Abstract
Purpose
To investigate the influence of teeth and dental restorations on the facial skeleton's gray value distributions in cone-beam computed tomography (CBCT).
Methods
Gray value selection for the upper and lower jaw segmentation was performed in 40 patients. In total, CBCT data of 20 maxillae and 20 mandibles, ten partial edentulous and ten fully edentulous in each jaw, respectively, were evaluated using two different gray value selection procedures: manual lower threshold selection and automated lower threshold selection. Two sample t tests, linear regression models, linear mixed models, and Pearson's correlation coefficients were computed to evaluate the influence of teeth, dental restorations, and threshold selection procedures on gray value distributions.
Results
Manual threshold selection resulted in significantly different gray values in the fully and partially edentulous mandible. (p = 0.015, difference 123). In automated threshold selection, only tendencies to different gray values in fully edentulous compared to partially edentulous jaws were observed (difference: 58–75). Significantly different gray values were evaluated for threshold selection approaches, independent of the dental situation of the analyzed jaw. No significant correlation between the number of teeth and gray values was assessed, but a trend towards higher gray values in patients with more teeth was noted.
Conclusions
Standard gray values derived from CT imaging do not apply for threshold-based bone segmentation in CBCT. Teeth influence gray values and segmentation results. Inaccurate bone segmentation may result in ill-fitting surgical guides produced on CBCT data and misinterpreting bone density, which is crucial for selecting surgical protocols.
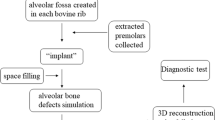
Graphical Abstract

Created with BioRender.com
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Cone-beam computed tomography (CBCT) is dentistry’s most commonly used tool for three-dimensional display of the facial skeleton [1] In implant dentistry and craniomaxillofacial surgery, CBCT plays a significant role in preoperative planning, visualization, assessment of bony structures, and surgical guide generation [2, 3].
For the computer-assisted visualization of anatomy and the design and preoperative production of surgical tools (e.g., drill guides), CBCT data are used in conjunction with specific software. It is used for preoperative visualization and treatment planning, virtual surgery, and CAD/CAM (computer-aided design/computer-aided manufacturing) guides for resection and reconstruction [4].
Medical image data typically are two- or three-dimensional regular scalar fields, where each scalar value is represented by a picture/volume element (pixel/voxel). Each volume element (voxel) has a specific gray value, representing the tissue density it captures. In CT imaging, such scalar values represent radiodensity measured in Hounsfield Units (HU). Based on these values, tissues of different radiopacity can be discriminated. A three-dimensional representation of the imaged volume is visualized by selecting a range of gray values/HU. Only voxels in that particular range and specific anatomical structures (e.g., bone) are displayed by choosing an upper and a lower threshold for gray values [5]. The procedure of assigning a label to particular structures is defined as binary segmentation. The respective segment of the data volume can be converted into a surface representation by extracting the boundaries of the segment via triangulation [6]. Such a surface model is often used for treatment planning [7].
The more contrast an image displays, the easier is the segmentation of anatomical structures, whereas minor differences in density among adjacent structures complicate segmentation. A large variety of factors such as tube voltage, tube current, detector type, voxel size, the field of view (FOV), and reconstruction algorithm, respectively, may cause a shift of density values of the complete volume in either direction [8]. Furthermore, image artifacts in the form of noise, scatter, extinction, beam hardening, exponential edge gradient effect, aliasing, ring artifacts, and moving artifacts result in density values not correlating with anatomical structures. [9] Default values transferred from CT imaging may not apply to CBCT [10,11,12]. A transfer of gray values into pseudo-Hounsfield units was proposed. However, the diagnostic capacity of this procedure for clinical image data is missing [12]. The most commonly used segmentation algorithms in clinical routine are semi-automatic, with a standard upper and lower threshold for gray values (global thresholding) and a user's input for surface model generation [13, 14].
