Abstract
Purpose
Particulate bovine bone substitutes (BS) are commonly used in oral regeneration. However, more literature is needed focusing on comparative analyses among various particulate bovine BS. This study evaluates pre-clinical and clinical data of different particulate bovine BS in oral regeneration.
Methods
A narrative review was conducted by screening the PubMed database Included in the review were pre-clinical and clinical studies until 2024 comparing a minimum of two distinct particulate bovine BS. In addition to examining general data concerning manufacturing and treatment processes, biological safety, physical and chemical characteristics, and graft resorption, particular emphasis was placed on assessing pre-clinical and clinical data related to ridge preservation, sinus floor elevation, peri-implant defects, and various forms of alveolar ridge augmentation utilizing particulate bovine BS.
Results
Various treatment temperatures ranging from 300 to 1,250 °C and the employment of chemical cleaning steps were identified for the manufacturing process of particulate bovine BS deemed to possess biosecurity. A notable heterogeneity was observed in the physical and chemical characteristics of particulate bovine BS, with minimal or negligible graft resorption. Variations were evident in particle and pore sizes and the porosity of particulate bovine BS. Pre-clinical assessments noted a marginal inclination towards favorable outcomes for particulate bovine BS subjected to higher treatment temperatures. However, clinical data are insufficient. No distinctions were observed regarding ridge preservation, while slight advantages were noted for high-temperature treated particulate bovine BS in sinus floor elevation.
Conclusions
Subtle variances in both pre-clinical and clinical outcomes were observed in across various particulate bovine BS. Due to inadequate data, numerous considerations related to diverse particulate bovine BS, including peri-implant defects, must be more conclusive. Additional clinical studies are imperative to address these knowledge gaps effectively.
Graphical abstract

Similar content being viewed by others
Background
Dental implantology has grown significantly, emerging as a hallmark of modern dentistry and prosthodontics [1]. A pivotal challenge in this field is ensuring an adequate supply and quality of bone within the alveolar ridge, a critical factor for successful implant placement [2]. A minimum alveolar width of 4 mm and height of 7 mm are deemed necessary for effective implant placement [3]. Unfortunately, the alveolar ridge undergoes continuous three-dimensional atrophy following tooth loss [4], with atrophy rates ranging from 25% within one year to 40–60% within five years of the initial bone volume [5,6,7,8]. Consequently, ridge preservation techniques have been established to mitigate this process within specific parameters [9,10,11].
Moreover, conditions such as craniofacial malformations, periodontal disease, trauma, or post-tumor therapy may further compromise the alveolar bone [12]. Subsequently, short and diameter-reduced implants have been introduced for placement in situations with limited bone availability [13, 14]. Despite these advancements, regeneration of the alveolar crest is often necessary to address alveolar ridge atrophy. Various surgical techniques have been developed, including sinus floor elevation and guided bone regeneration (GBR) [15]. The ideal grafting material should possess osteogenic, osteoinductive, and osteoconductive properties, along with rapid and adequate vascularization and bone remodeling capabilities and high-volume stability to serve as a placeholder until the defect is remodeled by newly formed bone [8, 16]. These prerequisites have led to autogenous bone being recognized as the “gold standard” for alveolar ridge augmentation, owing to its optimal physiological compatibility, expedited healing, and effective integration [17].
Conversely, the drawbacks associated with autogenous bone grafts, including donor site morbidity and potential nerve injuries, are frequently documented [18,19,20,21]. As an alternative to autogenous grafts, bone substitutes (BS) of various origins have been developed, including allogeneic (from the same species, human), xenogeneic (from different species, such as bovine, porcine, or equine), and alloplastic (synthetic) materials [11, 22]. Those derived from bovine sources are particularly prevalent among xenogeneic grafts, demonstrating numerous satisfactory long-term clinical outcomes [23, 24]. These bovine-derived BS have exhibited significant biocompatibility and advantageous regenerative potential [25], which could be further improved by biofunctionalization the bovine BS using, for example, platelet-rich fibrin or hyaluronic acid [26,27,28,29,30]. Hence, bovine BS are extensively utilized in regenerative dentistry and oral regeneration, particularly in high- or low-temperature treated forms, such as spongious grafts [31]. Evidence suggests that bovine BS can yield comparable outcomes to autogenous grafts, especially in sinus floor elevation and GBR [16, 32]. This equivalence has been corroborated even regarding implant survival rates following sinus elevation and ridge augmentation using BS [33]. In addition, xenogeneic BS used to preserve the alveolar ridge, especially in conjunction with a barrier membrane, can significantly reduce additional bone grafting procedures. On the other hand, alveolar ridge preservation may incur higher costs and has a limited effect on increasing soft tissue quality or quantity of the alveolar ridge [34, 35]. Deproteinized bovine BS comprises an inorganic hydroxyapatite-supported structure with osteoconductive properties and protracted resorption kinetics [36,37,38]. Residual graft material has been detected even a decade post-augmentation, but the extent of osteoclastic activity surrounding bovine BS remains debatable [16, 39, 40]. Given the variety of particulate bovine BS available, it remains to be seen which BS is most suitable for specific clinical scenarios, each with its advantages and limitations.
This narrative review aims to evaluate pre-clinical and clinical data comparing different particulate bovine BS for oral regeneration.
Methods
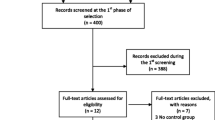
A narrative review was conducted by systematically searching the PubMed database up to February 2024, utilizing various combinations of search terms including “particulate”, “bovine”, “bone substitute”, “bone graft”, “pre-clinical”, “clinical”, “in-vitro”, “in-vivo”, “ridge preservation”, “sinus floor elevation”, “peri-implant defects”, “alveolar ridge augmentation”, and “titanium mesh”. Pre-clinical and clinical studies that compared at least two distinct particulate bovine BS were included in the narrative review. Studies that compared particulate bovine BS with other types of particulate BS (e.g., synthetic BS), different particulate xenogeneic BS (e.g., porcine and equine), particulate bovine BS with bovine bone blocks, and identical particulate bovine BS with and without biological substitute modifications (e.g., platelet-rich fibrin, PRF), as well as those that exclusively evaluated a single particulate bovine BS, were excluded. The review focused on general information regarding manufacturing and treatment processes, biological safety, physical and chemical characteristics, and graft resorption of the included particulate bovine BS. Additionally, specific attention was given to pre-clinical data and clinical outcomes related to ridge preservation, sinus floor elevation, peri-implant defects, lateral and vertical alveolar ridge augmentations, and particulate bovine BS for filling titanium meshes.
