Abstract
Purpose
This study aims to evaluate the amount of distortion using computer-guided implant surgery with 3D printed surgical guides in limited edentulous spaces.
Materials and methods
25 bone level self-tapping implants (Straumann® BL and BLT) were randomly inserted in either distal or intercalary posterior mandibular edentulism using a fully digital protocol and 3D printed surgical guides. Amount of inaccuracy was evaluated after superimposing the 3 coordinates of virtually planned and final implant images, which were obtained using intra-oral scans and scan bodies. Four evaluation parameters were considered: origo-displacement, error depth, apical displacement and angle between the planned and the placed implant.
Results
The average of distortion was 0.71 mm for the origo-displacement, 0.36 mm for the error depth, 0.52 mm for the horizontal displacement and 3.34º for the error angle.
Conclusion
The major reason of exclusion was CBCT artifacts. Results of this study were aligned with the results of previous studies concerning partially edentulous spaces. CAD/CAM manufacturing process did not result in significant distortion whilst the biggest part of distortions originated from the surgical process. The learning curve in computer-guided implant surgery presented an important source of inaccuracy.
Trial registry
This trial is registered to the ClinicalTrials.gov Protocol Registration.
-
Name of the registry: ClinicalTrials.gov Protocol Registration.
-
Trial registration number: NCT06277076.
-
Date of registration: February 17, 2024 Retrospectively registered.
-
URL of trial registry record: https://register.clinicaltrials.gov/NCT06277076.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Static Implant guided surgery (SIGS) or Computerized Implant Guided Surgery (CIGS) is nowadays commonly used in our dental practice. In this digital workflow, implant positioning is planned pre-operatively based on cone beam computed tomography (CBCT) and optical scan of the patient, and the surgical procedure is then performed accordingly using templates [1]. Besides optimal 3D implant positioning, guided surgery has several advantages such as better prosthetically-driven implant placement, respect of the neighboring anatomy, and reduced treatment duration. Furthermore, it presents a precious communication tool to discuss treatment options with prosthodontists, lab technicians, as well as patients. All these inputs considerably enhance the esthetic and functional outcomes of implant treatments [2,3,4].
Accuracy and precision of implant placement are crucial in cases of adjacent anatomical structures, limited crestal volume, or planned immediate loading protocol [5]. Static guided implant surgery showed better accuracy than both free-hand [6,7,8] and dynamic guided implant surgery (navigation surgery) [9]. However, static guided implant surgery consists of several steps, and each one could present various sources of distortions. The cumulative amount of these distortions constitutes the final amount in terms of inaccuracy.
Among these sources of distortion is the superimposition of CBCT images and intra-oral surface scan during planning, especially in cases of artifacts. Also, the gap between sleeve and spoon, gap between drills and spoon, length of the drills, drilling movement as well as skills of the surgeon are sources of inaccuracy in computer-guided protocols [10, 11].
Moreover, the concerned length of edentulism is highly related to the amount of distortion. While most articles on guided-surgery accuracy combine the results of all types of edentulism, a recent systematic review highlights the difference in results between fully and partially edentulous cases. Thus, the amount of deviation varies based on the type of edentulism. The larger the edentulous space, the higher is the inaccuracy of guided implant positioning [12]. This is in relation with the type of tissue supporting the surgical guide. For instance, mucosa and tooth-supported guides are far better than bone-supported ones in terms of stability and accuracy [13].
Accordingly, several techniques, such as fixation pins and temporary implants, are proposed to stabilize the surgical guide and reduce distortion values. Also, addition of supportive reinforcement bars within the resin material of surgical guides is used to avoid bending and limit deviations [14].
The present study focuses on partially edentulous jaws, specifically distal-shortened mandible and bounded spaces of two to three teeth. The aim is to evaluate the accuracy and precision of fully guided implant surgery in partially edentulous mandibular spaces.
Materials and methods
Population
Patients presenting at Saint Joseph University of Beirut dental clinics with a distal-shortened mandible or distal intercalary space of two to three missing premolars or molars (class I, II or VI according to Kennedy’s classification on edentulous spaces) and requiring implant-supported reconstructions were selected to participate in this study.
For each case two implants were placed with a fully guided procedure followed by the insertion of two to three splinted temporary resin crowns that were virtually designed and prepared. Temporary crowns were loaded either immediately or conventionally (after 2 months) depending on primary stability.
