Abstract
Background
Physician empathy is important to patients across the socio-economic spectrum. However, whether socioeconomic status (SES) influences how patients’ judge physician empathy is not known. We investigated how patients’ perceptions of their general practitioners’ (GPs) empathy related to objectively measured patient-centeredness of the GPs and their detection and response to emotional cues.
Methods
Secondary analysis of 112 videoed consultations of 8 GPs with the high and low empathy scores as rated by patients using the Consultation and Relational Empathy (CARE) Measure working in high or low deprivation settings in Scotland. Objective assessment involved the Measure of Patient-Centredness (MPCC) which has 3 components (exploring disease and illness experience, understanding the whole person, and finding common ground) and the Verona coding system (which measures emotional cues, concerns and responses).
Results
GPs rated by patients as being empathic were more patient-centred overall than those rated as less empathic, in both high (p = 0.03) and low deprivation areas (p = 0.05). In high deprivation areas, perceived empathy was related to finding common ground (p = 0.02) whereas in low deprivation areas it was related to understanding the whole person (p= 0.01). In high deprivation areas, empathic GPs also had significantly different responses to emotional cues and concerns than GPs perceived as having low empathy.
Conclusion
Socioeconomic status appears to affect how patients judge practitioner empathy. This study emphasises the importance of finding common ground and detecting and responding actively to emotional cues in consultations in high deprivation areas. Further research on a larger sample is warranted.
Similar content being viewed by others
Background
Empathy is widely regarded as a crucial attribute of healthcare professionals, and research has shown the importance of empathy in general practice consultations in achieving higher patient satisfaction, enablement, and improvement in some health outcomes [1-5]. Empathy has been defined in the clinical context as involving an ability to a) understand the patient’s situation, perspective and feelings (and their attached meanings) b) to communicate that understanding and check it’s accuracy, and c) to act on that understanding with the patient in a helpful (therapeutic) way [1]. Clinical empathy is thus closely related to the concept of patient-centred care although it is only recently that the overlap between these concepts has become more explicit [6,7].
Measuring empathy in routine consultations is usually done by patient assessment, using patient rated experience measures (PREMS). The Consultation and Relational Empathy (CARE) Measure is one widely used measure which was developed and validated in general practice in areas of both high and low socioeconomic deprivation [8,9]. Such an inclusive approach is important given the wide differences in health and healthcare needs that exist between affluent and poor areas [10]. Inequalities in health occur between affluent and poor in most countries [11], but within western Europe, Scotland has had the highest level of health inequality for many decades now [12,13]. Although the social determinants of health are the key cause of such inequality, healthcare itself is an important determinant too. Despite the provision of universal coverage of healthcare to all citizens within the United Kingdom over the last 70 years, there has long been an ‘inverse care law’ in operation, in which the provision of good quality care varies inversely with the need for it in the population served [14,15]. Because general practitioners (GPs) are not distributed in the UK according to population need, GPs working in deprived areas face higher demands, and more stress [11].
We have previously shown that GP empathy as perceived by the patient, is necessary for patient enablement in both high and low deprivation areas [16] - without empathy, enablement does not occur. However, there is currently a lack of studies that link patients’ perceptions of their GPs’ empathy (however measured) in individual consultations with observed specific consultation behaviours and responses. This may be important in order to understand how patients from differing backgrounds ‘judge’ physician empathy. Differences in this could lead to, for example, tailored specific interventions to improve perceived empathy in patients from deprived areas compared with more affluent patients.
In our previous work on a large dataset of videoed consultations in general practice in high and low deprivation areas, consultations in deprived areas were found to be less patient-centred than in affluent areas, when assessed by a validated objective observer-rated method [17]. However, this study did not explore differences in patient-centred consulting behaviours between GPs perceived as being high or low in empathy in deprived areas and affluent areas.
The detection of emotional cues and the type of response by practitioners may also be an important factor in empathic accuracy and may strengthen the therapeutic relationship between doctor and patient [18-20]. Cues are verbal or non-verbal hints exhibited by patients which suggest an underlying unpleasant emotion, and have been found to be very common in general practice consultations [20]. How the detection and response to such cues by GPs relates to patients’ views of the GPs’ empathy, in high and low deprivation settings, is not known.
