Abstract
Background
Surgery for perforated rectal cancer is technically difficult because of paralytic dilatation due to generalized fecal peritonitis, the presence of a bulky tumor, and fecal retention due to obstruction. Transanal total mesorectal excision (TaTME) is the latest minimally invasive transanal technique pioneered to facilitate difficult pelvic dissections. It can provide a good surgical field linearly from the perineal side and reduce manipulations from the intraabdominal side. Here, we present two cases of emergency TaTME performed for perforated rectal cancer.
Case presentation
The patients were a 38-year-old female and a 75-year-old male. They were diagnosed with perforated rectal cancer and were in a state of septic shock. Emergency Hartmann’s procedure was performed in both cases. Intraoperative findings showed fecal contamination of the entire abdomen and dilated intestines and bulky tumors with perforation. The female patient had multiple uterine fibroids, and the male patient had an enlarged prostate. For both patients, dissection of the mesorectum to the anal side of the tumor and transection of the rectum on the anal side of the tumor via a linear stapler were considered difficult because of the insufficient surgical field of view into the pelvis. Therefore, a two-team approach with TaTME was adopted. En bloc resection of the rectum was completed by collaboration of the abdominal team and the transanal team, and the autonomic nerves were successfully preserved. Finally, the specimens were resected, and the anal edge of the rectum was closed with a purse-string suture by the transanal team. Although these two cases were emergency surgeries in difficult situations, the cancer lesions were successfully and safely removed without involvement of the resection margin.
Conclusions
This is the first report of emergency TaTME. Although these cases were emergency operations in a situation where it was difficult to pursue radical resection—and often times in these situations, the operation may end with only stoma creation—the specimens were safely resected. Emergency TaTME is a useful procedure for treatment of perforated rectal cancer.
Similar content being viewed by others
Background
Perforated colorectal cancer, which frequently leads to septic shock, is an extremely serious condition with high mortality and morbidity rates [1,2,3]. Patients undergo surgery with the dual life threats of a malignant disease and sepsis due to perforated peritonitis. Moreover, the operation is complicated by factors, such as paralytic bowel dilatation from generalized fecal peritonitis, bulkiness of the tumor, and fecal retention due to obstruction.
Total mesorectal excision (TME) for rectal cancer is a widely performed procedure. However, the transection of the rectum with a linear stapler becomes difficult because of the limitations either in visualizing or in handling the linear cutter in the deep pelvic space, especially for male patients with narrow pelvises, extreme obesity, bulky tumors, large uterine fibroids, enlarged prostates, or tumors in the lower rectum. Transanal total mesorectal excision (TaTME) is the latest minimally invasive transanal technique pioneered to facilitate difficult pelvic dissections [4]. Although it is difficult to pursue radical resection for perforated rectal cancer, and the operation may end with only stoma creation without tumor resection, the application of TaTME allows for a relatively short operation time while ensuring the ability to cure the cancer. At our institution, we have adopted and have been promoting the two-team approach with TaTME for difficult cases of perforated rectal carcinoma with poor surgical views while maintaining speed and safety, which are both important factors when performing emergency surgery. To the best of our knowledge, this is the first report of emergency TaTME.
Case presentation
Case 1: A 38-year-old female patient was brought to the hospital urgently with complaints of abdominal pain and high fever and was diagnosed with obstructive rectal cancer 8 cm from the anal verge, with multiple liver metastases as well as multiple uterine fibroids (Fig. 1). The cancer had perforated, causing panperitonitis, and she was in a state of septic shock. Emergency laparoscopic Hartmann’s procedure was performed. A 12-mm trocar was inserted through an umbilical incision, and then the pneumoperitoneum was created. Another 12-mm trocar was placed in the right lower quadrant, and three 5-mm trocars were inserted in the left lower quadrant and bilateral lateral regions.