Thirteen patients were included in this study with twenty-five implants eligible for accuracy evaluation. Deviation of final implant position compared to virtually planned implant position was assessed after superimposing the two scanned 3D images.
Inclusion criteria
-
Age over 18 years old.
-
Acceptable oral hygiene with no signs of active periodontal disease or local infection.
-
ASA 1 and 2.
-
Non or Light smoking (< 10 cigarettes per day).
-
Acceptable intermaxillary space (44 mm minimum).
-
Minimal crestal width of 5.5 mm.
-
Minimal residual bone height of 10 mm above the alveolar nerve canal.
Exclusion criteria
-
Head and neck irradiation.
-
Bone grafted sites.
-
Severe bruxism.
-
CBCT with exaggerated artifacts.
-
Limited intermaxillary space.
An Institutional Review Board (IRB) approval was given by the Committee for the Protection of Human Subjects (CPHS) of the Saint Joseph University of Beirut-Lebanon, and an informed consent was signed by all patients.
Pre-operative planning
A pre-operative CBCT was taken with an open mouth of 2 cm to prevent any overlap or artifact from the opposite arch. DICOM files (Digital Imaging and Communications in Medicine) derived from the CBCT were imported into Implant Studio (3Shape® Copenhagen, Denmark) planning software.
An optical surface scan was performed using TRIOS (3Shape® Copenhagen, Denmark) optical scan. The resulting 3oxz file (optical 3D image) was exported to the Implant Studio software as well (stage 1 A and 1B Fig. 1).
The 4 stages of the digital workflow leading to deviation assessment. Stage 1 and 2 are pre-implant placement; Stage 3 and 4 are post-implant placement. 1 A- DICOM/DCM File exported from CBCT to the planning software for super-imposition; 1B- 3OXZ file exported from the intra-oral scanner to Implant Studio software for superimposition and implant planning; 2- STL file used to print the surgical guide and 3OXZ file used to design and mill the crowns in the dental Lab; 3- Implant scanning and 3OXZ file export to Trios Dental System for flag matching with the scan-body; 4-The Information of the planned implant (4 A) and the placed implant (4B) with coordinates embedded are exported as DCM files to the deviation test tool. (3OXZ: 3Shape Order Exchange Zip File; DICOM/DCM: Digital Imaging and Communications in Medicine; STL: Standard Tessellation Language)
The two 3D images were subsequently superimposed and implant placement was planned in a prosthetically-driven manner. A 2 mm security distance from the alveolar nerve, that was set by the 6th ITI consensus conference in 2018 (6), was respected in this study.
In case of distal edentulous space, a lateral fixation pin was planned to strengthen the guide, prevent its distal bending, and achieve multiple tissue support (mucosal, dental and pin support). After implant planning and guide design (see stage 2 Fig. 1), an STL file (Stereo Lithography interface format) was obtained for guide printing, a 3oxz file for temporary resin crowns fabrication, and a DICOM file for future superimposition with the final implants position (stage 4 A Fig. 1).
Surgical guide and crown manufacturing
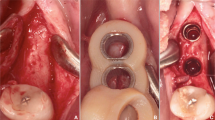
STL files were used to print the resin surgical guide with a 3D printer - Envisiontec (Envisiontec Vida HD, Envisiontec Inc, USA). Lateral windows for seating check, additional bars for reinforcement and metal rods inserted into the resin for higher rigidity were designed (Fig. 2).
For immediate loading protocols, virtual splinted crowns were designed using a Dental System DS Software (3Shape, Copenhagen, Denmark) and produced by a milling machine (Amann Girrbach AG, Koblach, Austria).
To basically evaluate the accuracy of CAD/CAM processes, a mandibular cast was printed with replicas of planned implants inserted into this model, and three tests were effectuated (Fig. 3). Firstly, the surgical guide fit was checked by seating the later over the printed model and appraising its stability. Secondly, implant placement procedure was tested performing a simulation and evaluating if the laser mark of implant holder corresponds to the planned level of offset. Thirdly, the crown fit was assessed on the corresponding screw-retained Variobase abutments from Straumann. These tests proved the accuracy of pre-operative steps related to the digital workflow. Thus, CAD/CAM protocol was free from any source of distortion.