The aim of the current study was to explore whether and how patients’ perceptions of the GPs’ empathy in consultations in high and low deprivation areas relates to a) observer-rated patient-centred behaviours and b) the detection and responses of the GPs to patients emotional cues and concerns.
Methods
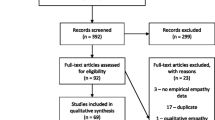
The study objectives were investigated by means of a secondary analysis of data collected between 2006–2008 by Mercer and colleagues as part of a research project on the consultation in general practice in areas of high and low deprivation which we have previously described [17]. Ethical approval for the study was obtained from the Local Research Ethics Committee and informed consent was gained from all participating GPs and patients. The original study was funded by the Chief Scientist Office of the Scottish Government (CSO Ref: CZH/4/267). It was independently reviewed and given a favourable opinion by the local research ethics committee in Scotland, UK (approval number: REC/06/SO701/43).
Consultation data
Practices were recruited from the upper and lower quartile of deprivation (Scottish Index of Multiple Deprivation, SIMD 2006) in the Greater Glasgow and Clyde Area, Scotland, UK [17]. The mean deprivation score for all practices in the upper quartile was 49 (range 41–62) and 14 (range 5–22) for the lower quartile. The full study involved 20 practices, 47 GPs and 659 patients in whom consultations were videoed and CARE Measure scores were collected immediately afterwards (13 practices, 25 GPs, 356 patients in high deprivation areas and 7 practices, 22 GPs, 303 patients in low deprivation areas) as previously described [17]. The mean deprivation (SIMD) scores of the participating practices were 46 (range 41–58) in the high deprivation group and 13 (range 5–22) in the low deprivation group, thus closely matching the mean scores of all practices in the two quartiles shown above. The mean SIMD scores of the participating patients in the original study was 49 (SD 20) and 14 (SD 15) in the high and low deprivation groups, respectively. For the current secondary analysis, the 47 GPs were ranked according to their mean CARE measure scores and the two GPs with the highest and the two with the lowest perceived empathy scores (mean CARE Scores) in both high and low deprivation groups were selected (thus 8 GPs in total) and all their recorded consultations included (112 in total). The mean deprivation scores of the participating patients in the current study were 52 (SD 22) and 10 (SD 8) in the high and low deprivation groups, respectively. Thus there is clear evidence of representativeness in terms of deprivation level at all levels of the previous and current study.
Analysis
Patient-centred behaviour was assessed by the Measure of Patient-Centred Communication (MPCC) which consists of three components (exploring disease and illness experience, understanding the whole person, and finding common ground) which are added to give a total score [21]. The coding of the consultations had been carried out as previously reported [17].
The patients emotional cues and concerns and GP responses were measured using the Verona Emotional Sequences of cues and concerns (Verona-CoDES-CC) system, which is an in-depth system that enables rigorous, detailed descriptive coding of patients cues and concerns. Cues can be verbal or non verbal hints that allows a patient to suggest an unpleasant underlying emotion. Concerns are defined as clear and unambiguous expressions of an unpleasant current or recent emotion where the emotion is explicitly verbalized and health practitioners’ responses refer to the immediate of delayed response the GP gives to a patient elicited cue or concern [22] (Figure 1).
Verona-CoDES-CC, coding provider responses (Del Piccolo et al. [ 22 ] ).
Each of the consultations was analysed for cues, concerns and responses using the following steps:
-
1.
Each consultation was transcribed verbatim. Notes were added to the transcription that provided them with points of reference and context to behaviours that were being carried out either by the patient or the practitioner during the consultation.
-
2.
Two coders (one student, JML and one researcher, MH) were trained in using the Verona-CoDes-CC by an originator of the system (GH) who also provided on-going expertise and advice.
-
3.
Inter-rater reliability was measured for cues , concerns and health provider responses using Cohen’s Kappa [23] on 20 consultations. Two cycles of inter rater reliability were undertaken to measure on an utterance by utterance scale. Overall the coders (JML and MH) achieved an excellent inter-rater reliability score for cues, concerns (0.95 respectively) and health provider responses (0.91). The achieved inter rater reliability scores were above average when compared to previous studies using the Verona coding system [24-26].
The cycles of inter rater reliability took place between September 2009 and January 2010. The remaining study coding of the 112 consultations was undertaken between January and August 2010. In the current analysis we explore health practitioners response to the second level shown in Figure 1 (i.e., explicit and non-explicit, inviting and non-inviting).