In a literature review by van Eijnatten et al., a trained clinician's global thresholding with laborious post-processing showed the highest accuracy [13]. Due to the remaining inaccuracies, more advanced techniques have been developed to gain accurate segmentations without manual post-processing. Fully automated segmentation algorithms provide comparable results to trained clinicians using a defined gray value range and automated threshold selection [15, 16]. These techniques, however, have not been implemented in commercially available clinical treatment planning software [13].
The accuracy of the segmented bone surface is crucial for the fit of a drill guide and the transfer of a virtually planned surgery to the intraoperative site [17,18,19,20]. The potential error introduced by bone segmentation and surface reconstruction could lead to a poor fit of the drill guide and consecutive harm to vital anatomical structures or a misinterpretation of the bone density, resulting in an inappropriate drilling protocol and consecutive missing primary stability of dental implants. Whereby the influence of dental implants on gray values in CBCT is widely known and studied, to the best of our knowledge, there is no study evaluating the impact of teeth with dental restorations on the resulting distribution of gray values in CBCT images and thereby, surface geometry resulting from segmentation and surface reconstruction [21,22,23]. Existing teeth may influence the overall gray value distribution in the data set by adding a diverse number of gray values, representing enamel, dentin, and dental restorations, which may lead to a shift in the constitution of the data set.
This study aimed to compare different bone segmentation thresholds from different methods in fully and partially edentulous patients to investigate if present teeth with dental restorations influence gray value distribution and, therefore, the geometry of surface models resulting from segmentation.
The study's primary outcome is to determine whether the grey value distribution in CBCT is influenced by the presence of teeth with dental restorations or other foreign bodies (e.g., radiographic stents). The secondary outcome is the impact of manual and automated threshold selection on segmentation. The study aims to evaluate whether there is a statistically significant difference in grey values between CBCT scans with and without teeth or foreign bodies and assess these structures' impact on bone segmentation.
The study aims to test the null hypothesis that teeth or other foreign bodies do not influence the grey value distribution in CBCT.
Materials and methods
Data set selection
The study protocol complied with the STROBE guidelines and was approved by the Ethics Committee of the Charité—Universitätsmedizin Berlin, Germany (EA4/111/21). It conforms to the Declaration of Helsinki and the European Medicines Agency Guidelines for Good Clinical Practice. Forty CBCT data sets of partially and fully edentulous jaws acquired between January 2018 and February 2021 for dental implant planning were selected. (Fig. 1) Thereof, twenty upper and twenty lower jaws, ten edentulous and ten partially edentulous jaws, respectively. Partially edentulous jaws were assigned to Kennedy classes 1 and 2, and the number of remaining teeth and dental restorations were recorded, regardless of their size. All CBCT scans were standardized using ProMax 3D Max, Pro Face Med Series H23 120 kV (SCS Sophisticated Computer tomographic Solutions GmbH, Aschaffenburg, Germany) with 120 kV tube voltage and 5 mA tube current, isotropic voxel size of 0.2 mm, bit depth 16 using a Field of View of 20 × 10 cm and exported in DICOM format.
Case series of a bone-supported surgical guide, designed and fabricated using CBCT. Outline of the surgical guide and CBCT in sagittal (a), axial (b), and coronal (c) plane. Mandibular segmentation with prosthetic setup (d), implant position (e), and 3D surgical guide (f). Clinical images of implant placement with the surgical guide in situ (g), drilled implant positions with direction markers (h), and implants in situ (i)
Segmentation procedure
Bone segmentation was performed with manual threshold selection, automated threshold selection of the complete data set, and automated threshold selection of the region of interest, respectively, using Amira ZIBEdition (Version 2021.27, https://amira.zib.de/). All segmentations were performed on a reporting monitor (MX217-HB, EIZO Europe GmbH, Germany) under the same lighting conditions (RK 5 due to DIN 6868-157) by the same investigator (OW) after calibration for adequate segmentation results. All manual segmentations were performed twice witch in a distance of 3 months. The data sets were navigated in corono-axial direction. The mean of both selected manual selected thresholds was used for further analysis. Intra-examiner reproducibility was 99,4%.
