Abstract
Background
Fungal infection may develop because of immunosuppression after organ transplantation, in which invasive types, such as Aspergillus and Mucorales, fungi cause morbidity. We present a case of disseminated mucormycosis due to Cunninghamella bertholletiae after ABO-incompatible living donor liver transplantation (LDLT).
Case presentation
A 47-year-old man with decompensated liver cirrhosis and hepatocellular carcinoma underwent an ABO-incompatible LDLT using a graft procured from his son, who had a different blood type. Rituximab and mycophenolate mofetil were administered 3 weeks before LDLT as immunosuppressive therapy. Although liver graft function improved, mass-like infiltrates appeared in the lungs following intubation for > 1 week due to impaired consciousness. The brain magnetic resonance imaging findings were normal. Decreased ejection fraction and ST elevation were detected on echocardiography and electrocardiography, respectively. There was no dominant stenosis on coronary arteriography. The recipient underwent segmentectomy of the right lung 20 days after LDLT. C. bertholletiae was identified from a specimen using polymerase chain reaction, thus establishing a diagnosis of mucormycosis. Multiple infarctions in the brain, heart, and kidney developed within 2 weeks. Treatment with amphotericin B was ineffective. The patient developed circulatory collapse, and a temporary pacemaker and percutaneous coronary intervention were required for cardiac infarction. The recipient died of cardiac failure 27 days after the LDLT. Autopsy revealed disseminated mucormycosis involving the brain, thyroid, heart, lung, liver, gastrointestinal tract, and both kidneys. In addition, fungal endocarditis may have been responsible for septic emboli in multiple organs, resulting in multiple organ invasion. Hypothrombocytopenia was present since the pre-transplant period, and the recipient was diagnosed posthumously with myelodysplastic syndrome due to hereditary abnormalities. Multiple factors such as organ transplantation, bone marrow dysfunction, immunosuppression, and inadequate administration of antifungal reagents might have promoted mucormycosis development in our patient.
Conclusions
Mucormycosis by C. bertholletiae is a fatal complication; thus, early diagnosis and treatment are warranted before multiple organ invasion.
Similar content being viewed by others
Background
Fungal infections develop in 20–42% of liver transplant recipients due to immunosuppression after liver transplantation [1]. Invasive fungi, such as Aspergillus and Mucorales fungi, cause mortality in over 90% and 60% of liver transplant recipients, respectively [2, 3]. Mucormycosis is characterized by extensive angioinvasion. In particular, infections caused by Cunninghamella bertholletiae have significantly higher mortality rates than those of other Mucorales [4,5,6]. We present a case of disseminated mucormycosis due to C. bertholletiae after ABO-incompatible living donor liver transplantation (LDLT).
Case presentation
A 47-year-old man with diabetes mellitus, decompensated liver cirrhosis due to non-alcoholic steatohepatitis, and hepatocellular carcinoma (HCC) underwent LDLT with splenectomy using a right hemiliver graft procured from his son. His pre-transplant model for end-stage liver disease score was 18 points, indicating that he was a suitable (not too severe) candidate for liver transplantation. Preoperative culture screening and β-d glucan were negative. The HCC lesion was 2 cm in diameter within the Milan criteria.
This was a case of ABO-incompatible LDLT from a type-B-positive donor to an O-positive recipient. The patient was administered intravenous rituximab at a dose of 375 mg/m2 3 weeks before the LDLT and oral mycophenolate mofetil (MMF) 2 g/day starting 2 weeks prior to the LDLT for induction immunosuppression. Post-transplant immunosuppression comprised tacrolimus, MMF, and steroids. The patient received oral fluconazole (100 mg/day) for 10 days to prevent fungal infections before switching to micafungin. The trough level of tacrolimus was adjusted by daily measurement, targeting a concentration of 10 ng/mL (Fig. 1). Post-transplant surveillance to detect fungal infection consisted of chest X-ray twice a day, culture screening of the sputum sample twice a week, and β-d glucan testing once a week.
