Abstract
Background
Mucinous cystic neoplasm of the liver (MCN-L) is a rare cystic tumor as defined by the 2010 World Health Organization classification. MCN-L usually does not communicate with or grow into the bile duct. Herein, we present a rare case of MCN-L with a polypoid nodule protruding into the bile duct.
Case presentation
A 69-year-old woman was referred to our hospital for elevated serum liver enzyme levels and obstructive jaundice. The patient also complained of abdominal pain in the right hypochondriac region. Abdominal ultrasonography showed a cystic lesion in segment 4 (S4) of the liver. Computed tomography revealed a 4-cm multilocular cystic lesion with a thick wall and multiple septal formations, showing a cyst-in-cyst appearance in S4. Endoscopic retrograde cholangiography showed a contrast defect between the left hepatic duct and the common bile duct, which was suspected to be a nodular lesion in the bile duct. Bile cytology and biopsy of the nodular lesion showed no malignant findings. Based on these findings, the differential diagnosis in this patient included intraductal papillary neoplasm of the bile duct and MCN-L, which had malignant potential. The patient underwent left hemihepatectomy, including caudate lobe excision with bile duct resection and right hepatocholangiojejunostomy. Macroscopic findings showed a 40 × 29 mm multilocular cystic lesion with a polypoid nodule that protruded into the left intrahepatic bile duct. As an ovarian-like stroma was observed in both cystic and polypoid lesions microscopically, the histopathological diagnosis was MCN-L. The postoperative course was uneventful, and the patient was discharged 24 days after surgery. The patient is currently alive without recurrence 22 months after the surgery.
Conclusion
Although MCN-L rarely communicates with the bile duct, it is necessary to consider that MCN-L could grow into the bile duct, occasionally causing obstructive jaundice.
Similar content being viewed by others
Background
Mucinous cystic neoplasm of the liver (MCN-L) is a rare cystic tumor as defined by the 2010 World Health Organization (WHO) classification [1]. In general, MCN-L occurs most often in the left lobe of the liver of middle-aged women [2]. Histologically, MCN-L is distinguished from intraductal papillary mucinous neoplasm of the bile duct (IPNB) by the presence of ovarian-like stroma (OLS), but it is sometimes difficult to differentiate on imaging. MCN-L rarely communicates with the bile duct, unlike IPNB. Herein we report a rare case of MCN-L that communicated with bile duct and a polypoid nodule prolapsing into the bile duct.
Case presentation
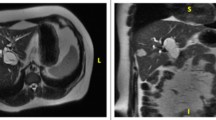
A 69-year-old woman was referred to our hospital for the investigation and treatment of elevated serum liver enzyme levels and obstructive jaundice. She also complained of tenderness in her right hypochondriac region. Laboratory tests revealed elevated levels of hepatobiliary enzymes (aspartate transaminase: 91 U/l, alanine transaminase: 249 U/l, alkaline phosphatase: 990 U/l, γ-glutamyl transpeptidase: 761 U/l, total bilirubin: 1.7 mg/dl) and jaundice. Carcinoembryonic antigen, carbohydrate antigen 19-9, alpha fetoprotein, and protein levels induced by vitamin K absence or antagonist-II were within the normal range. The preoperative liver function test was classified as Child–Pugh grade A. Abdominal ultrasonography showed a cystic lesion in segment 4 (S4) of the liver (Fig. 1a). Computed tomography (CT) revealed a 4 cm multilocular cystic lesion with multiple septal formations showing a cyst-in-cyst appearance in S4 (Fig. 1b). In addition, a nodule extending from the left hepatic duct to the common bile duct was observed, which was suspected to have arisen from the cystic wall (Fig. 1c). Endoscopic retrograde cholangiography (ERC) showed a contrast defect from the left hepatic duct to the common bile duct, which was suspected to be a nodular lesion in the bile duct (Fig. 1d). Bile cytology and biopsy of the nodular lesion showed no malignant findings. Based on these findings, the differential diagnosis in this patient included IPNB and MCN-L which had malignant potential. In addition, because the tumor had a nodular part, the coexistence of a malignant neoplasm was suspected. The patient underwent left hemihepatectomy, including caudate lobe excision with bile duct resection and right hepatocholangiojejunostomy. The operative time was 574 min, and blood loss was 490 ml. Macroscopic findings of the resected tumor showed a 40 × 29 mm multilocular cystic lesion with a polypoid nodule prolapsing into the left intrahepatic bile duct and, confirming communication between the tumor and the bile duct (Fig. 2). Microscopic findings revealed that the cyst wall was covered with columnar epithelium and OLS was observed extensively in the cyst wall stroma (Fig. 3a). Immunostaining showed that the cyst wall was positive for estrogen receptors (ER) (Fig. 3b). OLS was also observed in the polypoid lesion (Fig. 3c), and ER was positive in the polypoid lesion (Fig. 3d) as well as cyst wall. Histopathological diagnosis was MCN-L and no malignancy was observed. The postoperative course was uneventful and the patient was discharged 24 days after surgery. Follow-up imaging showed no evidence of recurrent disease 22 months postoperatively.
