Abstract
Background
Dental implant placement is safe and predictable, yet optimal management of anticoagulated patients remains controversial. Whilst cessation of anticoagulation pre-operatively should decrease risks of bleeding, risk of thrombosis increases. We aim to define risk of bleeding in patients on oral anticoagulation who are undergoing dental implant placement, in order to establish best management.
Methods
This systematic review is registered with the National Institute for Health Research (NIHR) PROSPERO database (Registration No: CRD42021233929). We performed a systematic review as per Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidance. Studies were identified using an agreed search strategy within the OVID Gateway (this included Pubmed, MEDLINE, Cochrane Collaborative). Studies assessing bleeding complications in patients who were undergoing dental implant placement were selected. The primary outcome was bleeding events in anticoagulated patients undergoing dental implant placement. Secondary outcomes included any complication requiring further intervention.
Results
We identified 182 studies through screening, and after review of titles and abstracts reduced this to 8 studies. In these studies, 1467 participants received at least 2366 implants. Studies were analysed for quality using the ROBINS-I risk of bias tool. Four studies were retrospective case reviews, and four were prospective reviews, three of which also blinded the operator to anticoagulation status. There was significant heterogeneity between the included studies. Meta-analysis showed an increased risk of bleeding (RR, 2.30; 95% CI, 1.25-4.24 p = 0.37 I = 7%) when implants were placed in the presence of anticoagulation however these were not clinically significant haemorrhagic events.
Conclusion
The continuation of anticoagulants peri-operatively during dental implant surgery does increase the risk of clinically non-significant peri- and post-operative bleeding. Dental implant surgery encompasses a broad spectrum of procedures ranging from minor to more invasive surgery with simple local haemostatic measures mitigating the risk of bleeding. The decision to discontinue anticoagulants prior to dental implant surgery must consider patient and surgical factors with the clinician undertaking a risk-balance assessment.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Dental implant placement is safe and predictable, yet optimal management of anticoagulated patients remains controversial. Weighing up the risks and benefits of placing dental implants in anticoagulated patients and whether stopping or pausing anticoagulation peri-procedurally mitigates bleeding risk remains unclear. Regular review of all available evidence, with meta-analysis, allows better understanding of these risks and benefits.
The volume of dental implant placement has proliferated in the past 20 years, with over 10,000 mandibular implants placed per year in the UK [1]. Refinements in implant design and procedural protocols have decreased complication rates to around 2%, yielding 1- and 5-year survival rates of around 99% and 94% respectively [2]. However, variation in practice remains, particularly regarding medical management of patients undergoing implant placement. Detailed review of the evidence may allow further gains in optimising management.
Management of the anticoagulated patient has evolved with the introduction of direct oral anticoagulants (DOACs) and concurrent reduction in use of warfarin. DOACs have a number of advantages over warfarin—they have been shown to cause fewer life threatening haemorrhages than warfarin [3], have shorter half-life, do not require alterations in daily dosing, and reversal agents are now available for all DOACs [4]. Yet, there are not yet clear protocols for management of patients on DOACs undergoing surgical procedures. Whilst cessation of anticoagulation pre-operatively would decrease bleeding risk, it would also increase risk of embolic events [5].
Equipoise exists in the literature, with some authors advocating no alteration to anticoagulation protocols when placing dental implants [6], and others advising that pausing anticoagulation is necessary [7]. Systematic review of the literature and meta-analysis is required to define bleeding risk of anticoagulated patients undergoing dental implant placement, and hence determine optimal management of this patient group.
Methods
This systematic review is registered with the National Institute for Health Research (NIHR) PROSPERO database (Registration No: CRD42021233929) and has been designed and reported in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) [8].
Search strategy
Searches were conducted via Ovid Gateway (including MEDLINE, PubMed and Cochrane Collaboration), PubMed from inception to January 2021, ISI Web of Science, from inception to June 2020. Search terms included “dental implants”, “zygomatic implants”, “oral implants” and “anticoagulants”, “warfarin”, “direct oral anticoagulants”, “DOAC”, “rivaroxaban”, “apixaban”, “dabigatran” and “bleeding”, “complications”.