Results
Manufacturing and treatment process of particulate bovine bone substitutes
The primary objective of the treatment process is to eliminate all organic bone components, including proteins, potentially immunologically active substances, and pathogens. Only the mineral bone matrix, particularly hydroxyapatite with an ultra- and nanostructure like human bone, should remain intact. Variations in the manufacturing processes of particulate bovine BS account for differences in material properties even though the origin of the bovine bone remains constant. To produce high-temperature treated bovine BS, the bone raw material undergoes stepwise heating to temperatures exceeding 1,200 °C, followed by multiple cleaning and washing steps using only water. In this regard, heat treatment appears to be the most prevalent preparation method [41]. The elevated temperature offers the advantage of eliminating organic compounds and safely eradicating pathogens such as bacteria, viruses, and prions [42]. In contrast, low-temperature treated bovine BS is prepared through a heat treatment process reaching temperatures up to 300 °C, followed by a chemical cleaning step involving highly concentrated alkaline sodium hydroxide [43]. Due to these distinct processing methods, high-temperature treated bovine BS exhibits highly pure and crystalline hydroxyapatite ceramic characteristics, featuring interconnected pores and a super hydrophilic surface texture. Additionally, its hydroxyapatite crystal size is increased by 500–1,000% compared to human bone. Conversely, low-temperature treated bovine BS displays a texture with hydroxyapatite crystal sizes increased by 200–300% and a more fiber-like structure [43, 44]. Table 1 summarizes different manufacturers’ different low- and high-temperature treated bovine BS.
In summary, distinctions must be made between high-temperature and low-temperature treated particulate bovine BS, with both heat and chemical treatment processes utilized depending on the specific product and manufacturer.
Biological safety of particulate bovine bone substitutes
The fundamental prerequisite for utilizing BS derived from natural sources is thoroughly removing tissue, organic constituents, immunogenic substances, and pathogens to mitigate the risks of disease transmission and adverse reactions. The initial step in ensuring material safety involves carefully selecting donor animals. Bovine bones, particularly femoral heads, sourced from registered slaughterhouses in countries classified as having negligible risk for bovine spongiform encephalopathy (BSE) by the World Organization for Animal Health (OIE), are utilized in the production of both high- and low-temperature treated BS [45, 46]. Another crucial safety measure involves employing approved heat treatment methods independently or with chemical cleaning. It is established that temperatures exceeding 800 °C significantly reduce the risk of transmitting prion diseases, particularly BSE, to an acceptable minimum [47]. Conversely, for low-temperature treated BS, prion inactivation primarily relies on treatment with highly concentrated sodium hypochlorite [45, 48, 49]. In 2011, Kim et al. conducted a systematic review to assess the risk of prion disease transmission associated with bovine BS. Residual protein structures were found in low-temperature treated BS [50], in contrast to high-temperature treated BS [51]. No literature was found regarding the efficacy of BSE prion inactivation during the manufacturing process of bovine BS. However, a patented method in Canada combines sodium hypochlorite and temperatures exceeding 600 °C, claiming to produce a BSE prion-free bovine bone grafting substitute (CA2649970C). In summary, while bovine BS may theoretically pose a risk of transmitting BSE prions, the current available information does not allow for quantification of this risk [52]. From a practical-clinical standpoint, there have been no reported instances of disease transmission through bovine BS, suggesting that their application is unlikely to result in transmission complications [43].
Physical and chemical characteristics of particulate bovine bone substitutes
As per the manufacturer specifications, the particle size of high-temperature treated bovine BS ranges from 500 to 1,000 μm, whereas that of low-temperature treated BS ranges from 250 to 1,000 μm. Literature on human bone indicates an average particle size of approximately 280 μm [53]. High-temperature treated BS exhibits a porosity of 72%, whereas low-temperature treated BS ranges from 75 to 80% [54]. Both bovine BS formulations consist of crystalline components and possess calcium/phosphate ratios ranging from 1.75 to 1.33. Both variants demonstrate the release of calcium ions, albeit at lower levels than human bone (high-temperature treated BS: 4 mg/g; low-temperature treated BS: 12 mg/g; human bone: 20 mg/g) [53]. In addition to porosity, pore sizes are noteworthy, with a systematic review reporting pore sizes of bovine BS ranging from 1.3 to 1,000 μm [41, 55]. In brief, there is a notable heterogeneity in the characteristics of different bovine BS, particularly in porosity, crystallinity, and calcium/phosphate ratio [41]. Biomechanical properties of bovine BS are also affected by rehydration. In the case of bovine BS blocks, high-temperature treated BS demonstrated limited height reduction following rehydration compared to dry conditions, with no alteration in rigidity [56]. Regarding hydrophilicity, high-temperature treated BS exhibited increased hydrophilicity compared to low-temperature treated BS [56].
Resorption of particulate bovine bone substitutes
Ideally, bovine BS undergoes gradual remodeling into newly formed bone through a process known as “creeping substitution” [57]. For low-temperature treated BS, a minimal or complete absence of resorption is postulated [36, 58,59,60] with similar assumptions for high-temperature treated BS, where a prolonged resorption rate may be anticipated, if any [61]. Nonetheless, comparable stability in maxillary sinus volumes following sinus floor elevation with either low- or high-temperature treated BS has been observed [57, 62], suggesting similar resorption characteristics between the two BS. In conclusion, both low- and high-temperature treated bovine BS demonstrate minimal or negligible degradation within the body, thus qualifying them as potential permanent substitutes for bone regeneration and integration. A study assessing circumferential defect filling around implants in minipigs with either high- or low-temperature treated BS revealed equivalent outcomes regarding graft resorption and new bone formation at 8 and 12 weeks post-implantation [63].
