Abstract
Introduction
Intravenous oxygen therapeutics present an appealing option for improving arterial oxygenation in patients with acute hypoxemic respiratory failure, while limiting iatrogenic injury from conventional respiratory management.
Methods
We used an established two-hit murine model of acute lung injury (ARDS/VILI) to evaluate the effect of intravenous dodecafluoropentane (DDFPe) on oxygen saturation and bronchoalveolar lavage cell counts and protein levels. Twenty hours after challenge with intratracheal lipopolysaccharide, mice were intubated and ventilated with high tidal volumes (4 h) to produce acute lung injury. DDFPe (0.6 mL/kg) or saline was administered by IV bolus injection at the initiation of mechanical ventilation and again at 2 h. Oxygen saturation was measured every 15 min. Bronchoalveolar lavage was performed at the conclusion of the experiment.
Results
The two-hit ARDS/VILI model produced substantial inflammatory acute lung injury reflected by markedly increased bronchoalveolar lavage (BAL) cell counts compared to BAL cell counts in spontaneous breathing controls (5.29 ± 1.50 × 10–6 vs 0.74 ± 0.014 × 10–6 cells/mL) Similarly, BAL protein levels were markedly elevated in ARDS/VILI-challenged mice compared with spontaneous breathing controls (1109.27 ± 223.80 vs 129.6 ± 9.75 ng/mL). We fit a linear mixed effects model that showed a significant difference in oxygen saturation over time between DDFPe-treated mice and saline-treated mice, with separation starting after the 2-h injection. DDFPe-treated ARDS/VILI-challenged mice also exhibited significant reductions in BAL cell counts but not in BAL protein.
Conclusion
DDFPe improves oxygen saturation in a murine model of ARDS/VILI injury with the potential for serving as an intravenous oxygen therapeutic.
Similar content being viewed by others
Introduction
Perfluorocarbons are low molecular density molecules that are uniquely both hydrophobic and lipophobic and can dissolve large volumes of gas [1]. When emulsified with surfactant, the perfluorocarbon emulsion provides an opportunity for intravenous oxygen transport. This could be potentially useful in oxygenation threatening diseases from embolism (e.g., stroke, heart attack), hemorrhage, or acute lung injury. Acute lung injury, especially the most severe form–acute respiratory distress syndrome, presents significant clinical challenges during noninvasive respiratory support, preoxygenation for tracheal intubation, and during mechanical ventilation largely because of ventilation:perfusion mismatch and intrapulmonary shunt.
Intravenous perflurocarbons are a potential novel solution for these challenges posed by acute lung injury. While intratracheal perfluorocarbons have shown harm in clinical trials for liquid ventilation, [2] intravenous perfluorocarbons have potential as a small particle oxygen therapeutic. Dodecafluoropentane emulsion (DDFPe) [NanO2™, NuvOx Pharma (Tucson, AZ)] is one such promising perfluorocarbon. DDFPe, is 2% weight/volume dodecafluoropentane emulsion, with a lower boiling point, higher oxygen carrying capacity at lower doses, and improved safety profile compared to previous perfluorocarbons, [3, 4] which make it an ideal candidate for intravenous O2 delivery [5]. In this study, we used an established preclinical model of acute lung injury to evaluate the potential of DDFPe to improve oxygen saturation in conditions of low ventilation:perfusion and high intrapulmonary shunt.
Methods
Murine model
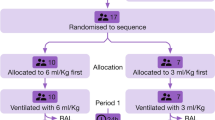
We used an established two-hit mouse model of acute lung injury for these experiments [6, 7] to model acute respiratory distress syndrome with hypoxemia to evaluate the effect of bolus doses of DDFPe on oxygen saturation, and to avoid using an unestablished model of apnea. C57BL/J6 male mice (n = 14, 8–10 weeks) were used for the experiments. Twelve mice were anesthetized with intraperitoneal ketamine (100 mg/kg) and xylazine (5 mg/kg), and then intubated with a 20-gauge intravenous catheter. Lipopolysaccharide (0.5 mg/kg) was then given by intratracheal injection, mice were extubated and allowed to recover for 20 h. After the recovery period, the mice were re-sedated with ketamine and xylazine by intraperitoneal injection, with additional doses and bupremorphone (0.3 mg/kg) given as needed for pain and to ensure deep sedation during the experiment, reintubated and placed on a mechanical ventilator (Harvard Apparatus, Boston, MA).