Imaging examination findings. a Abdominal ultrasonography showed a 49 × 29-mm cystic lesion with a septum in Segment 4 (S4). b Computed tomography (CT) revealed a 4-cm multilocular cystic lesion with multiple septal formations showing a cyst-in-cyst appearance in S4 (arrow). c CT revealed polypoid nodule (oval) protruded in the left hepatic duct from the cystic lesion (arrow). d Endoscopic retrograde cholangiography showed a contrast defect in the left hepatic duct to common bile duct which was suspected to be a nodular lesion in the bile duct (arrow)
Microscopic findings of the resected tumor. a The cyst wall was covered with columnar epithelium, and ovarian-like stroma (OLS) was observed extensively in the cyst wall stroma. b Immunostaining showed the sample was positive for estrogen receptors (ER). c In the polypoid lesion, OLS was observed as well as cyst wall. d Immunostaining also showed that the polypoid lesion was ER positive
Discussion
The WHO classified mucin-producing bile duct tumors of the liver as MCN-L or IPNB in 2010 [1]. MCN-L is defined as a cyst-forming epithelial neoplasm, usually demonstrating no connection with the bile ducts, whereas IPNB shows communication with the bile duct. OLS plays an important role in distinguishing between MCN-L and IPNB. Thus, OLS has been established as a diagnostic criterion for MCN-L by the WHO.
MCN-L is rare, accounting for less than 5% of all cystic lesions of the liver [3]. Generally, MCN-L occurs predominantly in females, as in our patient. Typical symptoms of MCN-L are nonspecific, such as epigastralgia and abdominal distension [4]. MCN-L is sometimes asymptomatic and rarely presents with obstructive jaundice because it does not communicate with the bile duct. However, our case was symptomatic because of a polypoid lesion that grew into the bile duct and caused bile duct obstruction.
On imaging examinations such as ultrasonography, CT, and magnetic resonance imaging (MRI), MCN-L often forms a cyst-in-cyst structure without communication to the bile duct. It is a multilocular cyst with an internal septum, and its contents are mainly mucus. The sensitivity and specificity of imaging findings for diagnosing MCN-L have been reported to be 81% and 95%, respectively [5]. There is thickening of the cyst wall and a contrast effect with or without calcification. MRI findings changes depending on the composition of intracystic liquid. It is typically hypointense on T1-weighted images and hyperintense in T2-weighted images. However, it varies depending on the presence of hemorrhage or protein content [6].
It is difficult to differentiate between MCN-L and IPNB preoperatively. Another differential diagnosis is cholangiocarcinoma with cystic changes [7]. In our patient, it was difficult to preoperatively differentiate MCN-L from other diseases as although a cyst-in-cyst appearance was present, there was a nodule protruding into the bile duct, which was atypical for MCN-L.
The differential diagnoses of nodules formed in the bile ducts include hepatocellular carcinoma (HCC) with bile duct invasion and intraductal growth (IG) cholangiocellular carcinoma (CCC). When these tumors grow into the bile duct, the lesions in the bile duct have an irregular surface. Takano et al. stated that the smooth, round surface of the tumor in the bile duct is characteristic of MCN-L, unlike HCC invasion and IG-type CCC [8]. In our case, ERC revealed a smooth oval contrast defect similar to previously reported cases. Preoperative histopathological examination of biopsy for the nodular lesion in the bile duct also showed no malignant findings.
Histologically, MCN-L is a cyst-forming epithelial tumor composed of cuboidal or columnar epithelium and variable mucin-producing epithelium. The subepithelial layer consisted of densely organized, spindle-shaped cells resembling OLS. OLS is a mesenchyme consisting mainly of dense spindle-shaped cells and resembles the native ovarian interstitium not only in its histological morphology, but also in its immunohistochemical characteristics, including hormone receptor expression, such as ER and progesterone receptor expression. OLS in epithelial tissue forming cysts is necessary for the pathological diagnosis of MCN-L. The presence of gonads in the vicinity of the liver is thought to be responsible for the migration of gonadal cells to the liver surface during embryonic development and for the formation of the ovarian stroma in MCN-L [9]. In this case, OLS was observed not only in the area forming the cyst wall, but also in the polypoid nodule protruding into the bile duct. These findings confirmed that MCN-L had spread into the bile ducts.
