Abstract
Background
Coronavirus disease 2019 outbreak is the first reported case in Wuhan, China in December 2019 and suddenly became a major global health concern. According to the European Centre for Disease Prevention and Control, on August 4, 2020 the reported cases of coronavirus disease 2019 were 18,456,952 cases worldwide, 11,691,229 recovered with 697,719 deaths. Evidence on Burden, admission and outcome of Coronavirus Disease in 2019 among Asthmatic patients has not been published in Africa. This research protocol will, therefore, be driven to conduct systematic review and meta-analysis of the Coronavirus Disease in 2019 burden, admission and outcome among Asthmatic patients in Africa.
Methods
All observational studies among Asthmatic patients in Africa and written without language limitation will be included. A search technique was applied using Databases (PubMed / MEDLINE, EMBASE, HINARI, Cochrane Library, World Health Organization COVID-19 database, Africa Wide Knowledge and Web of Science). Two independent authors carried out data extraction and assess the risk of bias using a predetermined and structured method of data collection. We will use random-effects to estimate the overall pooled burden, admission and outcome of COVID-19 Asthmatic patients in Africa. To assess possible publication bias, funnel plot test and Egger’s test methods will be used. This systematic and meta-analysis review protocol will be reported based on the Preferred Reporting Items for Systematic reviews and Meta-Analysis protocol guidelines.
Discussion
The description will be used to show the COVID-19 distribution data by interest variables such as residence, setting, and person-level characteristics. The findings of this review will notify health care professionals about the burden, admission and outcome of COVID − 19 in asthmatic patient, while providing evidence to bring about the requisite improvements in clinical practice for asthmatic patients.
Systematic review registration
This review is registered in the PROSPERO International Prospective Register of Systematic reviews with the registration number of CRD42020202049.
Similar content being viewed by others
Background
In December 2019, a new virus (initially called ‘Novel Coronavirus 2019-nCoV’ and later renamed to SARS-CoV-2) causing severe acute respiratory syndrome (coronavirus disease COVID-19) emerged in Wuhan, Hubei Province, China, and rapidly spread to other parts of China and other countries around the world and it suddenly became a major global health concern [1]. The World Health Organization (WHO) has called the outbreak of coronavirus disease 2019 (COVID-19) a global emergency [2].
COVID-19’s clinical symptoms vary from asymptomatic illness to flu-like disease, including high morbidity and mortality from multi-organ failures. The majority of patients diagnosed with COVID-19 have developed mild symptoms including sore throat, dry cough, and fever. The majority of them have resolved spontaneously. Some have developed multiple fatal complications, such as: septic shock, extreme pneumonia, and organ failure [3].
According to the European Centre for Disease Prevention and Control, on August 4, 2020, the reported cases of coronavirus disease 2019 were 18,456,952 cases worldwide, 11,691,229 recovered with 697,719 deaths. The United States has the largest number of confirmed cases 4,862,285 cases, 2,447,525 recovered with 158,931 deaths in the world and followed by Brazil has 2,751,665cases, 1,912,319 recovered and with 94,702 deaths. In Africa, the total number of confirmed were 972,374 cases, 633,289recovered and 20,682 deaths. South Africa has the largest number of reported 511,485 cases with 8366 total deaths cases in Africa [1, 4].
According to different Studies, clinical features of COVID-19 infection is varied based on the groups and showed greater risks for the development of pneumonia as a serious type of infection among the elderly people and with chronic comorbidities, especially systemic arterial hypertension, diabetes mellitus and immunosuppression. Additionally, official Chinese information showed that 8% of pregnant women with COVID-19 were serious cases and may also be especially susceptible to infection [5,6,7,8]. Patients with asthma have likely to develop severe COVID-19 and other complications than patients without Asthma [9].