For manual threshold selection, the CBCT data set was cropped to the region of interest (ROI), the tooth-bearing maxilla or mandible, by visual inspection (Fig. 2). A global threshold was manually selected by visual inspection of the resulting iso-surface and marked areas in coronal and axial slices. The chosen lower threshold value was used for further analysis.
For automated threshold selection using the complete CBCT, the gray value range was limited from -500 to 1250 to generate a nearly bimodal gray value histogram and calculate a lower threshold value [16]. The resulting segmentation was inspected visually, and the selected lower threshold value was used for further analysis.
For automated threshold selection of the region of interest, the image was cropped to the ROI, the maxilla or the mandible, respectively. The threshold selection process was similar to the previously described in the complete CBCT volume. The resulting 120 different lower threshold values were used for further statistical analysis (Fig. 3).
Example histograms for manual and automated lower threshold selection in the complete CBCT and ROI, edentulous mandible. Showing the total spectrum of the gray values in CBCT in manual lower threshold selection (a) and the limited spectrum of gray values from -500 to 1250 in automated threshold selection in complete CBCT (b) and ROI (c). Selected threshold for each procedure is marked
Statistical analysis
Two sample T tests were used to compare threshold values of partially and total edentulous jaws in both maxilla and mandible. Linear regression models were applied to evaluate the influence of the opposite jaw on the threshold results of each segmentation procedure within each jaw type (maxilla, mandible). Linear mixed models were applied to compare the results of the different segmentation procedures in each jaw. For paired subsequent tests, the method of Scheffe was used to correct for multiple testing. Pearson's correlation coefficients were computed to evaluate an association of the number of teeth and dental restorations and gray values for each segmentation procedure. The level of significance was set at α = 0.05. STATA software (Release 17, StataCorp LLC, College Station, TX, USA) was used for statistical analysis.
Results
The remaining number of teeth in the partially edentulous patients and the teeth in the opposing for each patient are shown in Table 1 for the ROI maxilla and Table 2 for the ROI mandible.
The gray values for each manual and automated selection for the maxilla and mandible are displayed in the Additional file 1: Tables S1 and S2.
The distribution of lower threshold values for each jaw and all segmentation procedures are shown in Fig. 4. Mean values and standard deviations for each jaw and all segmentations procedures are shown in Table 3.
Two-sample t tests showed no significantly lower threshold values for manual threshold selection in partially compared to fully edentulous maxillae. Significantly different gray values were found for partially and fully edentulous mandibles (p = 0.0088), with lower gray values in fully edentulous mandibles (difference 130). Automated threshold selection tends to lower gray values in fully compared to partially edentulous mandibles, in the complete CBCT (p = 0.087, difference 58) and maxilla, in the cropped CBCT data set (p = 0.090, difference 75) could be found. The opposing jaw did not have a significant influence on gray values.
The comparison of segmentation procedures in the maxilla showed a significant difference in automated threshold selection of the complete CBCT vs. manual threshold selection (p < 0.001) with higher values in automated selection (difference: 65). Automated threshold selection of the complete CBCT resulted in significantly higher threshold values than the cropped CBCT (p < 0.001, difference 73). No significant difference was shown between manual and automated threshold selection in the cropped data set. In the mandible significant differences could be shown in all comparisons: automated complete CBCT vs. manual (p < 0.001, difference: 133), automated cropped CBCT vs. manual (p = 0.004, difference: 67) and automated complete CBCT data set vs. cropped data set (p = 0.007, difference: 64).
The comparison of automated threshold selection in the cropped data set and manual threshold selection resulted in significantly lower gray values in fully edentulous maxillae (p = 0.001 difference: 62) and partially edentulous mandibles (p < 0.001, difference: 110). Conversely, in partially edentulous maxillae, significantly higher gray values were observed (p = 0.009, difference: 49). Both threshold selection methods resulted in no significant differences in edentulous mandibles.