Study selection
Abstract screening was undertaken by two authors (BD/SK) to ascertain relevance to the research question. The full texts were obtained and then screened independently.
Data extraction
Reviewing authors collected data regarding study type, number of participants and implants in the anticoagulated group and none-anticoagulated (control) group respectively and peri-operative anticoagulation protocol. Further data included reported outcome complications (haemorrhage, haematoma formation, purpura, bleeding requiring further intervention). Corresponding authors were contacted where data was missing, or articles were inaccessible.
Outcomes
The primary outcome was any significant bleeding (as defined and reported by each respective study) requiring treatment. This may have been reported within the immediate peri-operative phase or bleeding complications within 7 days of primary surgery.
Risk of bias assessment
Studies were assessed for risk depending upon their methodology. For non-randomised studies the The Risk Of Bias In Non-randomised Studies of Interventions (ROBINS-I) tool was used [9]. This was stratified into four escalating categories with 0 and 1 representing no information and low risk respectively to 4 indicating serious risk of bias.
Data analysis
Analysis was carried out via direct comparison meta-analysis using Review Manager ® version 5 [10]. Analysis was performed to calculate the risk ratios (RR) of any reported bleeding complication with a confidence interval (CI) of 95%. Clinical and statistical heterogeneity was assessed using a random-effects model and I2 respectively, where an I2 score of 0 indicates complete homogeneity between studies. Studies and data were split into two subgroups following reported peri-operative anticoagulation protocol. These were split into studies which continued and discontinued anticoagulant therapy peri-operatively respectively.
Results
Study selection
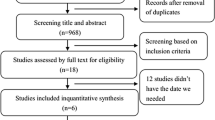
A total of 182 original studies following limiting to English language and removing non-duplicates were identified from the searches and from screening. Abstract screening removed 170 studies not relevant to the study. Full texts of 12 articles were obtained for further assessment, resulting in exclusion of a further 4 studies. Finally, 8 studies [6, 11,12,13,14,15,16,17] met eligibility criteria for this review and were included for full analysis (Fig. 1).
Study characteristics
All articles included were observational cohort studies. There were 4 retrospective [6, 11, 12, 17] and 4 prospective [13,14,15,16]; of the prospective studies, 3 [13, 14, 16] blinded the operator from which patients were taking anticoagulants. A total of 1467 participants were included with a minimum of 2366 implants placed across all studies. There were 3 studies [6, 15, 17] which did not report the number of implants placed within their respective cohorts; therefore, the total number of implants was under-estimated to reflect a singular implant for the number of participants within those studies. Further information on the study characteristics are included in Table 1.
In order to minimise clinical heterogeneity with study protocols, the analysis was split into two subgroups. The studies were split dependant upon their peri-operative protocols in which one group (1) continued anticoagulation peri-operatively without a pause [6, 12, 13, 15,16,17] and those which (2) discontinued in the immediate pre-operative period [11, 14] and restarted 6-12 h post-operatively.
There was variability in the oral anticoagulants included within the studies. In total, three studies [11, 13, 14] compared a single direct oral anticoagulant (DOAC) with a control group of no anticoagulant with three studies [6, 12, 15] grouping patients on either warfarin or any other DOACs. One [16] compared warfarin alone with a control group of patients not taking warfarin and one [17] study comparing patients on warfarin and an antiplatelet with a control group of no anticoagulants or antiplatelets.
There was variability when reporting outcome measures (complications) between the studies.
