Abstract
Background
Peptide receptor radionuclide therapy with 177Lu-DOTATATE is a recognized option for treating neuroendocrine tumors and has few toxicities, except for the kidneys and bone marrow. The bone marrow dose is generally derived from a SPECT/CT image-based method with four timepoints or from a blood-based method with up to 9 timepoints, but there is still no reference method. This retrospective single-center study on the same cohort of patients compared the calculated bone marrow dose administered with both methods using mono, bi- or tri-exponential models. For the image-based method, the dose was estimated using Planetdose© software. Pearson correlation coefficients were calculated. We also studied the impact of late timepoints for both methods.
Results
The bone marrow dose was calculated for 131 treatments with the blood-based method and for 17 with the image-based method. In the former, the median absorbed dose was 15.3, 20.5 and 28.3 mGy/GBq with the mono-, bi- and tri-exponential model, respectively. With the image-based method, the median absorbed dose was 63.9, 41.9 and 60.8 with the mono-, bi- and tri-exponential model, respectively. Blood samples after 24h post-injection did not evidence any change in the absorbed bone marrow dose with the bi-exponential model. On the contrary, the 6-day post-injection timepoint was more informative with the image-based model.
Conclusion
This study confirms that the estimated bone marrow dose is significantly lower with the blood-based method than with the image-based method. The blood-based method with a bi-exponential model proved particularly useful, without the need for blood samples after 24h post-injection. Nevertheless, this blood-based method is based on an assumption that needs to be more validated. The important difference between the two methods does not allow to determine the optimal one to estimate the true absorbed dose and further studies are necessary to compare with biological effects.
Similar content being viewed by others
Introduction
Peptide receptor radionuclide therapy (PRRT) with 177Lu-DOTATATE or 177Lu-oxodotreotide, a somatostatin analog radiolabeled with 177Lu, is a recognized therapeutic option for metastatic or symptomatic patients with midgut WHO grade I-II neuroendocrine tumors. It has proven short- and long-term efficacy in terms of progression-free survival and symptom control even if the objective response rate was only 18%, as previously demonstrated by the NETTER-1 study [1]. The standard treatment consists in four intravenous injections of 7.4 GBq of 177Lu-DOTATATE administered every 8 weeks. This therapy is well tolerated as few toxicities have been reported for kidney and bone marrow [2, 3]. Nevertheless, severe hematotoxicity may occur. For example, the NETTER 01 study reported grade 3 or 4 thrombopenia (2%) and lymphopenia (9%), and myelodysplastic syndrome (MDS) can occur in about 2% and leukemia in about 1% of treated patients [4, 5]. Estimating the absorbed dose to the bone marrow to personalize and optimize treatment could possibly limit the hematological toxicity, which could be particularly challenging in the event of retreatment or further cytotoxic treatment. However, the methodology for estimating the absorbed dose in bone marrow is not standardized and the exact dose–effect relationship remain elusive. Significant but weak correlations between image-based estimates of the red-bone-marrow absorbed dose and hematological toxicity have been demonstrated [6]. Hagmarker et al. found a significant correlation between the absorbed dose in bone marrow and decreased platelet counts [7], whereas Garske-Roman et al. found that bone marrow dosimetry did not predict toxicity [8]. For Forrer et al. there is no correlation between red marrow absorbed dose and short-term acute hematological toxicity [9].
In the literature, the bone marrow dose is basically derived from an image-based method or from a blood-based method, with some crossover between both. Both have advantages and drawbacks. To calculate the time activity curve (TAC), both methods require several acquisitions or blood samples after each 177Lu-DOTATATE administration, which implies patient availability and compliance. In the imaging method, each acquisition lasts more than 40 min with possible motion artefacts. In both methods, the assumption is that the activity concentration in bone marrow is the same as in blood [9]. In the image-based method, it is assumed that the absorbed dose of a limited area, mostly the lumbar spine, represents the total bone marrow activity. No standard method yet exists, and Table 1 shows the published methods to calculate the bone marrow dose, acquisition or blood sampling timepoints, the model used, and the estimated absorbed dose in bone marrow. The threshold of the absorbed dose in bone marrow for severe hematological toxicity is still unclear and is dependent on the patient’s risk factors. It was initially set at 2 Gy based on 131I therapy data [10]. Considerable differences exist depending on the method used and few comparisons are available. Page et al. recommends using image-based dosimetry in clinical treatment for the red marrow dose as the blood-based method may underestimate it by a factor of 4 [11].