Correlation for evaluating the number of teeth and gray values selected by the different procedures showed no significant correlations but slight tendencies to a higher gray value in patients with more teeth for automated segmentation (Fig. 5). The restorations material showed no significant correlation to higher gray values.
Discussion
The selected threshold levels were significantly different for the maxilla and mandible and the three threshold selection procedures. Teeth influenced the selected gray values for the segmentation of bone. These effects were not only present around the teeth but in the whole data set, reflected in threshold values for segmentation. The influence of teeth on gray value distribution was more substantial for automated threshold selection and lower for manual threshold selection.
Gray values represent the tissue in each voxel and are used for density measurements of bone and surface model creation and display. An accurate surface model of craniofacial bone is crucial for digital surgery planning and guide production [24]. Manual threshold selection and a modified way for objective threshold selection are the most widely used techniques for surface model creation and exhibit good clinical results. However, they require individual input [13, 15].
To evaluate the influence of teeth on grey values, partially edentulous patients were selected according to the average number of remaining teeth. An average of eight teeth in the maxilla and nine in the mandible for patients between 65 and 74 years in Germany was presumed [25]. The included patients had an average of 7.5 teeth in the maxilla and 6.9 teeth in the mandible, representing the demographic distribution. To the author's knowledge, the number and distribution of teeth were previously not regarded to analyze gray values in CBCT. The former studies focused on the influence of metal restorations and dental implants on the surrounding gray values in vitro and in vivo; however, the impact of teeth on the complete data set has not been investigated [21,22,23].
Different segmentation methods, threshold levels, and acquisition specifications on (CB)CT-derived surface models were previously evaluated, and optical scans were used as a reference to assess accuracy in vitro and in vivo [5, 13,14,15, 26,27,28,29,30,31,32,33,34]. A literature review of different image segmentation methods used for medical imaging data reported deviations of 0.04 mm to 1.9 mm between surface models. The most used method, global threshold selection, resulted in deviations below 0.6 mm and implied extensive manual post-processing [13]. Standard values for bone segmentation of the whole skull and manual global threshold selection deviated − 2.3 mm to 4.8 mm from optical scans of cadavers [5]. Deviations between models created with manual global threshold selection of the mandible by an experienced clinician and laser surface scans of the cadaver mandible were 0.76 mm ± 0.39 mm [14]. Intra- and inter-examiner deviations of surfaces derived from manual threshold selection were reported with 0.18 mm and 0.15–0.26 mm, respectively [33]. Surface deviations of 0.6 mm were reported for models created with manual and automated threshold selection [15].
Due to the variances between the different image segmentation methods, manual global threshold selection, the most used method in medical image segmentation, and automated threshold selection were used in this study. All manual threshold selections were performed once, by one experienced clinician, under the same circumstances, without blinding. Automated threshold selection did not require individual input from the examiner and was adopted in the presented study as previously described [15]. The threshold range from -500 to 1250 was set based on Misch et al. and Norton et al. to transform the original histogram into a bimodal histogram for a well-defined threshold selection [16, 35, 36]. This method was used on the complete data set and the cropped data set and not on single slices, as described by Vaitiekunas et al. [15].
This study's main goal was to evaluate the influence of teeth and dental restorations on the gray value distribution, represented in selected threshold levels for bone segmentation, not the comparison of surface models generated by the described threshold selection procedures. Nevertheless, the comparison of both segmentation methods showed that automated and manual threshold selection differed, which can influence the surgical outcome by an over or underestimation of bone quantity and the misinterpretation of bone quality.
The mean gray values in the presented study were lower than the gray values for CBCT in a previous study. However, they ranged among the stated Hounsfield Units for CT [5, 32]. Grey values are not calibrated among CBCT systems, the field of view, voltage, voxel size, and bit value. Therefore, they may not be directly transferred or defined as Hounsfield units [10, 12, 37]. For standardization within the entire cohort, all CBCT data sets were acquired using the exact specifications and the same CBCT device, as recommended for minimizing the influences of the specific CBCT device and acquisition parameters [8, 9].
