Abstract
Background
Calcifying fibrous tumors (CFTs) are rare benign tumors. Because CFTs sometimes relapse, radical resection with adequate margins is necessary. We report a case of ileal CFT resected using single-port laparoscopic surgery.
Case presentation
A 33-year-old man presented with chief complaints of abdominal pain and vomiting. Computed tomography demonstrated a 45-mm-sized pelvic mass with partial calcification in the ileum. The patient was diagnosed with an ileal tumor, and partial resection of the ileum was performed using the single-port laparoscopic technique. Pathologic findings revealed hypocellular spindle cells with dense hyalinized collagen, interspersed calcification, and infiltration of lymphoplasmacytic cells. Immunohistochemical analysis showed that the factor XIIIa was positive and other tumor-specific markers were negative. Based on these findings, the tumor was finally diagnosed as a CFT.
Conclusions
Although CFT is benign, multifocal and recurrent CFTs have been reported. Therefore, careful intraperitoneal observation and curative resection are necessary. Single-port laparoscopic surgery is acceptable, both in terms of curability and minimal invasiveness.
Similar content being viewed by others
Background
Calcifying fibrous tumors (CFTs) are rare benign tumors characterized by hypocellular spindle cells, hyalinized collagen, lymphoplasmacytic infiltrate, and scattered calcification, and are categorized as bone and soft-tissue tumors [1]. However, CFTs can occur in any part of the body, including the gastrointestinal tract [2].
A curative resection of CFTs with a sufficient margin is necessary, and in most cases, laparotomy has been performed [2]. In recent years, however, there have been advances in laparoscopic surgery, and laparoscopic resection of CFTs has also been reported in some cases [3,4,5]. Single-port laparoscopic surgery, in which all laparoscopic working ports approach the abdominal wall through the same incision, has been developed as a much less invasive method and has been reported to provide better cosmetic results, reduced postoperative pain, and improved oncological safety [6].
Herein, we present a case of ileal CFT resected using single-port laparoscopic surgery.
Case presentation
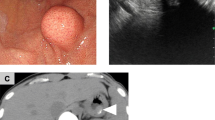
A 33-year-old man without a previous medical or surgical history presented with chief complaints of abdominal pain and vomiting. Physical examination revealed tenderness in the lower abdomen. Laboratory data were unremarkable: C-reactive protein level, 0.16 mg/dL; white blood cell count, 9600 /μL; neutrophil count, 91.3%; and lymphocyte count, 5.4%. Ultrasonography and radiography revealed no findings that could cause abdominal pain. Contrast-enhanced computed tomography (CT) demonstrated a 45-mm-sized mass with partial calcification in the ileum (Fig. 1), without any signs of invagination, obstruction, or volvulus. No other findings suggesting the cause of abdominal pain were observed on CT. The patient was diagnosed with an ileal tumor. After the examination, the patient’s condition improved spontaneously. Several weeks later, for detailed examination of the tumor, magnetic resonance imaging (MRI) was performed, which revealed a tumor with hypointense signal on both T1-weighted (T1WI) and T2-weighted images (T2WI), and isointense signal on gadolinium-enhanced T1WI (Fig. 1). Based on these findings, the differential diagnoses were a gastrointestinal stromal tumor, chronic distending hematoma, leiomyoma, and CFT.
CT and MRI images. A 45-mm-sized mass (blue arrow head) with partial calcification was observed in the ileum on enhanced CT. The mass was hypointense signal on both T1WI and T2WI, and isointense signal on gadolinium-enhanced T1WI. CT computed tomography, MRI magnetic response image, T1WI T1-weighted image, T2WI T2-weighted image
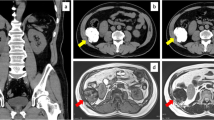
Laparoscopic surgery was performed for the pathological diagnosis and treatment. Two 5-mm ports were placed through a vertical 4-cm skin incision in the umbilicus using EZ access and Lap Protector (Hakko Medical, Nagano, Japan). Intraoperatively, a white-colored tumor was found in the ileum, 100 cm from the terminal ileum (Fig. 2). Careful observation of the entire abdominal cavity did not detect any other tumors, lymph node metastasis, or dissemination. After careful observation, the tumor was lead extracorporeally through the umbilical incision and a partial resection of the ileum was performed. Reconstruction was performed with a functional end-to-end anastomosis. Macroscopic findings revealed that the tumor was pedunculated and located on the antimesenteric side. Microscopic findings revealed that the tumor extended from the muscularis propria to the subserosa. A few spindle cells and infiltration of lymphoplasmacytic cells were observed with dense hyalinized collagen and interspersed calcification in the background (Fig. 3). Immunohistochemical findings revealed negative or nearly negative results for CD34, c-kit, DOG-1, desmin, S100, anaplastic lymphoma kinase, vimentin and smooth muscle actin. Factor-XIIIa was positive. The MIB-1 labeling index was less than 1%. Over 40% of the plasma cells in the stroma were IgG4 positive. The tumor was eventually diagnosed as a CFT. The patient was discharged on postoperative day 7 without any complications. No recurrence has been observed in the 6 months since the surgery.