One study [6] required patients to self-report bleeding and of those who required urgent clinical assessment, the bleeding was quantified subjectively. Four studies [11, 13, 14, 16] analysed bleeding in accordance to criteria set out by Bacci et al. [16] which categorises bleeding complications into four stages with escalating levels of haemostatic control. One [12] study qualified bleeding within 24 h as a primary outcome measure with anything > 24 h considered a secondary outcome with associated features of haematoma, purpura or ecchymoses. One study [17] did not qualify the criteria for bleeding complications and was based on subjective assessment of the patient. One study [15] defined their own criteria of bleeding as low, moderate or severe with escalating levels of intervention for haemostatic control. All included studies reviewed patients at least once within a 7-day post-operative period or same day assessment in the case of urgent bleeding.
Risk of bias
The risks of bias within the methodology of the included studies are shown in Fig. 2 and Table 2. RCTs are assessed in Fig. 2 in accordance with Cochrane Collaboration’s tool for assessing bias [19] and non-randomised studies analysed using the Risk of Bias in Non-Randomised Studies – of Intervention tool (ROBINS-I) [9] (Table 2).
Effects of intervention
Table 3 summarises the findings between the respective peri-operative protocols utilised for management of anticoagulation in dental implant surgery. When comparing continuation of anticoagulants peri-operatively to the control of no anticoagulation (Fig. 2), the relative risk of the studies demonstrate an increased risk of peri-operative bleeding complications when anticoagulants are continued (RR, 2.30; 95% CI, 1.25—4.24 p = 0.37 I = 7%); however, the quality of evidence is low with risk of bias throughout (Table 2). Despite the increased risk of bleeding, across the entire cohort of 1467 participants, only two participants required hospitalisation for the severity of bleeding [15] of which one participant was anticoagulated and the other was not. All the studies that reported bleeding complications were managed with local haemostatic measures without the need for further interventions. There was insufficient data to perform a meaningful meta-analysis on whether pausing anticoagulation (Fig. 3) reduces the risk of bleeding complications (RR 1.45, 95% CI, 0.22-9.70).
Discussion
There are different approaches to the management of anticoagulation in dental implant surgery. Practice with DOACs ranges from continuing anticoagulation, pausing anticoagulation prior to the day of surgery or bridging protocols with low molecular weight heparin (LMWH). National guidance classifies dental implant surgery as higher risk of post-operative bleeding complications [7]. The Scottish Dental Clinical Effectiveness Programme (SDCEP) guidance acknowledges the paucity of high quality data to support recommendations given in the guideline. For patients on DOACs, recommendations for procedures with high risk of bleeding complications are to withhold the morning dose of the drug [7]. Furthermore, for patients on warfarin, the advice is to treat patients with international normalised ratios (INR) of ≤ 4 (checked within 24 h of surgery) without a pause in their anticoagulation. Both these recommendations are based on low quality evidence as acknowledged in the guideline.
Implant procedures range from simple immediate single placements following dental extraction to more complex bi-maxillary oral reconstructive surgery (zygomatic or pterygoid implants) with associated grafting procedures. The nature of bleeding risk is not just dependent upon anticoagulation status but also of how invasive the surgery is. Most of the studies included did not stratify groups into the respective intervention to assess bleeding risk of procedure specific interventions. This is an important factor when considering a pause of the patients’ anticoagulation.
There are no randomised controlled clinical trials evaluating the effect of anticoagulation on bleeding; however, there are prospective blinded studies [13, 14, 16]. These studies continued anticoagulation peri-operatively and blinded only the surgeon to group allocation (anticoagulated and none anticoagulated). None of the included studies performed power calculations or intention to treat analysis.
The evaluation of bleeding within the peri-operative period of the included studies is fraught with bias. Bacci et al. [16] defined a criteria in which to objectively assess bleeding with an escalating level of intervention to reflect the severity of bleeding. This scale is a four tier system graded from no bleeding, slight bleeding (defined as a slight ooze) managed with compressive gauze only. The moderate category is defined as bleeding with large clots disrupting the surgical field requiring additional haemostatic measures, and severe are categorised as patients requiring systemic medical management to achieve haemostasis [16].