Pre-clinical studies
Pre-clinical in vitro data
Concerning pre-clinical in vitro data, a study examined the effects of various particulate bovine, synthetic, and allogeneic BS (cerabone® (botiss biomaterials GmbH, Zossen, Germany), Bio-Oss® (Geistlich biomaterials Vertriebsgesellschaft mbH, Baden-Baden, Germany; bovine each), maxresorb® (botiss biomaterials GmbH; synthetic), maxgraft® (botiss biomaterials GmbH; allogeneic)) and their combination with platelet-rich fibrin (PRF) on various cell characteristics (cell viability, proliferation rate, and migration ability) of osteoblasts after 24 h in vitro. No differences were observed between the two tested particulate bovine BS under native conditions [26]. Another study addressed PRF-biofunctionalization, investigating the potential benefits of injectable PRF (iPRF) on four different particulate bovine BS (cerabone®; Bio-Oss®; creos™ xenogain® (Nobel Biocare AG, Kloten, Switzerland); MinerOss® X (BioHorizons, Birmingham, AL, USA)) and its impact on osteoblasts in vitro. Cell viability, metabolic activity, and gene expressions (alkaline phosphatase, ALP; osteocalcin, OCN; and bone morphogenetic protein-2, BMP-2) were analyzed at measurement timepoints after 3, 7, and 10 days. For native, non-iPRF modified BS, cerabone® exhibited the highest cell viability at all time points, while MinerOss® X showed the most increased metabolic activity after 3 days and cerabone® after 7 and 10 days. Overall, the authors observed a clear trend of favorable outcomes regarding cell viability and metabolic activity for high-temperature treated particulate bovine BS compared to low-temperature treated ones [29]. Another in vitro study investigated the effects of low-temperature (Bio-Oss®) and high-temperature treated BS (Osteograf®, DENTSPLY Friadent Ceramed, Lakewood, NJ, USA) and high-temperature bovine hydroxyapatite modified with p-15 on osteoblast cell viability, proliferation rate, and cell morphology. Osteograf® demonstrated higher proliferation rates and improved cell differentiation than Bio-Oss®, as confirmed by scanning electron microscopy [64]. In terms of optimal treatment temperatures, a study evaluated three different temperature durations and temperatures (3 h at 300 °C, 3 h at 300 °C followed by 6 h at 530 °C, and 3 h at 300 °C followed by 2 h at 1000 °C) and Bio-Oss®, on bone marrow stromal cells (migration, proliferation, differentiation) in vitro. In addition, calvaria defects in rabbits were employed to analyze bone regeneration and graft degeneration. The study found that 3 h at 300 °C followed by 6 h at 530 °C induced the highest cell attraction and improved cell differentiation, while both 3 h at 300 °C and 3 h at 300 °C followed by 6 h at 530 °C resulted in higher bone fraction after 6 and 12 weeks in vivo [65]. Ortiz-Puigpelat investigated the blood absorption of different bovine BS and demonstrated a significantly increased blood absorption of NuOss® (ACE Surgical Supply Inc, Brockton, MA, USA) and Bio-Oss® compared to Smartbone® (IBI SA Industrie Biomediche Insubri SA, Mezzovico-Vira, Switzerland) [66].
In summary, pre-clinical in vitro data may provide slight evidence of minor advantages of high-temperature treated BS, such as improved biocompatibility in cell cultures.
Pre-clinical in vivo data
In terms of pre-clinical in vivo data, synthetic calcium phosphate and two particulate bovine BS (low-temperature treated Bio-Oss®, high-temperature treated BonAP® (Legeros, New York University, NY, USA)) were implanted into the femoral epiphysis of rats and evaluated after three weeks. The bone ingrowth for the synthetic calcium phosphate was higher due to its increased resorption rate [67]. A recent review by Peric Kacarevic et al. synthesized findings from eight studies focusing on low-temperature treated BS (Bio-Oss®, seven studies in the rabbit calvaria model and one in sheep), three studies examining high-temperature treated BS (cerabone®, two studies in rabbit and rat calvaria models and one periapical study in cats), and one comparative study between high and low-temperature treated BS (cerabone® and Bio-Oss®) in the rabbit calvaria model, yielding overall comparable results. Depending on the time, new bone formation rates ranged from 0 to 57%. After 14–30 days, Bio-Oss® demonstrated an average new bone formation rate of 19%, whereas cerabone® exhibited 20%. After 42–84 days, Bio-Oss® showed an average new bone formation rate of 24%, while cerabone® displayed 47%. Finally, after 112–168 days, Bio-Oss® demonstrated an average new bone formation rate of 43%, whereas cerabone® exhibited 26% [43]. In a study by Manfro et al., three bovine BS (Bio-Oss®, bonefill® (Bionnovation biomaterials, São Paulo, Brazil), and GenOx® (Baumer, São Paulo, Brazil)) were analyzed, with blood clot augmentation as a control. Histomorphometric analysis revealed that Bio-Oss® and Bonefill® exhibited greater new bone formation compared to GenOx® and blood clots after 8 and 12 weeks [68]. Conversely, in a recent study utilizing the rat calvaria model to compare Bio-Oss® and Bonefill® with blood clots, no significant differences were observed between the two bone substitutes and the control group without bone substitutes [69]. Another investigation in the rabbit calvaria model compared Laddec® (BioHorizons, Birmingham, AL, USA) with Bio-Oss® for the augmentation of critical 8 mm defects. Both materials demonstrated comparable and complete defect regeneration with slow resorption rates at 4 and 8 weeks, with Bio-Oss® augmented defects exhibiting less soft tissue migration [70]. A study investigated the characteristics of different particulate bovine BS using a minipig model with bilaterally induced mandibular bony defects (total n = 72). The study group design comprised a control group without BS, low-temperature treated BS (Bio-Oss®), and high-temperature treated BS (cerabone®), both combined with a porcine pericardium membrane. Harvesting and micro-CT analysis was conducted at 4-, 8-, and 12-weeks post-implantation. No volumetric differences were observed among the groups after 4 weeks. However, at 8 and 12 weeks, the control group and cerabone® exhibited a significantly higher percentage of new bone formation compared to Bio-Oss® [71]. In another study, the same BS (Bio-Oss® and cerabone®) were compared for sinus floor augmentation in rabbits. Histometric and micro-CT analyses indicated that both biomaterials facilitated bone growth within the elevated space, with no significant differences observed between the two BS. Consequently, the authors concluded that both biomaterials are equally suitable for sinus floor augmentation [72]. Subsequently, critical-sized alveolar ridge defects in canines (n = 27 animals, total n = 54 defects) were filled with either InterOss® (SigmaGraft biomaterials, Fullerton, CA, USA) or Bio-Oss® (both low-temperature treated), while empty, non-filled defects served as controls. Data analysis was conducted at 4-, 8-, and 12-weeks post-implantation. No significant differences were observed between the experimental groups regarding graft resorption, bony integration, percentage of mineralized bone volume, and density based on radiographic analysis. Histologic examination similarly revealed no discernible differences between the two groups, although there was a non-significant trend towards increased bone formation for InterOss® compared to Bio-Oss® after 8 and 12 weeks [73]. In another study, bone level tapered implants (BLT) were inserted into the mandibles of 10 minipigs, where circumferential defects measuring 4 mm in depth and 2 mm in width were created around the implants. These defects were filled with particulate bovine BS (cerabone®, Bio-Oss®). Harvesting and data analysis were conducted at 8- and 12-weeks post-implantation. No significant differences were detected regarding new bone formation, bone substitute resorption, or bone-implant contacts, with similar outcomes observed across both groups [63]. In a separate investigation, alveolar defects were induced in 6 beagles and filled with either InterOss® or A-Oss® (Osstem Implant, Seoul, Korea; both low-temperature treated) using GBR four weeks post-defect creation. Both BS resulted in new bone formation, with no significant disparities observed in histological, histomorphometric, and volumetric analyses [74].
In summary, pre-clinical in vivo data failed to elucidate substantial variances between the various particulate bovine BS. However, a subtle tendency towards variances in new bone formation between low- and high-temperature treated bovine BS was observed across distinct healing intervals, with potential slight benefits favoring high-temperature treated bovine BS after 2–3 months.
