Abstract
Background
Neuromuscular and vascular hamartoma is a rare lesion of the small intestine, with only 26 cases reported since its initial description in 1982. No occurrence of hamartoma in the appendix has been reported until now.
Case presentation
A 60-year-old man had been suffering from longstanding right lower quadrant pain. Abdominal computed tomography showed a slight swelling of the appendix as the possible cause of his pain. Laparoscopic appendectomy with partial resection of the cecum was performed for diagnostic and therapeutic purposes. An 18 × 10-mm lesion located on the tip of the appendix was found in the resected specimen. Pathological examination showed that the lesion was covered with normal mucosa and consisted of adipose tissue, smooth muscle fibers, small vessels, and neural fibers. These findings were consistent with neuromuscular and vascular hamartoma of the appendix.
Conclusion
This is the first report of neuromuscular and vascular hamartoma arising from the appendix.
Similar content being viewed by others
Background
Neuromuscular and vascular hamartoma (NMVH) is a rare lesion of the small intestine, often clinically presenting as non-specific abdominal pain, recurrence of obstructive symptoms, and gastrointestinal bleeding. First described by Fernando and McGovern in 1982, this lesion consists of an aberrant proliferation of neural, muscular, and vascular elements in the small intestine [1]. Only 26 cases have been reported since its initial description, and NMVH occurred in the small intestine in all cases except one, in which it was found in the cecum [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20]. To our knowledge, NMVH occurring in the appendix has not been reported in the English literature until now. We report the first case of NMVH of the appendix.
Case presentation
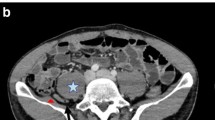
A 60-year-old man complaining of longstanding right lower quadrant pain for 4 years was referred to our hospital for further investigation and intervention. Abdominal examination revealed spontaneous pain in the lower right abdomen without rebound tenderness or palpation of a tumor. Blood examination showed no abnormal values including tumor markers. Abdominal computed tomography (CT) identified a slight swelling of the appendix (about 10 mm) without obvious neoplastic tumors or lymphadenopathy (Fig. 1). Colonoscopy showed elevation of the mucosa around the appendiceal orifice (Fig. 2). We considered the swollen appendix to be the cause of his pain and performed a laparoscopic appendectomy with partial resection of the cecum for diagnostic and therapeutic purposes. Intraoperative findings were a slight swelling of the appendix but no tumor exposure on the serosal surface of the appendix and cecum (Fig. 3). The surgical specimen contained a submucosal lesion located on the tip of the appendix that measured 18 × 10 mm (Fig. 4). Microscopically, this lesion was covered with normal mucosa, arose from submucosa, and contained abundant adipose tissue (Fig. 5). Smooth muscle fiber bundles, small vessels, and neural fiber bundles were collected and scattered irregularly in the submucosa, and there was no evidence of malignancy (Fig. 6). Each component of this lesion was confirmed by immunohistochemical examination. Vascular endothelium, neural fibers, and smooth muscle fibers were immunostained with CD34 (Fig. 7a), S-100 (Fig. 7b), and desmin (Fig. 7c)/smooth muscle actin (Fig. 7d) antibodies, respectively. These pathological findings were consistent with previous reports, and this lesion was diagnosed as NMVH. The patient’s right lower abdominal pain disappeared immediately after surgery, and was thought to be caused by the NMVH.
Immunohistochemical staining. Immunohistochemical staining revealed vascular endothelium (a: CD34), neural fibers (b: S-100), and smooth muscle fibers including perivascular fibers (arrows) (c: Desmin, d: smooth muscle actin), respectively. Immunoperoxidase staining. Original magnification, a: × 200; b, c, d: × 100
Discussion
To date, 27 cases of NMVH have been reported, including the present case (Table 1). The mean patient age is 53.7 (12–91) years, and there are 10 males and 15 females, with age unknown in 4 cases and sex unknown in 2 cases. Most of the patients complained of abdominal pain, and 3 patients had Crohn’s disease as a comorbidity. NMVH originated in the small intestine in all cases except one in which it originated in the cecum [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20]. Therefore, this report appears to be the first case of NMVH occurring in the appendix.
The only findings in this case were longstanding right lower quadrant pain and a slight swelling of the appendix on CT imaging. As a cause of the swollen appendix without inflammation, the latency of cancer and carcinoid tumors was considered. However, we presumed that the preoperative diagnosis was less likely to be a progressive disease such as cancer because no worsening of abdominal pain or tumor formation had been observed for the 4 years since onset. For these reasons, we performed a laparoscopic appendectomy for diagnostic and therapeutic purposes. The patient’s right lower abdominal pain disappeared immediately after surgery, indicating that it was likely caused by the NMVH. Although a detailed mechanism for the abdominal pain was unclear, a rise in the internal pressure of the appendix was considered as one possible cause.
NMVH has been thought to be a hamartoma that consists of an aberrant proliferation of neural, muscular, and vascular elements in the intestine [1]. However, Shepherd and Jass suggested that NMVH may represent an abnormal histologic consequence of chronic inflammatory bowel disease, especially Crohn’s disease [3]. Other authors reported that NMVH might not be a rare entity but rather a process of chronic inflammation [22, 23]. However, considering that most of the patients in the previous reports did not exhibit prominent fibrosis of the intestinal wall when observed in the chronic inflammatory state, it is thought that NMVH may exist as a separate entity [18]. For such reasons, the debate continues as to whether this lesion is truly a hamartoma or represents a “burnt-out” phase of various chronic pathologies.
The case presented here showed no histological features such prominent fibrosis that would indicate active or “burnt out” Crohn’s disease or another reactive process induced by chronic inflammation. Therefore, we consider this NMVH of the appendix to be an entity separate from any special state of chronic inflammation.