Some of the included studies [11, 13, 14, 16] adopted the grading published by Bacci et al. [16] as a more objective analysis and subsequently reported bleeding complications in accordance with this scale. The variability in the means of reporting bleeding complications creates heterogeneity in what is reported in the literature and may lead to an over or under reporting of complications.
Other meta-analyses have demonstrated conflicting relative risk ratios in patients on oral anticoagulants undergoing dental surgery. Shi et al. [20] reported an increase risk of bleeding in patients on oral anticoagulants compared to a control group of no anticoagulant, whilst a meta-analysis by Nematullah et al. [21] reported no significantly increased risk of bleeding in patients who continue warfarin therapy to those who discontinue. Furthermore, other research has been conducted to assess the risk of bleeding for oral surgical procedures in patients on oral anticoagulants [22,23,24]; however, there remains a degree of uncertainty due to discrepancies in methodology and outcome measures reported. These studies did not exclusively assess the risk of bleeding in patients undergoing dental implant surgery but rather a multitude of different oral surgical procedures.
Clearly, the decision to discontinue anticoagulation for dental implant surgery must not be taken lightly. There is evidence that discontinuation of anticoagulant therapy may increase the risk of venous thrombo-embolism causing significant morbidity or even mortality for patients [5, 25]. A study by Wahl et al. of 5431 patients undergoing dental surgical procedures, 2763 had warfarin reduced or withdrawn peri-operatively and there were subsequently 22 (0.8%) thrombo-embolic and 6 (0.2%) fatal complications [5]. The indication for anticoagulation could be for either prophylactic or therapeutic purposes and therefore must be considered carefully in the surgical consultation. Discontinuation of anticoagulation must be balanced with individual bleeding risk and patients considered on an individual basis.
All the included studies reinforce the importance of local haemostatic measures when managing patients on oral anticoagulants. Throughout the entire cohort included in this study, only two patients (one within the anticoagulated and other in the non-anticoagulated group respectively) [15] required hospitalisation due to the severity of haemorrhage, with all other studies reporting managing bleeding with simple local measures. This reinforces national guidelines which advise the prophylactic use of local haemostatic measures following oral surgical procedures [7].
Limitations
Several of the included studies had systematic differences leading to variability in reporting of outcomes. This meta-analysis includes patients undergoing all forms of dental implant surgery; however, this is a broad range from single to multiple placements. Only one study [12] considered full arch rehabilitation as the modality of surgery when comparing anticoagulated patients with the remainder of the studies containing a mix of single and multi-implant placements. Single implant placements are considered far less invasive than a full arch osseo-integrated rehabilitation or zygomatic implants. None of the studies included zygomatic or pterygoid implants and our findings should not be extrapolated to encompass this patient group. Future clinical studies show aim to ascertain the risk of bleeding complications from higher risk and more invasive dental implant surgery.
This systematic review only considered single anticoagulant vs no anticoagulation. There is evidence that dual antiplatelets can exacerbate bleeding leading to a higher risk of complications [26, 27]. Furthermore, this review did not take into consideration patients who take anticoagulants in combination with antiplatelets. There is evidence that a combination of these two drugs can increase bleeding risk [28]; however, this has not been shown in studies for patients undergoing oral surgical procedures.
Conclusions
Based on the available data and within the limitations of the published studies included in this meta-analysis, the continuation of anticoagulants peri-operatively during dental implant surgery does increase the risk of clinically non-significant peri- and post-operative bleeding. The decision to discontinue anticoagulants prior to dental implant surgery must be a patient specific one and involve a careful risk balance assessment. This should be done in consultation with the patient and where necessary their prescribing physician. All the studies demonstrate that any bleeding complications following dental implant surgery can easily be managed with local haemostatic measures. Dental implant surgery ranges from smaller interventions which carry a lower risk of bleeding to more invasive full mouth surgical rehabilitation such as bimaxillary and zygomatic implants. Further research should aim to reflect the respective bleeding risks for anticoagulated patients for these more invasive surgical procedures than that of single implants. This will help the development of more tailored guidance specific to procedures that may potentially carry a higher risk of bleeding.