Clinical studies
Particulate bovine bone substitutes for ridge preservation
In the context of ridge preservation, a prospective, single-center randomized study compared two bovine BS (Bio-Oss®; Endobon®, Zimmer Biomet, Warsaw, Indiana, USA) when applied with a resorbable membrane. This study involved 60 patients and 40 extraction sites, with 20 sites allocated to each bovine BS. Histological analysis was performed after 4 months, coinciding with implant placement. The results indicated no differences in new bone formation between the two tested particulate bovine BS. There were no significant differences in implant survival rate, which was 100% for Bio-Oss® and 95% for Endobon® after 24 months follow-up [75]. Furthermore, a multicenter prospective randomized controlled trial (RCT) compared two different particulate bovine BS, one high-temperature treated (Endobon®) and the other low-temperature treated BS (Bio-Oss®), for ridge preservation. The study involved 38 patients and a total of 62 augmented extraction sites. Defects were covered with resorbable collagen membranes, and re-evaluation occurred after 6 months in conjunction with implant placement. Histologic evaluations were performed for data analysis, revealing similar outcomes between the two bovine BS, with comparable levels of new bone formation (28.5 ± 20% and 31.4 ± 18%) [76]. In a RCT by Shakibaie et al., Bio-Oss® and cerabone® were compared at 20 adjacent extraction sites in 10 patients. Successful implant therapy was achieved at all extraction sites, regardless of the BS. However, the Bio-Oss® group exhibited superior outcomes in terms of crestal gingival healing process (CGHP), mean transversal crestal ridge resorption (MTRR), and mean implant primary stability (MIPS) [77].
In summary, the existing data do not suggest significant differences regarding the efficacy of different particulate bovine BS for ridge preservation. A RCT showed marginal benefits of low-temperature treated bovine BS over high-temperature treated counterparts in ridge preservation, specifically in crestal gingival healing, transversal crestal ridge resorption, and primary implant stability. However, the available data are inadequate to support an evidence-based conclusion.
Particulate bovine bone substitutes for sinus floor elevation
Peric Kacarevic et al. synthesized bone formation rates observed in elevated sinuses from clinical studies, which, in line with preclinical analyses, exhibited similarity between the included bovine BS (Bio-Oss® and cerabone®) [43]. However, only two clinical trials investigated two different bovine BS (Bio-Oss® and cerabone®) for sinus floor elevation over 8 months and 4 years. One of these studies reported a significantly higher radiographically determined volume loss after four years with Bio-Oss® compared to cerabone® (33.4 ± 3.1% and 23.4 ± 3.6%, respectively). Another study demonstrated an increased rate of new bone formation for cerabone® (29.13%) compared to Bio-Oss® (24.63%) [43, 57, 62]. Additionally, another study analyzed the osteoconductivity index (OI) of Bio-Oss® and cerabone® through histological examination and micro-CT scans, quantifying the contact length between the particulate bovine BS and the newly formed bone as a percentage. Twenty patients underwent sinus floor elevation, with the resultant voids filled using either cerabone® or Bio-Oss®. Biopsies were obtained after 5 months in conjunction with implant placement. Micro-CT scans revealed comparable OI between the two groups (cerabone®: 92.72 ± 8.77%, Bio-Oss®: 88.84 ± 8.81%). Regarding tissue distribution assessed via micro-CT scans, no significant differences were observed. Cerabone® exhibited increased bone tissue (50.12 ± 10.97%), decreased substitute remnants (16.12 ± 10.11%), and less connective tissue (33.77 ± 10.81%) compared to Bio-Oss® (44.02 ± 10.48%, 18.06 ± 12.53%, 37.92 ± 8.28%, respectively). Histologically, cerabone® displayed decreased bone tissue (20.4 ± 8.22%), increased substitute remnants (29.82 ± 11.75%), and less connective tissue (49.78 ± 10.37%) compared to Bio-Oss® (23.95 ± 8.89%, 23.47 ± 8.26%, 52.57 ± 3.89%, respectively), albeit without statistical significance [46]. A comparative study assessed sinus floor elevation using Bio-Oss® and Lumina-Bone Porous® (Criteria Biomateriais, São Paulo, Brazil) in a split-mouth model involving 13 patients. Lumina-Bone Porous® is a xenogeneic BS processed without high temperatures and undergoes chemical sterilization instead. Clinical, radiological, and histological evaluations were conducted. Both bovine BS induced significant bone gain in elevated sinuses after 6 months compared to baseline. Histologically, no significant differences in newly formed bone were observed between the two particulate bovine BS. However, Bio-Oss® exhibited significantly more residual BS material [78]. In another study, the efficacy of Biocera® (Oscotec Inc., Gyeongi, Korea) and Bio-Oss® for sinus floor elevation was compared in five patients with elevation procedures performed on both maxillary sinuses. Histological assessment was carried out after 6 to 8 months. Results revealed minimal, non-significant differences in new bone formation between Bio-Oss® (28.46 ± 5.28%) and Biocera® (29.94 ± 8.72%) [79]. A prospective study examined histological aspects of new bone formation following sinus floor elevation using Bio-Oss® and cerabone®. The study enrolled 22 patients with approximately 3 mm residual bone height who underwent two-stage implant placements. Histological analysis after 6 months revealed no differences between new bone formation and residual BS material [40]. In a RCT, a comparison was made between a high-temperature treated particulate bovine BS (Alpha Bio’s Graft®, a private label of cerabone®, botiss biomaterials GmbH, Zossen, Germany) and a low-temperature treated one (Bio-Oss®) for sinus floor elevation. After 6 months, similar augmentation heights (> 95%) and percentages of new bone (> 30%) were observed, with a slightly reduced amount of residual bone in the high-temperature treated group (40.68 ± 16.32%) compared to the low-temperature treated group (43.43 ± 19.07%). However, the differences were not significant [80]. Canellas et al. conducted a systematic review and meta-analysis to evaluate various xenogeneic BS for sinus floor elevation. Eleven studies were included in the analysis, focusing on histological assessments of newly formed bone and graft residues. Among the comparisons involving particulate bovine BS, Bio-Oss® exhibited significantly higher graft residues compared to Lumina-Bone Porous® (Criteria Biomateriais, São Paulo, Brazil) (19.9% vs. 14.6%, p = 0.015) The survival rate of dental implants for augmented area with Lumina Bone Porous® was 88.88%, while for Bio-Oss® group was 100% at 3-year follow-up after final prosthetic restoration [78]. No significant differences were found between Bio-Oss® and InduCera® Dual Coat (Oscotec Inc., Bundang-gu, Seongnam, Gyeonggi-do, South Korea) [81]. Similarly, no significant differences were observed when comparing Osseous® (Sistema de Implantes Nacional, São Paulo, Brazil) and Bio-Oss®, either in newly formed bone or graft residues [82, 83]. In a retrospective study, 36 patients with a ridge height of less than 4 mm in the posterior maxilla underwent sinus floor elevation using three different BS: Bio-Oss®, cerabone®, and Ti-Oss® (Chiyewon, Gyeonggido, South Korea). Biopsies were obtained for histological and histomorphometric analysis at six months postoperatively, and volumetric measurements were conducted one week and six months post-surgery. The Ti-Oss® group exhibited inferior outcomes compared to the Bio-Oss® and cerabone® groups, displaying significantly higher levels of bone resorption and less new bone formation. Additionally, all groups experienced a significant reduction in graft volume between one week and six months post-surgery [84]. Hieu et al. radiographically compared the height of the Bio-Oss® and OCS-B® (Nibec, Seoul, Korea) graft materials after sinus floor elevation and found that a smaller amount of Bio-Oss® maintained greater absolute volume over time compared to OCS-B®. There was no significant change in the Bio-Oss® group, while the OCS-B® group showed a significant decrease in bone height up to a follow-up period of 25 months, with no significant differences found when comparing both BS [85]. Figures 1, 2 and 3 present histological sections from biopsies after sinus floor elevations with three different bovine BS after healing times ranging from 5 to 8 months.
