Abstract
Background
Pancreatic cancer with distant metastases is classified as “unresectable,” for which the standard treatment is systemic chemotherapy. The effectiveness of radical resection for pancreatic cancer with distant metastases is unknown. Here, we report a case of long term survival treated with conversion surgery following chemotherapy after diagnostic metastasectomy for pancreatic cancer with synchronous liver metastasis.
Case presentation
A 73-year-old man was referred to our hospital to examine and treat for cancer of the pancreatic body. Computed tomography (CT) scan revealed a 26-mm hypovascular tumor in contact with the common hepatic artery (CHA) (> 180°), the celiac artery (< 180°), and portal vein at the pancreatic body. Resectability was determined as “borderline resectable.” Two courses of gemcitabine plus S-1 combination therapy (GS) were administered as neoadjuvant chemotherapy (NAC). CT scan showed tumor shrinkage (21 mm), determined as stable disease (SD) according to Response Evaluation Criteria in Solid Tumors (RECIST). Although the abdomen was opened for radical resection, a small nodule on the liver was detected and removed. Since the nodule was diagnosed as adenocarcinoma by intraoperative frozen section, resection of the primary tumor was not performed. After three subsequent courses of GS therapy, no distant metastases were detected under radiological findings. Distal pancreatectomy with celiac artery resection (DP-CAR) was performed as radical surgery 6 months after the initial diagnosis. Histological diagnosis was well-differentiated tubular adenocarcinoma, showing ypT1 ypN1 M1 stage IV, negative surgical margin (R0), and grade III in the Evans classification. S-1 was administered every other day from 6 months after resection up to the present. The patient has been alive with no recurrence for 5 years after the initial diagnosis and 4.5 years after the resection.
Conclusion
There is a case that received survival benefits from conversion surgery following chemotherapy after diagnostic metastasectomy in pancreatic cancer with synchronous liver metastasis.
Similar content being viewed by others
Background
Pancreatic cancer with distant metastases (M1) is classified as “unresectable,” for which the standard treatment is systemic chemotherapy. Although pancreatic resection and metastasectomy for M1 pancreatic cancer are suggested to be safe [1, 2], the prognostic contribution of radical surgery for M1 pancreatic cancer is unclear. Recently, reports on the effectiveness of conversion surgery after chemotherapy or chemoradiotherapy for initially unresectable locally advanced or M1 pancreatic cancer have been increasing due to the development of anticancer drugs [3, 4]. On the other hand, there are few reports of multidisciplinary treatment using a combination of radical resection and pre/post-operative chemotherapy for synchronous M1 pancreatic cancer. Here, we report a long-term survival case treated with a combination of conversion surgery following chemotherapy after diagnostic metastasectomy for pancreatic cancer with synchronous liver metastasis, showing 4.5-year recurrence-free survival and 5-year survival after initial diagnosis.
Case presentation
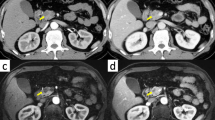
A 73-year-old man visited a previous hospital due to upper abdominal pain. The patient had a past history of diabetes mellitus, hypertension, hyperlipidemia, and vestibular schwannoma. Abdominal computed tomography (CT) scan revealed wall thickening of the swollen gallbladder and a 26-mm hypovascular tumor in contact with the common hepatic artery (CHA) (> 180°), the celiac artery (< 180°), and portal vein at the pancreatic body (Fig. 1). The patient was diagnosed as pancreatic body cancer, and acute cholecystitis had also occurred. Laparoscopic cholecystectomy was performed for the acute cholecystitis, and simultaneous washing cytology was negative. After that, the patient was referred to our hospital for further examination and treatment of the pancreatic cancer. All of the examined tumor markers were within the normal range (CEA 1.7 ng/ml, CA19-9 2.0 ng/ml, DUPAN-2 60 U/ml, SPan-1 1.0 U/ml, CA-125 12.4 U/ml). Since serum CA19-9 was at an undetectable level, Lewis antigen of the patient might be negative. No liver metastasis was found by gadoxetic acid-enhanced magnetic resonance imaging (EOB-MRI). According to the National Comprehensive Cancer Network (NCCN) Guidelines Version 2.2016, the resectability was determined to be “borderline resectable.” Distal pancreatectomy with celiac artery resection (DP-CAR) after neoadjuvant chemotherapy (NAC) was planned. Two courses of gemcitabine (GEM) plus S-1 combination therapy (GS) were performed as NAC [5]. GEM was given at a dose of 1000 mg/m2 on days 1 and 8 of a 21-day cycle, and S-1 was administered at a dose of 40 mg/m2 twice daily on days 1–14 followed by a 7-day rest. Enhanced CT scan after NAC showed a 21-mm pancreatic tumor, indicating stable disease (SD) in the Response Evaluation Criteria in Solid Tumors (RECIST) (Fig. 2). EOB-MRI and fluorine-18 fluorodeoxyglucose (FDG) positron emission tomography (PET) after NAC revealed no distant metastases. Coil embolization of the CHA and left gastric artery was done 3 days before surgery in order to prevent ischemic changes of the liver and stomach. Laparotomy was performed for DP-CAR 3 months after the initial diagnosis. A 3-mm tumor was