Recently, the EANM dosimetry committee published its recommendations for the dosimetry of 177Lu-labeled somatostatin-receptor and PSMA-targeting ligands [6]. For 177Lu-PRRT, the median value for the red marrow absorbed dose across all the studies is 50 mGy/GBq. The total-body time activity curve (TAC) is generally biphasic, as is the case for the blood TAC. The recommendation for dosimetry is to measure the activity concentration in the blood even if sequential planar or SPECT/CT whole-body imaging is also possible.
Another issue that hampers the use of dosimetry in general is the fact that late timepoints are crucial to correctly estimate the absorbed dose [6]. This late timepoint, which is usually somewhere between 144 and 168h post-injection, may be difficult to establish as it implies that the patient needs to come back to the institute. With the blood-based method, it is still not clear whether this late timepoint has any value.
To our knowledge, no publication on the two methods has compared the impact of different models for dosimetry with patients acting as their own control. The aim of this study was to evaluate and compare the impact of the mono-, bi- and tri-exponential models for the blood-based method and the image-based method. We evaluated and compared the impact of the late timepoints in both methods to estimate the bone marrow dose administered in 177Lu-DOTATATE therapy.
Material and methods
Patients
A retrospective study was conducted on 59 patients treated in our institution for neuroendocrine tumors (NET) with 177Lu-DOTATATE (Lutathera ®) between 2019 and 2021. In a standard study, patients received 4 cycles of 177Lu-DOTATATE at the recommended activity of 7400 MBq during a 30-min intravenous perfusion. The interval between each cycle was eight weeks. The study was declared to the Health Data Hub (number: F20230102114415).
Blood sampling
Six to nine blood samples were collected at 0.5, 1, 2, 4, 8, 16, 24, 72 and 144 h post-injection in each patient. Blood was collected in the arm contralateral to that in which 177Lu-DOTATATE was injected. Blood samples were centrifuged at 1000xg for 10 min at ambient temperature. Radioactivity was measured in 1 ml aliquots of plasma using a WIZARD2™ 2480-0010 Gamma Counter (Perkin Elmer, MS, USA). A calibration curve with 177Lu-DOTATATE was established to normalize the data obtained with the gamma counter. Radioactivity-time data were expressed in MBq/L after correction for radioactive decay between the time of the sampling and the measurement according to the equation:
where C(t)corr is 177Lu-Dotatate concentration at time t corrected for radioactive decay, C(t)measured is the 177Lu-Dotatate concentration measured at time tmeasured, T1/2,177Lu is the half-time disintegration of 177Lu and T0 is the time of 177Lu-Dotatate injection [29].
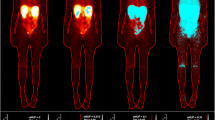
Image acquisition
Abdominal SPECT/CT acquisitions were planned at 4, 24, 96 and 144 h post-injection. The last timepoints were modified depending on weekend constraints. Images were acquired on a GE Discovery NM CT 670 system, which is composed of two 15.8 mm (5/8″) NaI (Tl) crystal detectors and a 40 × 54 cm axial FOV. Medium-energy general purpose (MEGP) collimators were used. All images were acquired with a 20% energy window around the main photopeak of 177Lu of 208 keV and a lower scatter window of 10% around 178 keV and an upper scatter window of 10% around 241 keV. Matrix size was 128 × 128 and 60 projections of 40 s were acquired over 360°. Images were reconstructed using the OSEM algorithm (5 iterations, 10 subsets) with correction of attenuation with low-dose CT images, scatter and resolution recovery.
Dosimetry
For the blood-based method, the activity concentration was fitted by a mono-, bi- or tri- exponential curve to infinity to estimate the area under the curve (AUC) using an in-house Python program (Python 3.10, numpy and matplotlib libraries). The mass and self-dose S-value used to calculate the absorbed dose to the bone marrow were those of the EANM recommendations [6].