For treatment, complete resection is recommended because MCN-L is considered a potential malignancy even though previous reports have suggested that the probability of malignant transformation is less than 20% [10]. Surgical resection of patients with MCN-L has been reported to achieve a 100% 5-year survival rate [4]. Therefore, even in asymptomatic cases of MCN-L, surgical treatment is recommended. Indication for liver resection includes a tumor size of the tumor larger than 100 mm, the tumor increases over time, or symptoms appear [2].
We searched previous reported cases of MCN-L which grew into the bile duct, using the key words “mucinous cystic neoplasm of the liver” on PubMed (Table 1) [8, 11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. We chose only MCN-L diagnoses based on the presence of OLS and excluded cases that were complicated by IPNB. The median age of the 19 patients, including our patient, was 41 years (range, 25–69 years). Our patient is the oldest among the patients and all patients were women. The median tumor size was 55 mm (range, 18–83 mm). Zen et al. reported that the mean tumor diameter in 54 MCN-L cases was 100 mm (29–240 mm) [2]. MCN-L prolapsing into the bile duct tends to be smaller size than normal MCN-L. This may be because MCN-L with growth into bile duct causes symptoms such as liver dysfunction and obstructive jaundice even if small tumor size. The most common primary site of the tumor was S4, similar to that in our patient. No malignant findings were observed in any of the reported cases. Prolapse of a nodular lesion into bile duct is not always associated with tumor malignancy.
MCN-L is usually considered a cystic tumor that does not communicate with the bile ducts, but it can grow into the bile ducts, as noted in our case. Although it is difficult to obtain a definitive diagnosis of MCN-L preoperatively, surgical treatment can provide a good prognosis and feasible treatment owing to its malignant potential. As the cause of MCN-L communication with the bile ducts remains still unknown, further investigation is needed on the accumulation of cases.
Conclusion
Herein, we report an extremely rare case of MCN-L with a polypoid nodule prolapsing into the bile duct. Although MCN-L rarely communicates with the bile duct, we should keep in mind that MCN-L could grow into the bile duct, occasionally causing obstructive jaundice. Further case accumulation and pathophysiological analysis are needed. We believe that this case report contributes to the elucidation of its pathogenesis.
Availability of data and materials
Not applicable.
Abbreviations
- MCN-L:
-
Mucinous cystic neoplasm of the liver
- WHO:
-
World Health Organization
- IPNB:
-
Intraductal papillary mucinous neoplasm of bile duct
- OLS:
-
Ovarian-like stroma
- CT:
-
Computed tomography
- ERC:
-
Endoscopic retrograde cholangiography
- ER:
-
Estrogen receptor
- MRI:
-
Magnetic resonance imaging
- HCC:
-
Hepatocellular carcinoma
- CCC:
-
Cholangiocellular carcinoma
References
Nakanuma Y, Curado M-P, Franceschi S, et al. WHO classification of tumours of the digestive system. 4th ed. Lyon: WHO; 2010. p. 217–24.
Zen Y, Jang KT, Ahn S, Kim DH, Choi DW, Choi SH, et al. Intraductal papillary neoplasms and mucinous cystic neoplasms of the hepatobiliary system: demographic differences between Asian and Western populations, and comparison with pancreatic counterparts. Histopathology. 2014;65:164–73.
Budzynska A, Hartleb M, Nowakowska-Dulawa E, Krol R, Remiszewski P, Mazurkiewicz M. Simultaneous liver mucinous cystic and intraductal papillary mucinous neoplasms of the bile duct: a case report. World J Gastroenterol. 2014;20:4102–5.
Kubota K, Nakanuma Y, Kondo F, Hachiya H, Miyazaki M, Nagino M, et al. Clinicopathological features and prognosis of mucin-producing bile duct tumor and mucinous cystic tumor of the liver: a multi-institutional study by the Japan Biliary Association. J Hepato-Biliary Pancreat Sci. 2014;21:176–85.
Zen Y, Pedica F, Patcha VR, Capelli P, Zamboni G, Casaril A, et al. Mucinous cystic neoplasms of the liver: a clinicopathological study and comparison with intraductal papillary neoplasms of the bile duct. Mod Pathol. 2011;24:1079–89.
Mortelé KJ, Ros PR. Cystic focal liver lesions in the adult: differential CT and MR imaging features. Radiographics. 2001;21:895–910.
Nakayama Y, Kato Y, Okubo S, Takahashi D, Okada R, Nishida Y, et al. A case of mucinous cystic neoplasm of the liver: a case report. Surg Case Rep. 2015;1:9.
Takano Y, Nagahama M, Yamamura E, Maruoka N, Mizukami H, Tanaka JI, et al. Prolapse into the bile duct and expansive growth is characteristic behavior of mucinous cystic neoplasm of the liver: report of two cases and review of the literature. Clin J Gastroenterol. 2015;8:148–55.