detected on the surface of the liver (segment IV) and was removed. The liver tumor was diagnosed as adenocarcinoma by intraoperative frozen sections (Fig. 3). Therefore, resection of the primary tumor was not performed. Three subsequent courses of GS were administered. Afterward, no distant metastases were seen in CT scan, MRI, or FDG-PET (Fig. 4). The RECIST was unevaluable due to the artifact of the coil. DP-CAR was performed 6 months after the initial diagnosis. Intraoperative findings showed negative washing cytology and no distant metastases. The operative time was 429 min, and the amount of bleeding was 1150 ml. The proliferation of atypical cells with low papillary structure and disruption of the cell polarity was observed histologically in the main pancreatic duct. The tumor cells had nuclear enlargement and nuclei of irregular shape in the invasive portion, showing degeneration by chemotherapy. The histological diagnosis was well-differentiated tubular adenocarcinoma (Fig. 5). TNM classification of the Union for International Cancer Control (UICC) (7th edition) was ypT1 ypN1 M1, Stage IV. No carcinoma cells were detected in the surgical margin (R0). Because of the widespread fibrous tissue and some residual tumor cells, the histopathological effect of chemotherapy was determined as grade III in the Evans classification [6]. Although grade C of delayed gastric emptying (DGE), defined by the International Study Group of Pancreatic Surgery (ISGPS), developed after the surgery, the patient was discharged after 91 postoperative days. S-1 was administered every other day at a dose of 100 mg/day from 6 months after the resection up to the present. The patient has been alive with no recurrence for 5 years from an initial diagnosis and 4.5 years after DP-CAR.
Abdominal CT scan at the initial diagnosis at the previous hospital. The white arrows indicate the pancreatic tumor. a A 26-mm hypovascular tumor in contact with the common hepatic artery (CHA) (> 180°) was seen in the pancreatic body. b The main tumor contacted the PV and bifurcation of Ce. CHA common hepatic artery, Ce celiac artery, SA splenic artery, PV portal vein
Abdominal CT scan after two courses of GS. The white arrows indicate the pancreatic tumor. a The size of the main tumor was reduced from 26 mm to 21 mm. The abnormal shadow of the soft tissue around CHA did not increase. b The abnormal shadow around the bifurcation of Ce did not change. CHA common hepatic artery, Ce celiac artery, SA splenic artery
Representative histological photographs of resected specimen (hematoxylin and eosin staining). a The viable adenocarcinoma cells invaded into pancreatic tissue with the formation of various ductal structures (×50, bar; 500 μm). b The tumor cells extended to the main pancreatic ducts (×100, bar; 250 μm). c The tissue around the CHA was replaced with fibrous tissue (×50, bar; 500 μm). d The fibrous tissue included many histiocytes containing hemosiderin (arrowhead) (×400, bar; 50 μm)
Discussion
Pancreatic cancer is one of the most lethal malignancies. Gillen et al., based on an analysis of 111 studies from 1966 to 2009, reported that the proportions of resectable pancreatic cancer, locally advanced/unresectable pancreatic cancer, and metastatic pancreatic cancer at the initial diagnosis were approximately 10–20, 30–40, and 50–60%, with a median survival time (MST) for metastatic pancreatic cancer of only 5–9 months [7]. Recently, two powerful regimens, oxaliplatin, leucovorin, irinotecan, plus 5-fluorouracil (FOLFIRINOX) and GEM plus nab-paclitaxel (G+nab-P), are being used as the standard treatment for metastatic pancreatic cancer. MST has been reported to be 10.7–11.1 months with FOLFIRINOX [8, 9] and 8.5–13.5 months with G+nab-P [10, 11]. Although the development of chemotherapy has improved the prognosis of pancreatic cancer, long-term survival cases treated with chemotherapy alone are still rare. There are several reports about the effectiveness of resection for liver metastases in pancreatic cancer. It has been reported that liver resection for synchronous liver metastasis in pancreatic cancer did not contribute to improving the prognosis [12, 13]. On the other hand, Tachezy et al. has reported that synchronous resection of the primary tumor and liver metastases in pancreatic cancer prolonged survival compared with non-resection [14]. Although this study had a patient selection bias of a surgical indication for liver metastases, cases that received a survival benefit from surgical resection for primary tumor and liver metastasis exist, as in our case. Hackert et al. reported that pancreatic resection and metastasectomy for oligometastatic pancreatic cancers contributed to a prolonged survival of 10% in selected patients [1]. In this study, 4.7% of patients with liver metastasis underwent prior liver resection, followed by chemotherapy and pancreatic resection. Also, Buc et al. has described that a case of pancreatic cancer with a synchronous single liver metastasis has undergone conversion surgery following chemotherapy after diagnostic metastasectomy as in our case and has been alive without recurrence over 2 years from initial diagnosis [15]. Pancreatic cancer with small superficial liver oligometastases which are diagnosed at the time of surgery without detection by pre-operative imaging might be a good candidate for this strategy, namely conversion surgery after diagnostic metastasectomy.
