Abstract
Background
Trastuzumab-based chemotherapy is a standard treatment regimen for human epithelial growth factor 2 (HER2)-positive gastric cancer. This is a case of a patient who has survived 12 years after being diagnosed with advanced gastric cancer with multiple liver and lung metastases.
Case presentation
A woman in her 70s underwent total gastrectomy, cholecystectomy, and left hepatic lobectomy for gastric cancer with liver metastasis. One month after the surgery, multiple liver metastases appeared. After two courses of S-1 + CDDP chemotherapy, the liver metastases disappeared, and new lung metastases occurred. Because the primary tumor was HER2 positive, S-1 + CDDP + trastuzumab chemotherapy was performed. After one course of chemotherapy, the blood test showed pancytopenia, and CDDP was discontinued. S-1 + trastuzumab chemotherapy was then initiated, and as a result, the lung metastases disappeared. The patient is alive without recurrence 12 years after the surgery.
Conclusions
We encountered a case of long-term survival after multidisciplinary treatments for HER2-positive advanced gastric cancer with multiple liver and lung metastases.
Similar content being viewed by others
Background
HER2-positive gastric cancer is found in about 15–20% of all gastric cancer cases. It has been reported that the HER2-positive status is an independent poor prognostic factor in gastric cancer patients who underwent surgical resection [1]. Since the publication of the ToGA trial, trastuzumab-based chemotherapy has been considered a standard treatment for HER2-positive advanced gastric cancer [2]. We report a case of 12-year survival after multidisciplinary treatments for HER2-positive advanced gastric cancer with multiple liver and lung metastases.
Case presentation
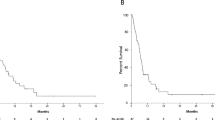
A woman in her 70s visited our hospital with a complaint of hematemesis. Upper gastroscopy revealed a type 2 tumor in the posterior wall of the upper body of the stomach (Fig. 1). Biopsy revealed a moderately differentiated tubular adenocarcinoma. Computed tomography (CT) showed that the lymph nodes were enlarged along the lesser curvature of the stomach, with a metastatic lesion in the left lobe of the liver (Fig. 2a, b). The clinical diagnosis was gastric body adenocarcinoma with lymph node metastasis and liver metastasis. According to the Japanese classification of gastric carcinoma [3], the clinical stage was cT3N1H1P0, stage IV. The patient underwent total gastrectomy, D2 lymph node dissection, cholecystectomy, and left hepatic lobectomy (Fig. 3a) with R0 resection. Postoperative pathology was diagnosed as pT3N3aH1CY0P0, stage IV (Fig. 3b). However, one month after the surgery, multiple liver metastases appeared (Fig. 4a) and CEA has risen again (Fig. 5). After two courses of S-1 + CDDP chemotherapy (S-1 80 mg day1-21, CDDP 60 mg/m2 day 8), the liver metastases disappeared (Fig. 4b) [4] and CEA has dropped within the normal range (Fig. 5), but new lung metastases appeared (Fig. 4c). Because the primary tumor was HER2 positive (immunohistochemistry (IHC) 2 + /fluorescence in situ hybridization-positive), S-1 + CDDP + trastuzumab chemotherapy (S-1 80 mg day 1–21, CDDP 30 mg/m2 day 8, trastuzumab 174 mg) [5] was performed. Since S-1 Plus CDDP therapy was effective for liver metastasis, so we did not dare to change from S1 plus CDDP to capecitabine plus CDDP. After one course of chemotherapy, the blood test showed pancytopenia, and CDDP was discontinued. The lung metastasis disappeared after four courses of S-1 + trastuzumab chemotherapy (Fig. 4d). Considering bone marrow function and general status, S-1 + trastuzumab chemotherapy was continued until 1 year postoperatively, followed by trastuzumab alone for 1 year before chemotherapy was completed. The patient is alive without recurrence 12 years after the surgery.
Discussion
Hepatic metastases are diagnosed synchronously in 3–14% of patients with gastric cancer [6]. Liver metastasis from gastric cancer (LMGC) is a systemic disease with an unfavorable prognosis. Systemic chemotherapy is considered the first therapeutic option for LMGC, but it fails to achieve satisfactory outcomes. The Japan Clinical Oncology Group reported a 5-year OS rate of only 1.7% in patients with metastasis confined to the liver and treated with systemic chemotherapy alone [7, 8]. On the other hand, there are highly selected cases when such metastases are found to be clinically resectable. Markar et al. reported that the median 1-year, 3-year, and 5-year survival were 68%, 31%, and 27%, respectively [6]. Guner et al. [9] suggested that the indications for liver resection are the following: no extrahepatic hematogenous metastasis; no peritoneal dissemination; the possibility of complete eradication of liver metastasis after liver resection; and adequate primary tumor control with complete removal of the primary gastric tumor and lymph nodes for synchronous metastasis. Since these indications were met in this case, total gastrectomy with D2 lymph node resection plus hepatectomy was carried out.