At the onset of mechanical ventilation, mice were randomly assigned to injection with either DDFPe (0.6 mL/kg) or an equivalent volume of saline (n = 6/group) into the surgically exposed right jugular vein. A second bolus was given at 120 min. Mice were ventilated to induce ventilator-induced lung injury (VILI) throughout the experiment by using a tidal volume of 30 mL/kg, respiratory rate of 75 breaths/min, and ambient FiO2 without positive end-expiratory pressure for four hours. Handlers were not blinded to treatment assignment.
Oxygen saturation was continuously monitored using the MouseStat® monitor (Kent Scientific Corporation, Torrington, CT) on the pad of a hind leg paw and measurements were recorded as an average over 30 s every 15 min. We fit a linear mixed effects model to the oxygen saturation data with a random intercept per mouse, and conducted linear hypothesis tests of group differences at each time point using Kenward–Roger adjustments to the denominator degrees of freedom and standard errors.
At the termination of each experiment (after 4 h of mechanical ventilation), bronchoalveolar lavage (BAL) fluid was collected by instilling 1 mL of HBSS (Invitrogen, Grand Island, NY) through the tracheal catheter, followed by slow recovery of the fluid. The remaining two mice did not undergo any study interventions (i.e., anesthesia and intubation for LPS injection, or mechanical ventilation), except anesthesia to facilitate bronchoalveolar lavage. Cells were recovered from the resulting bronchoalveolar lavage fluid by centrifugation (500 g, 20 min, 4 °C) and counted using an automated cell counter (TC20; Bio-Rad, Hercules, CA). BAL indices are reported as mean ± standard deviation and compared using a student’s t test. All animal care procedures and experiments were approved by the University of Arizona Animal Care and Use Committee (Approval #13-490).
Results
The two-hit model produced the predicted inflammatory acute lung injury with an increased bronchoalveolar lavage cell count in the DDFPe (3.08 ± 0.88 cells/mL, n = 6) and saline (5.29 ± 1.50 cells/mL, n = 6) groups compared to spontaneous breathing unexposed control mice [0.74 ± 0.014 × 10–6 cells/mL, (n = 2)]. Mice exposed to ARDS/VILI also exhibited an increase in BAL protein compared to spontaneous breathing unexposed control mice [DDFPe: 996.89 ± 246.8, saline: 1109.27 ± 223.80 vs 129.6 ± 9.75) ng/mL]. Examination of BAL protein values showed no difference in protein content between the saline-treated and the DDFPe-treated groups but a significant reduction in BAL cell count in mice receiving DDFPe (Fig. 1).
Bronchoalveolar lavage analysis at the end of the experiment demonstrated an inflammatory acute lung injury with the two-hit model for both saline-treated and DDFPe-treated mice (n = 12) compared to spontaneously breathing mice that were not exposed to LPS injection or mechanical ventilation (n = 2). There was a statistically significant decrease in cell count (p = 0.01) with DDFPe-treated mice compared to saline-treated mice (dashed line, left panel), but no difference in protein concentration (p = 0.33) (right panel). Error bars represent standard deviation
Oxygen saturation measurements were variable between mice at each measurement (Fig. 2). The mean oxygen saturation at the initiation of mechanical ventilation was 95–96% for both the saline-control group and the DDFPe-treated group, but steadily declined to a mean of 91% for saline controls and 89% for DDFPe-treated mice over the first 2 h. After 4 h of ARDS/VILI exposure, the mean oxygen in the saline-treated group fell further to 76% with a mean 4 h difference of − 19%. In contrast, mean oxygen saturation levels in the DDFPe treated group exhibited a mean 4 h difference of -10%. In the linear mixed effects model, there was an overall significant difference between the DDFPe-treated and saline-treated mice (p < 0.001), and the linear estimates show separation between the groups starting at the 2-h dose (Table 1).
