Abstract
Objectives
Expound upon priorities for basic/translational science identified in a recent paper by a group of experts assigned by the Society of Critical Care Medicine and the European Society of Intensive Care Medicine.
Data sources
Original paper, search of the literature.
Study selection
This study is selected by several members of the original task force with specific expertise in basic/translational science. Data extraction and data synthesis are not available.
Conclusions
In the first of a series of follow-up reports to the original paper, several members of the original task force with specific expertise provided a more in-depth analysis of the five identified priorities directly related to basic/translational science. This analysis expounds on what is known about the question and what was identified as priorities for ongoing research. It is hoped that this analysis will aid the development of future research initiatives.
Similar content being viewed by others
The Sepsis-3 Task Force, jointly sponsored by the Society of Critical Care Medicine (SCCM) and The European Society of Intensive Care Medicine (ESICM), recently redefined sepsis as “life-threatening organ dysfunction caused by a dysregulated host response to infection” [1]. One objective underlying this new definition was to refocus basic research into the pathobiology of this deadly syndrome. Specifically, the Task Force members sought to (1) emphasize that organ dysfunction is a key, defining characteristic of sepsis; (2) broaden the scope of investigation to include aspects of the host response beyond immunologic changes; and (3) direct studies toward identifying the links between the host response to infection and the development of organ dysfunction. The papers that resulted from the work of the Task Force have generated both enthusiasm and controversy. Most of the response, however, has focused not on the redefinition but rather on the evidence-based clinical criteria used by the Task Force to identify patients with sepsis from patients with uncomplicated infection. The definition is inherently difficult to examine in the clinical arena because clinical identifiers of “organ dysfunction” and “dysregulated host response” are limited. Therefore, the Task Force explicitly stressed that future research into the basic science of sepsis focus on clinically applicable identifiers of “organ dysfunction” and “dysregulated host response.”
A second major collaboration between the SCCM and the ESICM is the Surviving Sepsis Campaign (SSC). In formalizing their joint responsibilities for the SSC, the leaders of both societies established a Research Committee. The first task of the committee was to identify future research priorities. The deliberations of the committee led to the joint publication of “Surviving Sepsis Campaign Research Priorities for Sepsis and Septic Shock” in the journals Critical Care Medicine and Intensive Care Medicine in August 2018 [2, 3]. The initial document presented a broad overview of research priorities in several critical care domains with an expressed intention to, in the future, publish separate papers with more detailed descriptions for each domain. This paper, focusing on basic/translational science, contains the effort to fulfill that promise.
Methods
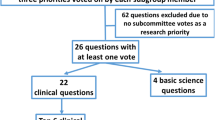
The content of the initial paper published by the SSC Research Committee [2, 3] was developed by asking each committee member to identify the research questions that most urgently required answers. Using a modified Delphi approach, the Task Force members reduced the original 88 suggestions to a series of questions focused on clinical care and four directed toward “basic science.” The final queries were presented in the original publication. Three Task Force members with specific expertise were tasked with generating expanded reviews of the four basic science questions as well as one additional query focusing on epigenetics. Each question was addressed by one of the three task force members. These in-depth reviews were then edited by the group as a whole, with added input from the committee co-chairs. The final result is presented here.
Overview of the presentation
The five basic science questions identified by the Task Force as a whole are as follows:
-
1.
What mechanisms underlie sepsis-induced cellular and subcellular dysfunction?
-
2.
How does sepsis alter bioenergetics and/or metabolism (both enhancement and failure)?
-
3.
How does sepsis (and/or approaches used to manage sepsis) alter phenotypes and interactions in the host microbiome and do alterations in the microbiome affect outcomes?
-
4.
How do epigenetics influence the pathobiology of sepsis?
-
5.
What mechanisms initiate, sustain, and terminate recovery after sepsis?
The format for each of the five questions directly mirrors that used in the previously published overview, which contains a more extensive description of the methods [2, 3].
Question 1: What mechanisms underlie sepsis-induced cellular and subcellular dysfunction?