Surgery has potential benefits for a subset of patients with hepatic metastases, but hepatectomy for gastric cancer is still debated. This is because the high hepatic recurrence rate of 15–94% and general recurrence rate of 55–96% of LMGC imply that micrometastases remain in situ after surgery [10].
There are only limited data regarding pulmonary metastasis from gastric cancer. Kong et al. [11] reported an overall rate of pulmonary metastases of 0.96% (n = 20,187). They found that pulmonary metastases were most commonly the result of hematogenous metastasis which was significantly associated with liver metastases. In this case, we diagnosed the lung metastasis because nodular shadows appeared on chest CT after liver metastasis occurred in the early postoperative period and CA19-9 was also elevated (Fig. 5). But attention was required because diagnostic imaging was different from the typical lung metastasis of gastric cancer. Typical radiological findings of lung metastases include multiple rounds, variable-sized nodules and diffuse thickening of the stroma. However, atypical radiological features of metastases are often encountered, making it difficult to distinguish metastases from other non-malignant lung diseases [12]. In this case, the radiological characteristics of the lung tumor (Fig. 6) mimicked pneumonia, making it difficult to differentiate it from infection. Seo [12] and Abe [13] reported that the radiological findings of metastases from an adenocarcinoma of the gastrointestinal tract indicate air-space nodules, consolidation containing an air bronchogram, and focal or extensive ground-glass opacities.
In this case, hepatic recurrence and lung metastasis that occurred in the early postoperative period were severe problems. However, S-1 + CDDP chemotherapy followed by trastuzumab combination chemotherapy was successful, resulting in CR, and long-term survival without chemotherapy was obtained. The pathological findings of both the primary lesion and liver metastasis were HER2-positive, and trastuzumab was effective against lung metastasis, suggesting that lung metastasis also had HER2-positive status. Bozzetti et al. supported our speculation that the HER2 status of the primary tumor of gastric cancer and corresponding metastases are maintained and unchanged during the metastatic process [14]. The overall survival time for HER2-positive unresectable gastric cancer was 16.0 months in the ToGA trial [2], which was better than the 11.8 months for negative cases, but it was even longer at 12 years in this case. In the ToGA trial, a CR rate of 5% has been reported; however, there have not been many studies on the complete response in HER2-positive patients with gastric cancer with Herceptin. There is not enough data on the outcome of treatment after a complete response, so it cannot be said definitively. Even if a complete response is achieved, it is important to select an appropriate treatment based on factors such as the patient’s condition and risk of recurrence. This case is considered an exceptional long-term survivor of Her2-positive Stage IV advanced gastric cancer. The long-term survival is because there was no peritoneal metastasis and no recurrence in the residual liver and lungs after CR. In this case, a possible explanation for achieving CR is that the HER-2-positive status did not change during chemotherapy [15, 16].
Under the current guidelines, there is an option that the expression of HER2 should have been examined before surgery, and conversion surgery should have been attempted. In other words, gastrectomy plus hepatectomy without chemotherapy should have been avoided. However, this case underwent surgery in 2010 before Herceptin (Roche, Basel Switzerland) was approved in Japan in March 2011. There is no comprehensive report of conversion surgery for LMGC, and prospective studies with appropriate eligibility criteria are required. Several studies of conversion surgery for LMGC have recently been reported [8, 10, 17]. Fujitani et al. [8] supposed that tumor progression on preoperative chemotherapy was demonstrated to be associated with a poor outcome, even after potentially curative hepatectomy, suggesting that tumor control before surgery was crucial to offer a chance of prolonged remission. The response to neoadjuvant chemotherapy should be considered an unfavorable prognostic index, thus avoiding additional surgery [17, 18]. In the future, perioperative chemotherapy using trastuzumab, trastuzumab deruxtecan [19] as an antibody–drug conjugate, ramucirumab as an angiogenesis inhibitor, or anti-PD-1 antibody [20, 21] and anti-PDL-1 antibody as an immune check inhibitor is expected to enhance the antitumor effect and improve surgical outcomes.
Conclusion
We report a case of long-term survival after multidisciplinary treatments for HER2-positive advanced gastric cancer with multiple liver and lung metastases.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- HER2:
-
Human epithelial growth factor 2
- CDDP:
-
Cisplatin
- CEA:
-
Carcinoembryonic antigen
- BMS:
-
Bone marrow suppression
References
Gravalos C, Jimeno A. HER2 in gastric cancer: a new prognostic factor and a novel therapeutic target. Ann Oncol. 2008;19:1523–9.
Bang YJ, Van Cutsem E, Feyereislova A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. 2010;376(9742):687–97.
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–12.