There are few reports of conversion surgery with simultaneous metastasectomy after chemotherapy for pancreatic cancer with synchronous liver metastases. As far as we could determine, there were only two cases that underwent conversion surgery after FOLFIRINOX, reported by Schneitler et al. [16]. One has been alive for 24 months after the diagnosis and 18 months after the resection. The other has been alive for 17 months since the diagnosis and 9 months after resection with no recurrence. In these cases, conversion surgery with simultaneous metastasectomy might have contributed to the prolongation of survival. Further observation is needed to evaluate the long-term prognosis.
FOLFIRINOX or G+nab-P improves the prognosis of metastatic pancreatic cancer. Currently, the standard regimen for metastatic pancreatic cancer is FOLFIRINOX or G+nab-P. GS therapy showed a better response rate for patients with locally advanced or metastatic pancreatic cancer than GEM or S-1 monotherapy in the GEST study [17]. GS as neoadjuvant for resectable and borderline resectable pancreatic cancer could contribute to R0 resection and overall survival [5]. Currently, a phase III randomized controlled trial of neoadjuvant GS for resectable pancreatic cancer (Prep-02/JSAP-05; UMIN000009634) is ongoing.
FOLFIRINOX or G+nab-P is expected to increase the number of patients with metastatic pancreatic cancer well-controlled for a certain period and patients undergoing conversion surgery as in our case. The median progression-free survival (PFS) of FOLFILINOX and G+nab-P has been reported to be 5.6–6.4 months [5, 6] and 5.5–6.5 months [7, 8], respectively. It might be better to consider the PFS in the timing of conversion surgery.
Conclusions
The present case received survival benefits from conversion surgery following chemotherapy after diagnostic metastasectomy for pancreatic cancer with synchronous liver metastasis.
Abbreviations
- CHA:
-
Common hepatic artery
- CT:
-
Computed tomography
- DGE:
-
Delayed gastric emptying
- DP-CAR:
-
Distal pancreatectomy with celiac artery resection
- EOB-MRI:
-
Gadoxetic acid-enhanced magnetic resonance imaging
- FDG:
-
Fluorine-18 fluorodeoxyglucose
- FOLFIRINOX:
-
Oxaliplatin, leucovorin, irinotecan, plus 5-fluorouracil
- G+nab-P:
-
Gemcitabine plus nab-paclitaxel
- GEM:
-
Gemcitabine
- GS:
-
Gemcitabine plus S-1 combination therapy
- ISGPS:
-
International Study Group of Pancreatic Surgery
- MST:
-
Median survival time
- NAC:
-
Neoadjuvant chemotherapy
- NCCN:
-
National Comprehensive Cancer Network
- PET:
-
Positron emission tomography
- PFS:
-
Progression-free survival
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- UICC:
-
Union for International Cancer Control
References
Hackert T, Niesen W, Hinz U, Tjaden C, Strobel O, Ulrich A, et al. Radical surgery of oligometastatic pancreatic cancer. Eur J Surg Oncol. 2017;43:358–63.
Seelig SK, Burkert B, Chromik AM, Tannapfel A, Uhl W, Seelig MH. Pancreatic resections for advanced M1-pancreatic carcinoma: the value of synchronous metastasectomy. HPB Surg. 2010;2010:579672.
Satoi S, Yamaue H, Kato K, Takahashi S, Hirono S, Takeda S, et al. Role of adjuvant surgery for patients with initially unresectable pancreatic cancer with a long-term favorable response to non-surgical anti-cancer treatments: results of a project study for pancreatic surgery by the Japanese Society of Hepato-Biliary-Pancreatic Surgery. J Hepatobiliary Pancreat Sci. 2013;20:590–600.