What is known
The redefinition of sepsis by the Sepsis-3 Task Force focuses on the importance of organ dysfunction as the sine qua non of the disorder [1]. As a result, there is a compelling need to develop new clinical constructs for dysfunction in individual organ systems, as well as to continue to advance animal models to more accurately reflect human sepsis [4]. The process is hampered by (1) lack of a true gold standard to identify sepsis and (2) a need to develop indices of organ dysfunction that can be measured in patients, where access to cells is limited. There is little to be done about the first point. To address the second, it will first be necessary to identify the cellular abnormalities that underlie dysfunction in specific organ systems. These abnormalities can then be related to updated proxy measures that correlate, as closely and specifically as possible, with the actual cellular changes that lead to sepsis-induced organ dysfunction. However, access to clinical samples is limited, most often to what can be obtained from sampling blood, urine, or less frequently with biopsy or lavage specimens. Thus, WBCs are likely to be all that is routinely available. As a result, there is an imperative to use either models or in silico constructs to identify cellular abnormalities consistent with sepsis-induced dysfunction in different organs. Correlation of these abnormalities with measurements that can be made using blood or urine, or with noninvasive functional testing (e.g., echocardiography) will provide a clinically useful approach to organ dysfunction.
-
A)
Pathobiological changes that constitute “dysfunction” have been identified in several organ systems. These abnormalities reflect a small number of identifiable patterns.
-
1.
Some pathobiological abnormalities are consistent with changes in clinical variables that are commonly measured. These changes can therefore be used to indicate the presence of organ dysfunction and to follow its clinical course. For example, pathologic abnormalities in the lung (edema in intra-alveolar septa and air spaces, debris—the “hyaline membrane”—lining alveoli, loss of type 1 pulmonary epithelial cells via necrosis and apoptosis, loss of synthetic capacity by type-2 cells) [5,6,7] are consistent with the clinical presentation of lung injury (development of hypoxemia, reduced compliance, atelectasis, and multifocal lung consolidation) that are often used to assess respiratory function in patients.
-
2.
In other cases, changes consistent with organ dysfunction have been identified under experimental conditions and in animal models. However, these variables are not routinely measured clinically, nor have surrogates that correlate with these abnormalities been clinically validated. For example, sepsis-induced abnormalities in hepatic detoxification (e.g., transcellular bile acid transport) and biosynthesis (e.g., hepatocellular gene expression) have been described at the basic level [8,9,10]. However, these variables are not currently measured in the clinical realm, where hepatic dysfunction from any cause is assessed using serum levels of transaminases and elevations of bilirubin that are relatively nonspecific and not diagnostic of sepsis-induced hepatocellular dysfunction. Thus, a better understanding of pathobiology is required to identify measurements with clinical utility.
-
3.
Although some aspects of sepsis pathobiology have been well-described, their significance can be interpreted in two completely contradictory ways. As an example, consider sepsis-induced abnormalities in WBCs, which include elevated cytokine elaboration, reduced bacterial killing/clearance, and depressed responses to stimulation with inflammatory agonists [11]. However, elevated cytokine expression can reflect the response to two different, diametrically opposite stimuli. High levels of tumor necrosis factor (TNF)-α or interleukin (IL)-6 can induce inflammation and may directly damage cells. Thus, the increased elaboration might in itself be pathologic; appropriate therapy would therefore be blockade of their activity. However, in animal models of sepsis, there is impairment of intracellular pathways that are activated by these cytokines—that is, cells do not have the expected response to cytokines. The adaptive response to this situation would be to overcome the defect with increased cytokine elaboration and release, much as primary adrenal insufficiency results in enhanced release of thyroid-stimulating hormone from the pituitary [12]. If elevated levels of TNF-α and IL-6 represent a compensatory mechanism to counteract these defects, therapy would involve increasing TNF/IL-6 abundance or activity even further. It is conceivable that both possibilities can occur concurrently. That is, the response of some cells to cytokines may be inadequate (e.g., hepatocytes, as identified in animal models), which drives up levels of IL-6 and TNF-α. These high levels, however, may be toxic to other cells (e.g., pulmonary or gastrointestinal tract [GI] epithelial cells). In effect, the elaboration and secretion of cytokines may be driver of pathology, a beneficial response to pathology, both, or an incidental change. Thus, while it is clear that sepsis elevates TNF-α/IL-6 levels, a better understanding of the impetus underlying these changes is required to intervene effectively.
-
4.
In some cases, it may be impossible to separate sepsis pathobiology from the effects of treatment. The best example lies in attempts to differentiate acute respiratory distress syndrome (ARDS) from ventilator- or fluid-induced lung injury. A better understanding of differences in the cellular pathobiology of these disorders is therefore required.
-
5.
