Abstract
Background
Hydrosalpinx and pyosalpinx are rare gynecologic problems during adolescence, especially in girls without a history of sexual activity. They are even rarer in women with Hirschsprung’s disease (HD). We herein report a case of pyosalpinx in an adolescent girl with HD treated by transvaginal ultrasound-guided drainage.
Case presentation
The present patient was a 12-year-old girl (weight 83 kg; height 159 cm; body mass index 32.8 kg/m2). She had undergone five laparotomies for long-segment HD by 2 years. Her menarche had occurred at 10 years. She was admitted with lower abdominal and anal pain. Computed tomography (CT), magnetic resonance imaging (MRI), and transvaginal ultrasound showed left pyosalpinx and abdominal abscess. Surgical drainage was necessary; however, she had a history of polysurgery and was severely obese, so laparotomy was considered to carry a high risk. Transvaginal ultrasound was deemed more likely to reach the abscess safely. Therefore, she was treated with transvaginal ultrasound-guided drainage by a gynecologist skilled in the procedure. She was discharged home after 52 days. One year and nine months after discharge, there was no reformation of either the abscess or pyosalpinx.
Conclusions
Adolescent girls with HD are at risk of developing hydrosalpinx. Depending on the defecation status, pyosalpinx may also develop. As a less-invasive surgical treatment, transvaginal ultrasound-guided drainage can avoid laparotomy. Collaboration with a gynecologist is essential for the diagnosis and treatment of this clinical condition. Pediatric surgeons should communicate with gynecologists for such cases beginning around puberty for continuous follow-up.
Similar content being viewed by others
Background
Hirschsprung’s disease (HD) is a congenital disorder among neurocristopathies. HD is defined as the absence of ganglionic cells with hypertrophied cholinergic fibers in the myenteric and submucosal plexus of the distal rectum extending proximally for varying lengths, causing functional obstruction. HD remains a relatively rare congenital malformation [1], with a prevalence of approximately 1 in 5000 live births, and it has a high predisposition among males (male:female ratio approximately 3–4:1) in Japan [2, 3].
Hydrosalpinx is defined as fluid collection in the lumen of the fallopian tube owing to a distal obstruction. Menarche starts with a peak of stimulating hormones (FSH, LH), leading to an increase in glandular tissue and epithelial cells in the tubes. These changes subsequently activate the ovarian function and tubal motility. These events may lead to hydrosalpinx. Primary hydrosalpinx occurs because of inherent alterations in anatomy and physiology. However, secondarily acquired cases are the most frequent and include infections, adhesions, endometriosis, and neoplasms [1]. When intra-abdominal or vaginal infection occurs in hydrosalpinx, an abscess accumulates in the fallopian tube, resulting in pyosalpinx. However, hydrosalpinx and pyosalpinx are rare gynecologic problems during adolescence, especially in girls without a history of sexual activity [4].
We herein report a case of pyosalpinx in an adolescent girl with HD treated by transvaginal ultrasound-guided drainage.
Case presentation
The present patient was a 12-year-old girl (weight 83 kg; height 159 cm; body mass index 32.8 kg/m2). She had undergone five laparotomies for long-segment HD by 2 years. After these operations, complications of anal stenosis and fecal incontinence occurred. She was followed up for these complications, but she had refused to undergo periodic medical examinations for the most recent 4 years. Her menarche had occurred at 10 years. The last menstrual period was 3 weeks prior to presentation, and the patient’s menstrual cycle was normal.
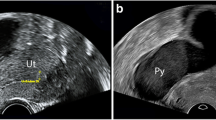
She was admitted with lower abdominal and anal pain. Fever elevation (38.5 °C), tachycardia, and tachypnea were noted. Her underwear sometimes became soiled due to fecal incontinence; therefore, a pad was worn. Her laboratory tests revealed an inflammatory response and acute renal failure (WBC 21,250 µL, CRP 54.77 mg/dL, BUN 27 IU/L, Cre 1.21 mg/dL). Computed tomography (CT) showed a multicystic mass in the pelvis and abdominal cavity (Fig. 1). In addition, magnetic resonance imaging (MRI) demonstrated that the multicystic mass was dorsal to the vagina and rectum (Fig. 2). Transvaginal ultrasound showed findings compatible with those of CT and MRI. She was thus diagnosed with left pyosalpinx and abdominal abscess.
Surgical drainage was necessary, but she had a history of polysurgery and was severely obese, so laparotomy was considered to carry a high risk for her. Transvaginal ultrasound was deemed more likely to reach abscesses safely. Therefore, she was treated with transvaginal ultrasound-guided drainage by a gynecologist skilled in the procedure. Under transvaginal ultrasound, we used an 18G needle to obtain oocytes by puncturing into the pyosalpinx and abdominal abscess (Fig. 3). Drainage was performed five times during hospitalization. A total of 370 ml of purulent discharge was collected. Cultures from the pyosalpinx detected Bacteroides fragilis, Escherichia coli, and Fusobacterium nucleatum. Antibiotic therapy was also provided (TAZ/PIPC, MPEM, VCM, MCFG).