The patient’s liver graft function gradually improved, and serum bilirubin levels decreased postoperatively (Fig. 1). After the LDLT, the patient’s level of consciousness remained impaired, with a Glasgow Coma Scale of G3V1M5, and he required intubation for > 1 week without respiratory failure. His oxygen saturation was maintained > 98% at 30% fraction of inspired oxygen. Brain magnetic resonance imaging was unremarkable. We temporally switched his tacrolimus to cyclosporine due to suspected adverse effects. However, there was no improvement in his consciousness. He underwent tracheotomy on postoperative day (POD) 9.
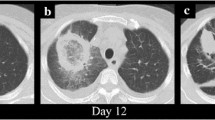
Chest radiography showed a right mid-zone infiltrate (Fig. 2a, b). Serum β-d-glucan levels were within the normal range until POD 6, but started to increase on POD 12 (Fig. 1). Bronchoalveolar lavage revealed microscopic filamentous fungus on POD 13. Micafungin was administered, followed by voriconazole (assuming aspergilloma); subsequent chest computed tomography (CT) showed right middle lung lobe infiltration. Surgery was planned since the lesion continued to grow (Fig. 2b).
Lung lesion. a, b Pulmonary CT scan images show a small ground-glass nodule in the right upper lobe of the lung on POD 5 (a, yellow arrowhead) and that the size of the nodule gradually increased to 57 × 29 × 33 mm on POD 16 (b, yellow arrowhead). c, d Thoracoscopy identifies the nodule with subserous bleeding in the right upper lobe (segment 3) of the lung (c, white arrowhead), and the specimen obtained by subsegmentectomy consists of necrosis with bleeding but without abscess formation (d, white arrowhead). e Two-day culture from the specimen forms a cotton-like fungus on the plate of Sabouraud dextrose agar. f, g Microscopic findings reveal broad, aseptate hyphae (arrows) with wide-angle branching (arrowheads), suggesting mucor infection. h–j Alveolar tissue pathologically includes multiple bleeding necrosis foci with fungal emboli (arrows) in most arteries (hematoxylin and eosin stain). Arteries, including small capillaries, are fully filled by emboli (arrows) surrounding bleeding necrosis. These emboli comprise red blood cells and hyphae (arrowheads), stained with Grocott (i) and periodic acid–Schiff (j). CT computed tomography, POD postoperative day
Preoperative examination revealed decreased ejection fraction (40%) on echocardiography and ST elevation on electrocardiography. There was no dominant stenosis on cardiac arteriography on POD 19.
Right lung segmentectomy was performed on POD 20 (Fig. 2c, d). C. bertholletiae was identified by polymerase chain reaction (PCR) from operative specimens cultured using Sabouraud dextrose agar culture medium (BD, Fukushima, Japan) (Fig. 2e–g). β-d-glucan level elevated five times the upper limit of the normal range (60.93 pg/mL), and amphotericin B (AmB) was started at 5 mg/kg IV on POD 22 (Fig. 1).
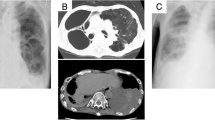
On POD 23, the patient’s circulatory dynamics collapsed, and he developed bigeminy and atrial-ventricular block, thus requiring a temporary pacemaker. Enhanced CT scans revealed multiple myocardial (Fig. 3a), cerebral (Fig. 4), and renal (Fig. 4) infarctions on POD 27. Cardiac arteriography revealed multiple peripheral occlusions (Fig. 3d). The patient’s cardiac arterial occlusion did not resolve despite percutaneous coronary intervention. An intra-aortic balloon was inserted for circulatory support; however, the recipient died of cardiac failure on POD 28.
Heart lesions. a Enhanced CT reveals an unenhanced area in the heart wall, suggesting multiple myocardial infarctions on POD 27. b Percutaneous cardiogram showing non-stenotic coronary arteries with multiple peripheral disruptions (yellow arrowheads). c–f Autopsy; multiple myocardial infarctions are penetrating the whole wall of the heart (green arrow). Vegetation is formed along with the chordae tendineae in the left ventricle (d, green arrowheads). Coronary arteries are patent but filled with fungal thrombosis on the peripheral side (e). Fibrin-containing fungal hyphae (arrowheads) cover the endothelium in all chambers, indicating fungal endocarditis (f). CT computed tomography, POD postoperative day
Autopsy findings. The brain, thyroid, liver graft, and kidney have infarctions (yellow arrowheads). A thrombus filled with fungal hyphae stained by Grocott is detected in a branch of the portal vein in the liver graft (yellow arrow). The stomach and intestine have multiple ulcers (green arrows), pathologically represented as bleeding necroses. Many fungal hyphae (arrowheads) are seen in atrial thrombosis (arrows) and tissues of the brain, kidney, stomach, and intestine
Hypothrombocytopenia was present since the pre-transplant period, which worsened after the LDLT. The patient’s bone marrow had reduced megakaryocytes and a pseudo-Pelger–Huët anomaly on POD 16. The recipient was diagnosed posthumously with myelodysplastic syndrome due to hereditary abnormalities.