Statistical analysis was carried out using SPSS version 18. Differences between groups were assessed by the appropriate parametric and non-parametric tests.
Results
Patient and consultations characteristics
Patients in the high and low GP empathy (CARE measure) groups showed no significant difference in the mean ages in the low deprivation group but in the high deprivation group the mean age of patients in the low CARE group was significantly lower than in the high CARE group (Table 1). There was no significant difference in gender distribution between the high and low empathy groups. The extent of the difference in perceived GP empathy (mean CARE measure scores) between the high and low CARE groups in both low and high deprivation groups is also shown in Table 1. Consultation length did not differ significantly between the high and low empathy GPs in either setting (results now shown).
GPs patient-centredness in the consultation
Table 2 shows the observed patient-centredness of the GPs in the consultation using the MPCC. Total scores were higher in the GPs in the high empathy group compared with the low empathy group in affluent (p = 0.05) and deprived (p = 0.03) areas. In terms of the three components of the MPCC, component 1 (exploring disease and illness experience) was not significantly different between high and low empathy GPs in either affluent or deprived areas. Component 2 (understanding the whole-person) was significantly higher in the high empathy GPs compared with the low empathy ones in the affluent areas but not in the deprived. Component 3 (finding common ground), conversely, was significantly higher in the high empathy GPs in the deprived areas compared with low empathy GPs, but this was not found in the affluent areas (Table 2).
Patient’s emotional cues, concerns and GP responses in the consultation
Table 3 shows the coded emotional cues and concerns in high and low empathy (CARE Measure) consultations. Cues were more common than expressed emotional concerns in all groups. The number of cues (p = <0.001) and concerns (p = 0.02) was significantly higher in the high empathy GP consultations compared with the low empathy GPs in the high deprivation group. However, this difference was not observed in the low deprivation group.
In terms of the observed GP responses to these cues and concerns, there were significantly more inviting (code I) health provider responses in the high empathy GP consultations compared with the low empathy GPs in the high deprivation setting (Table 3). This was mainly due to more inviting non-explicit responses (code IN) (Figure 2). There were also more non-inviting responses (code N) in the high empathy consultations than low empathy on the deprived setting, although this was much less common than the inviting responses (Figure 2).
Discussion
In this secondary analysis of 112 videoed consultations we have found that GPs rated by patients as being empathic were generally more patient-centred overall than those rated as less empathic. In high deprivation areas, perceived empathy was significantly related to finding common ground in the consultation whereas in low deprivation areas it was significantly related to understanding the whole person. In high deprivation areas, empathic GPs also had significantly different responses to emotional cues and concerns than GPs perceived as having low empathy. Thus we have found evidence to suggest that patients of differing socioeconomic status use different criteria within consultations when judging the GPs empathy.
Results in relation to previous studies
We are not aware of any previous studies that have triangulated patients’ perceptions of physician empathy with observed measures of patient-centred behaviour. Patient centeredness in GP consultations has however been previously linked with improved patient trust [27], patient satisfaction [28], and improved outcomes [29,30]. We are also not aware of any studies that have used the Verona coding system to assess emotional cues and concerns, and practitioners responses in high and low deprivation setting, nor related this to patients’ perceptions of GP empathy. It is well established within the literature that patient express more cues than concerns within the consultation setting [24-26,31] and this was confirmed in the present study.
More Inviting (I) yet not always explicitly stated health provider responses were associated with patient’s perceptions of empathy in the high deprivation group. This finding suggests that in the deprived areas the way the GP responds to emotional cues is positively associated with patient perceptions of empathy.
Strengths and limitations
A major strength of the present study was the availability of both videoed consultations and patients’ views of the GPs empathy measured by a self-reported validated questionnaire (CARE Measure) on the same consultations. This enabled triangulation of perceived views with observed behaviours. In addition the availability of data from consultations in areas of high or low deprivation added to the richness of the dataset. Although the sample size was modest, the coding of both patient-centredness (using the MPCC) and the patient’s emotional cues and concerns and GPs responses (Verona-CoDES-CC) represented a considerable amount of effort of the part of the researchers.
However, the weaknesses include the fact that it was a retrospective secondary analysis with a small l and highly selected sample and cannot therefore be regarded as necessarily representative of the setting and context. Thus generalizability cannot be assumed and further research is warranted. The analysis was descriptive, and should be regarded as a first step in exploring interesting potential differences in how patients from different socioeconomic levels perceived GP empathy.