Oxygen saturations over time for mice treated with saline (red) and mice treated with DDFPe (blue), n = 6 for each group. Raw data are presented (thin lines) along with overlayed model estimates (thick). Time zero is the initiation of mechanical ventilation with injurious tidal volumes, 20 h after intratracheal lipopolysaccharide injection. DDFPe or saline was given at 0 and 120 min
The change in oxygen saturation after the dose of DDFPe or saline at 2 h under hypoxemic conditions was interesting. The difference between the mean O2 saturation immediately prior to injection and the mean O2 saturation after injection in the control saline group was − 7.5% (91% and 83%, respectively), whereas mean O2 saturation in the NanO2 treated group rose from 89% to 91%, mean difference + 2.5%, net difference 10% [95% CI: 2.7,17.3], p = 0.01).
Discussion
These results show that in a ‘two-hit’ model of acute lung injury, intravenously administered DDFPe improved oxygen saturation. The mice had similarly declining oxygen saturation trajectories until 2 hours when the second injection of DDFPe while hypoxemic rapidly increased oxygen saturation and changed the trajectory for the remainder of the experiment. These results indicate that DDFPe is a viable candidate for an intravenous oxygen therapeutic. Although the mechanism of action is not completely understood, DDFPe appears to improve arterial oxygen content despite disruptions in ventilation:perfusion mismatch induced by both endothelial (lipopolysaccharide) and epithelial injury (volutrauma).
It is interesting that a reduction in bronchoalveolar lavage cell count, but not total protein was observed in DDFPe-treated mice compared to controls. One hypothesis is that DDFPe may reduce oxidative stress leading to reduced cellular infiltration but not affecting capillary leak. This is aligned with a study by Hou and colleagues that showed perfluorooctyl bromide (Oxygent) reduced pulmonary edema and inflammatory cellular infiltration, and improved PaO2 when given prophylactically in an LPS induced acute lung injury model [8]. In our study, LPS induced injury had progressed for 20 h before the onset of the “second hit” of injurious mechanical ventilation. However, this hypothesized mechanism for DDFPe requires further exploration as a possible alternative explanation is less severe injury in the DDFPe-treated mice.
DDFPe has demonstrated efficacy in preclinical models in reducing cerebral damage from acute ischemic stroke, [9,10,11,12] and decreasing myocardial damage in acute myocardial infarction [13]. DDFPe was also shown to rapidly improve PaO2 in a porcine model of intrapulmonary shunt induced by bead instillation into the bronchial tree [14], as well as improve tissue hypoxia in preclinical hemorrhage, stroke, and acute chest syndrome models [11, 15, 16]. Our results add to the existing preclinical studies demonstrating the potential for DDFPe to restore systemic oxygenation and attenuate hypoxic tissue injury. In addition, DDFPe can be administered repeatedly to restore oxygenation [14], which increases the therapeutic utility for treating acute hypoxemic respiratory failure across the spectrum of disease.
The improvement in oxygen saturation seen in this study is a potentially clinically translatable option for overcoming the challenges imposed by ventilation:perfusion mismatch and shunt in patients with acute hypoxemic respiratory failure. Tracheal intubation in particular is dangerous in this patient population, as it carries significant risk of oxygen desaturation leading to peri-intubation cardiac arrest [17, 18]. This risk is attenuated by preoxygenation, but the most severe cases with high intrapulmonary shunt are often refractory to preoxygenation and drastically limit, or eliminate, the possibility of a safe apnea time [19,20,21]. In these cases, pulmonary blood flow is not resaturated by the high oxygen content of the functional residual capacity and patients rapidly desaturate [19]. A single dose of DDFPe during the preoxygenation period could potentially improve oxygen saturation and reduce the risk of critical desaturation during intubation. After the 2-h dose of DDFPe, when the mice were hypoxemic, the mean difference in oxygen saturation was 10% higher in DDFPe-treated mice compared to saline-controls. Future experiments under apnea while hypoxemic are warranted to further evaluate the potential efficacy for this indication.