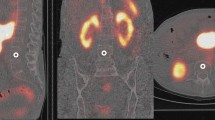
For the image-based method, dosimetry was performed using the PlanetDose® software from DOSIsoft. It used reconstructed images and allowed the full processing: organ-based rigid registration using CT images, rigid propagation of the structures, time integrated activity coefficient (TIAC) fitting (several fitting options) and organ absorbed dose (dose kernel or local deposition model with or without density correction) [30]. For bone marrow, the trabecular part of the vertebrae between L2 and L4 was delineated to estimate the absorbed dose [22, 31]. To reduce the error, the union of these three volumes of interest was considered in one structure. The mono-, bi- and tri-exponential models were used, as it commonly found in the literature and the absorbed dose was estimated by using the local deposition method with density correction.
For both methods, the used fitting functions had the following expression:
Mono-exponential: \(a*{e}^{-bx}\)
Bi-exponential: \(a*{e}^{-bx}+c*{e}^{-dx}\)
Tri-exponential: \(a*{e}^{-bx}+c*{e}^{-dx}+f*{e}^{-gx}\)
Where a, b, c, d, f and g were coefficients to determine.
The goodness of fit of the models was measured using R2.
To estimate the influence of the late timepoints for the blood-based method, we estimated the absorbed dose with only the timepoints before 24 h post-injection. For the image-based method, we kept only three timepoints by deleting the last one and compared the absorbed dose to the one calculated with all the timepoints.
Statistics
To compare the different methods/models and the influence of the timepoints, Bland–Altman plots have been built.
Results
Patient characteristics are shown in Table 2.
Blood-based method
As some patients received several 177Lu-DOTATATE infusions, the study took 131 treatments into account: 48 for the first infusion, 38 for the second, 26 for the third and 19 for the fourth. Before analyzing the 131 treatments, we investigated the possibility to pool all the data without differentiating the cycles. As the results were similar, we estimated that all the data could be analyzed without differentiating the cycles (see Additional file 1). Table 3 and Fig. 1 show the median absorbed dose to the bone marrow calculated with the mono-, bi- or tri-exponential model for the blood-based method.
For the evaluation of the fitting, the coefficient of determination (R2) was calculated. It was always higher for the tri-exponential model (median: 0.999, min: 0.849, max: 1) than for the bi-exponential model (median: 0.999, min: 0.849, max: 0.999). Its lower median value was for the mono-exponential model (median: 0.979, min: 0.849, max: 0.998).
For the first phase, the effective half-lives vary between 0.2 h and 5.8 h. For the second phase, they vary between 1.6 h and 34.6 h.
Image-based method
Thirteen patients and seventeen treatments were studied for the influence of the model on the median absorbed dose to the bone marrow calculated with the image-based method (Table 4).
The goodness of fit of the models was measured using R2. The median was 0.22 (min: −3.2, max: 0.36) for the mono-exponential model, 0.78 (min: 0.71, max: 0.99) for the bi-exponential model and 0.72 (min: −0.51, max: 0.99) for the tri-exponential model.
In four cases, the tri-exponential model gave non-physical results.
As the fitting is not good for the mono-exponential model, we did not consider this model in the rest of this article.
Differences between the two methods (image or blood) and the different exponential models are shown in Figs. 2 and 3 with the Bland–Altman plots.
It was not possible to find a relationship between the doses calculated with these two methods that would be usable for all the patients (Table 4). One example of the plots for a patient is given in Additional file 1: Figures S6 and S7.
Influence of late timepoints
Blood-based method
To investigate the influence of the late timepoints in the blood-based method, we excluded the timepoints collected after 24 h in 45 treatments (Table 5).
The Bland–Altman plots to compare the influence of the late timepoints with the blood-based method are given in Fig. 4 for the bi-exponential model and Fig. 5 for the tri-exponential model. The plot for the mono-exponential model is not provided as it was not relevant (no difference).
Image-based method
To study the influence of the late timepoints in the image-based method, we excluded the fourth image in 11 treatments. The relative difference in the absorbed dose in bone marrow calculated with the bi-exponential model varied in most patients from −58.9 to 78%. In one patient, the dose varied from 0.32 to 1.3 Gy (311%). In another patient, it varied from 0.36 to 2.9 Gy (715%) by deleting the fourth timepoint.