There have been different reports about COVID-19 [10,11,12,13]. Forty-five percent (45%) patients with COVID − 19 receive non-invasive respiratory support via a non-rebreathing oxygen face mask [14]. Sputum cells among patients with asthma may give a risk for COVID-19 morbidity [15]. The prevalence of COVID-19 among asthmatic patient was 9% [16]. Yet, there is no pooled result of the COVID-19 burden, admission and outcome among asthmatic patients in Africa. This research protocol will, therefore, be driven to conduct systematic review and meta-analysis of the COVID-19 burden, admission and outcome among asthmatic patients in Africa.
Methods
Protocol registration
This review is registered in the PROSPERO International Prospective Registry of Systematic Reviews (CRD42020202049) and reported according to Preferred Reporting Items for Systematic reviews and Meta-Analysis protocol (PRISMA-P) guidelines [17] (Table 1).
Eligibility criteria
Types of study
All observational studies; including cross-sectional studies, cohort, case-control, and baseline results from randomized controlled trials carried out in Africa will be included.
Participants/population
All Asthmatic patients (all studies include all age groups) who are African residence and laboratory-confirmed and/or clinically diagnosed with having COVID-19.
Intervention(s), exposure(s)
Asthma with COVID-19 infection. Therefore, we want to assess disease burden, admission and outcome of COVID-19 on asthmatic patients will be reviewed.
Outcomes
Morbidity, admission, Mortality and other clinical outcomes of COVID-19 among asthmatic patients (Prevalence rate, infection rate Clinical characteristics include symptoms (such as symptoms of upper respiratory tract infection, myalgia, fever, cough, dyspnea/shortness of breath, electrolyte imbalance and organ failure). laboratory/imaging (chest X-ray, CT, C-Reactive protein and whole blood count), and outcomes of Asthma (recovery, complications and death) and COVID-19 outcomes.
Settings
Hospital-based studies.
Language
Without the restriction of language all published and unpublished papers will be included in this review.
Method of diagnosis
No limitation on diagnostic methods but subgroup review will be carried out based on diagnostic instruments. Interim guidance from the WHO and/or any diagnostic criteria proposed by the WHO shall be considered ‘WHO interim guidance for laboratory biosafety related to 2019-nCoV’ [18, 19] (Table 2).
Exclusion criteria
Studies that have not clarified the requirements for the COVID-19 outcome level; studies that have not been conducted in humans, qualitative studies, studies that lack valid data required to determine the outcome will not be included. Studies such as experimental studies, commentaries, editorials, letters, case reports, or case series will be excluded from this review.
Search strategy and data source
A search technique was applied using online Databases (PubMed / MEDLINE, EMBASE, HINARI, Cochrane Library, WHO COVID-19 database, Africa Wide Knowledge and Web of Science) from February to August 2020 (Table 3). The quest was performed either individually or in combination using the following keywords: Admission, Asthma, burden, COVID-19, outcome and prevalence. Search terms to be used: “Wuhan coronavirus” OR “COVID-19” OR “novel coronavirus” OR “2019-nCoV” OR “Coronavirus outbreak” OR “SARS-CoV-2” OR “SARS2” OR “Severe acute respiratory syndrome coronavirus 2” OR “Burden” OR “Outcome”. Other searching terms will be “mortality” OR “prevalence” OR “incidence” OR “Asthma complication of COVID-19”.
Selection and data collection process
Data were extracted using a standardized method of data extraction. Two assessors (AH and WA) will autonomously extract data using the predefined standardized extraction form from the included studies. For further consideration of whether to include in the study or not, full texts for the qualifying titles and/or abstracts, including those where there is ambiguity, will be collected. The agreement between the reviewers of the study will be calculated using Cohen’s λ statistics. Disagreements will be resolved by mediation, and arbitration by a third reviewer (GM) will occur when necessary. Reasons for excluding articles will be noted.
Where there is missing information, authors have been contacted for additional details to ensure study eligibility. Where necessary, up to three emails have been sent to the corresponding author to request additional information before excluding the study. We will consider the most recent, detailed, and with the highest sample size for studies that appear in more than one published article. We shall treat each survey as a separate study for surveys that appear in one article with multiple surveys conducted at different time points. Data extraction was including information: first author, publishing month, country and/or region, signs and symptoms, complications, diagnostic criteria, comorbidity, COVID-19, study area, prevalence and/or incidence, characteristics of the study (study design, response rate).