Availability of data and materials
The datasets of the current study are available from the corresponding author on reasonable request.
Abbreviations
- UK:
-
United Kingdom
- DOAC:
-
Direct oral anticoagulants
- NIHR:
-
National Institute for Health Research
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- ROBINS-I:
-
The Risk Of Bias In Non-randomised Studies of Interventions
- LMWH:
-
Low molecular weight heparin
- INR:
-
International normalised ratio
- RR:
-
Risk ratios
- CI:
-
Confidence intervals
- RCT:
-
Randomised controlled trial
- SDCEP:
-
Scottish Dental Clinical Effectiveness Programme
- PROSPERO:
-
International Prospective Register of Systematic Reviews
References
Royal College of Surgeons (Faculty of Dental Surgery). Briefing for House of Lords debate on dental implants and periodontal checks. 2014.
Guo Q, Lalji R, le AV, Judge RB, Bailey D, Thomson W, et al. Survival rates and complication types for single implants provided at the Melbourne Dental School. Aust Dent J. 2015;60(3):353–61. https://doi.org/10.1111/adj.12248.
Eikelboom J, Merli G. Bleeding with direct oral anticoagulants vs warfarin: clinical experience. Am J Emerg Med. 2016;34(11S):3–8. https://doi.org/10.1016/j.ajem.2016.09.046.
Levy JH, Douketis J, Weitz JI. Reversal agents for non-vitamin K antagonist oral anticoagulants. Nat Rev Cardiol. 2018;15(5):273–81. https://doi.org/10.1038/nrcardio.2017.223.
Wahl MJ, Pinto A, Kilham J, Lalla RV. Dental surgery in anticoagulated patients--stop the interruption. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119(2):136–57. https://doi.org/10.1016/j.oooo.2014.10.011.
Manor Y, et al. A retrospective analysis of dental implantation under anticoagulant treatment. Clin Oral Investig. 2020.
Scottish Dental Clinical Effectiveness Programme (SDCEP) Management of dental patients taking anticoagulants or antiplatelet drugs: dental clinical guidance. 2015 [cited 2020; Available from: https://www.sdcep.org.uk/wp-content/uploads/2015/09/SDCEP-Anticoagulants-Guidance.pdf.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9, W64. https://doi.org/10.7326/0003-4819-151-4-200908180-00135.
Sterne JA, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
The Cochrane Collaboration, Review Manager (RevMan) Version 5.4 2020.
Galletti G, et al. Implant placement in patients under treatment with rivaroxaban: a retrospective clinical study. Int J Environ Res Public Health. 2020;17(12). 4607. 1-13.
Sannino G, Capparé P, Montemezzi P, Alfieri O, Pantaleo G, Gherlone E. Postoperative bleeding in patients taking oral anticoagulation therapy after ‘All-on-four’ rehabilitation: a case-control study. Int J Oral Implantol (Berl). 2020;13(1):77–87.
Gomez-Moreno G, et al. Dental implant surgery in patients in treatment with the anticoagulant oral rivaroxaban. Clin Oral Implants Res. 2016;27(6):730–3. https://doi.org/10.1111/clr.12653.
Gomez-Moreno G, et al. Dental implant surgery in patients in treatment by dabigatran. Clin Oral Implants Res. 2018;29(6):644–8. https://doi.org/10.1111/clr.12785.
Clemm R, Neukam FW, Rusche B, Bauersachs A, Musazada S, Schmitt CM. Management of anticoagulated patients in implant therapy: a clinical comparative study. Clin Oral Implants Res. 2016;27(10):1274–82. https://doi.org/10.1111/clr.12732.