Furthermore, she had difficulty avoiding constant perineal fecal contamination because of her obesity. To improve the patient’s pubic hygiene, she underwent daily pubic washing and the insertion of chloramphenicol vaginal tablets. Once her activities of daily living had improved, the method of pubic washing was switched to self-cleaning, and she started wearing a menstrual cup all day to prevent retrograde vaginal infection. Enema and antidiarrheal drugs were used to improve fecal incontinence. Her general condition improved dramatically with multidisciplinary treatment.
She was discharged home after 52 days. CT was performed 1 month after discharge, and the abdominal abscess and pyosalpinx were found to have resolved (Fig. 4). The use of a menstrual cup was switched from all day to use only during the day. One year and nine months after discharge, the absence of abscess and pyosalpinx was confirmed. She is currently regularly seen by a pediatric surgeon and gynecologist.
Discussion
Pyosalpinx in adolescent girls who are not sexually active is very rare and even rarer in women with HD [5]. According to a single-center study of HD, 17 cases with hydrosalpinx have been reported [1]. Concerning pyosalpinx, 22 patients were under 18 years, only one of whom reportedly had HD. Three of the 22 cases had poor defecation function [6]. To our knowledge, there have only been five reported cases of pyosalpinx with HD, including our own (Table 1). Most of these cases occurred after the onset of menstruation. Two patients had poor defecation control.
There have been several reports of an association between HD and hydrosalpinx. Pelvic surgery, pelvic inflammation, nerve damage, and neurological abnormalities have been noted. Furthermore, in patients with HD, smooth muscle cells in the fallopian tube or their innervation may be impaired and affect tubal peristalsis [10,11,12,13]. Recently, 5 of 17 girls (approximately 30%) who underwent surgery for HD were found to have hydrosalpinx, and all cases were bilateral, suggesting that congenital absence or reduction of fallopian tube nerve fibers may be involved [1]. In other words, not only acquired factors, such as surgery but also, the congenital factor of decreased nerve fibers related to HD may be a cause of hydrosalpinx. Therefore, it should always be kept in mind that HD girls may develop hydrosalpinx. Although this case is unilateral, considering the possibility of impaired fallopian tube function as well as adhesion, there is a possibility that contralateral hydrosalpinx may develop in the future, so careful follow-up is necessary.
Treatment of pyosalpinx includes conservative treatment (antibiotics), laparoscopic drainage, fluoroscopic drainage, laparoscopic salpingostomy, and fallopian tube resection [14]. Hospitalization for transvaginal echo-guided puncture drainage is reported to be shorter than that for antibiotic administration alone [15]. In the present case, transvaginal ultrasound-guided drainage was selected in cooperation with the gynecologist, and laparotomy was avoided. In HD patients, transabdominal drainage may be difficult because of intestinal adhesions due to a history of undergoing laparotomy several times. In addition, transrectal drainage may be difficult due to an abnormal pelvic anatomy, depending on the radical surgical approach applied. Therefore, a transvaginal approach is a useful route. In our case, the patient had both a history of polysurgery and obesity, so laparotomy or transabdominal ultrasound-guided drainage were considered high-risk procedures. Transvaginal drainage was very safe and effective in this case.
Fecal incontinence is a postoperative complication of HD. The present patient had undergone Swenson surgery and was in a state of chronic soiling. Poor defecation leads to poor pubic hygiene and increases the risk of developing the disease from retrograde infection of the vagina. Obesity leads to poor hygiene due to physical restraints [16]. In our case, thorough instruction in self-treatment and prevention of retrograde infection by wearing a menstrual cup were very effective in improving the vaginal environment.
Hydrosalpinx and pyosalpinx are common diseases in adult women but very rare in adolescent girls. Adolescent girls who have undergone HD surgery have a risk of developing hydrosalpinx. Furthermore, the risk of pyosalpinx depends on the defecation status. Therefore, pediatric surgeons should communicate with gynecologists beginning around puberty for continuous follow-up in these patients.
Conclusion
Adolescent girls with HD are at risk of developing hydrosalpinx. Depending on the defecation status, pyosalpinx may develop. Defecation control is important for preventing pyosalpinx. As a less-invasive surgical treatment, transvaginal ultrasound-guided drainage can avoid laparotomy. Collaboration with a gynecologist is essential for making an accurate diagnosis and for performing appropriate treatment. Pediatric surgeons should communicate with gynecologists beginning around puberty for continuous follow-up of these patients.