Certain aspects of sepsis pathobiology have proven remarkably difficult to understand. Evidence may suggest the presence of global organ dysfunction and of abnormalities in processes specific to certain cell types, but it is difficult to sort out the complex combination of dysfunction in individual types of cells and the interaction between these cells. Consider sepsis-induced acute kidney injury. Identified specific abnormalities include (1) reduced glomerular filtration rate (GFR) despite, (2) adequate or high renal blood flow (RBF) [13], (3) poorly understood defects in tubular function [14], and (4) aberrant or attenuated responses to exogenous modulation, for example, by hormones. Although a comprehensive explanation that encompasses all of these defects has been proposed [14] and appears to be present in a rodent model [15], it has not been validated in large animals or in clinical sepsis. Decreased GFR despite adequate or supra-normal RBF can reflect dilation of the efferent (postglomerular) arteriole, but how this change might relate to altered resorption and transport in the tubules is unknown. Correlations between changes in biomarkers for GFR (serum levels of creatinine, neutrophil gelatinase-associated lipocalin [NGAL], or cystatin-C) and those reflecting tubular dysfunction (kidney injury marker [KIM]-1, insulin-like growth factor binding protein [IGFBP]-7) are lacking. How KIM-1 and NGAL IGFBP-7 are related to actual defects in tubular function is unclear. Further, it is difficult to differentiate the risk of renal compromise (often termed “stress”) from actual dysfunction or injury. That is, an early period of inflammatory activation and perhaps proximal tubular dysfunction/injury precedes abnormalities (uremia, acidosis, abnormal electrolyte levels such as hyperkalemia) that have historically been used to indicate a need for renal replacement therapy. As is the case with other organs (e.g., heart, liver), the correlation between dysfunction and histologic evidence of damage is obscure. Thus, a far more complete understanding of the pathobiologic changes that cause dysfunction in different types of cells and/or processes in individual organ systems and of how sepsis disrupts interactions between different types of cells is of key importance.
-
B)
Sepsis pathobiology may reflect dysfunction is closely related cell types that are present in a number of distinct organ systems. For example, experimental and clinical evidence indicates the presence of sepsis-induced defects in protein synthesis in hepatocytes, type 2 pulmonary epithelial cells, and “central,” that is, pituitary, endocrine cells [5,6,7,8,9,10, 16,17,18,19,20]. Conversely, each cell or type of cell may develop a specific defect or manifest dysfunction in a unique manner. For example, sepsis upregulates production and release of cytokines by monocytes and lymphocytes [11] but decreases production and release of surfactant or surfactant proteins by type II pulmonary epithelial cells [5,6,7] or of hormones by endocrine or pituitary cells [18,19,20].
-
C)
As mentioned above, sepsis is associated with defects in cytokine signal transduction pathways. Data suggest that this type of abnormality may alter the response to other mediators. Impairment of endocrine signal transduction in sepsis has been well-described [19]. Sepsis also downregulates β-adrenergic and other G-protein receptor-mediated pathways [21, 22], which contributes to sepsis-induced cardiac dysfunction [23]. More recent data indicate defective signal transduction in pathways responding to steroid hormones, for example, glucocorticoids [24].
-
D)
There is an important extension of the described defects in cytokine- and hormone-mediated cellular responses. Cytokines, which are primarily produced by immune and endothelial cells, and hormones, which circulate, represent pathways by which cells in one tissue or organ system can be “informed” of changes that occur elsewhere. For example, a decrease in blood pressure or oxygen content in the blood supplying the brain is sensed by specialized cells of the carotid artery and trigger the release of epinephrine, vasopressin, and angiotensin, which in turn increase cardiovascular function, thereby restoring substrate delivery to the brain. Similarly, immune and endothelial cells respond to the presence of either damage-associated molecular patterns (DAMPs) or pathogen-associated molecular patterns (PAMPs) by elaborating and releasing cytokines, which can then alter activity in adjacent cells. Activation of circulating immune cells makes it possible for the transmission of DAMP/PAMP—induced responses to remote cells, tissues, and organ systems. In effect, endocrine and immune changes function, in part, as part of an organism-wide communications system. Sepsis impairs these forms of communication by attenuating the ability of cells to respond to cytokine and endocrine mediators.