In cases of reduced mouth opening, a lateral window was created in the sleeve and guide to prevent any pressure during drilling procedures.
Simulation proving the accuracy of the pre-operative steps related to the digital workflow: a- Printed cast with preparation for implant digital analog. b- Control of the surgical guide seating. c- Simulation of free-hand implant insertion by checking the laser-mark of the implant holder. d- Positioning the screw-retained splinted crowns to validate the accuracy of their seating once again
Guided implant surgery protocol
Only one experienced and skilled investigator was in charge to perform all the surgeries in respect with the consistency of the protocol.
After local anesthesia, the surgical guide was seated, 1.25 mm fixation pins (Straumann) were placed, stability of the surgical guide was checked, and special attention for rocking or loose fit of the guide was accorded. Surgical guides were tooth-mucosa supported and were stabilized with fixation pins (Fig. 4). Depending on the thickness of the tissue and the amount of keratinized tissue around the implantation area, the investigators decided to either choose a flapless or open-flap procedure.
The followed drilling protocol was according to the implant studio planning, using adequate guided surgical cassette, drills with stoppers, and metallic drill handles. After implant site preparation, implants were inserted in a fully guided manner through the sleeve using a guided surgery implant holder with corresponding off-set laser marks. Bone level (BL) and bone level tapered (BLT) Roxolid implants (Straumann AG, Basel, Switzerland) with a diameter of either 3.3–4.1 mm and length of 8–10 mm were chosen.
After the surgery, patients were asked to take the following medications for seven days: Diclofenac as NSAID twice daily, Paracetamol 1 g if needed and mouthwash with Chlorhexidine Digluconate 0.12% three times per day.
Measured parameters
1. Primary stability assessment
_ At the last rotation during implant insertion, a customized adaptor for the digital ratchet of the insertion torque (IT) device (DTA, by studio AIP Srl, Italy) was used as an implant holder and the values were recorded with a transducer connected to a computer via Bluetooth wireless. A graph displayed the variation of IT with each rotation on DT1 2.2 software, and the highest value was considered the maximum insertion torque in Ncm.
_ Implant stability quotient ISQ was also recorded following the resonance frequency analysis RFA using the Osstell AB ISQ device (Ostell ISQ; Integration Diagnostics AB, Göteborg, Sweden).
The ISQ records were only scored to follow with time the evolution of the implant stability, since it is considered as an assessment which can provide prospective monitoring and shows fluctuations in stiffness of the implant interface as bone matures from primary to secondary contact [15].
In the current study the ISQ was only a variable used to monitor the behavior of the secondary stability after immediate loading.
_ When primary stability of the two implants reached 30 Ncm and above, an immediate loading protocol was applied by inserting two splinted, prefabricated and milled screw-retained crowns on top of Variobase abutments for bridge (Straumann AG, Basel, Switzerland). (Fig. 5)
2. Assessment of the deviations
A preliminary clinical visual check of the distortions was observed at the moment of insertion of the pre-milled splinted crowns. For adjustment of misfitted temporary restorations due to inaccuracy of implant placement, a relining or reparation with resin material was performed to ensure a passive fit (Fig. 6).
The real assessment of the deviations was performed only at eight weeks after implant placement. Intra-oral surface scans of the final implants’ positions were registered using a digital scan body. Resulting 3oxz output files were exported to the Dental system DS software of 3Shape to generate a DCM file of the placed implant. Afterwards, the deviations between virtual implant VI and placed implant PI positions were calculated with a “comparison tool” developed by 3Shape company for research purposes (Fig. 7; stage 4 Fig. 1).
Four different measures were provided to calculate the amount of distortion in millimeter (mm) or in degree: Origo Displacement OD (mm), Horizontal Displacement HD (mm), Error Depth ED (mm) and Error Angle EA (degree) (Fig. 8).
Results
Mean deviation of parameters between VI and PI positions for 25 implants was: 0.71 mm for Origo-Displacement, 0.36 mm for Error Depth, 0.52 mm for Horizontal Displacement and 3.34º for Error Angle (Table 1). Minimal and maximal deviation values of the four parameters are presented in Table 1.
PI showed significantly better accuracy in ED compared to HD. Minimal ED was 0.01 mm and maximal ED was 0.8 mm, while minimal HD was 0.12 mm and maximal HD was 1.25 mm.