Conclusion
We experienced a case of NMVH occurring in the appendix. Although NMVH is a benign disease, it should be included in the differential diagnosis of neoplastic lesions not only in the small intestine but also in the appendix.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- CT:
-
Computed tomography
- NMVH:
-
Neuromuscular and vascular hamartoma
References
Fernando SS, McGovern VJ. Neuromuscular and vascular hamartoma of small bowel. Gut. 1982;23:1008–12.
Smith CE, Filipe MI, Owen WJ. Neuromuscular and vascular hamartoma of small bowel presenting as inflammatory bowel disease. Gut. 1986;27:964–9.
Shepherd NA, Jass JR. Neuromuscular and vascular hamartoma of the small intestine: is it Crohn’s disease? Gut. 1987;28:1663–8.
Kwasnik EM, Tahan SR, Lowell JA, Weinstein B. Neuromuscular and vascular hamartoma of the small bowel. Dig Dis Sci. 1989;34:108–10.
Salas A, Casellas F, Sanz J, Garcia F, Margarit C, Malagelada JR. Neuromesenchymal hamartoma of the small bowel. J Clin Gastroenterol. 1990;12:705–9.
Cortina G, Wren S, Armstrong B, Lewin K, Fajardo L. Clinical and pathologic overlap in nonsteroidal anti-inflammatory drug-related small bowel diaphragm disease and the neuromuscular and vascular hamartoma of the small bowel. Am J Surg Pathol. 1999;23:1414–7.
de Sanctis S, Qureshi T, Stebbing JF. Clinical and pathologic overlap in nonsteroidal anti-inflammatory drug-related small bowel diaphragm disease and the neuromuscular and vascular hamartoma of the small bowel. Am J Surg Pathol. 2001;25:539–41.
Scintu F, Capra F, Giordano M, Frau G, Mascia R, Comella D, et al. [Neuromuscular and vascular hamartoma of the small intestine. Report of a clinical case and review of the literature]. In Italian. Chir Ital. 2001;53:393–8.
Shiomi T, Kameyama K, Kawano Y, Shimizu Y, Takabayashi T, Okada Y. Neuromuscular and vascular hamartoma of the cecum. Virchows Arch. 2002;440:338–40.
Company MM, Usamentiaga E, Torralba J, Bonet L. [Small bowel diaphragm disease associated with NSAIDs with histology of neuromuscular and vascular hamartoma. Case report and literature review]. In Spanish. Gastroenterol Hepatol. 2005;28:228–31.
Theodosiou E, Voulalas G, Salveridis N, Pouggouras K, Manafis K, Christodoulidis K. Neuromesenchymal hamartoma of small bowel--an extremely rare entity: a case report. World J Surg Oncol. 2009;7:92.
Krishnamurthy V, Basavaraj V, Sunila, Vimalambike MG. Neuromuscular and vascular hamartoma of the small bowel: a rare cause of intestinal obstruction. J Lab Phys. 2010;2:109–10.
Kaplan JL, Goldstein AM, Shenoy-Bhangle A, Badizadegan K. Neuromuscular and vascular hamartoma of the small intestine in a child. J Pediatr Gastroenterol Nutr. 2013;56:e33–5.
Ren B, Cao W. Neuromuscular and vascular hamartoma: is it a true hamartoma? J Clin Pathol. 2014;67:284–7.
Setaffy L, Osuna MJ, Plieschnegger W, del Pino Florez Rial M, Geboes K, Langner C. Cryptogenic multifocal ulcerous stenosing enteritis (CMUSE), and neuromuscular and vascular hamartoma (NMVH): two sides of the same coin? Endoscopy. 2015;47:345–8.
Crothers JW, Zenali M. Neuromuscular and vascular hamartoma of the small intestine: an exuberant reparative process secondary to chronic inflammation. Int J Surg Pathol. 2015;23:673–6.
Liu N, Pan Y, Li ZS, Shi YP, Zhang XY, Wu GS, et al. Neuromuscular and vascular hamartoma: a rate entity or special phase of Crohn’s disease. J Dig Dis. 2015;16:52–4.
Elstner KE, Vickers CR, Gett RM, Qiu MR, Killen LV. Neuromuscular and vascular hamartoma as an unusual cause of small bowel obstruction. Int J Surg Case Rep. 2016;26:1–3.
Caruso ML, Cavalcanti E, De Michele F, Ignazzi A, Carullo R, Mastronardi M. Small bowel capsule endoscopy revealing neuromuscular and vascular hamartoma of the jejunum: a case report. Medicine (Baltimore). 2018;97:e0196.
Pattnaik SA, Mitra S, Mishra TS, Purkait S, Kumar P, Naik S. A vasculitis-associated neuromuscular and vascular hamartoma presenting as a fatal form of abdominal cocoon. Int J Surg Pathol. 2019;27:108–15.
Acknowledgements
Authors thank Prof. Tina Tajima of St. Marianna University School of Medicine for her meticulous English editing of the paper.
Funding
This study was not funded.
Author information
Authors and Affiliations
Contributions
Takahiro Sasaki described and designed the report. Tomohisa Furuhata edited the manuscript. Takehito Otsubo supervised the overall writing of the manuscript. Masashige Nishimura, Tatsunori Ono, Akiyoshi Noda, Hirotaka Koizumi, and Nobuyoshi Miyajima collected the data and discussed the contents of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Competing interests
The authors declare no potential conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sasaki, T., Furuhata, T., Nishimura, M. et al. An extremely rare case of neuromuscular and vascular hamartoma of the appendix. surg case rep 6, 216 (2020). https://doi.org/10.1186/s40792-020-00970-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-020-00970-2