Histological sections (H&E-stained) 5–8 months after sinus floor elevation with a low-temperature treated bovine BS (Bio-Oss®). (A) Early osteogenesis around bone substitute (BS) granules forming woven bone (b), ct = connective tissue, black arrows = osteoblasts; original magnification (o.m.) 20-fold. (B) Advanced osteogenesis around BS residual granules, b = newly formed woven bone, ct = connective tissue; o.m. 20-fold
Histological sections (H&E-stained) 5–8 months after sinus floor elevation with a high-temperature treated bovine BS (cerabone®). (A) Early osteogenesis around bone substitute (BS) granules forming woven bone (b), granules mostly lost due to decalcification, ct = highly vascularized connective tissue, v = vessels; original magnification (o.m.) 10-fold. (B) Advanced osteogenesis around BS granules forming woven bone (b) partly remodeling into lamellar bone, granules mostly lost due to decalcification, ct = connective tissue; o.m. 10-fold
Histological sections (H&E-stained) 5–8 months after sinus floor elevation with a bovine BS (MinerOss®). (A) Early osteogenesis around cluster of small bone substitute (BS) granules forming woven bone (b), ct = connective tissue; original magnification (o.m.) 10-fold. (B) Advanced osteogenesis around larger BS granules forming woven bone (b), ct = connective tissue; o.m. 10-fold
In summary, the data gleaned from individual clinical studies indicate subtle clinical distinctions among various particulate bovine BS for sinus floor elevation in certain aspects. In brief, low-temperature treated BS tented to an increased long-time bone volume loss. High-temperature-treated BS seemed to improve new bone formation and decrease the amount of connective tissue. The potential differences between bovine-derived BS are only evident or by trend in individual studies and do not permit evidence-based conclusions.
Particulate bovine bone substitutes for peri-implant defects
In a comparative study, EndoBon® and Bio-Oss® were evaluated for filling peri-implant defects in 24 patients diagnosed with peri-implantitis. Various parameters, including bone level, intrabony defect depth, probing depth, bleeding on probing, and suppuration on probing, were assessed at 6- and 12-months post-treatment. Both bovine BS significantly improved all measured parameters at both time points. However, no significant differences were observed between the two groups for any parameter at any time point [86].
The available data does not suggest relevant differences between different particulate bovine BS for treating peri-implant defects. An evidence-based assessment is not possible due to the available data.
Particulate bovine bone substitutes for lateral and vertical ridge augmentation
Lim et al. conducted a comparative study to evaluate two low-temperature treated bovine BS, Bio-Oss® and A-Oss® (Osstem Implant, Prague, Czechia) for lateral augmentation during simultaneous implant insertion. The study included eight patients in each group. Implants were placed concurrently with the augmentation using a double-layer technique involving internal allograft and external xenogeneic BS, covered by a preformed ultrafine titanium mesh and a resorbable collagen membrane. All implants were successfully prosthetically treated. After a twelve-month follow-up period, both groups exhibited graft volume shrinkage, with a reduction of 46% in the Bio-Oss® group and 40.8% in the A-Oss® group. However, no significant differences were observed in graft volume changes over time or in bone density between the two groups [87].
The available data does not suggest relevant differences between different particulate bovine BS for lateral and vertical ridge augmentation. Due to the current state of available data, a definitive evidence-based assessment is unfeasible.
Particulate bovine bone substitutes for titanium mesh filling
No studies were found comparing different particulate bovine BS for titanium mesh filling.
Conclusions
This narrative review identified a shortage of data directly comparing various particulate bovine BS in oral regeneration. Regarding preclinical data, high-temperature treated particulate bovine BS may offer slight advantages, such as enhanced in vitro biocompatibility compared to low-temperature treated counterparts. Regarding sinus floor elevation, there is a trend towards small benefits with high-temperature treated particulate bovine BS regarding volume loss, new bone formation and the amount of connective tissue. It warrants acknowledgment that pivotal clinical metrics including implant survival, implant success, and ridge volume preservation frequently remain unexplored within existing literature. While many publications focus on the assessment of newly formed bone, an indispensable aspect, such analysis alone fails to comprehensively evaluate the clinical efficacy of BS. No significant differences were noted for other clinical indications, and no specific recommendations favoring specific particulate bovine BS could be made. Further clinical investigations are urgently required to address this data gap and compare different particulate bovine BS across various clinical indications.
Data availability
No datasets were generated or analysed during the current study.
References
Alghamdi HS, Jansen JA. The development and future of dental implants. Dent Mater J. 2020;39(2):167–72.
Chrcanovic BR, Albrektsson T, Wennerberg A. Bone Quality and Quantity and Dental Implant failure: a systematic review and Meta-analysis. Int J Prosthodont. 2017;30(3):219–37.
Poli PP, Beretta M, Cicciù M, Maiorana C. Alveolar ridge augmentation with titanium mesh. A retrospective clinical study. Open Dent J. 2014;8:148–58.
Hong CE, Lee JY, Choi J, Joo JY. Prediction of the alveolar bone level after the extraction of maxillary anterior teeth with severe periodontitis. J Periodontal Implant Sci. 2015;45(6):216–22.
Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restor Dent. 2003;23(4):313–23.
Carlsson GE, Bergman B, Hedegard B. Changes in contour of the maxillary alveolar process under immediate dentures. A longitudinal clinical and x-ray cephalometric study covering 5 years. Acta Odontol Scand. 1967;25(1):45–75.
Sanz M, Vignoletti F. Key aspects on the use of bone substitutes for bone regeneration of edentulous ridges. Dent Mater. 2015;31(6):640–7.
Kämmerer P, Buttchereit I, Pabst A. Allogener Knochen - Knochenersatzmaterial oder Ersatz für autologe Transplantate?.
Avila-Ortiz G, Chambrone L, Vignoletti F. Effect of alveolar ridge preservation interventions following tooth extraction: a systematic review and meta-analysis. J Clin Periodontol. 2019;46(Suppl 21):195–223.