Quality assessment and risk of bias in individual studies
A tool developed by Hoy et al. for prevalence studies will be used to evaluate the likelihood of bias and quality of studies included in this review [20]. The tool contains 11 items; items 1–4 assess the external validity, 5–10 assess the internal validity, and item 11 offers a description of the overall risk by the reviewer based on the responses of the above 10 items which are rated 1 if yes and 0 if no. Studies are graded as low (< 3), moderate risk (4-6) or high (7-9) risk of bias. Two reviewers did this exercise, and disputes will be resolved through discussion and, where possible, through arbitration involving a third author. Besides, adequate sampling methods, consistent methods and procedures for collecting data, recorded methods of quality control and representative sample size will be considered as indicators of the study quality. Studies of high quality will be studies that revealed all the points mentioned above.
Data management
A framework was developed a priori to guide the screening and selection process, based on the inclusion and exclusion criteria. The tool will be piloted and revised before data extraction begins. First, to delete duplicates, the search results will be uploaded to EndNote software. The remaining articles will be put on Rayyan, a smartphone and a web-based software system that facilitates the collaboration between reviewers involved in the screening and selection of studies to be included in the review [21].
Data items
Data extraction was including: authors, month, country and/or region, sample size, type of publication, study area, characteristics of the study (study design, response rate).
Outcomes and prioritization
The primary outcome is the burden, admission and outcome of COVID − 19 among asthmatic patients in African.
Data analysis and presentation of results
R software and R studio will be used during analyzing the Data. All analyses will be carried out using a “metaprop” routine for Windows using R version 3.5.3 [22]. Results will be reported as proportions with corresponding 95% confidence intervals (CIs). Forest plots will be drawn to represent the combined outcome of COVID-19 and the extent of statistical heterogeneity among studies. The statistical heterogeneity will be evaluated using the χ2 test and quantified using the calculation of the I2 statistics with values of 25, 50 and 75% being representative of low, medium and high heterogeneity, respectively [23]. If there will be heterogeneity between studies, we will use a meta-analysis of random-effects [24] to estimate the aggregate pooled burden, admission and outcome of COVID-19 among asthmatic patients in Africa. To assess possible publication bias, funnel plot test and Egger’s test methods will be used [25]. P-value < 0.10 on the Egger’s test is considered statistically significant for bias in writing.
Data synthesis
The study-specific outcome of COVID-19 among asthmatic patients will be recalculated using Crude numerators and denominators from individual studies. A meta-analysis will be performed on variables that are similar across the included studies. Because there will be heterogeneity among the studies, the random effect model will be used to determine the pooled burden, admission and outcome of COVID-19 in Africa. African Geographic regions, diagnostic methods, and based on their ethnic background where the study was conducted will be summarized by a subgroup analysis.
Discussion
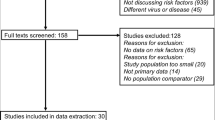
This review will be done based on the PRISMA-P guidelines and the PRISMA flow diagram and also used to document the different phases of the review process [17] (Fig. 1).
The findings of this review will notify to health program planners, decision-makers and health care professionals about the burden, admission and outcome of COVID − 19 among asthmatic patients, while providing evidence to bring good quality health care, the good emphasis for the problem, improvements in clinical practice. Conferences, peer-review articles, and social media sites will share conclusions from this study.
Conclusion
This systematic review and meta-analysis will be expected to quantify the burden, admission and outcome of COVID-19 among asthmatic patients in Africa.
Availability of data and materials
This study has not been submitted and considered for publish in any journal. The datasets used and/or analyses during the study will be presented within the manuscript and available from the corresponding author on request.