-
B)
A third major long-range communication system within organisms is the nervous system. Multiple lines of evidence indicate that sepsis induces impairment in both the peripheral nervous system and CNS [25,26,27,28]. The peripheral neuropathy of sepsis/critical illness has been well-described. Several more recent findings have demonstrated that sepsis impairs signaling originating in the brain that limits responses in other organ systems. The orexinergic system of the hypothalamus was recently reported to modulate, at least in part, depressed activity/arousal, bradycardia, hypothermia, and hypopnea in experimental sepsis (analogous to the tachycardia, hyperthermia, and tachypnea that initially characterize the human response). This defect in orexinergic signaling also alters pituitary hormone release. All these changes were reversed when orexin was administered into the cerebrospinal fluid [27]. Finally, sepsis interferes with the “inflammatory reflex,” a negative feedback loop in the vagus nerve where ascending signals “inform” the brain of inflammatory events in the periphery while descending signals limit the cytokine response to those same responses [28,29,30,31]. A number of studies have demonstrated brain inflammation in experimental sepsis, most often implicating microglia [29, 30].
-
E)
A substantial body of evidence suggests that sepsis causes a global defect in a basic cellular or subcellular function in many cell types. The ubiquitous presence of such an abnormality would produce dysfunction in many different cell types, irrespective of their specific function or location. For example, there are numerous reports of sepsis-induced mitochondrial dysfunction in multiple cell types [19, 20, 27]. Abnormalities have been reported in mitochondrial oxidative phosphorylation, with impairment described in all four complexes of the electron transport chain (ETC) [32,33,34,35,36]. The resulting energy deficit could disable cell-specific functions in any cell that is mitochondria-dependent.
-
F)
Finally, dysfunction in a single type of cell that is present in virtually all organs could underlie cell- and organ-specific dysfunction. For example, endothelial cells, which are present in all tissues, actively produce inflammatory mediators and coagulation intermediaries during sepsis and contribute to sepsis-induced vascular dysfunction and leak [18, 37]. Thus, differential or sequential development of endothelial dysfunction in different vascular beds might mediate aspects of sepsis-induced organ dysfunction.
What is not known—gaps in our understanding—directions for future research
-
1.
Does a global defect that is shared by multiple cell types underlie all forms of sepsis-induced cellular dysfunction?
-
2.
Are there unique mechanisms of dysfunction that are specific to different types of cells, including different types of cells within a single organ?
-
3.
Do cells of similar embryologic origin (e.g., epithelium) become dysfunctional in ways that differ from other types of cells?
-
4.
Do cells with similar functions (e.g., elaboration/release of proteins, lipids) develop unique forms of dysfunction that differ from that of cells with different basic functions (e.g., all cells that contract)?
-
5.
Endothelial cells are present in virtually all organ systems and may directly modulate organ function. Does endothelial cell dysfunction underlie dysfunction in other organ systems?
Question 2: how does sepsis alter bioenergetics and/or metabolism (both enhancement and failure)?
What is known
Many of the effects of sepsis on bioenergetics and/or metabolism have been well-described [38, 39]. In general, sepsis is associated with an increase in metabolic rate, as reflected in oxygen consumption and overall substrate utilization [40]. There is, however, a reduction in adenosine triphosphate (ATP) utilization in many tissues [41,42,43,44]. This limitation occurs in concert with maintenance of ATP abundance, suggesting that the decreased use reflects an attempt to conserve ATP availability to avoid cell death [45]. In this setting, “aerobic glycolysis” is stimulated and assumes a greater role in ATP production. That is, despite what would appear to be more than adequate oxygen availability, substrate is shunted into the glycolytic pathway, resulting in the generation of lactate. Sepsis differs from other states where aerobic glycolysis is present (e.g., aerobic exercise) because of the ability of the liver to use lactate for gluconeogenesis (the Cori cycle) or bicarbonate is impaired [46]. This limitation contributes to hyperlactatemia and a metabolic acidosis. Thus, the aerobic glycolysis of sepsis constitutes a clinical example of the Warburg effect [47,48,49].