Avila-Ortiz G, Elangovan S, Kramer KW, Blanchette D, Dawson DV. Effect of alveolar ridge preservation after tooth extraction: a systematic review and meta-analysis. J Dent Res. 2014;93(10):950–8.
Kämmerer PW, Al-Nawas B. Bone reconstruction of extensive maxillomandibular defects in adults. Periodontol 2000. 2023;93(1):340–57.
Dau M, Kämmerer PW. Kurze Implantate vs. Augmentation Der Junge Zahnarzt. 2017;2:15–24.
Torres-Alemany A, Fernández-Estevan L, Agustín-Panadero R, Montiel-Company JM, Labaig-Rueda C, Mañes-Ferrer JF. Clinical behavior of short Dental implants: systematic review and Meta-analysis. J Clin Med. 2020;9(10).
Sohrabi K, Mushantat A, Esfandiari S, Feine J. How successful are small-diameter implants? A literature review. Clin Oral Implants Res. 2012;23(5):515–25.
Ladha K, Sharma A, Tiwari B, Bukya DN. Bone augmentation as an adjunct to dental implant rehabilitation in patients with diabetes mellitus: a review of literature. Natl J Maxillofac Surg. 2017;8(2):95–101.
Baldini N, De Sanctis M, Ferrari M. Deproteinized bovine bone in periodontal and implant surgery. Dent Mater. 2011;27(1):61–70.
Chavda S, Levin L. Human studies of Vertical and Horizontal Alveolar Ridge Augmentation comparing different types of bone graft materials: a systematic review. J Oral Implantol. 2018;44(1):74–84.
Kloss FR, Offermanns V, Kloss-Brandstätter A. Comparison of allogeneic and autogenous bone grafts for augmentation of alveolar ridge defects-A 12-month retrospective radiographic evaluation. Clin Oral Implants Res. 2018;29(11):1163–75.
Silva FM, Cortez AL, Moreira RW, Mazzonetto R. Complications of intraoral donor site for bone grafting prior to implant placement. Implant Dent. 2006;15(4):420–6.
Kämmerer PW, Heimes D, Hartmann A, Kesting M, Khoury F, Schiegnitz E et al. Clinical insights into traumatic Injury of the Inferior Alveolar and Ligual nerves: a Comprehensive Approach from diagnosis to therapeutic interventions. Clin Oral Invest. 2024.
Heimes D, Pabst A, Becker P, Hartmann A, Kloss F, Tunkel J, et al. Comparison of morbidity-related parameters between autologous and allogeneic bone grafts for alveolar ridge augmentation from patients’ perspective – a questionnaire-based cohort study. Clin Implant Dent Relat Res. 2024;26(1):170–82.
Troeltzsch M, Troeltzsch M, Kauffmann P, Gruber R, Brockmeyer P, Moser N, et al. Clinical efficacy of grafting materials in alveolar ridge augmentation: a systematic review. J Craniomaxillofac Surg. 2016;44(10):1618–29.
Qian SJ, Mo JJ, Si MS, Qiao SC, Shi JY, Lai HC. Long-term outcomes of osteotome sinus floor elevation with or without bone grafting: the 10-year results of a randomized controlled trial. J Clin Periodontol. 2020;47(8):1016–25.
Urban IA, Ravidà A, Saleh MHA, Galli M, Lozada J, Farkasdi S, et al. Long-term crestal bone changes in implants placed in augmented sinuses with minimal or moderate remaining alveolar bone: a 10-year retrospective case-series study. Clin Oral Implants Res. 2021;32(1):60–74.
Campana V, Milano G, Pagano E, Barba M, Cicione C, Salonna G, et al. Bone substitutes in orthopaedic surgery: from basic science to clinical practice. J Mater Sci Mater Med. 2014;25(10):2445–61.
Blatt S, Thiem DGE, Kyyak S, Pabst A, Al-Nawas B, Kämmerer PW. Possible implications for Improved Osteogenesis? The combination of platelet-rich fibrin with different bone substitute materials. Front Bioeng Biotechnol. 2021;9:640053.
Kämmerer PW, Schiegnitz E, Alshihri A, Draenert FG, Wagner W. Modification of xenogenic bone substitute materials–effects on the early healing cascade in vitro. Clin Oral Implants Res. 2014;25(7):852–8.
Kyyak S, Blatt S, Pabst A, Thiem D, Al-Nawas B, Kämmerer PW. Combination of an allogenic and a xenogenic bone substitute material with injectable platelet-rich fibrin - A comparative in vitro study. J Biomater Appl. 2020;35(1):83–96.
Kyyak S, Blatt S, Schiegnitz E, Heimes D, Staedt H, Thiem DGE, et al. Activation of human osteoblasts via different bovine bone substitute materials with and without Injectable platelet Rich Fibrin in vitro. Front Bioeng Biotechnol. 2021;9:599224.
Kyyak S, Pabst A, Heimes D, Kämmerer PW. The influence of Hyaluronic Acid Biofunctionalization of a bovine bone substitute on osteoblast activity in Vitro. Mater (Basel). 2021;14(11).
Schorn L, Fienitz T, De Donno F, Sterner-Kock A, Maul AC, Holtmann H, et al. Critical-size defect augmentation using sintered and non-sintered bovine bone matrix - an experimental controlled study in Minipigs. J Oral Maxillofac Surg. 2021;79(9):1866–73.
Song YW, Jung HJ, An YZ, Jung UW, Lee JS. Addition of autogenous bone chips to deproteinized bovine bone mineral does not have additional benefit in lateral ridge augmentation-A preclinical in vivo experimental study. Clin Oral Implants Res. 2021;32(9):1105–14.
Al-Nawas B, Schiegnitz E. Augmentation procedures using bone substitute materials or autogenous bone - a systematic review and meta-analysis. Eur J Oral Implantol. 2014;7(Suppl 2):S219–34.
Barootchi S, Tavelli L, Majzoub J, Stefanini M, Wang HL, Avila-Ortiz G. Alveolar ridge preservation: complications and cost-effectiveness. Periodontol 2000. 2023;92(1):235–62.
Mardas N, Macbeth N, Donos N, Jung RE, Zuercher AN. Is alveolar ridge preservation an overtreatment? Periodontol 2000. 2023;93(1):289–308.
Klein MO, Kämmerer PW, Götz H, Duschner H, Wagner W. Long-term bony integration and resorption kinetics of a xenogeneic bone substitute after sinus floor augmentation: histomorphometric analyses of human biopsy specimens. Int J Periodontics Restor Dent. 2013;33(4):e101–10.
Benke D, Olah A, Möhler H. Protein-chemical analysis of Bio-oss bone substitute and evidence on its carbonate content. Biomaterials. 2001;22(9):1005–12.