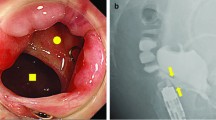
Computed tomography in Case 1. a Computed tomography showed a large amount of fecal mass in the colon and free air (yellow arrows) in the pelvis. A large mass was observed in the liver. b There was wall thickening in the rectum (yellow arrows), and the oral side of the rectum was dilated and had a fecal mass. Multiple uterine fibroids were seen, and ascites with free air was observed around them
Laparoscopic examination revealed fecal contamination of the entire abdomen, a dilated intestinal tract, and multiple uterine fibroids. A bulky tumor was observed at the peritoneal reflexion, and the perforation was on the anterior wall of the tumor. Resection of the perforated rectum along with the tumor was considered necessary. The uterus was lifted up to the abdominal wall; however, the surgical view in the pelvis was poor, and it was judged that the dissection of the mesorectum to the anal side of the tumor and the transection of the rectum on the anal side of the tumor with a linear stapler would be technically difficult.
Therefore, a two-team approach with TaTME was adopted. The details of this technique have been described in other reports [5,6,7]. Then, en bloc resection of the rectum was completed by collaboration with the transanal team while preserving the autonomic nerves. Finally, the specimen was removed, and the anal side of the rectum was closed with a purse-string suture by the transanal team (Fig. 2). The operative time was 205 min with a small amount of blood loss. On the 7th postoperative day, the drain discharge became cloudy, suggesting the presence of a pelvic abscess. Contrast examination through the drain showed no residual rectum, and the stump rupture was negative. Drainage gradually decreased, the drain was removed on Day 21, and the patient was discharged on Day 25. Pathological examination confirmed tubular adenocarcinoma of the rectum (pT3N2a [5/16]), with negative margins and a complete mesorectum (Fig. 3a). Chemotherapy aimed at conversion surgery for liver metastases was started. As a result, the patient underwent complete liver metastasis resection by “liver resection by associating liver partition and portal vein ligation for staged hepatectomy (ALPPS)” 7 months after the initial surgery. Ten months have passed since the initial surgery, and the patient is still alive without recurrence.
Resected specimen. a Case 1: pathological findings were 90 × 56 mm, well-differentiated adenocarcinoma (tub1), pT3, pN2 [5/16] and distal margin of 28 mm. b Case 2: pathological findings were 65 × 58 mm, well-differentiated adenocarcinoma (tub1), pT3, pN0 [0/13] and distal margin of 20 mm. A perforation was observed in the rectal sigmoid colon away from the tumor
Case 2: A 75-year-old male who underwent drug therapy for an enlarged prostate experienced abdominal pain after taking laxatives for colonoscopy. After a thorough examination, the patient was diagnosed with obstructive rectal cancer 7 cm from the anal verge and perforation of the rectum on the oral side of the tumor (Fig. 4). He was in a state of septic shock. Emergency open Hartmann’s procedure was performed. The rectum was perforated toward the mesentery, and furthermore, the peritoneum was perforated, and contaminated ascites was found in the peritoneal cavity. He had a narrow pelvis with a bulky tumor, and intestinal dilatation was observed due to fecal impaction. It was believed that dissection of the mesorectum to the anal side of the tumor and transection of the rectum on the anal side of the tumor with a linear stapler would be difficult. Therefore, a two-team approach with TaTME was adopted (Fig. 5). After that, the same procedure was performed as for Case 1. The operative time was 194 min with a small amount of blood loss. Pathological examination confirmed tubular adenocarcinoma of the rectum (pT3N0 [0/10]), with negative margins and a complete mesorectum (Fig. 3b). The postoperative clinical course was good, and the patient was discharged from the hospital on the 17th postoperative day. One year has passed since the surgery, and the patient is currently recurrence-free.
Discussion
The mortality rate for perforated colorectal cancer is as high as 11–44% [1,2,3]. Perforated colorectal cancer accounts for 14–21% of colorectal perforations, and such cases have been reported to have a higher mortality rate than other types of perforations [8]. Perforated colorectal cancer also often causes septic shock. Sepsis and frequent postoperative complications exacerbate the condition and increase mortality. Even if patients survive the emergency situation, the risk of local recurrence and the survival rate are poor [9, 10].