Two explanations for the sepsis-induced changes in glycolysis have been advanced. The first posits that increased glycolysis in sepsis reflects a defect in the microvasculature that impairs the delivery of oxygen to metabolically active tissues. Interestingly, the changes may be attenuated by hemodynamic targeted interventions [50]. The alternative implicates a defect in mitochondrial function that leads to a decrease in oxygen utilization. The latter is supported by abundant evidence of defective oxidative phosphorylation in sepsis. Importantly, these two putative mechanisms are not mutually exclusive; indeed, evidence suggests that both are operative in sepsis. Which specific complexes in the ETC are impaired is incompletely understood, and appears to depend on the tissue, or, in animals, the model. Decreased activity has been identified in each of the five complexes in ETC [33, 34]. Importantly, complex II serves as an enzyme in both oxidative phosphorylation and in the Krebs cycle. Therefore, impairment would enhance the diversion of substrate into glycolysis, a change that has been hypothesized to underlie the Warburg effect [51]. One of the consequences of impaired mitochondrial function, whether as a result of a defect in either the microcirculation or the mitochondria themselves, has been termed “hibernation” or “oxygen conformance” [52,53,54]. In this state, nonvital functions are shut down in order to maintain cell viability despite inadequate oxygen delivery or utilization.
Sepsis is also known to alter substrate preference, with a relative decrease in the utilization of glucose (glucose intolerance) relative to fat and protein [55,56,57]. As a result, septic patients tend to be hyperglycemic. In later stages, oxidation of fatty acids may also be impaired, as reflected in elevated serum levels of lipoproteins, free fatty acids, and triglycerides [47,48,49]. There is accelerated catabolism of skeletal muscle and possibly smooth muscle as well [58]. In addition, the effects of micronutrient (e.g., vitamins, trace metals) are also impaired, reflecting either deficiency or altered activity [59].
Changes in metabolism may also reflect the influence of “communications” pathways (described under question 1)—humoral (i.e., cytokine/white cell-mediated), endocrine, neuronal—on cellular function. Cytokine-mediated changes are well-described; the initial description of the metabolic effects of TNF was based on observations in diseased cattle—cachexia despite grossly lipemic serum. Studies in clinical sepsis and/or animal models have identified impaired activity of hormones that are known to affect metabolism (e.g., insulin, glucagon, T3/4, growth hormone, epinephrine/norepinephrine cortisol) and of less well-studied endocrine agents (adiponectin, leptin, ghrelin). Indeed, relative endocrine resistance is a characteristic finding [60]. Some studies suggest that sepsis alters the CNS effects of leptin and ghrelin, which are integral in central modulation of metabolism [61, 62]. Recent studies implicate alterations in the activity of the orexinergic and basal forebrain muscarinic systems in the brain in sepsis-induced metabolic changes [27, 28].
Several recent cohort studies and meta-analyses have suggested a protective role for obesity in critically ill patients [63,64,65]. However, the data are far from conclusive and mechanistic explanations are lacking. Indeed, basic studies in mice suggest that diet-induced obesity increases sepsis-induced inflammation as well as injury to the heart and liver [66,67,68,69].
What is not known—gaps in our understanding—directions for future research
-
1.
What causes the increased metabolic rate noted in sepsis?
-
2.
What mechanisms mediate alterations in oxidative phosphorylation? In particular, what underlies the altered activity in specific ETC complexes?
-
3.
What mechanisms alter sepsis-induced changes in pathway (e.g., glycolysis, beta-oxidation, nitrogen cycle), substrate (e.g., carbohydrate, fat, protein, micronutrient), and/or cell (e.g., cardiomyocyte, hepatocyte) specific metabolism?
-
4.
What mechanisms underlie sepsis-induced defects in endocrine activity?
-
5.
How does sepsis affect brain circuits that control metabolism?
-
6.
How do cytokines alter metabolic pathways?
-
7.
Do metabolic pathways influence inflammation, and if so, how?
-
8.
Are changes in energetics observed in all cells or are they cell-type-specific?
-
9.
Are defects affecting energetics present only in mitochondria or are there also changes in other subcellular structures?
-
10.
Is obesity protective against sepsis? Why are results in human sepsis and animal models discrepant?
Question 3: how do the microbiota and the microbiome contribute to the pathobiology of sepsis?
What is known
In a number of disease states, pathology is determined by an alteration in the interactions between the host and its complex microbial ecosystem. These changes, which likely affect outcomes of critically ill and septic patients, are the subjects of intense clinical and basic science investigations. The development of culture-independent methods to detect microbial genes has revolutionized this research and greatly enhanced microbe identification [70,71,72]. We now appreciate the enormous diversity of microbial species (microbiota) and microbial genomes (microbiome) that exist within human ecosystems (e.g., GI tract [gut], lungs, skin, etc.), as well as the importance of the microbiome to human health and disease [70]. It has become clear that the gut microbiome plays an important role in patients with sepsis, suggesting that the microbiome and host-microbiome interactions may be therapeutic targets [73].