In all three threshold selection procedures, higher values were found in partially edentulous patients than fully edentulous patients, except in the maxilla in manual segmentation. This influence seems higher in automated threshold selection methods than in manual threshold selection. Gray value differences ranging from 24 to 110 between fully and partially edentulous patients are assumed to influence surface models significantly [34]. Deviations of up to 0.5 mm between bone surfaces were previously reported for gray value adaption of 60 [34]. Although Hounsfield units cannot be directly assigned to CBCT, especially for density measurements, it is widely used in implant planning software for preoperative bone density evaluation [11]. Especially in situations with remaining teeth, this evaluation may be impaired by the correlation of higher gray values and remaining teeth.
To interpret the results, one should be aware of the limitations of this study. No sample size calculation was performed due to the characteristics of a pilot study. This might result in an underpowered analysis. Using this data, sample size calculations can be performed in further studies to provide adequate power. All investigations were performed on a small cohort without calibrating for bone quality and quantity. The study cohort includes patients of each age and potential secondary diagnoses affecting bone density. Nevertheless, these patients represent patients in daily practice for whom the described techniques are applied for computer-aided design and manufacturing. The size of dental restorations was not considered, which is a downside of this study and should be addressed in further investigations.
Conclusions
Standard gray values do not apply for bone segmentation in CBCT as teeth influence the gray values and surface models resulting from segmentation. The clinical consequence are ill-fitting surgical guides produced on CBCT data and misinterpretation of bone density, both needed for fully guided implant surgery and determination of implant loading protocols. Automated bone segmentation may not be recommended for clinical routine, especially in partially edentulous patients. Every clinician should be aware of the potential over- and underestimation of bone and misinterpretation of bone quality in CBCT imaging in relation to the known artifacts and existing teeth. Automated segmentation methods, considering anatomical and acquisition specifications as shown in this study, could improve surface model generation using CBCT data.
Availability of data and materials
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CBCT:
-
Cone-beam computed tomography
- CAD/CAM:
-
Computer-aided design/computer-aided manufacturing
- HU:
-
Hounsfield Units
- FOV:
-
Field of view
- DICOM:
-
Digital Imaging and Communications in Medicine
References
Alamri HM, Sadrameli M, Alshalhoob MA, Sadrameli M, Alshehri MA. Applications of CBCT in dental practice: a review of the literature. Gen Dent. 2012;60(5):390–400 (quiz 1-2).
Abou-ElFetouh A, Barakat A, Abdel-Ghany K. Computer-guided rapid-prototyped templates for segmental mandibular osteotomies: a preliminary report. Int J Med Robot. 2011;7(2):187–92.
Huang MF, Alfi D, Alfi J, Huang AT. The use of patient-specific implants in oral and maxillofacial surgery. Oral Maxillofac Surg Clin North Am. 2019;31(4):593–600.
Venkatesh E, Elluru SV. Cone beam computed tomography: basics and applications in dentistry. J Istanb Univ Fac Dent. 2017;51(3 Suppl 1):S102–21.
van Eijnatten M, Koivisto J, Karhu K, Forouzanfar T, Wolff J. The impact of manual threshold selection in medical additive manufacturing. Int J Comput Assist Radiol Surg. 2017;12(4):607–15.
Zachow S, Zilske M, Hege H-C. 3D reconstruction of individual anatomy from medical image data: segmentation and geometry processing. 2007.
Zachow S. Computational planning in facial surgery. Facial Plast Surg. 2015;31(5):446–62.
Pauwels R, Stamatakis H, Bosmans H, Bogaerts R, Jacobs R, Horner K, et al. Quantification of metal artifacts on cone beam computed tomography images. Clin Oral Implants Res. 2013;24:94–9.