Discussion
In this retrospective study, we compared the image- and blood-based methods and used three models to calculate the absorbed dose in bone marrow after 177Lu-DOTATATE therapy. Three exponential models were studied for the blood-based method and the image-based method. The latter was limited by the small number of treatments.
The median absorbed dose ranged from 15.3 to 63.9 mGy/GBq depending on the method used, which is coherent with the median literature value of 50 mGy/GBq (range 2 to 150 mGy/GBq) [6] (see Table 1). With the blood-based method, the tri-exponential model gave a higher median absorbed dose than the bi-exponential model, which also gave a higher median dose than the mono-exponential model. The tri-exponential model was not always accurate and sometimes gave an infinite AUC, that is maybe due to the low number of points especially for the image-based method where we only have 4 points [32].
Like Page et al. [11] or Beykan et al. [33] who found that blood-based bone marrow absorbed doses were by a factor of three lower than image-based bone marrow absorbed doses, we observed that the absorbed dose in bone marrow calculated with the image-based method was systematically higher than that calculated with the blood-based method. This result was obtained whatever the model used. Hemmingsson et al. who found similar results, explain it by the presence of somatostatin-receptor type 2 on CD34-positive hematopoietic stem cells in the red marrow that causes a specific uptake in the red marrow through late elimination [34].
Lubberink et al. [35] showed a fast metabolism of 177Lu-DOTATATE: the fraction of intact Lutathera decreased rapidly during the first 24 h with the major part of radioactivity consisting of smaller metabolites. This finding could explain the much higher concentrations in bone marrow than in blood and so the much higher bone marrow-absorbed doses found for image-based than for blood-based dosimetry. Another element could be taken in consideration to explain these results: the transchelation competition of the DOTA chelator, used to link the radioisotope in 177Lu-DOTATATE, with the transferrin present in the blood perturbing the in vivo stability of 177Lu-DOTATATE [36]. What we know is that in addition to circulating blood, there is an expression of somatostatin receptors on lymphocytes and activated leukocyte subtypes involved in haematological toxicity [37, 38].
The lowest bias between the two methods was obtained when using a bi-exponential model with the image-based method, very likely because the blood TAC follows a bi-phasic pattern [39]. We also observed a loss of accuracy between the models when the doses increase. Unfortunately, we did not find a systematic relationship between the two methods because as Hemmingsson et al. concluded [34], it is highly patient-dependent. However, this result needs to be confirmed with more data.
Like Page et al. [11] or Hagmarker et al. [7], we observed that the way the absorbed dose was estimated had a great impact on the results. To the best of our knowledge, it is impossible to determine which value is the most reliable as the bone marrow dosimetry is the most challenging [40] and in 177Lu-DOTATATE therapy, it is not systematically linked to biological effects and toxicity prediction. Garske-Roman et al. [8] found that bone marrow dosimetry did not predict toxicity and Forrer et al. [9] that no conclusions can be drawn concerning the relationship between calculated bone marrow absorbed dose and risk of developing myelodysplastic syndrome. On the contrary, Hagmarker et al. [7] found a correlation between bone marrow absorbed dose and platelets count decreasing and Svensson et al. [18] a correlation between bone marrow absorbed dose and haematological toxicity.
The influence of the late timepoints seemed lesser with the blood-based method for points sampled after one day and using the mono or bi-exponential model, which is contrary to the literature [6]. On the other hand, a late timepoint is important when using the tri-exponential model as it tries to cover all the relevant part of the time activity curve. Late timepoints are required with the image-based method to obtain a relevant result.
Based on these data, it would now be interesting to use a population-based pharmacokinetic model to assess the absorbed dose in bone marrow after 177Lu-DOTATATE administration and to compare the findings with our results obtained by standard practices using image-based dosimetry and the blood-based method.
Conclusion
By comparing different methods and models for the peptide receptor radionuclide therapy of gastroenteropancreatic neuroendocrine tumors using 177Lu-DOTATATE, we confirmed that the blood-based method estimates the bone marrow dose significantly lower than the image-based method. If the blood-based method is used, a bi-exponential model proved particularly useful as the estimated bone marrow dose with sampling time after 24h post-injection was not different from the one estimated without sampling time after 24 h post-injection. This method is more accessible as it takes less time for the patient and the gamma camera’s availability so the cost is reduced. Nevertheless, this blood-based method is based on an assumption that needs to be more validated.
