Abstract
Background
Cap polyposis (CP) is extremely rare in Japan, and there is no established cure. We report a case in which CP was improved by surgical treatment.
Case presentation
A 48-year-old man was investigated at a local hospital because of diarrhea and bloody stools in 2018. The patient was treated with metronidazole for suspected amoebic dysentery, but his symptoms did not improve. Subsequent close examination revealed possible CP, but treatment with 5-aminosalicylic acid and a steroid enema had no effect. The patient was then referred to our hospital. The bloody stools, diarrhea, and abdominal pain worsened despite medical treatment, so laparoscopic-assisted total proctocolectomy and ileal J-pouch anal anastomosis with ileostomy were performed. CP has no known cause or established treatment, but Helicobacter pylori (HP) infection has been reported in many CP cases in Japan, and HP eradication is often successful. This patient was HP-negative and did not improve with antimicrobial treatment, but the symptoms improved after surgery.
Conclusions
Even after surgery, CP recurrence reportedly occurs within a short period in many cases. However, our patient has had no signs of CP recurrence during 1 year of follow-up.
Similar content being viewed by others
Cap polyposis (CP) is an inflammatory disease of the large intestine that was first reported in 1985 and has characteristic clinical, endoscopic, and histopathological findings [1]. Some cases of CP have been reported in Japan, but it is an extremely rare disease that is difficult to differentiate from other inflammatory bowel diseases. The etiology of CP is unclear and there is no established cure. Even after surgery, recurrence within a short period is common [2, 3]. In Japan, it has been reported that Helicobacter pylori (HP) eradication is successful in the treatment of CP [2, 4]. Herein, we report a case in which surgical treatment was effective for CP resistant to medical treatment.
Case presentation
A 48-year-old man presented at a local hospital because of diarrhea and bloody stools in 2018 and was started on probiotics. There was no relevant medical history and/or family history. The patient’s symptoms did not improve, and he represented at the local hospital 2 months later. Total colonoscopy (TCS) revealed wart-like erosions resembling octopus suckers from the sigmoid colon to the rectum, suggesting amoebic dysentery. However, stool cultures and biopsied colonic mucosa did not show dysenteric amoebae at that time. The patient was started on oral metronidazole (MNZ), but the symptoms did not improve and there were no improvements seen on repeat TCS performed 2 months later. The patient was also negative for amoebic dysentery antibody at that time and CP was suspected based on the TCS findings, but a definitive diagnosis was not reached. Administration of oral 5-aminosalicylic acid (5-ASA) and a steroid enema also resulted in no improvements in the symptoms. The patient was then referred to the Department of Internal Medicine of our hospital for further examination and medical treatment.
TCS performed at our hospital revealed reddened mucosa and multiple raised lesions from the middle of the transverse colon to the rectum; these lesions were covered with white moss (Fig. 1). Pathological examination showed inflammatory cell infiltration in the interstitium, and granulation tissue in the superficial layer, consistent with CP. A diagnosis of CP was made based on the clinical symptoms, and endoscopic and pathological findings. The patient was negative for HP. However, as all other treatments had been ineffective and HP eradication has been reported to be effective in treating CP in Japan, a proton pump inhibitor, amoxicillin, and clarithromycin were administered. The symptoms persisted despite these treatments, and the patient’s weight reduced from 78 to 60 kg.
In May 2019, the patient was admitted to the Department of Internal Medicine of our hospital due to exacerbation of his symptoms. Laboratory tests showed hypoalbuminemia, mild elevations in the C-reactive protein level and erythrocyte sedimentation rate, and a normal white blood cell count. There were no abnormal stool culture findings on admission. The patient was resistant to medical treatment and was admitted to our department, because he wished to undergo surgery.