Implications for practice and future research
The implications of this research for practice are that GPs may need to learn to use different consultation behaviours when consulting in areas of high or low deprivation. This has implications for training, and also for issues of time and continuity, and need to be viewed in the broader context of health inequalities and the inverse care law [10,14,15].
Future research should use more robust statistical methods including multi-level modelling and multi-regression analysis, on a substantially larger sample, which was outwith the scope of the current study (which was part of a postgraduate research degree). With regard to the Verona Coding definitions of Emotional Sequences for cues and concerns (Verona-CoDES-CC), future research could build upon the analyses of sequences of consultations already reported [32]. The purpose of this approach would be to assess if patterns of cues lead to trends in health provider responses not only within the single consultation but also over a series of meetings between the same patients and practitioners, or for certain types of consultations (i.e. emotional compared with physical complaints).
Conclusions
In this retrospective secondary analysis of 112 videoed consultations we have found that GPs rated by patients as being empathic were generally more patient-centred overall than those rated as less empathic. In high deprivation areas, perceived empathy was significantly related to finding common ground in the consultation whereas in low deprivation areas it was significantly related to understanding the whole person. In high deprivation areas, empathic GPs also had significantly different responses to emotional cues and concerns than GPs perceived as having low empathy. Thus we have found evidence to suggest that patients of differing socioeconomic status use different criteria within consultation when judging the GPs empathy with a standard validated tool. This has implications for the training of GPs in communication skills. Further work, using more robust analysis on a larger sample is warranted however as generalizability from such a limited and selected sample cannot be assumed.
References
Mercer SW, Reynolds S. Empathy and quality of care. Br J Gen Pract. 2002;52(Suppl):S9–12.
Neumann M, Bensing J, Mercer SW, Ermstmann N, Ommen O, Pfaff H. Analyzing the “nature” and “specific effectiveness” of clinical empathy: A theoretical overview and contribution towards a theory-based research agenda. Patient Educ Couns. 2009;74(3):339–46.
Hojat M. Ten Approached for enhancing empathy in Health and Human Services Cultures. J Health Hum Serv Adm. 2009;31(4):412–50.
Jani BD, Blane DN, Mercer SW. The role of empathy in therapy and the physician-patient relationship. Res Complement Med. 2012;19(5):2–6.
Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract. 2013;63(606):e76–84.
Stewart M, Fortin M. Multimorbidity and patient-centred care, pp 22–25. In: Mercer SW, Salisbury C, Fortin M, editors. The ABC of Multimorbidity. Oxford: Wiley-Blackwell; 2014. ISBN-10: 111838885; ISBN-13: 978–1118383889.
Bikker AP, Cotton P, Mercer SW. Embracing Empathy in Healthcare. A universal approach to person-centred, empathic healthcare encounters. London, New York: Radcliffe; 2014. ISBN-13: 978 190936 8187.
Mercer SW, Maxwell M, Heaney D, Watt GCM. The consultation and relational empathy (CARE) measure: development and preliminary validation and reliability of an empathy-based consultation process measure. Fam Pract. 2004;21(6):699–705.
Mercer SW, McConnachie A, Maxwell M, Heaney D, Watt GCM. Relevance and practical use of the Consultation and Relational Empathy (CARE) Measure in general practice. Fam Pract. 2005;22(3):328–34.
Mercer SW, Watt GCM. The inverse care law: clinical primary care encounters in deprived and affluent areas of Scotland. Ann Fam Med. 2007;5(6):503–10.
Commission on Social Determinants of Health. Closing the gap in a generation. Health equity through action on the social determinants of health. Geneva: World Health Organisation; 2008.
Audit Scotland. Health inequalities in Scotland. 2012. Available at: http://www.auditscotland.gov.uk/docs/health/2012/nr_121213_health_inequalities.pdf.
The Scottish Government. Long-term Monitoring of Health Inequalities: Headline Indicators. 2012. Available at: http://www.scotland.gov.uk/Resource/0040/00406782.pdf.
Hart JT. The inverse care law. Lancet. 1971;297:405–12.
Watt G. The inverse care law today. Lancet. 2002;360:252–4.