Erdogan D, Kloek J, Lamers WH, Offerhaus GJA, Busch ORC, Gouma DJ, et al. Mucinous cystadenomas in liver: management and origin. Dig Surg. 2010;27:19–23.
Sutton CD, White SA, Berry DP, Dennison AR. Intrahepatic biliary cystadenoma causing luminal common bile duct obstruction. Dig Surg. 2000;17:297–9.
Shima Y, Horimi T, Shibuya Y, Sakurama K, Nishie M, Morita S. Resected cystadenoma of the common bile duct. J Hepato-Biliary Pancreat Surg. 2004;11:438–40.
Park JH, Lee DH, Kim HJ, Ko YT, Lim JW, Yang MH. Unilocular extrahepatic biliary cystadenoma mimicking choledochal cyst: a case report. Korean J Radiol. 2004;5:287–90.
Preetha M, Chung AYF, Lim-Tan SK, Lim DTH, Thng CH. Intrahepatic biliary cystadenoma presenting with obstructive jaundice. Asian J Surg. 2004;27:243–5.
Baudin G, Novellas S, Buratti MS, Saint-Paul MC, Chevallier P, Gugenheim J, et al. Atypical MRI features of a biliary cystadenoma revealed by jaundice. Clin Imaging. 2006;30:413–5.
Gonzalez M, Majno P, Terraz S, Morel P, Rubbia-Brandt L, Mentha G. Biliary cystadenoma revealed by obstructive jaundice. Dig Liver Dis. 2009;41:e11–3.
Siriwardana PN, Pathirana A. Episodic biliary obstruction due to an intrahepatic biliary cystadenoma: a case report. J Med Case Rep. 2009;3:9032.
Yi B, Cheng QB, Jiang XQ, Liu C, Luo XJ, Dong H, et al. A special growth manner of intrahepatic biliary cystadenoma. World J Gastroenterol. 2009;15:6134–6.
Saravanan MN, Singh B, Ravindranath K, Raghavendra RRV. Episodic jaundice due to an intrahepatic biliary cystadenoma with biliary stricture masquerading as hydatid cyst. Trop Gastroenterol. 2010;31:332–5.
Hennessey DB, Traynor O. Extrahepatic biliary cystadenoma with mesenchymal stroma: a true biliary cystadenoma? A case report. J Gastrointest Liver Dis. 2011;20:209–11.
Harmouch T, Vullierme MP, Sauvanet A, Paradis V, Amarti A. Hepatobiliary cystadenoma revealed by a jaundice: a case report. Case Rep Gastrointest Med. 2011;2011:895605.
Vyas S, Markar S, Ezzat T, Rodriguez-Justo M, Webster G, Imber C, et al. Hepato-biliary cystadenoma with intraductal extension: unusual cause of obstructive jaundice. J Gastrointest Cancer. 2012;43 Suppl 1:S32-37.
Soochan D, Keough V, Wanless I, Molinari M. Intra and extra-hepatic cystadenoma of the biliary duct. Review of literature and radiological and pathological characteristics of a very rare case. BMJ Case Rep. 2012. https://doi.org/10.1136/bcr.01.2012.5497.
Abe Y, Kasuya K, Itoi T, Kikuchi S, Ikeuchi N, Ishii K, et al. Hepatobiliary cystadenoma of the liver prolapsing into the extrahepatic bile duct (with video). Gastrointest Endosc. 2012;75:1099 (discussion 1099–1100).
Rayapudi K, Schmitt T, Olyaee M. Filling defect on ERCP: biliary cystadenoma, a rare tumor. Case Rep Gastroenterol. 2013;7:7–13.
Chandrasinghe PC, Liyanage C, Deen KI, Wijesuriya SR. Obstructive jaundice caused by a biliary mucinous cystadenoma in a woman: a case report. J Med Case Rep. 2013;7:278.
Pattarapuntakul T, Ovartlarnporn B, Sottisuporn J. Mucinous cystic neoplasm of the liver with extrahepatic growth presenting with ascending cholangitis diagnosed by endoscopic ultrasound features: a case report. J Med Case Rep. 2018;12:33.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
YF and AM wrote the first draft of the manuscript, which was revised by AK. YF, AM, SS, KS and TO performed the surgery. TT, SK, and AK participated in the postoperative management. TO contributed to pathological diagnosis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Informed consent was obtained from the patient for publication of this case report and any accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fukui, Y., Murata, A., Shimizu, S. et al. Mucinous cystic neoplasm of the liver with polypoid nodule prolapsing into the bile duct: a case report and review of literature. surg case rep 8, 177 (2022). https://doi.org/10.1186/s40792-022-01511-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-022-01511-9