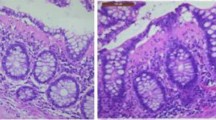
Intraoperatively, we found polyps from the rectum to the middle of the transverse colon, and inflammation in the anal canal. Therefore, we performed a laparoscopic-assisted total proctocolectomy and J-type ileal pouch anal anastomosis (IPAA) with ileostomy (Fig. 2). After the operation, his symptoms rapidly improved, and he started eating on postoperative day 3. He was discharged without problems on postoperative day 14. Postoperative pathological examination of the resected specimen showed multiple elevated lesions from the descending colon to the rectum. The apex of each lesion was capped with granulation tissue with inflammatory exudate, and the crypt epithelium was hyperplastic, consistent with CP (Fig. 3). There was no recurrence of symptoms or polyps in the ileal pouch, and stoma closure was performed 3 months after surgery. Approximately 1 year has passed since the stoma closure, and there has been no recurrence observed.
Discussion
There are no definitive diagnostic criteria for CP. CP is a condition in which nonspecific inflammatory polyps develop mainly in the rectum and sigmoid colon, and the symptoms of CP are mucus secretion, diarrhea, bloody stools, and sometimes abdominal pain [2]. Blood tests often show hypoproteinemia, and the characteristic endoscopic findings of CP include multiple broad-based bulging lesions from the rectum to the sigmoid colon, with mucus attachment on the surface [2]. Pathological examination shows that the mucosal surface of the lesions is covered with inflammatory granulation tissue, which is called Cap [2]. The diagnosis of CP in Japan is based on the abovementioned characteristic symptoms and examination findings, which were used to diagnose CP in the present patient.
It has been theorized that the mechanism of CP may be mechanical stimulus or infection, but the definitive cause remains unknown [1, 2, 4]. There is currently no established treatment for CP, although various treatments have been used. 5-ASA is often ineffective in treating CP, while steroids cause temporary improvements followed by relapse [2, 5]. Although there are reports that MNZ is effective for CP [6], there are also reports that MNZ is ineffective [1, 2]; the response rate of MNZ is 28.6% [5]. Similarly, some reports that infliximab is effective in treating CP [7], while others report that it is ineffective [8]. In Japan, HP eradication has reportedly been successful in treating many cases of CP [2, 4]. In our case, various treatments such as MNZ, 5-ASA, steroids, and HP eradication therapy were not effective. Most of the previously reported cases of successful treatment of CP via HP eradication have involved patients with confirmed HP infection, and the relationship between HP infection and CP is drawing attention [2, 4]. However, there are reports of CP in patients who are HP-negative, as in our case [9]. The present patient underwent upper gastrointestinal endoscopy during his first visit to the local hospital and was HP-negative on rapid urease testing performed at that time. Even after CP was suspected, the fecal HP antigen and serum HP antibody titers were negative. Our patient did not have HP infection, which is probably why HP eradication treatment was ineffective. As our patient was resistant to medical treatment and had diarrhea, bloody stools, and abdominal pain, he was finally treated surgically.
The general indication for surgery for CP is resistance to medical treatment, and symptoms such as diarrhea and abdominal pain improve quickly after surgery. However, previous reports have shown that recurrence is not uncommon in patients who have undergone surgery, and the surgical procedure performed varies depending on the extent of the lesions [2, 2]. Gallegos et al. performed right hemicolectomy to treat recurrence in the right colon after left hemicolectomy [3]. In the present case, CP was found from the anal canal to the middle of the transverse colon, and anastomosis between the transverse colon and the anus was difficult because of the large distance. Therefore, we performed IPAA.
Our patient’s symptoms improved rapidly after resection. No recurrence of CP was observed in the ileal pouch, the stoma was closed about 3 months later, and no recurrence has been observed in 1 year of follow-up. After total proctocolectomy, the number of stools may increase and soiling may occur due to changes in the stool properties, which may reduce quality of life. However, the anal function is often maintained after IPAA for ulcerative colitis [10, 11], and it is likely that the outcome will be the same after IPAA for different diseases. In the present case, the number of stools after surgery was about four per day and there was no soiling; the patient was satisfied with the outcome. There are reports that soiling after IPAA is more likely in patients older than 55 years [12, 12]. As our patient was in his 40 s, the preoperative anal sphincter function was maintained, which may have led to the good outcome after IPAA.