Autopsy revealed multiple microscopic bleeding infarctions in the brain (Fig. 4), thyroid (Fig. 4), heart (Fig. 3), lung (Fig. 2), liver (Fig. 4), gastrointestinal tract (Fig. 4), and kidneys (Fig. 4). The cardiac arteries were patent but filled with fungal thrombi on the peripheral side. A fibrin-containing fungal mass covered the endothelium in all chambers, suggesting fungal endocarditis (Fig. 2d–f). Other organs also had multiple bleeding infarctions due to arterial septic emboli caused by fungi.
Discussion
Mucormycosis is caused by various genera of the order Mucorales of the class Zygomycetes, and the terms mucormycosis and zygomycosis are often used interchangeably [7]. Cunninghamella can also cause infection in humans, which affect multiple organ systems, including the rhinocerebral, pulmonary, cutaneous, and gastrointestinal systems, and cause severe infections [8]. In this case of mucormycosis after LDLT, the brain, lung, heart, gastrointestinal tract, liver, and kidneys were involved, and progression was rapid.
Mucormycosis is uncommon in developed countries [9]. Diabetes mellitus is the most common risk factor, followed by hematologic malignancies and solid organ or hematopoietic cell transplantation [9]. A review of mucormycosis in 116 organ transplant patients found that mucormycosis was caused by C. bertholletiae only in 6% of the cases [10]. To the best of our knowledge, only one case of C. bertholletiae invading multiple organs after liver transplantation has been reported since 1988 [11], wherein the diagnosis of C. bertholletiae infection was obtained only by a microscopic finding in autopsy; however, there were no representative images of multiple organ dissemination. Our study is the first to report detailed information, including several images on mucormycosis with multiple organ dissemination caused by C. bertholletiae after liver transplantation.
The initial right lung lesion was resected and used to diagnose mucormycosis. However, by that time, other symptoms such as altered consciousness and decreased ejection fraction rate (probably associated with the cerebral and cardiac invasions) had appeared. Pulmonary lesions are common in immunocompromised patients, including solid organ transplant recipients with mucormycosis [4, 10, 12]. Mucorales are ubiquitous in nature, and infection usually begins in a nasal turbinate or alveolus in susceptible individuals [9]. Pulmonary and rhino-orbital-cerebral mucormycosis are acquired by spore inhalation. Mucormycosis develops after a median of 5 months following solid organ transplantation, with a significantly earlier occurrence in liver transplant recipients [13]. Mucormycosis agents such as C. bertholletiae penetrate vasculature, resulting in mycotic thrombi, which can cause infarction with hemorrhagic necrosis [9]. Our case confirmed that the pulmonary lesion pathologically contained hemorrhagic necrosis caused by fungal emboli.
Cardiac mucormycosis caused Takotsubo myocarditis and an ultimately fatal cardiac infarction. Multiple myocardial infarctions due to fungal emboli were pathologically proven in autopsy specimens. The myocardia were most commonly affected in patients with disseminated pulmonary mucormycosis following solid organ transplantation [10].
Autopsy also revealed fibrin-containing hyphae covering the endothelium in all heart chambers, suggesting fungal endocarditis. Multiple organ infarctions occurred in quick succession; dissemination to multiple organs may have occurred originating from fungal endocarditis. Zhang et al. reported a case of endocarditis caused by C. bertholletiae infection after kidney transplantation [14].
Previous solid organ transplantation was associated with an increased risk of pulmonary, gastrointestinal, or disseminated infection in patients with mucormycosis [15]. An underlying hematological malignancy increases the risk of organ dissemination [3, 15], which occurs more frequently in the distant organs of immunosuppressed patients [10]. Our patient had infection-promoting factors, such as organ transplantation, bone marrow dysfunction, and immunosuppression. Prophylaxis might be needed against fungal infection, especially in the case of induced immunosuppression before transplantation, although the selection of anti-fungal reagents is complicated.