As a result, the important difference between the two methods does not allow to determine the optimal one to estimate the true absorbed dose and further studies are necessary to compare with biological effects.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AUC:
-
Area under the curve
- MDS:
-
Myelodysplastic syndrome
- NET:
-
Neuroendocrine tumors
- PRRT:
-
Peptide receptor radionuclide therapy
- TAC:
-
Time activity curve
References
Strosberg J, El-Haddad G, Wolin E, Hendifar A, Yao J, Chasen B, et al. Phase 3 trial of 177Lu-dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376:125–35.
Bodei L, Cremonesi M, Grana CM, Fazio N, Iodice S, Baio SM, et al. Peptide receptor radionuclide therapy with 177Lu-DOTATATE: the IEO phase I-II study. Eur J Nucl Med Mol Imaging. 2011;38:2125–35.
Sonbol MB, Halfdanarson TR, Hilal T. Assessment of therapy-related myeloid neoplasms in patients with neuroendocrine tumors after peptide receptor radionuclide therapy: a systematic review. JAMA Oncol. 2020;6:1086–92.
Bodei L, Kidd M, Paganelli G, Grana CM, Drozdov I, Cremonesi M, et al. Long-term tolerability of PRRT in 807 patients with neuroendocrine tumours: the value and limitations of clinical factors. Eur J Nucl Med Mol Imaging. 2015;42:5–19.
Sabet A, Ezziddin K, Pape U-F, Ahmadzadehfar H, Mayer K, Pöppel T, et al. Long-term hematotoxicity after peptide receptor radionuclide therapy with 177Lu-octreotate. J Nucl Med. 2013;54:1857–61.
Sjögreen Gleisner K, Chouin N, Gabina PM, Cicone F, Gnesin S, Stokke C, et al. EANM dosimetry committee recommendations for dosimetry of 177Lu-labelled somatostatin-receptor- and PSMA-targeting ligands. Eur J Nucl Med Mol Imaging. 2022 [cited 2022 Apr 6]; Available from: https://doi.org/10.1007/s00259-022-05727-7.
Hagmarker L, Svensson J, Rydén T, van Essen M, Sundlöv A, Gleisner KS, et al. Bone marrow absorbed doses and correlations with hematologic response during 177Lu-DOTATATE treatments are influenced by image-based dosimetry method and presence of skeletal metastases. J Nucl Med. 2019;60:1406–13.
Garske-Román U, Sandström M, Fröss Baron K, Lundin L, Hellman P, Welin S, et al. Prospective observational study of 177Lu-DOTA-octreotate therapy in 200 patients with advanced metastasized neuroendocrine tumours (NETs): feasibility and impact of a dosimetry-guided study protocol on outcome and toxicity. Eur J Nucl Med Mol Imaging. 2018;45:970–88.
Forrer F, Krenning EP, Kooij PP, Bernard BF, Konijnenberg M, Bakker WH, et al. Bone marrow dosimetry in peptide receptor radionuclide therapy with [177Lu-DOTA0, Tyr3]octreotate. Eur J Nucl Med Mol Imaging. 2009;36:1138.
Lassmann M, Hänscheid H, Chiesa C, Hindorf C, Flux G, Luster M. EANM dosimetry committee series on standard operational procedures for pre-therapeutic dosimetry I: blood and bone marrow dosimetry in differentiated thyroid cancer therapy. Eur J Nucl Med Mol Imaging. 2008;35:1405.
Page ER. Impact of 3D image based dosimetry on treatment planning in Peptide Receptor Radionuclide Therapy (PRRT). 381.
Kwekkeboom DJ, Willem H. Bakker, Peter P. M. Kooij, Mark W. Konijnenberg, Ananth Srinivasan, Jack L. Erion, et al. [177Lu-DOTA0,Tyr3]octreotate: comparison with [111In-DTPA0]octreotide in patients. Eur J Nucl Med. 2001;1319–25.