Miron RJ, Sculean A, Cochran DL, Froum S, Zucchelli G, Nemcovsky C, et al. Twenty years of enamel matrix derivative: the past, the present and the future. J Clin Periodontol. 2016;43(8):668–83.
Pardiñas López S, Froum S, Khouly I. Histomorphometric analysis of a Biopsy harvested 10 years after maxillary sinus augmentation with anorganic bovine bone matrix and plasma Rich in Growth factors: a Case Report. Implant Dent. 2015;24(4):480–6.
Mahesh L, Mascarenhas G, Bhasin MT, Guirado C, Juneja S. Histological evaluation of two different anorganic bovine bone matrixes in lateral wall sinus elevation procedure: a retrospective study. Natl J Maxillofac Surg. 2020;11(2):258–62.
Amid R, Kheiri A, Kheiri L, Kadkhodazadeh M, Ekhlasmandkermani M. Structural and chemical features of xenograft bone substitutes: a systematic review of in vitro studies. Biotechnol Appl Biochem. 2021;68(6):1432–52.
Barbeck M, Udeabor S, Lorenz J, Schlee M, Holthaus MG, Raetscho N, et al. High-temperature sintering of Xenogeneic Bone substitutes leads to increased Multinucleated Giant cell formation: in vivo and preliminary clinical results. J Oral Implantol. 2015;41(5):e212–22.
Peric Kacarevic Z, Kavehei F, Houshmand A, Franke J, Smeets R, Rimashevskiy D, et al. Purification processes of xenogeneic bone substitutes and their impact on tissue reactions and regeneration. Int J Artif Organs. 2018;41(11):789–800.
Barbeck M, Dard M, Kokkinopoulou M, Markl J, Booms P, Sader RA, et al. Small-sized granules of biphasic bone substitutes support fast implant bed vascularization. Biomatter. 2015;5:e1056943.
Wenz B, Oesch B, Horst M. Analysis of the risk of transmitting bovine spongiform encephalopathy through bone grafts derived from bovine bone. Biomaterials. 2001;22(12):1599–606.
Kapogianni E, Barbeck M, Jung O, Arslan A, Kuhnel L, Xiong X, et al. Comparison of material-mediated bone regeneration capacities of Sintered and non-sintered xenogeneic bone substitutes via 2D and 3D data. Vivo. 2019;33(6):2169–79.
22442-1 EI. EU-guidelines for medical devices utilizing animal tissues their derivatives – part 1: application of risk management. 2015.
Taylor DM, Fraser H, McConnell I, Brown DA, Brown KL, Lamza KA, et al. Decontamination studies with the agents of bovine spongiform encephalopathy and scrapie. Arch Virol. 1994;139(3–4):313–26.
Walker AS, Inderlied CB, Kingsbury DT. Conditions for the chemical and physical inactivation of the K. Fu. Strain of the agent of Creutzfeldt-Jakob disease. Am J Public Health. 1983;73(6):661–5.
Schwartz Z, Weesner T, van Dijk S, Cochran DL, Mellonig JT, Lohmann CH, et al. Ability of deproteinized cancellous bovine bone to induce new bone formation. J Periodontol. 2000;71(8):1258–69.
Tadic D, Epple M. A thorough physicochemical characterisation of 14 calcium phosphate-based bone substitution materials in comparison to natural bone. Biomaterials. 2004;25(6):987–94.
Kim Y, Nowzari H, Rich SK. Risk of prion disease transmission through bovine-derived bone substitutes: a systematic review. Clin Implant Dent Relat Res. 2013;15(5):645–53.
Berberi A, Samarani A, Nader N, Noujeim Z, Dagher M, Kanj W, et al. Physicochemical characteristics of bone substitutes used in oral surgery in comparison to autogenous bone. Biomed Res Int. 2014;2014:320790.
Barbeck M, Booms P, Unger R, Hoffmann V, Sader R, Kirkpatrick CJ, et al. Multinucleated giant cells in the implant bed of bone substitutes are foreign body giant cells-new insights into the material-mediated healing process. J Biomed Mater Res A. 2017;105(4):1105–11.
Weibrich G, Trettin R, Gnoth SH, Götz H, Duschner H, Wagner W. [Determining the size of the specific surface of bone substitutes with gas adsorption]. Mund Kiefer Gesichtschir. 2000;4(3):148–52.
Trajkovski B, Jaunich M, Müller WD, Beuer F, Zafiropoulos GG, Houshmand A, Hydrophilicity. Viscoelastic, and Physicochemical Properties Variations in Dental Bone Grafting substitutes. Mater (Basel). 2018;11(2).
Riachi F, Naaman N, Tabarani C, Aboelsaad N, Aboushelib MN, Berberi A, et al. Influence of material properties on rate of resorption of two bone graft materials after sinus lift using radiographic assessment. Int J Dent. 2012;2012:737262.
Sartori S, Silvestri M, Forni F, Icaro Cornaglia A, Tesei P, Cattaneo V. Ten-year follow-up in a maxillary sinus augmentation using anorganic bovine bone (Bio-Oss). A case report with histomorphometric evaluation. Clin Oral Implants Res. 2003;14(3):369–72.
Tadjoedin ES, de Lange GL, Bronckers AL, Lyaruu DM, Burger EH. Deproteinized cancellous bovine bone (Bio-Oss) as bone substitute for sinus floor elevation. A retrospective, histomorphometrical study of five cases. J Clin Periodontol. 2003;30(3):261–70.
Piattelli M, Favero GA, Scarano A, Orsini G, Piattelli A. Bone reactions to anorganic bovine bone (Bio-Oss) used in sinus augmentation procedures: a histologic long-term report of 20 cases in humans. Int J Oral Maxillofac Implants. 1999;14(6):835–40.
Tawil G, Barbeck M, Unger R, Tawil P, Witte F. Sinus floor elevation using the lateral Approach and Window Repositioning and a xenogeneic bone substitute as a Grafting Material: a histologic, histomorphometric, and Radiographic Analysis. Int J Oral Maxillofac Implants. 2018;33(5):1089–96.
Panagiotou D, Ozkan Karaca E, Dirikan Ipci S, Cakar G, Olgac V, Yilmaz S. Comparison of two different xenografts in bilateral sinus augmentation: radiographic and histologic findings. Quintessence Int. 2015;46(7):611–9.
Catros S, Sandgren R, Pippenger BE, Fricain JC, Herber V, El Chaar E. A Novel Xenograft Bone Substitute supports stable bone formation in Circumferential defects around Dental implants in Minipigs. Int J Oral Maxillofac Implants. 2020;35(6):1122–31.
Kübler A, Neugebauer J, Oh JH, Scheer M, Zöller JE. Growth and proliferation of human osteoblasts on different bone graft substitutes: an in vitro study. Implant Dent. 2004;13(2):171–9.
Xu AT, Qi WT, Lin MN, Zhu YH, He FM. The optimization of sintering treatment on bovine-derived bone grafts for bone regeneration: in vitro and in vivo evaluation. J Biomed Mater Res B Appl Biomater. 2020;108(1):272–81.