Hackert T, Sachsenmaier M, Hinz U, Schneider L, Michalski CW, Springfeld C, et al. Locally advanced pancreatic cancer: neoadjuvant therapy with folfirinox results in resectability in 60% of the patients. Ann Surg. 2016;264:457–63.
Motoi F, Ishida K, Fujishima F, Ottomo S, Oikawa M, Okada T, et al. Neoadjuvant chemotherapy with gemcitabine and S-1 for resectable and borderline pancreatic ductal adenocarcinoma: results from a prospective multi-institutional phase 2 trial. Ann Surg Oncol. 2013;20:3794–801.
Evans DB, Rich TA, Byrd DR, Cleary KR, Connelly JH, Levin B, et al. Preoperative chemoradiation and pancreaticoduodenectomy for adenocarcinoma of the pancreas. Arch Surg. 1992;127:1335–9.
Gillen S, Schuster T, Meyer Zum Buschenfelde C, Friess H, Kleeff J. Preoperative/neoadjuvant therapy in pancreatic cancer: a systematic review and meta-analysis of response and resection percentages. PLoS Med. 2010;7:e1000267.
Conroy T, Desseigne F, Ychou M, Bouche O, Guimbaud R, Becouarn Y, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364:1817–25.
Okusaka T, Ikeda M, Fukutomi A, Ioka T, Furuse J, Ohkawa S, et al. Phase II study of FOLFIRINOX for chemotherapy-naive Japanese patients with metastatic pancreatic cancer. Cancer Sci. 2014;105:1321–6.
Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369:1691–703.
Ueno H, Ikeda M, Ueno M, Mizuno N, Ioka T, Omuro Y, et al. Phase I/II study of nab-paclitaxel plus gemcitabine for chemotherapy-naive Japanese patients with metastatic pancreatic cancer. Cancer Chemother Pharmacol. 2016;77:595–603.
Klein F, Puhl G, Guckelberger O, Pelzer U, Pullankavumkal JR, Guel S, et al. The impact of simultaneous liver resection for occult liver metastases of pancreatic adenocarcinoma. Gastroenterol Res Pract. 2012;2012:939350.
Singh A, Singh T, Chaudhary A. Synchronous resection of solitary liver metastases with pancreaticoduodenectomy. JOP. 2010;11:434–8.
Tachezy M, Gebauer F, Janot M, Uhl W, Zerbi A, Montorsi M, et al. Synchronous resections of hepatic oligometastatic pancreatic cancer: disputing a principle in a time of safe pancreatic operations in a retrospective multicenter analysis. Surgery. 2016;160:136–44.
Buc E, Orry D, Antomarchi O, Gagniere J, Da Ines D, Pezet D. Resection of pancreatic ductal adenocarcinoma with synchronous distant metastasis: is it worthwhile? World J Surg Oncol. 2014;12:347.
Schneitler S, Kropil P, Riemer J, Antoch G, Knoefel WT, Haussinger D, et al. Metastasized pancreatic carcinoma with neoadjuvant FOLFIRINOX therapy and R0 resection. World J Gastroenterol. 2015;21:6384–90.
Ueno H, Ioka T, Ikeda M, Ohkawa S, Yanagimoto H, Boku N, et al. Randomized phase III study of gemcitabine plus S-1, S-1 alone, or gemcitabine alone in patients with locally advanced and metastatic pancreatic cancer in Japan and Taiwan: GEST study. J Clin Oncol. 2013;31:1640–8.
Acknowledgements
We thank Dr. Takahiro Kamiga for treating the patient at Sendai Tokushukai Hospital before referral to our hospital.
Funding
Michiaki Unno received funding from the Management Expenses Grants from the Government of Japan to national university corporations supplied every fiscal year.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article.
Author information
Authors and Affiliations
Contributions
MS and MM wrote the paper. AM and TT contributed to the creation of figures. HH, TH, MI, TT, KA, SM, HO, NS, TM, KN, TN, TK, FM, and MU reviewed the manuscript and revised it critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We obtained written informed consent from the patient.
Consent for publication
We obtained written informed consent for publication from the patients.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Shimura, M., Mizuma, M., Hayashi, H. et al. A long-term survival case treated with conversion surgery following chemotherapy after diagnostic metastasectomy for pancreatic cancer with synchronous liver metastasis. surg case rep 3, 132 (2017). https://doi.org/10.1186/s40792-017-0409-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-017-0409-9