis site is completely obstructed on contrast examination and when oral balloon dilatation has failed, retrograde balloon dilatation for the EAS should be performed via gastrostomy. Moreover, when an EAS recurs soon after dilatation, the patient should be evaluated for GERD. If severe GERD is observed, appropriate anti-reflux surgery must be performed before dilating the EAS.
Availability of data and materials
Not applicable.
Abbreviations
- EAS:
-
Esophageal anastomotic stricture
- EA:
-
Esophageal atresia
- GERD:
-
Gastroesophageal reflux disease
References
Baird R, Laberge JM, Lévesque D. Anastomotic stricture after esophageal atresia repair: a critical review of recent literature. Eur J Pediatr Surg. 2013;23:204–13.
Spitz L. Esophageal atresia. Lessons I have learned in a 40-year experience. J Pediatr Surg. 2006;41:1635–40.
Serhal L, Gottrand F, Sfeir R, Guimber D, Devos P, Bonnevalle M, et al. Anastomotic stricture after surgical repair of esophageal atresia: frequency, risk factors, and efficacy of esophageal bougie dilatations. J Pediatr Surg. 2010;45:1459–62.
Krishnan U, Mousa H, Dall’Oglio L, Homaira N, Rosen R, Faure C, et al. ESPGHAN-NASPGHAN guidelines for the evaluation and treatment of gastrointestinal and nutritional complications in children with esophageal atresia-tracheoesophageal fistula. J Pediatr Gastroenterol Nutr. 2016;63:550–70.
Nakagawa Y, Uchida H, Shirota C, Tainaka T, Sumida W, Makita S, et al. Preoperative contrast examinations help determine the appropriate cervical approach for congenital gross type C esophageal atresia: a report of two cases. Am J Case Rep. 2023;24: e938723.
Golonka NR, Hayashi AH. Early “sham” feeding of neonates promotes oral feeding after delayed primary repair of major congenital esophageal anomalies. Am J Surg. 2008;195:659–62.
LaRusso K, Joharifard S, Lakabi R, Nimer N, Shahi A, Kasasni SM, et al. Effect of transanastomotic feeding tubes on anastomotic strictures in patients with esophageal atresia and tracheoesophageal fistula: the Quebec experience. J Pediatr Surg. 2022;57:41–4.
El-Asmar KM, Youssef AA. Retrograde endoscopic dilatation for difficult caustic esophageal strictures: feasibility and effectiveness. J Pediatr Surg. 2019;54:1953–7.
Macher E, Michaud L, Guimber D, Bonnevalle M, Turck D, Gottrand F. Retrograde dilatation via gastrostomy of a proximal esophagoileal anastomotic stricture in an infant with esophageal atresia. Endoscopy. 2009;41:E10.
Pieretti R, Shandling B, Stephens CA. Resistant esophageal stenosis associated with reflux after repair of esophageal atresia: a therapeutic approach. J Pediatr Surg. 1974;9:355–7.
Van Biervliet S, Van Winckel M, Robberecht E, Kerremans I. High-dose omeprazole in esophagitis with stenosis after surgical treatment of esophageal atresia. J Pediatr Surg. 2001;36:1416–8.
Hagander L, Muszynska C, Arnbjornsson E, Sandgren K. Prophylactic treatment with proton pump inhibitors in children operated on for oesophageal atresia. Eur J Pediatr Surg. 2012;22:139–42.
Jones CE, Smyth R, Drewett M, Burge DM, Hall NJ. Association between administration of antacid medication and anastomotic stricture formation after repair of esophageal atresia. J Surg Res. 2020;254:334–9.
Catalano P, Di Pace MR, Caruso AM, Casuccio A, De Grazia E. Gastroesophageal reflux in young children treated for esophageal atresia: evaluation with pH-multichannel intraluminal impedance. J Pediatr Gastroenterol Nutr. 2011;52:686–90.
Fröhlich T, Otto S, Weber P, Pilic D, Schmidt-Choudhury A, Wenzl TG, et al. Combined esophageal multichannel intraluminal impedance and pH monitoring after repair of esophageal atresia. J Pediatr Gastroenterol Nutr. 2008;47:443–9.
Yasuda JL, Taslitsky GN, Staffa SJ, Clark SJ, Ngo PD, Hamilton TE, et al. Utility of repeated therapeutic endoscopies for pediatric esophageal anastomotic strictures. Dis Esophagus. 2020;33: doaa031.
Tambucci R, Angelino G, De Angelis P, Torroni F, Caldaro T, Balassone V, et al. Anastomotic strictures after esophageal atresia repair: incidence, investigations, and management, including treatment of refractory and recurrent strictures. Front Pediatr. 2017;5:120.
Thomson M, Tringali A, Dumonceau JM, Tavares M, Tabbers MM, Furlano R, et al. Paediatric gastrointestinal endoscopy: European society for paediatric gastroenterology hepatology and nutrition and European society of gastrointestinal endoscopy guidelines. J Pediatr Gastroenterol Nutr. 2017;64:133–53.
Burdick JS, Venu RP, Hogan WJ. Cutting the defiant lower esophageal ring. Gastrointest Endosc. 1993;39:616–9.
Samanta J, Dhaka N, Sinha SK, Kochhar R. Endoscopic incisional therapy for benign esophageal strictures: technique and results. World J Gastrointest Endosc. 2015;7:1318–26.
Hordijk ML, Siersema PD, Tilanus HW, Kuipers EJ. Electrocautery therapy for refractory anastomotic strictures of the esophagus. Gastrointest Endosc. 2006;63:157–63.
Koivusalo AI, Pakarinen MP, Lindahl HG, Rintala RJ. Revisional surgery for recurrent tracheoesophageal fistula and anastomotic complications after repair of esophageal atresia in 258 infants. J Pediatr Surg. 2015;50:250–4.
Kassabian S, Baez-Socorro V, Sferra T, Garcia R. Eosinophilic esophagitis in patients with esophageal atresia and chronic dysphagia. World J Gastroenterol. 2014;20:18038–43.
Pesce M, Krishnan U, Saliakellis E, Lopez R, Lindley KJ, Thapar N, et al. Is there a role for pH impedance monitoring in identifying eosinophilic esophagitis in children with esophageal atresia? J Pediatr. 2019;210:134–40.
Acknowledgements
The authors would like to thank the patient and the patient’s parents. YN was supported by the Nagoya University CIBoG WISE program from MEXT.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript. YN: investigation, writing—original draft, writing—review, and editing. HU: supervision, validation, review, and editing. AH: validation. CS: validation. WS: validation. SM: validation. KY: validation. HA: validation. AY: validation. DK: validation. YG: validation. TM: validation.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from the patient’s legal guardian for the publication of this case report.
Consent for publication
Written informed consent was obtained from the patient’s legal guardian for the publication of this case report.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nakagawa, Y., Uchida, H., Hinoki, A. et al. Refractory esophageal anastomotic stricture after esophageal atresia surgery improved with retrograde balloon dilatation through gastrostomy followed by laparoscopic fundoplication: a case report. surg case rep 9, 169 (2023). https://doi.org/10.1186/s40792-023-01754-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-023-01754-0