Ortiz-Puigpelat O, Simões A, Caballé-Serrano J, Hernández-Alfaro F. Blood absorption capacity of different xenograft bone substitutes. An in-vitro study. J Clin Exp Dent. 2019;11(11):e1018–24.
Daculsi G, Corre P, Malard O, Legeros R. Performance of bone ingrowth of biphasic calcium phosphate ceramic versus bovine bone substitute. Key Eng Mat. 2006;18:1379–82.
Manfro R, Fonseca FS, Bortoluzzi MC, Sendyk WR. Comparative, histological and histomorphometric analysis of three anorganic bovine xenogenous bone Substitutes: Bio-oss, Bone-Fill and Gen-Ox Anorganic. J Maxillofac Oral Surg. 2014;13(4):464–70.
Theodoro LH, Campista CCC, Bury LL, de Souza RGB, Muniz YS, Longo M, et al. Comparison of different bone substitutes in the repair of rat calvaria critical size defects: questioning the need for alveolar ridge presentation. Quintessence Int. 2024;0(0):0.
Gil LF, Nayak VV, Benalcázar Jalkh EB, Tovar N, Chiu KJ, Salas JC, et al. Laddec® versus Bio-Oss®: the effect on the healing of critical-sized defect - calvaria rabbit model. J Biomed Mater Res B Appl Biomater. 2022;110(12):2744–50.
Gomez J, Bergamo ET, Tovar N, Talib HS, Pippenger BE, Herdia V, et al. Microtomographic reconstruction of mandibular defects treated with xenografts and collagen-based membranes: a pre-clinical minipig model. Med Oral Patol Oral Cir Bucal. 2021;26(6):e825–33.
Ferreira Balan V, Botticelli D, Peñarrocha-Oltra D, Masuda K, Pires Godoy E, Xavier SP. Maxillary sinus floor augmentation with two different inorganic bovine bone grafts: an experimental study in rabbits. Chin J Dent Res. 2022;25(2):93–105.
Kim DM, Hong H, Lin JC, Nevins M. Evaluation of the bone-regenerating effects of two anorganic bovine bone grafts in a critical-sized Alveolar Ridge defect model. Int J Periodontics Restor Dent. 2017;37(4):e234–44.
Lee D, Lee Y, Kim S, Lee JT, Ahn JS. Evaluation of regeneration after the application of 2 types of deproteinized bovine bone mineral to alveolar bone defects in adult dogs. J Periodontal Implant Sci. 2022;52(5):370–82.
Sivolella S, Botticelli D, Prasad S, Ricci S, Bressan E, Prasad H. Evaluation and comparison of histologic changes and implant survival in extraction sites immediately grafted with two different xenografts: a randomized clinical pilot study. Clin Oral Implants Res. 2020;31(9):825–35.
Barone A, Todisco M, Ludovichetti M, Gualini F, Aggstaller H, Torrés-Lagares D, et al. A prospective, randomized, controlled, multicenter evaluation of extraction socket preservation comparing two bovine xenografts: clinical and histologic outcomes. Int J Periodontics Restor Dent. 2013;33(6):795–802.
Shakibaie B, Blatz MB, Sabri H, Jamnani ED, Barootchi S. Effectiveness of two differently processed bovine-derived xenografts for Alveolar Ridge Preservation with a minimally invasive tooth extraction Approach: a feasibility clinical trial. Int J Periodontics Restor Dent. 2023;43(5):540–9.
da Silva HF, Goulart DR, Sverzut AT, Olate S, de Moraes M. Comparison of two anorganic bovine bone in maxillary sinus lift: a split-mouth study with clinical, radiographical, and histomorphometrical analysis. Int J Implant Dent. 2020;6(1):17.
Moon JW, Sohn DS, Heo JU, Kim JS. Comparison of two kinds of bovine bone in maxillary sinus augmentation: a histomorphometric study. Implant Dent. 2015;24(1):19–24.
Fienitz T, Moses O, Klemm C, Happe A, Ferrari D, Kreppel M, et al. Histological and radiological evaluation of sintered and non-sintered deproteinized bovine bone substitute materials in sinus augmentation procedures. A prospective, randomized-controlled, clinical multicenter study. Clin Oral Investig. 2017;21(3):787–94.
Pang KM, Lee JK, Choi SH, Kim YK, Kim BJ, Lee JH. Maxillary sinus augmentation with calcium phosphate double-coated anorganic bovine bone: comparative Multicenter Randomized Clinical Trial with histological and radiographic evaluation. Implant Dent. 2019;28(1):39–45.
Canellas J, Drugos L, Ritto FG, Fischer RG, Medeiros PJD. Xenograft materials in maxillary sinus floor elevation surgery: a systematic review with network meta-analyses. Br J Oral Maxillofac Surg. 2021;59(7):742–51.
Calasans-Maia MD, Mourão CF, Alves AT, Sartoretto SC, de Uzeda MJ, Granjeiro JM. Maxillary sinus augmentation with a New Xenograft: a Randomized Controlled Clinical Trial. Clin Implant Dent Relat Res. 2015;17(Suppl 2):e586–93.
Cinar IC, Zboun M, Gultekin BA, Saglanmak A, Akay AS. Retrospective analysis of three different xenografts in maxillary sinus augmentation: histologic and three-dimensional radiologic study. Quintessence Int. 2023;54(8):640–9.
Hieu PD, Chung JH, Yim SB, Hong KS. A radiographical study on the changes in height of grafting materials after sinus lift: a comparison between two types of xenogenic materials. J Periodontal Implant Sci. 2010;40(1):25–32.
Polymeri A, Anssari-Moin D, van der Horst J, Wismeijer D, Laine ML, Loos BG. Surgical treatment of peri-implantitis defects with two different xenograft granules: a randomized clinical pilot study. Clin Oral Implants Res. 2020;31(11):1047–60.
Lim J, Jun SH, Tallarico M, Park JB, Park DH, Hwang KG et al. A randomized controlled trial of guided bone regeneration for Peri-implant Dehiscence defects with two anorganic bovine bone materials covered by Titanium Meshes. Mater (Basel). 2022;15(15).
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. No funding was received for this study. The study was neither commissioned nor conducted in cooperation with the German Armed Forces. The study does not reflect any opinion of the German Armed Forces.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
AP, PB, WG, and PWK performed the literature review. AP, PB, SB, WG, DH, DT, and PWK performed interpretation and critical discussion of the available data. AP, PB, and PWK wrote the manuscript. AP, PB, WG, DH, SB, DT, and PWK performed a critical revision of the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pabst, A., Becker, P., Götz, W. et al. A comparative analysis of particulate bovine bone substitutes for oral regeneration: a narrative review. Int J Implant Dent 10, 26 (2024). https://doi.org/10.1186/s40729-024-00544-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40729-024-00544-z