Research is needed using various dosing strategies to evaluate the potential role of DDFPe in acute hypoxemic respiratory failure patients. Studies are also needed on the mechanism of action and safety in humans. Perfluorocarbons have the potential to create microemboli in the pulmonary circulation [1], which could consequentially worsen dead space in a patient with ARDS, and tert-butylcyclohexane was shown to create thrombocytopenia in an animal model of LPS induced inflammation [22]. However, repeated doses of DDFPe were well-tolerated in human trials for stroke [16]. Finally, a more complex analysis model to allow an evaluation of non-linear effects of the data may be further revealing and future experiments should include this approach. However, there are not enough degrees of freedom in our data to allow such a model, and the distribution of our residuals are normally distributed and do not show obvious heteroscedasticity that would indicate such a model is necessary.
These results indicate that DDFPe is an appealing candidate for improving arterial oxygenation in the presence of ventilation:perfusion mismatch and intrapulmonary shunt.
Availability of data and materials
Data are available with appropriate ethics review and data use agreement.
Abbreviations
- DDFPe:
-
Dodecafluoropentane emulsion
- VILI:
-
Ventilator-induced lung injury
- BAL:
-
Bronchoalveolar lavage
- ARDS:
-
Acute Respiratory Distress Syndrome
References
Jagers J, Wrobeln A, Ferenz KB (2021) Perfluorocarbon-based oxygen carriers: from physics to physiology. Pflugers Arch 473(2):139–150
Galvin IM, Steel A, Pinto R, Ferguson ND, Davies MW. Partial liquid ventilation for preventing death and morbidity in adults with acute lung injury and acute respiratory distress syndrome. Cochrane Database Syst Rev 2013(7):CD003707.
Correas JM, Meuter AR, Singlas E, Kessler DR, Worah D, Quay SC (2001) Human pharmacokinetics of a perfluorocarbon ultrasound contrast agent evaluated with gas chromatography. Ultrasound Med Biol 27(4):565–570
Lundgren CE, Bergoe GW, Tyssebotn I (2004) The theory and application of intravascular microbubbles as an ultra-effective means of transporting oxygen and other gases. Undersea Hyperb Med 31(1):105–106
Graham K, Moon-Massat PF, Unger EC (2019) Dodecafluoropentane emulsion (DDFPE) as a resuscitation fluid for treatment of hemorrhagic shock and traumatic brain injury: a review. Shock 52(1S):50–54
Letsiou E, Rizzo AN, Sammani S, Naureckas P, Jacobson JR, Garcia JG et al (2015) Differential and opposing effects of imatinib on LPS- and ventilator-induced lung injury. Am J Physiol Lung Cell Mol Physiol 308(3):L259–L269
Quijada H, Bermudez T, Kempf CL, Valera DG, Garcia AN, Camp SM et al (2021) Endothelial eNAMPT amplifies pre-clinical acute lung injury: efficacy of an eNAMPT-neutralising monoclonal antibody. Eur Respir J 57(5):2002536
Hou S, Ding H, Lv Q, Yin X, Song J, Landen NX et al (2014) Therapeutic effect of intravenous infusion of perfluorocarbon emulsion on LPS-induced acute lung injury in rats. PLoS ONE 9(1):e87826
Brown AT, Arthur MC, Nix JS, Montgomery JA, Skinner RD, Roberson PK et al (2014) Dodecafluoropentane emulsion (DDFPe) decreases stroke size and improves neurological scores in a permanent occlusion rat stroke model. Open Neurol J 8:27–33
Culp WC, Brown AT, Lowery JD, Arthur MC, Roberson PK, Skinner RD (2015) Dodecafluoropentane emulsion extends window for tPA therapy in a rabbit stroke model. Mol Neurobiol 52(2):979–984
Culp WC, Woods SD, Skinner RD, Brown AT, Lowery JD, Johnson JL et al (2012) Dodecafluoropentane emulsion decreases infarct volume in a rabbit ischemic stroke model. J Vasc Interv Radiol JVIR 23(1):116–121