Difference in accuracy between intercalated implants with or without fixation pins and distally placed implants with fixation pins was not statistically significant. Results are divided into groups depending on the type of tissue support (Fig. 9).
Also, difference between the two different implant macro-designs in terms of accuracy was not statistically significant. BL and BLT Straumann implants showed respectively the following values of distortions: 0.67 and 0.74 mm for OD, 0.35 and 0.44 mm for ED, 0.49 and 0.56 mm for HD, and 3.36º and 3.31º for EA (Table 2).
Implant length showed difference in accuracy between the two implants used in the study. Mean values of 8 mm and 10 mm implants were respectively 0.87 and 0.63 mm for OD, 0.39 and 0.34 mm for ED, 0.67 and 0.46 mm for HD, and 3.50º and 3.18º for EA. Results showed better accuracy for longer implants, however they were not statistically significant. (Table 3).
Discussion
Guided implant surgery is comprised of several steps and each one could be a source of inaccuracy [12]. Firstly, radiographic artifacts may embed the superimposition of CBCT and digital scan surfaces as per many cases that were excluded from this study. Different CBCT sources, software, and segmentation techniques were proposed to reduce these artifacts but could not completely resolve this limitation [16].
Secondly, the process of CAM or digital manufacturing of the surgical guides and temporary crowns. In the current study, 3D printing the models were printed and the fit of surgical guides and milled crowns was tested. These control tests showed great accuracy; thus, deviations mainly resulted from the superimposition or the surgical phase.
Another source of deviation is limited inter-arch space which may prevent free insertion of drills into the sleeves and cause bending of the surgical guide. This issue could not be completely resolved even after creating lateral windows in the sleeves. This possible source of distortion was excluded from this study.
Several studies proved that a certain void exist between both sleeve and drill handle, and between drill handle and drill, which is responsible for a certain amount of deviation [17]. In all cases of this study, adequate guide retention and adaptation was ensured to avoid distortions and bending, sleeves were embedded into the resin to guarantee their rigid stabilization, and bars were added to reinforce the guide.
Moreover, Herekar et al. related implant macro-design to CIGS precision. Cylindrical implants were more likely to interfere with the cortical wall or be pushed away from it while tapered implants with narrow apexes were supposed to penetrate the cortical wall or stay away from it [12]. This is not in accordance with the results of this study where the difference between BL and BLT implants in terms of accuracy was not statistically significant.
Concerning implant length, 8 mm implants showed more distortion than the 10 mm implants in the current study. Similarly, Derksen et al. evaluated 145 implants and found long implants of 12 mm with no cortical interference to have significantly better accuracy in angular deviations than shorter implants [13]. Conversely, Vercruyssen et al. did not find any influence of implant length on CIGS accuracy [18]. While several other studies found that long implants have higher deviations at the apex. Accordingly, decreasing the drilling distance below the guided sleeve, by using shorter sleeve heights or shorter implants, could significantly increase the accuracy of CIGS [19,20,21].
Several studies evaluated the influence of tissue support on the accuracy of CIGS. A recent systematic review proved that mucosal-supported guides show significant reduction in angular deviation (P = 0.02), point-of-entry deflection (P = 0.002), and tip deviation (P = 0.04) when compared to bone guides. Whereas mucosa-supported and teeth-supported guides had no statistically significant difference for any of the outcome measures [22]. For these types of guides, Verhamme et al. recommended the use of fixation screws to decrease the bucco-lingual deviation. Fixation screws were used to stabilize all surgical guides in the present study, which explains the reduced deviation of OD and HD values [21].
On the other hand, this study was limited to edentulous spaces of two adjacent teeth without considering fully edentulous jaws, which explains the low level of cumulative distortions. A meta-analysis showed that partially edentulous cases have a significantly higher accuracy at entry point and at the apex when compared to fully edentulous cases [12]. Schnutenhaus in a study on partially edentulous spaces did not find a significant difference between implants placed in distal edentulous spaces and those in single tooth gaps [23]. These results are in accordance with the findings of the current study.