Abbreviations
- COVID-19:
-
Coronavirus Disease in 2019
- PRISMA-P:
-
Preferred Reporting Items for Systematic reviews and Meta-Analysis protocol
- WHO:
-
World Health Organization
References
Kamel Boulos MN, Geraghty EM. Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic and associated events around the world: how 21st century GIS technologies are supporting the global fight against outbreaks and epidemics. Int J Health Geogr. 2020;19:8. https://doi.org/10.1186/s12942-020-00202-8.
Novel CPERE. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(2):145.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13.
Organization WH. Novel Coronavirus ( 2019-nCoV): situation report, 3. 2020.
Shahid Z, Kalayanamitra R, McClafferty B, Kepko D, Ramgobin D, Patel R, et al. COVID-19 and older adults: what we know. J Am Geriatr Soc. 2020;68(5):926–9.
Du Y, Tu L, Zhu P, Mu M, Wang R, Yang P, et al. Clinical features of 85 fatal cases of COVID-19 from Wuhan. A retrospective observational study. Am J Respir Crit Care Med. 2020;201(11):1372–9.
Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809–15.
Qiao J. What are the risks of COVID-19 infection in pregnant women? Lancet. 2020;395(10226):760–2.
Song J, Zeng M, Wang H, Qin C, Hou HY, Sun ZY, et al. Distinct effects of asthma and COPD comorbidity on disease expression and outcome in patients with COVID-19. Allergy. 2020. https://doi.org/10.1111/all.14517.
Yu Y, Chen P. Coronavirus disease 2019 (COVID-19) in neonates and children from China: a review. Front Pediatr. 2020;8:287.
Lithander FE, Neumann S, Tenison E, Lloyd K, Welsh TJ, Rodrigues JC, et al. COVID-19 in older people: a rapid clinical review. Age Ageing. 2020;49(4):501–15. https://doi.org/10.1093/ageing/afaa093.
Nishiga, M., Wang, D.W., Han, Y. et al. COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat Rev Cardiol. 2020;17:543–58. https://doi.org/10.1038/s41569-020-0413-9.
Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiat. 2020;7(7):611–27. https://doi.org/10.1016/S2215-0366(20)30203-0.
Cummings MJ, Baldwin MR, Abrams D, Jacobson SD, Meyer BJ, Balough EM, et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet. 2020;395(10239):1763–70. https://doi.org/10.1016/S0140-6736(20)31189-2.
Peters MC, Sajuthi S, Deford P, Christenson S, Rios CL, Montgomery MT, et al. COVID-19 related genes in sputum cells in asthma: relationship to demographic features and corticosteroids. Am J Respir Crit Care Med. 2020;202(1). https://doi.org/10.1164/rccm.202003-0821OC.
Bousquet J, Jutel M, Akdis CA, Klimek L, Pfaar O, Nadeau KC, et al. ARIA-EAACI statement on asthma and COVID-19 (June 2, 2020). Allergy. 2020. https://doi.org/10.1111/all.14471.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
WHO reference number: WHO/COVID-19/laboratory/2020.4. https://www.who.int/publications-detail/global-surveillance-for-human-infectionwith-novel-coronavirus-(2019-ncov).
World Health Organization. Laboratory testing for coronavirus disease (COVID-19) in suspected human cases: interim guidance, 19 March 2020: World Health Organization; 2020. https://apps.who.int/iris/handle/10665/331501. License: CC BY-NC-SA 3.0 IGO.
Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–9.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014;72(1):39.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Acknowledgments
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
AH, WA, DB was conceived and designed the study. The conceptualization and design of the study were contributed by all authors. The initial protocol was drafted by GM, WA KZ, and TH. All authors contributed to the development of the selection criteria, the risk of a bias assessment strategy, and data extraction criteria. All authors read, provided feedback, and approved the final protocol.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hailay, A., Aberhe, W., Zereabruk, K. et al. The burden, admission, and outcomes of COVID-19 among asthmatic patients in Africa: protocol for a systematic review and meta-analysis. asthma res and pract 6, 8 (2020). https://doi.org/10.1186/s40733-020-00061-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40733-020-00061-x