Woods SD, Skinner RD, Ricca AM, Brown AT, Lowery JD, Borrelli MJ et al (2013) Progress in dodecafluoropentane emulsion as a neuroprotective agent in a rabbit stroke model. Mol Neurobiol 48(2):363–367
Strom J, Swyers T, Wilson D, Unger E, Chen QM, Larson DF (2014) Dodecafluoropentane emulsion elicits cardiac protection against myocardial infarction through an ATP-Sensitive K+ channel dependent mechanism. Cardiovasc Drugs Ther 28(6):541–547
Tyssebotn IM, Lundgren CE, Olszowka AJ, Bergoe GW (2010) Hypoxia due to shunts in pig lung treated with O2 and fluorocarbon-derived intravascular microbubbles. Artif Cells Blood Substit Immobil Biotechnol 38(2):79–89
Lundgren CE, Bergoe GW, Tyssebotn IM (2006) Intravascular fluorocarbon-stabilized microbubbles protect against fatal anemia in rats. Artif Cells Blood Substit Immobil Biotechnol 34(5):473–486
Culp WC, Onteddu SS, Brown A, Nalleballe K, Sharma R, Skinner RD et al (2019) Dodecafluoropentane emulsion in acute ischemic stroke: a phase Ib/II randomized and controlled dose-escalation trial. J Vasc Interv Radiol JVIR. 30(8):1244–1250
Mosier JM, Sakles JC, Law JA, Brown CA 3rd, Brindley PG (2020) Tracheal intubation in the critically ill. Where we came from and where we should go. Am J Respir Crit Care Med 201(7):775–788
De Jong A, Rolle A, Molinari N, Paugam-Burtz C, Constantin JM, Lefrant JY et al (2018) Cardiac arrest and mortality related to intubation procedure in critically ill adult patients: a multicenter cohort study. Crit Care Med 46(4):532–539
Mosier JM (2020) Physiologically difficult airway in critically ill patients: winning the race between haemoglobin desaturation and tracheal intubation. Br J Anaesth 125(1):e1–e4
Mosier JM, Hypes CD, Sakles JC (2017) Understanding preoxygenation and apneic oxygenation during intubation in the critically ill. Intensive Care Med 43(2):226–228
Mosier JM, Joshi R, Hypes C, Pacheco G, Valenzuela T, Sakles JC (2015) The physiologically difficult airway. West J Emerg Med 16(7):1109–1117
Pidcoke HF, Delacruz W, Herzig MC, Schaffer BS, Leazer ST, Fedyk CG et al (2022) Perfluorocarbons cause thrombocytopenia, changes in RBC morphology and death in a baboon model of systemic inflammation. PLoS ONE 17(12):e0279694
Acknowledgements
The authors would like to thank Julia Fisher, PhD for assistance with statistical analysis.
Funding
This work was funded by a University of Arizona Health Sciences Career Development Award. DDFPe was donated by NuVox Pharma.
Author information
Authors and Affiliations
Contributions
JMM conceived the study idea. JMM, JGNG, EU, SS, CK designed the experiment. JMM, SS, CK conducted the experiment and collected the data. JMM performed the statistical analysis with consultation from Julia Fisher, PhD. All authors interpreted the results. JMM and JGNG drafted the initial manuscript and all authors contributed significantly to the revisions. JMM takes responsibility for the project as a whole. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All animal care procedures and experiments were approved by the University of Arizona Animal Care and Use Committee (Approval #13-490).
Consent for publication
Not applicable.
Competing interests
None for JMM, SS, CK, or JGNG. Evan Unger is the CEO of NuVox Pharma.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mosier, J.M., Sammani, S., Kempf, C. et al. The impact of intravenous dodecafluoropentane on a murine model of acute lung injury. ICMx 11, 33 (2023). https://doi.org/10.1186/s40635-023-00518-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40635-023-00518-2