Previous studies regarding accuracy of guided surgery protocols used superimposition of two STL files: first coming from implant planning software and second from post-operative CBCT images. This superimposition was performed using different software such as the Geomagic [12, 21]. However, a second CBCT could increase the amount of distortion due to artifacts and expose the patient to more important irradiation. In a study conducted by Schnutenhaus et al. in 2016, the final implant position was obtained by taking a conventional impression, scanning it, and superimposing the digitalized model with the planned file using Geomagic software [23]. In the current study, the two optical scans of VI and PI were superimposed based on the same matrices containing 3D coordinates of the initial digital scan. This novel superimposition method did not require additional irradiation nor other software which may induce further distortions. No studies comparing these different assessment techniques were found in the literature.
The limitation of our study is with the small sample size in regard with the different implant macro-design and different length.
Conclusion
CIGS was a reliable choice for optimal prosthetically-driven implant surgery in partially edentulous spaces. However, some steps of CIGS were important sources of inaccuracy such as CBCT artifacts, superimposition technique, implant length, and surgical guide design. While the largest part of distortion originated from the surgical process, CAD/CAM manufacturing process did not result in any distortions. Controlling the distortion parameters decreases the amount of CIGS inaccuracy. Future studies with larger sample sizes must be conducted to validate the results of this study and compare the accuracy of CIGS in different types of edentulism.
Data availability
The authors confirm that there is no associated data included in this manuscript.
Abbreviations
- CAD-CAM:
-
Computerized aided design-Computerized aided manufacturing
- 3D:
-
Three dimensional
- SIGS:
-
Static Implant guided surgery
- CIGS:
-
Computerized Implant Guided Surgery
- CBCT:
-
Cone beam computed tomography
- ASA:
-
American Society of Anesthesiology score
- IRB:
-
Institutional Review Board
- CPHS:
-
Committee for the Protection of Human Subjects
- DICOM/ DCM:
-
Digital Imaging and Communications in Medicine
- STL:
-
Standard Tessellation Language
- 3oxz:
-
3Shape Order Exchange Zip File
- BL:
-
Bone level implant
- BLT:
-
Bone level tapered implant
- IT:
-
Insertion torque
- RFA:
-
Resonance frequency analysis
- ISQ:
-
Implant stability quotient
- VI:
-
Virtual implant position
- PI:
-
Placed implant position
- mm:
-
Millimeter
- OD:
-
Origo Displacement
- HD:
-
Horizontal Displacement
- ED:
-
Error Depth
- EA:
-
Error Angle
References
Younes F, Cosyn J, De Bruyckere T, Cleymaet R, Bouckaert E, Eghbali A. A randomized controlled study on the accuracy of free-handed, pilot-drill guided and fully guided implant surgery in partially edentulous patients. J Clin Periodontol. 2018;45:721–32.
Li J, Chen Z, Chan H-L, Sinjab K, Yu H, Wang H-L. Does flap opening or not influence the accuracy of semi-guided implant placement in partially edentulous sites? Clin Implant Dent Relat Res. 2019;21:1253–61.
Arısan V, Karabuda CZ, Özdemir T. Implant surgery using bone- and mucosa-supported stereolithographic guides in totally edentulous jaws: surgical and post-operative outcomes of computer-aided vs. standard techniques. Clin Oral Implants Res. 2010;21:980–8.
van Steenberghe D, Molly L, Jacobs R, Vandekerckhove B, Quirynen M, Naert I. The immediate rehabilitation by means of a ready-made final fixed prosthesis in the edentulous mandible: a 1-year follow-up study on 50 consecutive patients. Clin Oral Implants Res. 2004;15:360–5.
Bassil J, Abi Sleiman A, Mrad S, Noujeim Z. (2021) The Zygomatic Buttress as an Efficient Intraoral Donor Site for Limited Maxillary Reconstructions: A Case Series and Brief Literature Review. Case Rep. Dent. 2021.
Chen Z, Li J, Sinjab K, Mendonca G, Yu H, Wang H-L. Accuracy of flapless immediate implant placement in anterior maxilla using computer-assisted versus freehand surgery: a cadaver study. Clin Oral Implants Res. 2018;29:1186–94.
Vermeulen J. The Accuracy of Implant Placement by experienced surgeons: guided vs Freehand Approach in a simulated Plastic Model. Int J Oral Maxillofac Implants. 2017;32:617–24.
Noharet R, Pettersson A, Bourgeois D. Accuracy of implant placement in the posterior maxilla as related to 2 types of surgical guides: a pilot study in the human cadaver. J Prosthet Dent. 2014;112:526–32.