Bacci C, Berengo M, Favero L, Zanon E. Safety of dental implant surgery in patients undergoing anticoagulation therapy: a prospective case-control study. Clin Oral Implants Res. 2011;22(2):151–6. https://doi.org/10.1111/j.1600-0501.2010.01963.x.
Okamoto T, Hoshi K, Fukada K, Kataoka T, Kumasaka A, Kaibuchi N, et al. Factors affecting the occurrence of complications in the early stages after dental implant placement: a retrospective cohort study. Implant Dent. 2018;27(2):221–5. https://doi.org/10.1097/ID.0000000000000753.
Centre for Evidence - Based Medicine. Oxford Centre for Evidence-Based Medicine: levels of evidence (March 2009) 2009 [cited 2021; Available from: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009.
Higgins JP, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343(oct18 2):d5928. https://doi.org/10.1136/bmj.d5928.
Shi Q, et al. Post-operative bleeding risk in dental surgery for patients on oral anticoagulant therapy: a meta-analysis of observational studies. Front Pharmacol. 2017;8:58.
Nematullah A, Alabousi A, Blanas N, Douketis JD, Sutherland SE. Dental surgery for patients on anticoagulant therapy with warfarin: a systematic review and meta-analysis. J Can Dent Assoc. 2009;75(1):41.
Madrid C, Sanz M. What influence do anticoagulants have on oral implant therapy? A systematic review. Clin Oral Implants Res. 2009;20(Suppl 4):96–106. https://doi.org/10.1111/j.1600-0501.2009.01770.x.
Dunn AS, Turpie AG. Perioperative management of patients receiving oral anticoagulants: a systematic review. Arch Intern Med. 2003;163(8):901–8. https://doi.org/10.1001/archinte.163.8.901.
Kammerer PW, et al. Oral surgery during therapy with anticoagulants-a systematic review. Clin Oral Investig. 2015;19(2):171–80. https://doi.org/10.1007/s00784-014-1366-3.
Wahl MJ. Dental surgery in anticoagulated patients. Arch Intern Med. 1998;158(15):1610–6. https://doi.org/10.1001/archinte.158.15.1610.
Zabojszcz M, Malinowski KP, Janion-Sadowska A, Lillis T, Ziakas A, Sławska A, et al. Safety of dental extractions in patients on dual antiplatelet therapy - a meta-analysis. Postepy Kardiol Interwencyjnej. 2019;15(1):68–73. https://doi.org/10.5114/aic.2019.83773.
Napenas JJ, et al. Review of postoperative bleeding risk in dental patients on antiplatelet therapy. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115(4):491–9. https://doi.org/10.1016/j.oooo.2012.11.001.
Eikelboom JW, Hirsh J. Combined antiplatelet and anticoagulant therapy: clinical benefits and risks. J Thromb Haemost. 2007;5(Suppl 1):255–63. https://doi.org/10.1111/j.1538-7836.2007.02499.x.
Acknowledgements
Not applicable
Funding
None
Author information
Authors and Affiliations
Contributions
BD (1) concept/design, statistics, and data analysis/interpretation; (2) drafting of the article; (3) final approval and (4) accountable for all aspects of the work. SK (1) drafting of the article; (2) final approval and (3) accountable for all aspects of the work. OT (1) concept/design, statistics, and data analysis/interpretation and (2) drafting of the article. PG (1) concept/design, statistics, and data analysis/interpretation and (2) final approval. JD (1) concept/design, statistics, and data analysis/interpretation; (2) drafting of the article; (3) final approval and (4) accountable for all aspects of the work. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Basim ES Dawoud, Samuel Kent, Oliver Tabbenor, Pynadath George and Jagtar Dhanda declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dawoud, B.E.S., Kent, S., Tabbenor, O. et al. Dental implants and risk of bleeding in patients on oral anticoagulants: a systematic review and meta-analysis. Int J Implant Dent 7, 82 (2021). https://doi.org/10.1186/s40729-021-00364-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40729-021-00364-5