Discussion
CFT was first described as “childhood fibrous tumor with psammoma bodies” by Rosenthal et al. in 1988 [7]. CFTs can originate from anywhere in the gastrointestinal tract, including the small intestine. Pezhouh et al. reported a total of 13 CFT cases in the small intestine out of 28 cases of CFTs originating from the gastrointestinal tract and most cases were discovered incidentally [8]. However some cases were accompanied by acute abdominal symptoms and a summary of previous reports is shown in Table 1. [3,4,5, 9,10,11,12,13,14,15,16,17,18,19]. In this case, CT for abdominal symptoms detected the mass. Although CT findings did not show any evidence of obstruction, invagination, or volvulus caused by the mass, these phenomena may have occurred temporarily because other findings causing digestive symptoms were not observed. Temporary volvulus of the tumor with a stalk may be released immediately. Therefore, the possibility of CFTs causing acute abdominal symptoms should be considered.
CFT is a round hyper- or hypodense mass with calcification on CT, hypointense signal on T1WI and T2WI, and isointense signal on gadolinium-enhanced T1WI [2]. Microscopically, hypocellular spindle cells are observed against the background of abundant hyalinized collagen, along with scattered calcifications and lymphoplasmacytic infiltrates [8, 20]. Immunohistochemically, CFT is positive for Factor XIIIa, vimentin, and CD34, and negative for c-kit, DOG-1, desmin, S100, anaplastic lymphoma kinase, and smooth muscle actin [2, 21]. In this case, CT detected a hypointense mass with calcification, and MRI demonstrated that the mass was hypointense on T1WI and T2WI and isointense on gadolinium-enhanced T1WI. These findings are similar to those of previous reports. Microscopic findings of this case, characterized by hypocellular spindle cells, dense hyalinized collagen, interspersed calcifications, and lymphoplasmacytic infiltrates, were also consistent with previous reports. As for the immunohistochemical findings, factor XIIIa was positive and other tumor specific markers were negative. In addition, the MIB-1 index was low, suggesting a low cell growth potential. These results led to the diagnosis of CFT. Although small intestine CFT is rare and similar to other tumors such as GIST, it is important to consider this entity based on the imaging and pathological findings to avoid misdiagnosis.
CFT is a benign tumor and no recurrence of small intestine CFTs was reported (Table 1), while the recurrence rate of all types of CFTs is reported to be 10% [2]. Therefore, complete surgical resection is required. Although no cases of distant metastasis have been reported, some reports have shown multifocal lesions [9, 10, 13]. In addition, as CFTs are often located in the peritoneum or other organs, including the gastrointestinal tract in the abdomen [2], observation of the entire intraperitoneal region is important. Laparoscopic surgery is favorable for extensive intraabdominal observation through a small incision when compared with open laparotomy. Furthermore, we used a single-port laparoscopic technique to observe the entire abdominal cavity and resect the tumor in this case. Single-port laparoscopic surgery is cosmetically superior to multiport surgery [6]. Although single-port surgery requires technical training, the safety of single-port laparoscopic surgery has been reported to be compatible with conventional surgery [6]. Additional port placement can overcome the difficulty of single-port surgery. Therefore, single-port laparoscopic surgery for small intestine tumors, including CFT, is a reasonable method in terms of safety, reliability, and minimal invasiveness.
In summary, CFT is a rare benign lesion that may cause acute abdominal pain. After careful consideration based on the CT, MRI, or microscopic findings, single-port laparoscopic surgery is appropriate in terms of curability and minimal invasiveness.
Availability of data and materials
Not applicable.
Abbreviations
- CFT:
-
Calcifying fibrous tumor
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- T1WI:
-
T1-weighted image
- T2WI:
-
T2-weighted image
References
The WHO Classification of Tumors Editional Board. WHO classification of tumors soft tissue and bone tumours. 5th ed. Lyon: IARC Press; 2020.
Chorti A, Papavramidis TS, Michalopoulos A. Calcifying fibrous tumor: review of 157 patients reported in international literature. Medicine (Baltimore). 2016;95:e3690.