Jung RE, Schneider D, Ganeles J, Wismeijer D, Zwahlen M, Hämmerle CHF, Tahmaseb A. Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implants. 2009;24:92–109.
El Kholy K, Janner SFM, Schimmel M, Buser D. The influence of guided sleeve height, drilling distance, and drilling key length on the accuracy of static computer-assisted Implant surgery. Clin Implant Dent Relat Res. 2019;21:101–7.
Cassetta M, Bellardini M. How much does experience in guided implant surgery play a role in accuracy? A randomized controlled pilot study. Int J Oral Maxillofac Surg. 2017;46:922–30.
Tahmaseb A, Wu V, Wismeijer D, Coucke W, Evans C. The accuracy of static computer-aided implant surgery: a systematic review and meta-analysis. Clin Oral Implants Res 29 Suppl. 2018;16:416–35.
Tahmaseb A, Wismeijer D, Coucke W, Derksen W. Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implants. 2014;29:25–42.
Tahmaseb A, De Clerck R, Aartman I, Wismeijer D. Digital Protocol for reference-based guided surgery and Immediate Loading: a prospective clinical study. Int J Oral Maxillofac Implants. 2012;27:1258–70.
Akkocaoglu M, Uysal S, Tekdemir I, Akca K, Cehreli MC. Implant design and intraosseous stability of immediately placed implants a human cadaver study. Clin Oral Implants Res. p. 2005;16:202–9.
Flügge T, Derksen W, Te Poel J, Hassan B, Nelson K, Wismeijer D. Registration of cone beam computed tomography data and intraoral surface scans - a prerequisite for guided implant surgery with CAD/CAM drilling guides. Clin Oral Implants Res. 2017;28:1113–8.
Koop R, Vercruyssen M, Vermeulen K, Quirynen M. Tolerance within the sleeve inserts of different surgical guides for guided implant surgery. Clin Oral Implants Res. 2013;24:630–4.
Vercruyssen M, Coucke W, Naert I, Jacobs R, Teughels W, Quirynen M. Depth and lateral deviations in guided implant surgery: an RCT comparing guided surgery with mental navigation or the use of a pilot-drill template. Clin Oral Implants Res. 2015;26:1315–20.
D’haese J, Van De Velde T, Elaut L, De Bruyn H. A prospective study on the accuracy of mucosally supported stereolithographic surgical guides in fully edentulous maxillae. Clin Implant Dent Relat Res. 2012;14:293–303.
Verhamme LM, Meijer GJ, Soehardi A, Bergé SJ, Xi T, Maal TJ. An accuracy study of computer-planned implant placement in the augmented maxilla using osteosynthesis screws. Int J Oral Maxillofac Surg. 2017;46:511–7.
Verhamme LM, Meijer GJ, Bergé SJ, Soehardi RA, Xi T, de Haan AF, Schutyser F, Maal TJ. An accuracy study of computer-planned implant placement in the augmented maxilla using mucosa-supported surgical templates. Clin Implant Dent Relat Res. 2015;17:1154–63.
Raico Gallardo YN, da Silva-Olivio IRT, Mukai E, Morimoto S, Sesma N, Cordaro L. Accuracy comparison of guided surgery for dental implants according to the tissue of support: a systematic review and meta-analysis. Clin Oral Implants Res. 2017;28:602–12.
Schnutenhaus S, Edelmann C, Rudolph H, Luthardt RG. Retrospective study to determine the accuracy of template-guided implant placement using a novel nonradiologic evaluation method. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;121:e72–9.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, Clinical work, data collection and analysis were performed by Emile Chrabieh and assisted by Joseph Zaarour, Christine Hanna. The draft manuscript was written by Emile Chrabieh, Stephanie Mrad and Stephanie Rameh. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
An Institutional Review Board (IRB) approval was given by the Committee for the Protection of Human Subjects (CPHS) of the Saint Joseph University of Beirut-Lebanon.
Consent to participate
Written informed consent was obtained from the patients.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chrabieh, E., Hanna, C., Mrad, S. et al. Accuracy of computer-guided implant surgery in partially edentulous patients: a prospective observational study. Int J Implant Dent 10, 36 (2024). https://doi.org/10.1186/s40729-024-00552-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40729-024-00552-z