The operation for perforated colorectal cancer is difficult because of paralytic bowel dilatation with generalized fecal peritonitis, the presence of a bulky tumor, and fecal retention due to obstruction. In addition to performing surgery for life-saving purposes, it is also necessary to aim to cure the cancer. The perforated section should be resected to prevent the patient from being exposed to fecal contents. Resection is necessary to prevent tumor cells from spilling into the abdominal cavity. The 2017 World Journal of Emergency Surgery (WSES) guidelines recommend performing Hartmann’s procedure for perforated colorectal cancer patients in an unstable condition, such as patients with any signs of sepsis or septic shock [11]. The two cases we experienced were in a state of septic shock; thus, we performed Hartmann's procedure. If the perforation is in the rectum, a bulky tumor has to be removed in a narrow pelvis (especially in obese men). Large uterine fibroids and enlarged prostates may worsen the situation. In this study, the first case was a patient with a large uterine fibroid, and the tumor had invaded the peritoneal reflection; the second case was a male patient with a narrow pelvis and a large prostate.
TaTME was first reported by Sylla in 2010 [12] and is gradually being performed worldwide, especially in Europe. This is a novel technique developed to alleviate the difficulty of resecting mid and low rectal cancer, where the pelvis is anatomically strongly inclined. It can help provide a good surgical field even under difficult conditions, and the procedure can be performed linearly from the perineal side [5]. Ensuring a circumferential resection margin (CRM) is essential to decrease the rate of local recurrence [13]. However, ensuring a CRM with TME performed via the traditional transabdominal approach is technically difficult and is oncologically problematic for obese patients and for patients with bulky tumors, a large uterine fibroid, or a large prostate [14, 15]. In such cases, the CRM may be positive. CRM positivity is the factor most associated with local recurrence, and it influences the distant metastasis rate and the overall survival rate [13].
The International TaTME Registry group showed that a CRM is better secured with TaTME than with laparoscopic TME [4]. According to a systematic review that compared the pathological results of TaTME and laparoscopic TME for rectal cancer, TaTME has a lower rate of CRM positivity and is able to secure a larger CRM as well as the distal margin (DM). TaTME is superior in securing the CRM and DM [16]. Moreover, the two-team approach enables the operation to be performed in a coordinated manner from both the abdominal cavity and the perineal side.
Since there are no coherent reports of perforated rectal cancer, the results of the abdominal approach alone are unknown. However, despite the difficulty of the surgery, emergency TaTME allowed us to perform the surgery while securing both the CRM and the DM. There are two limitations to this technique. One is the high manpower requirement. It is difficult to gather enough surgeons to perform a surgery with a two-team approach in an emergency situation. In the two reported cases, we were only able to use the two-team approach from midway into the surgery. Applying the two-team approach from the beginning would have resulted in a significant reduction in the operation time, as well as an overall better outcome and postoperative course for the two patients with septic shock. The other limitation is the lack of long-term oncological results. Case 1 is 10 months post-operation, and Case 2 is 1 year post-operation, so long-term oncological results are not available to show in this case report. Case 1 was treated with chemotherapy for liver metastasis and conversion surgery using ALPPS. Both cases had good short-term results with no recurrence at the time of this report.
Conclusions
This report presents two cases of perforated rectal cancer treated by emergency TaTME. Although these cases were emergency operations in a situation where it was difficult to pursue radical resection and TaTME may end with only stoma creation, the specimens were safely resected without involvement of the resection margin. Emergency TaTME is considered to be a useful procedure for treatment of perforated rectal cancer.
Availability of data and materials
Not applicable.
Abbreviations
- TME:
-
Total mesorectal excision
- TaTME:
-
Transanal total mesorectal excision
- CRM:
-
Circumferential resection margin
- DM:
-
Distal margin
References
Gök MA, Kafadar MT, Yeğen SF. Perforated colorectal cancers: clinical outcomes of 18 patients who underwent emergency surgery. Prz Gastroenterol. 2021;16(2):161–5.