Wehrmann C, Senftleben S, Zachert C, Müller D, Baum RP. Results of individual patient dosimetry in peptide receptor radionuclide therapy with 177Lu DOTA-TATE and 177Lu DOTA-NOC | cancer biotherapy and radiopharmaceuticals. Cancer Biotherapy & Radiopharmaceuticals. 2007 [cited 2022 Nov 22]; https://doi.org/10.1089/cbr.2006.325
Jackson PA, Beauregard J-M, Hofman MS, Kron T, Hogg A, Hicks RJ. An automated voxelized dosimetry tool for radionuclide therapy based on serial quantitative SPECT/CT imaging. Med Phys. 2013;40:112503.
Sandström M, Garske-Román U, Granberg D, Johansson S, Widström C, Eriksson B, et al. Individualized dosimetry of kidney and bone marrow in patients undergoing 177Lu-DOTA-octreotate treatment. J Nucl Med. 2013;54:33–41.
Denoyer D, Lobachevsky P, Jackson P, Thompson M, Martin OA, Hicks RJ. Analysis of 177Lu-DOTA-octreotate therapy-induced DNA damage in peripheral blood lymphocytes of patients with neuroendocrine tumors. J Nucl Med. 2015;56:505–11.
Bergsma H, Konijnenberg MW, Kam BLR, Teunissen JJM, Kooij PP, de Herder WW, et al. Subacute haematotoxicity after PRRT with (177)Lu-DOTA-octreotate: prognostic factors, incidence and course. Eur J Nucl Med Mol Imaging. 2016;43:453–63.
Svensson J, Rydén T, Hagmarker L, Hemmingsson J, Wängberg B, Bernhardt P. A novel planar image-based method for bone marrow dosimetry in 177Lu-DOTATATE treatment correlates with haematological toxicity. EJNMMI Phys. 2016 [cited 2017 Jan 25];3. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC5031567/
Del Prete M, Buteau F-A, Beauregard J-M. Personalized 177Lu-octreotate peptide receptor radionuclide therapy of neuroendocrine tumours: a simulation study. Eur J Nucl Med Mol Imaging. 2017;44:1490–500.
Gosewisch A, Delker A, Tattenberg S, Ilhan H, Todica A, Brosch J, et al. Patient-specific image-based bone marrow dosimetry in Lu-177-[DOTA0, Tyr3]-Octreotate and Lu-177-DKFZ-PSMA-617 therapy: investigation of a new hybrid image approach. EJNMMI Res. 2018;8:76.
Del Prete M, Buteau F-A, Arsenault F, Saighi N, Bouchard L-O, Beaulieu A, et al. Personalized 177Lu-octreotate peptide receptor radionuclide therapy of neuroendocrine tumours: initial results from the P-PRRT trial. Eur J Nucl Med Mol Imaging. 2019;46:728–42.
Santoro L, Mora-Ramirez E, Trauchessec D, Chouaf S, Eustache P, Pouget J-P, et al. Implementation of patient dosimetry in the clinical practice after targeted radiotherapy using [177Lu-[DOTA0, Tyr3]-octreotate. EJNMMI Res. 2018;8:103.
Marin G, Vanderlinden B, Karfis I, Guiot T, Wimana Z, Reynaert N, et al. A dosimetry procedure for organs-at-risk in 177Lu peptide receptor radionuclide therapy of patients with neuroendocrine tumours. Phys Med. 2018;56:41–9.
Thakral P, Sen I, Pant V, Gupta SK, Dureja S, Kumari J, et al. Dosimetric analysis of patients with gastro entero pancreatic neuroendocrine tumors (NETs) treated with PRCRT (peptide receptor chemo radionuclide therapy) using Lu-177 DOTATATE and capecitabine/temozolomide (CAP/TEM). Br J Radiol. 2018;91:20170172.
Chicheportiche A, Artoul F, Schwartz A, Grozinsky-Glasberg S, Meirovitz A, Gross DJ, et al. Reducing the number of CTs performed to monitor personalized dosimetry during peptide receptor radionuclide therapy (PRRT). EJNMMI Phys. 2018;5:10.
Hallqvist A, Svensson J, Hagmarker L, Marin I, Rydén T, Beauregard J-M, et al. Optimizing the Schedule of PARP Inhibitors in Combination with 177Lu-DOTATATE: a dosimetry rationale. Biomedicines. 2021;9:1570.
Carter LM, Ramos JCO, Kesner AL. Personalized dosimetry of 177Lu-DOTATATE: a comparison of organ- and voxel-level approaches using open-access images. Biomed Phys Eng Express. 2021;7:057002.