Conclusion
We consider that laparoscopic-assisted total proctocolectomy and J-type IPAA with ileostomy may be a good option for CP, with little risk of recurrence.
Availability of data and materials
Not applicable.
Abbreviations
- CP:
-
Cap polyposis
- HP:
-
Helicobacter pylori
- TCS:
-
Total colonoscopy
- MNZ:
-
Metronidazole
- 5-ASA:
-
5-Aminosalicylic acid
- IPAA:
-
Ileal pouch anal anastomosis
References
Williams GT, Bussey HJR, Morson BC. Inflammatory cap polyps of the large intestine. Br J Surg. 1985;72:s133.
Akamatsu T, Nakamura N, Kawamura Y, Shinji A, Tateiwa N, Ochi Y, et al. Possible relationship between helicobacter pylori infection and cap polyposis of the colon. Helicobacter. 2004;9:651–6.
Gallegos M, Lau C, Bradly DP, Blanco L, Keshavarzian A, Jakate SM. Cap polyposis with protein-losing enteropathy. Gastroenterol Hepatol. 2011;7(6):415–20.
Oiya H, Okawa K, Aoki T, Nebiki H, Inoue T. Cap polyposis cured by helicobacter pylori eradication therapy. J Gastroenterol. 2002;37:463–6.
Suzuki H, Sato M, Akutsu D, Sugiyama H, Sato T, Mizokami Y. A case of cap polyposis remission by betamethasone enema after antibiotic therapy including Helicobacter pylori eradication. J Gastrointestin Liver Dis. 2014;23:203–6.
Kajiwara H, Uno Y, Ying H, Tanaka M, Munakata A. Features of cap polyposis by magnifying colonoscopy. Gastrointest Endosc. 2000;52:775–8.
Bookman ID, Redston MS, Greenberg GR. Successful treatment of cap polyposis with infliximab. Gastroenterology. 2004;126:1868–71.
Maunoury V, Breisse M, Desreumaux P, Gambiez L, Colombel JF. Infliximab failure in cap polyposis. Gut. 2005;54:313–4.
Tamura K, Matsuda K, Yokoyama S, Iwamoto H, Mizumoto Y, Nakamura Y, et al. Successful laparoscopic resection for cap polyposis: case report, literature review. Surg Case Rep. 2018;4:69.
Lightner AL, Mathis KL, Dozois EJ, Hahnsloser D, Loftus EV Jr, Raffals LE, et al. Results at up to 30 years after ileal pouch-anal anastomosis for chronic ulcerative colitis. Inflamm Bowel Dis. 2017;23(5):781–90.
Hahnloser D, Pemberton JH, Wolff BG, Larson DR, Crownhart BS, Dozois RR. The effect of ageing on function and quality of life in ileal pouch patients: a single cohort experience of 409 patients with chronic ulcerative colitis. Ann Surg. 2004;240(4):615–21.
Delaney CP, Fazio VW, Remzi FH, Hammel J, Church JM, Hull TL, et al. Prospective, agerelated analysis of surgical results, functional outcome, and quality of life after ileal pouchanal anastomosis. Ann Surg. 2003;238(2):221–8.
Weinryb RM, Liljeqvist L, Poppen B, Gustavsson JP. A longitudinal study of long-term quality of life after ileal pouch-anal anastomosis. Am J Surg. 2003;185(4):333–8.
Acknowledgements
We thank Kelly Zammit, BVSc, from Edanz Group (https://en-author-services.edanz.com/) for editing a draft of this manuscript.
Funding
We declare that each author received no funding for this study.
Author information
Authors and Affiliations
Contributions
TM and MU drafted the manuscript. KK, RK and YH managed the perioperative course. TK and SH collected the data. HI supervised the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Informed consent was obtained from the patient for publication of this report.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Minagawa, T., Ikeuchi, H., Kusunoki, K. et al. Cap polyposis treated with laparoscopic-assisted total proctocolectomy and ileal J-pouch anal anastomosis: a case report. surg case rep 7, 153 (2021). https://doi.org/10.1186/s40792-021-01214-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-021-01214-7