Schulze R, Heil U, Gross D, Bruellmann DD, Dranischnikow E, Schwanecke U, et al. Artefacts in CBCT: a review. Dentomaxillofac Radiol. 2011;40(5):265–73.
Pauwels R, Jacobs R, Singer SR, Mupparapu M. CBCT-based bone quality assessment: are Hounsfield units applicable? Dentomaxillofac Radiol. 2015;44(1):20140238.
Molteni R. Prospects and challenges of rendering tissue density in Hounsfield units for cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116(1):105–19.
Eguren M, Holguin A, Diaz K, Vidalon J, Linan C, Pacheco-Pereira C, et al. Can gray values be converted to Hounsfield units? A systematic review. Dentomaxillofac Radiol. 2022;51(1):20210140.
van Eijnatten M, van Dijk R, Dobbe J, Streekstra G, Koivisto J, Wolff J. CT image segmentation methods for bone used in medical additive manufacturing. Med Eng Phys. 2018;51:6–16.
Fourie Z, Damstra J, Schepers RH, Gerrits PO, Ren Y. Segmentation process significantly influences the accuracy of 3D surface models derived from cone beam computed tomography. Eur J Radiol. 2012;81(4):e524–30.
Vaitiekūnas M, Jegelevičius D, Sakalauskas A, Grybauskas S. Automatic method for bone segmentation in cone beam computed tomography data set. Appl Sci. 2020;10(1):236.
Otsu N. A threshold selection method from gray-level histograms. IEEE Trans Syst Man Cybern. 1979;9(1):62–6.
Winder J, Bibb R. Medical rapid prototyping technologies: state of the art and current limitations for application in oral and maxillofacial surgery. J Oral Maxillofac Surg. 2005;63(7):1006–15.
Stubinger S, Buitrago-Tellez C, Cantelmi G. Deviations between placed and planned implant positions: an accuracy pilot study of skeletally supported stereolithographic surgical templates. Clin Implant Dent Relat Res. 2014;16(4):540–51.
Nagata K, Fuchigami K, Hoshi N, Atsumi M, Kimoto K, Kawana H. Accuracy of guided surgery using the silicon impression and digital impression method for the mandibular free end: a comparative study. Int J Implant Dent. 2021;7(1):2.
Matsumura A, Nakano T, Ono S, Kaminaka A, Yatani H, Kabata D. Multivariate analysis of causal factors influencing accuracy of guided implant surgery for partial edentulism: a retrospective clinical study. Int J Implant Dent. 2021;7(1):28.
Martins LAC, Queiroz PM, Nejaim Y, Vasconcelos KF, Groppo FC, Haiter-Neto F. Evaluation of metal artefacts for two CBCT devices with a new dental arch phantom. Dentomaxillofac Radiol. 2020;49(5):20190385.
Candemil AP, Salmon B, Freitas DQ, Ambrosano GM, Haiter-Neto F, Oliveira ML. Metallic materials in the exomass impair cone beam CT voxel values. Dentomaxillofac Radiol. 2018;47(6):20180011.
Sancho-Puchades M, Hammerle CH, Benic GI. In vitro assessment of artifacts induced by titanium, titanium-zirconium and zirconium dioxide implants in cone-beam computed tomography. Clin Oral Implants Res. 2015;26(10):1222–8.
Kernen F, Benic GI, Payer M, Schar A, Muller-Gerbl M, Filippi A, et al. Accuracy of three-dimensional printed templates for guided implant placement based on matching a surface scan with CBCT. Clin Implant Dent Relat Res. 2016;18(4):762–8.
Jordan RA, Bodechtel C, Hertrampf K, Hoffmann T, Kocher T, Nitschke I, et al. The Fifth German Oral Health Study (Funfte Deutsche Mundgesundheitsstudie, DMS V)—rationale, design, and methods. BMC Oral Health. 2014;14:161.
Dong T, Xia L, Cai C, Yuan L, Ye N, Fang B. Accuracy of in vitro mandibular volumetric measurements from CBCT of different voxel sizes with different segmentation threshold settings. BMC Oral Health. 2019;19(1):206.