Murakami T, Nakagawa K, Suzuki Y. A case of calcifying fibrous predotumor of the jejunum treated by laparoscopic resection. J Clin Surg. 2006;10:1417–20 (In Japanese).
Hort A, Chen AZL, Moghadam A, Pang T. Calcifying fibrous tumour torsion: a rare cause of abdominal pain. BMJ Case Rep. 2020;13:e238220.
Nishina Y, Mori H, Miyake R, Tani S, Ueki T, Iida H, et al. A case of calcifying fibrous tumor of the small intestine treated by laparoscopic small bowel resection. Jpn J Gastroenterol Surg. 2020;53:901–7 (In Japanese).
Takemasa I, Sekimoto M, Ikeda M, Mizushima T, Yamamoto H, Doki Y, et al. Transumbilical single-incision laparoscopic surgery for sigmoid colon cancer. Surg Endosc. 2010;24:2321.
Rosenthal NS, Abdul-Karim FW. Childhood fibrous tumor with psammoma bodies. Clinicopathologic features in two cases. Arch Pathol Lab Med. 1988;112:798–800.
Pezhouh MK, Rezaei MK, Shabihkhani M, Ghosh A, Belchis D, Montgomery EA, et al. Clinicopathologic study of calcifying fibrous tumor of the gastrointestinal tract: a case series. Hum Pathol. 2017;62:199–205.
Chen KT. Familial peritoneal multifocal calcifying fibrous tumor. Am J Clin Pathol. 2003;119:811–5.
Liang HH, Chai CY, Lin CH, Lee CH, Wu CH, Chang CC. Jejunal and multiple mesenteric calcifying fibrous pseudotumor induced jejunojejunal intussusception. J Formos Med Assoc. 2007;106:485–9.
Emanuel P, Qin L, Harpaz N. Calcifying fibrous tumor of small intestine. Ann Diagn Pathol. 2008;12:138–41.
Giardino AA, Ramaiya NH, Shinagare AB, Jagannathan JP, Stachler MD, Raut CP. Case report: calcifying fibrous tumor presenting as an asymptomatic pelvic mass. Indian J Radiol Imaging. 2011;21:306–8.
Tseng IT, Chen S-T, Huang Z-Z, Tung H-I, Ker C-K. Multiple calcifying fibrous tumors in the small intestine and the mesentery. Formos J Surg. 2012;45:33–6.
Takeji M, Ninomiya K, Kito K, Furuya K, Maeda T, Yoshiyama H. Calcifying fibrous tumor of the small intestine: a case report. Jpn J Diag Pathol. 2013;30:305–8 (In Japanese).
Valladolid G, Weisenberg E, Sundaresan R, Maker AV. Calcifying fibrous tumor of the small intestine associated with castleman-like lymphadenopathy. J Gastrointest Surg. 2014;18:1205–8.
Wesecki M, Radziuk D, Niemiec S, Waniczek D, Lorenc Z. Calcifying fibrous tumor of the small bowel mesentery in a 27-year old male patient—case report. Pol Przegl Chir. 2014;86:436–9.
Minami T, Nishihira T, Miki A, Morioka H, Suzuki T, Otani T, et al. A calcifying fibrous tumor which developed in the small intestine causing ileus. Jpn J Gastroenterol Surg. 2015;48:436–41 (In Japanese).
Luques L, Atlan KA, Shussman N. A rare benign gastrointestinal lesion identified as a calcifying fibrous tumor. Clin Gastroenterol Hepatol. 2017;15:A25.
Sotiriou S, Papavramidis T, Hytiroglou P. Calcifying fibrous tumor of small bowel causing intussusception. Clin Gastroenterol Hepatol. 2019;17:e95.
Turbiville D, Zhang X. Calcifying fibrous tumor of the gastrointestinal tract: a clinicopathologic review and update. World J Gastroenterol. 2020;26:5597–605.
Zhou J, Zhou L, Wu S, Li R, Yang X, Xu H, et al. Clinicopathologic study of calcifying fibrous tumor emphasizing different anatomical distribution and favorable prognosis. BioMed Rese Int. 2019;2019:5026860.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
No funding was received for this case report.
Author information
Authors and Affiliations
Contributions
The first draft of the manuscript was written by KT and TA. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in this case report were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Ethical approval from the Facility of Science Committee at the Kyoto Prefectural University of Medicine was not required, as the present study was a case report without interventions for therapeutic purposes.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Takabatake, K., Arita, T., Kuriu, Y. et al. Calcifying fibrous tumor of the ileum resected by single-port laparoscopic surgery: a case report. surg case rep 8, 64 (2022). https://doi.org/10.1186/s40792-022-01423-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-022-01423-8