Availability of data and materials
Not applicable.
Abbreviations
- HD:
-
Hirschsprung’s disease
- FSH:
-
Follicle-stimulating hormone
- LH:
-
Luteinizing hormone
- BMI:
-
Body Mass Index
- CRP:
-
C-Reactive Protein
- CT:
-
Computed tomography
- MRI:
-
Magnetic Resonance Imaging
- TAZ/PIPC:
-
Tazobactam and piperacillin
- MPEM:
-
Meropenem
- VCM:
-
Vancomycin
- MCFG:
-
Micafungin
- ADL:
-
Active of Dairy Living
References
Palazón P, Saura L, de Haro I, Martín-Solé O, Albert A, Tarrado X, et al. Bilateral hydrosalpinx in patients with Hirschsprung’s disease. J Pediatr Surg. 2018;53:1945–50.
Taguchi T, Obata S, Ieiri S. Current status of Hirschsprung’s disease: based on a nationwide survey of Japan. Pediatr Surg Int. 2017;33:497–504.
Suita S, Taguchi T, Ieiri S, Nakatsuji T. Hirschsprung’s disease in Japan: analysis of 3825 patients based on a nationwide survey in 30 years. J Pediatr Surg. 2015;40:197.
Moralioglu S, Ozen IO, Demirogullari B, Basaklar AC. Pyosalpinx and hydrosaplinx in virginal adolescents: report of two cases. West Indian Med J. 2013;62:257–9.
Zainab K, Sujata G. Best practice in management of paediatric and adolescent hydrosalpinges: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2015;195:40–51.
Maraqa T, Mohamed M, Coffey D, Sachwani-Daswani GR, Alvarez C, Mercer L. Bilateral reccurent pyosalpinx in a sexually inactive 12-year-old girl secondary to rare variant of Mullerian duct anomaly. BMJ Case Rep. 2017. https://doi.org/10.1136/bcr-2016-218924.
Miyauchi K, Takahashi H, Shigeharu U, Nakata T, Taniguchi F, Kawachi K. A case of pyosalpinx in childhood after the radical operation of Hirschsprung’s disease. J Jpn Soc of Pediatr Surg. 1997;33:110–3.
Desai B, Ward T. Bilateral pyosalpinx in a peripubescent female with Hirschsprung’s disease: a case report. Int J Emerg Med. 2011. https://doi.org/10.1186/1865-1380-4-64.
Estors SB, Calleja AE, Hernandez CAE, Marhuenda IC. Pyosalpinx in a prepubescent girl with Hirschsprung’s disease. An Pediatr (Engl Ed). 2019;91:131–2.
Merlini L, Anooshiravani M, Peiry P, Scala GL, Hanquimet S. Bilateral hydrosalpinx in adolescent girls with Hirschsprung’s disease: association of two rare conditions. AJR Am Roentgenol. 2008;190:W278–82.
Staiano A, Santoro L, De Marco R, Miele E, Fiorillo F, Auricchio A, et al. Autonomic dysfunction in children with Hirschsprung’s disease. Dig Dis Sci. 1999;44:960–5.
Sandgren K, Laesson LT, Ekblad E. Widespread changes in neurotransmitter expression and number of enteric neurons and interstitial cells of Cajal in lethal spotted mice: an explanation for persisting dysmotility after operation for Hirschsprung’s disease? Dig Dis Sci. 2002;47:1049–64.
Wedel T, Van Eys GJ, Waltregny D, Glénisson W, Castronovo V, Vanderwinden MJ. Novel smooth muscle markers reveal abnormalities of the intestinal musculature in severe colorectal motility disorders. Neurogastroenterol Motil. 2006;18:526–38.
Agbor VN, Njim T, Aminde LN. Pyosalpinx causing acute appendicitis in a 32-year-old Cameroonian female: a case report. BMC Res Notes. 2016;9:368.
Singh-Ranger D, Sanusi A, Hamo I. Coliform pyosalpinx as a rare complication of appendicectomy: a case report and review of the literature on best practice. J Med Case Rep. 2008. https://doi.org/10.1186/1752-1947-2-97.
Dixon JB. The effect of obesity on health outcomes. Mol Cell Endocrinol. 2010;316:104–8.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors carried out the surgery and postoperatibe management. YS drafted the manuscript; YK critically revised the manuscript. All authors participated in the study design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Oral informed consent was obtained from the patient for the publication of this case report and accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sugai, Y., Kinoshita, Y., Kobayashi, T. et al. A rare case of pyosalpinx in adolescent girl with Hirschsprung’s disease who underwent transvaginal ultrasound-guided drainage. surg case rep 9, 74 (2023). https://doi.org/10.1186/s40792-023-01657-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-023-01657-0