Previous use of voriconazole is a significant risk factor for mucormycosis development [16, 17]. We transitioned the patient to voriconazole when an Aspergillus infection was suspected before diagnosing mucormycosis. Jeong et al. reported that prior antifungal prophylaxis, including voriconazole and fluconazole, was administered to 11% of patients with mucormycosis [3]. Dissemination might have expanded to include multiple organs during the administration of voriconazole.
The risk of mortality is approximately 11-fold higher in patients with disseminated mucormycosis than in those with localized disease [4]. Mucorales were grown on culture, and histopathological features contributed to a definitive diagnosis of mucormycosis [3]. The presence of broad, aseptate, or pauci-septate hyphae with wide-angle branching with tissue invasion provides evidence of mucormycosis [18]. However, early diagnosis of C. bertholletiae infection is difficult and may only be confirmed on autopsy [14]. Modern molecular-based methods are required for species identification and diagnosis because serologic tests are not available yet [19]. We suspected mucormycosis after culturing the operative specimen; C. bertholletiae was ultimately identified by PCR, detecting specific fungal DNA sequences.
Patient mortality increases if AmB-based therapy is delayed [20]. High-dose conventional AmB at a dose of 10 mg/kg/day for 6 months was reported to contribute to the successful treatment of disseminated mucormycosis after stem cell transplantation [21]. Surgical intervention with debridement of necrotic tissue and debulking improves survival in patients with pulmonary infections [12]. Surgery plus AmB produces superior results than those of AmB administration alone [5]. Discontinuation or reduction in immunosuppression was associated with a better survival rate in patients after solid organ transplantation [10]. AmB was administered after removing the pulmonary lesion; however, the treatment was not completed in our patient because of brain and heart involvement. AmB should be administered as quickly as possible to LDLT recipients with suspected fungal infection.
Conclusions
Mucormycosis caused by C. bertholletiae after liver transplantation is a rare but fatal complication; the subsequent organ invasion can be fast and aggressive. Early diagnosis and appropriate treatment using antifungal agents and surgery are necessary to prevent dissemination to multiple organs.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- AmB:
-
Amphotericin B
- CT:
-
Computed tomography
- HCC:
-
Hepatocellular carcinoma
- LDLT:
-
Living donor liver transplantation
- MMF:
-
Mycophenolate mofetil
- PCR:
-
Polymerase chain reaction
- POD:
-
Postoperative day
References
Biancofiore G, Bindi ML, Baldassarri R, Romanelli AM, Catalano G, Filipponi F, et al. Antifungal prophylaxis in liver transplant recipients: a randomized placebo-controlled study. Transpl Int. 2002;15:341–7.
Liu X, Ling ZX, Li LJ, Ruan B. Invasive fungal infections in liver transplantation. Int J Infect Dis. 2011;15:E298–304.
Jeong W, Keighley C, Wolfe R, Lee WL, Slavin MA, Kong DCM, et al. The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports. Clin Microbiol Infect. 2019;25:26–34.
Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. Epidemiology and outcome of Zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;41:634–53.
Jeong W, Keighley C, Wolfe R, Lee WL, Slavin MA, Chen SC, et al. Contemporary management and clinical outcomes of mucormycosis: a systematic review and meta-analysis of case reports. Int J Antimicrob Agents. 2019;53:589–97.
Almyroudis NG, Sutton DA, Fothergill AW, Rinaldi MG, Kusne S. In vitro susceptibilities of 217 clinical isolates of zygomycetes to conventional and new antifungal agents. Antimicrob Agents Chemother. 2007;51:2587–90.
Phoompoung P, Luong M-L. Treatment of non-aspergillus mold infections: a focus on mucormycosis and fusariosis. Curr Treat Options Infect Dis. 2019;11:401–17.
Pappas PG, Alexander BD, Andes DR, Hadley S, Kauffman CA, Freifeld A, et al. Invasive fungal infections among organ transplant recipients: results of the transplant-associated infection surveillance network (TRANSNET). Clin Infect Dis. 2010;50:1101–11.