Koizumi W, Narahara H, Hara T, et al. S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol. 2008;9:215–21.
Honma Y, Shimada Y, Takashima A, et al. Efficacy of S-1 plus cisplatin combination chemotherapy in patients with HER2-positive advanced gastric cancer. Int J Clin Oncol. 2014;19:863–70.
Markar S, Mikhail S, Malietzis G, et al. Influence of surgical resection of hepatic metastases from gastric adenocarcinoma on long-term survival: systematic review and pooled analysis. Ann Surg. 2016;263:1092–101.
Yoshida M, Ohtsu A, Boku N, et al. Long-term survival and prognostic factors in patients with metastatic gastric cancers treated with chemotherapy in the Japan Clinical Oncology Group (JCOG) study. Jpn J Clin Oncol. 2004;34:654–9.
Fujitani K, Kurokawa Y, Takeno A, et al. Prospective multicenter interventional study of surgical resection for liver metastasis from gastric cancer: R0 resection rate, and operative morbidity and mortality. Ann Surg Oncol. 2022;29:924–32.
Guner A, Yildirim R. Surgical management of metastatic gastric cancer: moving beyond the guidelines. Transl Gastroenterol Hepatol. 2019;4:58. https://doi.org/10.21037/tgh.2019.08.03.
Uggeri F, Ripamonti L, Pinotti E, et al. Is there a role for treatment-oriented surgery in liver metastases from gastric cancer? World J Clin Oncol. 2020;11:477–94.
Kong JH, Lee J, Yi CA, et al. Lung metastases in metastatic gastric cancer: pattern of lung metastases and clinical outcome. Gastric Cancer. 2012;15:292–8.
Seo JB, Im JG, Goo JM, et al. Atypical pulmonary metastases: spectrum of radiologic findings. Radiographics. 2001;21:403–17.
Abe Y, Suzuki M, Tsuji K, Sato M, et al. Lung metastasis from gastric cancer presenting as diffuse ground-glass opacities. Respir Med Case Rep. 2020;30: 101104.
Bozzetti C, Negri FV, Lagrasta CA, et al. Comparison of HER2 status in primary and paired metastatic sites of gastric carcinoma. Br J Cancer. 2011;104:1372–6.
Niikura N, Liu J, Hayashi N, et al. Loss of human epidermal growth factor receptor 2(HER2) expression in metastatic sites of HER2-overexpressing primary breast tumors. J Clin Oncol. 2012;30:593–9.
Makiyama A, Sukawa Y, Kashiwada T, et al. Randomized, phase II study of trastuzumab beyond progression in patients with HER2-positive advanced gastric or gastroesophageal junction cancer: WJOG7112G (T-ACT Study). J Clin Oncol. 2020;38:1919–27.
Arigami T, Matsushita D, Okubo K, et al. Indication and prognostic significance of conversion surgery in patients with liver metastasis from gastric cancer. Oncology. 2020;98:273–9.
Al-Batran SE, Goetze TO, Mueller DW, et al. The RENAISSANCE (AIOFLOT5) trial: effect of chemotherapy alone vs. chemotherapy followed by surgical resection on survival and quality of life in patients with limited-metastatic adenocarcinoma of the stomach or esophagogastric junction—a phase III trial of the German AIO/CAO-V/CAOGI. BMC Cancer. 2017;17:893.
Wilke H, Muro K, Van Cutsem E, et al. Ramucirumab plus paclitaxel versus placebo plus paclitaxel in patients with previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (RAINBOW): a double-blind, randomised phase 3 trial. Lancet Oncol. 2014;15:1224–35.
Janjigian YY, Shitara K, Moehler M, et al. First-line nivolumab plus chemotherapy versus chemotherapy alone for advanced gastric, gastro-oesophageal junction, and oesophageal adenocarcinoma (CheckMate 649): a randomised, open-label, phase 3 trial. Lancet. 2021;398(10294):27–40.
Janjigian YY, Kawazoe A, Yañez P, et al. The KEYNOTE-811 trial of dual PD-1 and HER2 blockade in HER2-positive gastric cancer. Nature. 2021;600(7890):727–30.
Acknowledgements
Not applicable.
Funding
We received no support from any funding.
Author information
Authors and Affiliations
Contributions
NT, MF, KT, and YT were responsible for the patient’s clinical management and data acquisition. SY and NT were responsible for drafting the manuscript and interpretation of data. NT, FY and KE were accountable for the critical revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was carried out in accordance with the principles of the Declaration of Helsinki.
Consent for publication
The patient has given consent for the publication of images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yoshioka, S., Takahashi, N., Fujisaki, M. et al. Long-term survival after multidisciplinary treatments for HER2-positive advanced gastric cancer with multiple liver and lung metastases. surg case rep 9, 139 (2023). https://doi.org/10.1186/s40792-023-01714-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-023-01714-8