Tan KK, Hong CC, Zhang J, Liu JZ, Sim R. Surgery for perforated colorectal malignancy in an Asian population: an institution’s experience over 5 years. Int J Colorectal Dis. 2010;25(8):989–95.
Lee IK, Sung NY, Lee YS, Lee SC, Kang WK, Cho HM, et al. The survival rate and prognostic factors in 26 perforated colorectal cancer patients. Int J Colorectal Dis. 2007;22(5):467–73.
Penna M, Hompes R, Arnold S, Wynn G, Austin R, Warusavitarne J, et al. Transanal total mesorectal excision: international registry results of the first 720 cases. Ann Surg. 2017;266(1):111–7.
Lacy AM, Tasende MM, Delgado S, Fernandez-Hevia M, Jimenez M, De Lacy B, et al. Transanal total mesorectal excision for rectal cancer: outcomes after 140 patients. J Am Coll Surg. 2015;221(2):415–23.
Arroyave MC, DeLacy FB, Lacy AM. Transanal total mesorectal excision (TaTME) for rectal cancer: step by step description of the surgical technique for a two-teams approach. Eur J Surg Oncol. 2017;43(2):502–5.
Trépanier JS, Fernandez-Hevia M, Lacy AM. Transanal total mesorectal excision: surgical technique description and outcomes. Minim Invasive Ther Allied Technol. 2016;25(5):234–40.
Kriwanek S, Armbruster C, Dittrich K, Beckerhinn P. Perforated colorectal cancer. Dis Colon Rectum. 1996;39(12):1409–14.
Ho YH, Siu SK, Buttner P, Stevenson A, Lumley J, Stitz R. The effect of obstruction and perforation on colorectal cancer disease-free survival. World J Surg. 2010;34(5):1091–101.
Asano H, Kojima K, Ogino N, Fukano H, Ohara Y, Shinozuka N. Postoperative recurrence and risk factors of colorectal cancer perforation. Int J Colorectal Dis. 2017;32(3):419–24.
Pisano M, Zorcolo L, Merli C, Cimbanassi S, Poiasina E, Ceresoli M, et al. 2017 WSES guidelines on colon and rectal cancer emergencies: obstruction and perforation. World J Emerg Surg. 2018;13:36.
Sylla P, Rattner DW, Delgado S, Lacy AM. NOTES transanal rectal cancer resection using transanal endoscopic microsurgery and laparoscopic assistance. Surg Endosc. 2010;24(5):1205–10.
Nagtegaal ID, Quirke P. What is the role for the circumferential margin in the modern treatment of rectal cancer? J Clin Oncol. 2008;26(2):303–12.
Atallah S, Martin-Perez B, Albert M, deBeche-Adams T, Nassif G, Hunter L, et al. Transanal minimally invasive surgery for total mesorectal excision (TAMIS-TME): results and experience with the first 20 patients undergoing curative-intent rectal cancer surgery at a single institution. Tech Coloproctol. 2014;18(5):473–80.
Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ, et al. Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA. 2015;314(13):1356–63.
Jiang HP, Li YS, Wang B, Wang C, Liu F, Shen ZL, et al. Pathological outcomes of transanal versus laparoscopic total mesorectal excision for rectal cancer: a systematic review with meta-analysis. Surg Endosc. 2018;32(6):2632–42.
Acknowledgements
None.
Funding
This work was supported by JSPS KAKENHI Grant Number JP 21H03244.
Author information
Authors and Affiliations
Contributions
HE operated on the patients and drafted the manuscript. KS critically revised the manuscript. TO and KE approved the final manuscript. NT, YT and TU managed pre- and postoperative care. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patients for the publication of this case report.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Enomoto, H., Suwa, K., Takeuchi, N. et al. Emergency transanal total mesorectal excision for perforated rectal cancer: a two-case series. surg case rep 8, 120 (2022). https://doi.org/10.1186/s40792-022-01480-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-022-01480-z