Petrikkos G, Skiada A, Lortholary O, Roilides E, Walsh TJ, Kontoyiannis DP. Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis. 2012;54(Suppl 1):S23-34.
Almyroudis NG, Sutton DA, Linden P, Rinaldi MG, Fung J, Kusne S. Zygomycosis in solid organ transplant recipients in a tertiary transplant center and review of the literature. Am J Transplant. 2006;6:2365–74.
Nimmo GR, Whiting RF, Strong RW. Disseminated mucormycosis due to Cunninghamella bertholletiae in a liver transplant recipient. Postgrad Med J. 1988;64:82–4.
Sun HY, Aguado JM, Bonatti H, Forrest G, Gupta KL, Safdar N, et al. Pulmonary Zygomycosis in solid organ transplant recipients in the current era. Am J Transplant. 2009;9:2166–71.
Singh N, Aguado JM, Bonatti H, Forrest G, Gupta KL, Safdar N, et al. Zygomycosis in solid organ transplant recipients: a prospective, matched case-control study to assess risks for disease and outcome. J Infect Dis. 2009;200:1002–11.
Zhang RB, Zhang JW, Szerlip HM. Endocarditis and hemorrhagic stroke caused by Cunninghamella bertholletiae infection after kidney transplantation. Am J Kidney Dis. 2002;40:842–6.
Jiménez C, Lumbreras C, Aguado JM, Loinaz C, Paseiro G, Andrés A, et al. Successful treatment of mucor infection after liver or pancreas-kidney transplantation. Transplantation. 2002;73:476–80.
Trifilio SM, Bennett CL, Yarnold PR, McKoy JM, Parada J, Mehta J, et al. Breakthrough Zygomycosis after voriconazole administration among patients with hematologic malignancies who receive hematopoietic stem-cell transplants or intensive chemotherapy. Bone Marrow Transplant. 2007;39:425–9.
Marty FM, Cosimi LA, Baden LR. Breakthrough Zygomycosis after voriconazole treatment in recipients of hematopoietic stem-cell transplants. N Engl J Med. 2004;350:950–2.
De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46:1813–21.
Millon L, Herbrecht R, Grenouillet F, Morio F, Alanio A, Letscher-Bru V, et al. Early diagnosis and monitoring of mucormycosis by detection of circulating DNA in serum: retrospective analysis of 44 cases collected through the French Surveillance Network of Invasive Fungal Infections (RESSIF). Clin Microbiol Infect. 2016;22(810):e1-8.
Chamilos G, Lewis RE, Kontoyiannis DP. Delaying amphotericin B-based frontline therapy significantly increases mortality among patients with Hematologic malignancy who have Zygomycosis. Clin Infect Dis. 2008;47:503–9.
Ota H, Yamamoto H, Kimura M, Araoka H, Fujii T, Umeyama T, et al. Successful treatment of pulmonary mucormycosis caused by Cunninghamella bertholletiae with high-dose liposomal amphotericin B (10 mg/kg/day) Followed by a lobectomy in Cord Blood Transplant Recipients. Mycopathologia. 2017;182:847–53.
Acknowledgements
We would like to thank Tatsuya Natori L.T. (Laboratory Technician), who identified Cunninghamella bertholletiae in an operative specimen, and Editage (www.editage.com) for English language editing.
Funding
None.
Author information
Authors and Affiliations
Contributions
AM was a major contributor in writing the manuscript and producing Figs. 1, 2, and 3. SH was a major contributor in creating Fig. 4. TU and KU performed the histological examination. TU suggested the investigation of cardiac mucormycosis. KU prepared the microscopic images. YO, KK, YM, TN, KY, and AS provided suggestions for the manuscript. YS was a major contributor in revising the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This report was approved by the Ethics Committee of Shinshu University School of Medicine, Matsumoto, Japan (No. 5190) and adhered to all applicable research standards.
Consent for publication
The patient and his family consented to the publication of this report.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mita, A., Hirano, S., Uehara, T. et al. Fatal disseminated mucormycosis due to Cunninghamella bertholletiae infection after ABO-incompatible living donor liver transplantation: a case report. surg case rep 8, 164 (2022). https://doi.org/10.1186/s40792-022-01516-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-022-01516-4