Vergnaud L, Giraudet A-L, Moreau A, Salvadori J, Imperiale A, Baudier T, et al. Patient-specific dosimetry adapted to variable number of SPECT/CT time-points per cycle for 177Lu-DOTATAE therapy. EJNMMI Phys. 2022;9:37.
Lambert M, Dierickx L, Brillouet S, Courbon F, Chatelut E. Comparison of two types of amino acid solutions on 177Lu-dotatate pharmacokinetics and pharmacodynamics in patients with metastatic gastroenteropancreatic neuroendocrine tumors. Curr Radiopharm. 2022;15:164–72.
Huizing DMV, Peters SMB, Versleijen MWJ, Martens E, Verheij M, Sinaasappel M, et al. A head-to-head comparison between two commercial software packages for hybrid dosimetry after peptide receptor radionuclide therapy. EJNMMI Phys. 2020;7:36.
Ferrer L, Kraeber-Bodéré F, Bodet-Milin C, Rousseau C, Gouill SL, Wegener WA, et al. Three methods assessing red marrow dosimetry in lymphoma patients treated with radioimmunotherapy. Cancer. 2010;116:1093–100.
Glass HI, de Garreta AC. The quantitative limitations of exponential curve fitting. Phys Med Biol. 1971;16:119.
Beykan, S et al. Patient-specific dosimetry of 177Lu-dotatate peptide receptor radionuclide therapy with high activities. Eur J Nucl Med Mol Imaging 2018;45(Suppl 1):S33 OP-081. 2018.
Hemmingsson J, Svensson J, Hallqvist A, Smits K, Johanson V, Bernhardt P. Specific Uptake in the Bone Marrow Causes High Absorbed Red Marrow Doses During [177Lu]Lu-DOTATATE Treatment. J Nucl Med [Internet]. 2023 [cited 2023 Sep 22]; Available from: https://jnm.snmjournals.org/content/early/2023/06/08/jnumed.123.265484
Lubberink M, Wilking H, Öst A, Ilan E, Sandström M, Andersson C, et al. In Vivo Instability of 177Lu-DOTATATE During Peptide Receptor Radionuclide Therapy. J Nucl Med. 2020;61:1337–40.
Walrand S, Jamar F. Renal and red marrow dosimetry in peptide receptor radionuclide therapy: 20 years of history and ahead. Int J Mol Sci. 2021;22:8326.
van Hagen PM, Krenning EP, Kwekkeboom DJ, Reubi JC, Anker-Lugtenburg PJ, Löwenberg B, et al. Somatostatin and the immune and haematopoetic system: a review. Eur J Clin Invest. 1994;24:91–9.
Derlin T, Bogdanova N, Ohlendorf F, Ramachandran D, Werner RA, Ross TL, et al. Assessment of γ-H2AX and 53BP1 foci in peripheral blood lymphocytes to predict subclinical hematotoxicity and response in somatostatin receptor-targeted radionuclide therapy for advanced gastroenteropancreatic neuroendocrine tumors. Cancers. 2021;13:1516.
Eberlein U, Nowak C, Bluemel C, Buck AK, Werner RA, Scherthan H, et al. DNA damage in blood lymphocytes in patients after 177Lu peptide receptor radionuclide therapy. Eur J Nucl Med Mol Imaging. 2015;42:1739–49.
Strigari L, Konijnenberg M, Chiesa C, Bardies M, Du Y, Gleisner KS, et al. The evidence base for the use of internal dosimetry in the clinical practice of molecular radiotherapy. Eur J Nucl Med Mol Imaging. 2014;41:1976–88.
Acknowledgements
The authors wish to thank Bertille Segier (IUCT-Oncopole) for helping in the statistics analysis.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
DV wrote the manuscript. SB provided input with the draft. DV, SP, SB analyzed the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
F20230102114415.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Comparison of the normalized absorbed dose to the bone marrow between the first cycle and the fourth one for 13 patients.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vallot, D., Brillouet, S., Pondard, S. et al. Impact of different models based on blood samples and images for bone marrow dosimetry after 177Lu-labeled somatostatin-receptor therapy. EJNMMI Phys 11, 32 (2024). https://doi.org/10.1186/s40658-024-00615-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40658-024-00615-5