Mercer SW, Jani B, Wong SY, Watt GCM. Patient enablement requires physician empathy: a cross-sectional study of general.practice consultations in areas of high and low socioeconomic deprivation in Scotland. BMC Fam Pract. 2012;13:6.
Jani, B., Bikker, A., Higgins, M., Fitzpatrick, B., Little, P., Watt, G.C.M.,et al. Patient-centeredness and the outcome of consultations with depressed patients in areas of high and low socioeconomic deprivation. Br J Gen Pract, 2012; DOI: 10.3399/bjgp12X653633.
Zimmermann C, Del Piccolo L, Finset A. Cues and concerns by patients in medical consultations: a literature review. Psychol Bull. 2007;133(3):438–63.
Levenstein JH, McCracken HE, McWhinney IR, Stewart B, Brown JB. The patient centred clinical method; a model for the doctor patient interaction in family medicine. Fam Pract. 1986;3(1):24–30.
Suchman AL, Markakis K, Beckman HB, Frankel R. A model of empathic communication in the medical interview. J Am Med Assoc. 1997;277(8):678–82.
Brown, J. D., Stewart, M., Ryan, B.L. Assessing communication between patients and physicians: The measure of patient-centred communication (MPCC). Thames Valley Family Practice Research Unit and Centre for Studies in Family Medicine. 2001. Working Paper Series, Papers 95–2, Second Edition.
Del Piccolo L, Finset A, Zimmermann C. Verona coding definitions of emotional sequences (VR-Codes): cues and concerns manual. 2009. Available at: http://www.each.nl/verona-coding-systems. (Accessed: 07/01/13).
Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46.
Oguchi M, Jansen J, Butow P, Colagiuri B, Divine R, Dhillion H. Measuring the impact of nurse cue-response behaviour on cancer patients’ emotional cues. Patient Educ Couns. 2010;82(2):163–8.
Eide H, Sibbern T, Egeland T, Finset A, Johannessen T, Miaskowski C, et al. Fibromyalgia patients’ communication of cues and concerns: interaction analysis of pain clinic consultations. Clin J Pain. 2011;27(7):602–10.
Zimmermann C, Del Piccolo L, Bensing J, Bergvik S, De Haes H, Eide H, et al. Coding patient emotional cues and concerns in medical consultations: the Verona coding definitions of emotional sequences (VR-CoDES). Patient Educ Couns. 2011;82(2):141–8.
Fiscella K, Meldrum S, Franks P, Shields CG, Duberstein P, McDaniel SH, et al. Patient trust: is it related to patient-centered behaviour of primary care physician? Med Care. 2004;42(11):1049–55.
Kinnersley P, Stott N, Peters T, Harvey I. The patient-centredness of consultations and outcome in primary care. Br J Gen Pract. 2000;49:11–6.
Little P, Everitt H, Williamson I, Warner G, Moore M, Gould C, et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. Br Med J. 2001;323:908–11.
Stewart M, Brown JB, Donner A, McWhinney IR, Oates J, Weston WW, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49(9):796–804.
Vatne T, Finset A, Ornes K, Ruland CM. Application of the verona coding definitions of emotional sequences (VR-CoDES) on a pediatric data set. Patient Educ Couns. 2010;80(3):399–404.
Zhou Y, Collinson A, Laidlaw A, Humphris G. How do medical students respond to emotional cues and concerns expressed by simulated patients during OSCE consultations? – a multilevel study. PLoS ONE. 2013;8(10):e79166.
Acknowledgements
We would like to thank the patients and practitioners who agreed to take part in the study. This study was supported by a University’s General Fund awarded to SWM to fund a PHD programme by J.M. Lundy. SWM was part-funded by the Scottish School of Primary Care.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
SWM, GCW, PL planned and led the original study and SWM, JML, GCW, and GMH planned the current secondary analysis. AB and MH carried out the analysis of the videos using the MPCC, with input from PL and SWM. JML carried out the analysis of the videos using Verona with training provided by GMH and inter-rater reliability checks done by MH. All authors contributed to the writing of the paper after the initial draft which JML and SWM wrote. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Lundy, JM., Bikker, A., Higgins, M. et al. General practitioners’ patient-centredness and responses to patients’ emotional cues and concerns: relationships with perceived empathy in areas of high and low socioeconomic deprivation. J of Compassionate Health Care 2, 2 (2015). https://doi.org/10.1186/s40639-015-0011-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40639-015-0011-6