Galibourg A, Dumoncel J, Telmon N, Calvet A, Michetti J, Maret D. Assessment of automatic segmentation of teeth using a watershed-based method. Dentomaxillofac Radiol. 2018;47(1):20170220.
Van Dessel J, Nicolielo LF, Huang Y, Slagmolen P, Politis C, Lambrichts I, et al. Quantification of bone quality using different cone beam computed tomography devices: accuracy assessment for edentulous human mandibles. Eur J Oral Implantol. 2016;9(4):411–24.
Poleti ML, Fernandes TM, Pagin O, Moretti MR, Rubira-Bullen IR. Analysis of linear measurements on 3D surface models using CBCT data segmentation obtained by automatic standard pre-set thresholds in two segmentation software programs: an in vitro study. Clin Oral Investig. 2016;20(1):179–85.
Engelbrecht WP, Fourie Z, Damstra J, Gerrits PO, Ren Y. The influence of the segmentation process on 3D measurements from cone beam computed tomography-derived surface models. Clin Oral Investig. 2013;17(8):1919–27.
Maret D, Telmon N, Peters OA, Lepage B, Treil J, Inglese JM, et al. Effect of voxel size on the accuracy of 3D reconstructions with cone beam CT. Dentomaxillofac Radiol. 2012;41(8):649–55.
Hassan B, Couto Souza P, Jacobs R, de Azambuja BS, van der Stelt P. Influence of scanning and reconstruction parameters on quality of three-dimensional surface models of the dental arches from cone beam computed tomography. Clin Oral Investig. 2010;14(3):303–10.
Schnutenhaus S, Graf M, Doering I, Luthardt RG, Rudolph H. Reproducibility of CBCT image analysis: a clinical study on intrapersonal and interpersonal errors in bone structure determination. Oral Radiol. 2019;35(2):152–8.
Friedli L, Kloukos D, Kanavakis G, Halazonetis D, Gkantidis N. The effect of threshold level on bone segmentation of cranial base structures from CT and CBCT images. Sci Rep. 2020;10(1):7361.
Misch CE. Contemporary implant dentistry. Implant Dent. 1999;8(1):90.
Norton MR, Gamble C. Bone classification: an objective scale of bone density using the computerized tomography scan. Clin Oral Implants Res. 2001;12(1):79–84.
Van Dessel J, Nicolielo LF, Huang Y, Coudyzer W, Salmon B, Lambrichts I, et al. Accuracy and reliability of different cone beam computed tomography (CBCT) devices for structural analysis of alveolar bone in comparison with multislice CT and micro-CT. Eur J Oral Implantol. 2017;10(1):95–105.
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
OW: contributed to conception and design, acquisition, analysis, and interpretation; drafted and critically revised the manuscript. SN: contributed to analysis and interpretation and critically revised the manuscript. KV: contributed to analysis and interpretation, performed the statistical analysis, and critically revised the manuscript. FK: contributed to analysis and interpretation and critically revised the manuscript. SZ: contributed to conception and design, granted the research license of Amira-ZIBEdition, drafted and critically revised the manuscript. MH: contributed to acquisition, interpretation, and critically revising the manuscript. TF: contributed to conception, design, and interpretation and critically revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol complied with the STROBE guidelines and was approved by the Ethics Committee of the Charité—Universitätsmedizin Berlin, Germany (EA4/111/21).
Consent for publication
All authors gave their final approval and agreed to be accountable for all aspects of the work.
Competing interests
The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Gray values for each segmentation procedure in the maxilla. Table S2. Gray values for each segmentation procedure in the mandible.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wagendorf, O., Nahles, S., Vach, K. et al. The impact of teeth and dental restorations on gray value distribution in cone-beam computer tomography: a pilot study. Int J Implant Dent 9, 27 (2023). https://doi.org/10.1186/s40729-023-00493-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40729-023-00493-z