The average healthy 70 kg adult human male is estimated to contain approximately 30 trillion host cells and to be colonized by nearly 40 trillion microbes [72, 74]. The gut microbiome is the largest in the human body and, perhaps because it can be assessed using fecal samples, has been the most extensively studied microbiome. The gut contains over 1000 species of bacteria, fungi, protozoa, and viruses containing nearly 9.9 million microbial genes [75]. These microbes live in complex and interactive communities and exhibit extensive geographic heterogeneity [75].
Recent studies indicate that the gut microbiome contributes to the regulation and maturation of biological function both within and outside of the GI tract [76]. The gut microbiome contributes to (1) pathogen containment, (2) immune maturation and functionality within and outside of the GI tract, (3) neurologic signaling, (4) host cell proliferation, (5) toxin elimination and drug modification, and (6) biosynthesis of compounds, including vitamins and neurotransmitters [77,78,79,80,81,82,83,84]. Dysbiosis, the development of imbalances in the composition and/or function of the host microbiome, has been implicated in a wide variety of human and animal disorders, including cardiovascular disease, autism spectrum disorders, metabolic disorders, and asthma [85,86,87,88,89,90,91]. Importantly, host-microbiota interactions are bi-directional; the two impact each other enormously.
A number of studies have suggested that the host microbiome is altered both by sepsis itself and by management approaches used to treat septic patients. Some have gone so far as to postulate that these changes contribute to the multiple organ dysfunction syndrome (MODS) [76, 92,93,94]. Alverdy and Krezalek [95] defined mechanisms by which they believe the microbiome becomes a “pathobiome” [95,96,97,98,99] that leads to “nonresolving MODS” [95, 96, 100].
-
A)
Multiple endogenous host and external factors contribute to the conversion of a healthy microbiome into a pathobiome in patients with sepsis.
Clinical studies have documented changes in the number of microbial species and genes, pathogenicity of different microbes, and microbial production of metabolites in the gut microbiome of adult patients following hepatectomy, trauma, cardiac arrest, and cerebrovascular events [101,102,103,104]. Clinical studies in the ICU arena have primarily focused on the microbiome of the general ICU population and not specifically on the subset of patients with sepsis. Sepsis-induced changes were suggested by a small clinical study of patients with severe systemic inflammatory response syndrome caused by sepsis (n = 18), trauma (n = 6), and burns (n = 1) [102] and likely contribute to findings in critically ill adults [100] and children [104]. Enrichment of the lung microbiome with gut bacteria has been reported in mice that have undergone cecal ligation and puncture (CLP) [105], a widely used model of abdominal sepsis that was first described in 1980 [106], and in critically ill patients with ARDS [105]. Finally, alterations in the gut microbiome have been reported in mice following experimental brain injury [107].
A number of factors alter the composition and pathogenicity of the human microbiome (Table 1) [73, 75, 78, 108,109,110,111,12,13,114]. Although the relative contribution of each of these factors to clinical changes in the microbiome during critical illness is difficult to discern, antibiotics and severity of illness seem to be major determinants [73].
Basic research directed at identifying the mechanisms underlying both gut dysbiosis and changes in the microbial virulence in species such as Candida, Staphylococcus, and Pseudomonas [79, 97, 99] has identified a number of contributors. Factors involved in the latter are both intrinsic (hormones, endorphins) and extrinsic factors (opiates, antibiotics, immunosuppressive agents). Recent studies have invoked quorum sensing, a complicated system that allows microbes to collectively respond to the environment [97, 116, 117]. Pseudomonas aeruginosa has been reported to adopt a more virulent phenotype in response to exogenous and endogenous opioids via quorum sensing mechanisms [97].
-
B)
Gut dysbiosis and the development of a pathobiome is associated with worse outcomes in septic patients.
Clinical studies suggest that sepsis is associated with the replacement of a diverse, health-promoting microbiome by a pathobiome that is harmful to the host [92, 94, 118, 119]. Animal studies support the contribution of this dysbiosis to septic pathobiology and MODS [120,121,122]. Dysbiosis is characterized by an altered microbiome that eliminates microbes such as Lactobacillus and Bifidobacterium that protect against overgrowth and limit epithelial adherence of pathogenic bacteria [123, 124]. The protective effects of the healthy microbiome may lie in the ability of Lactobacillus and obligate anaerobes to ferment nondigestible dietary fibers to short-chain fatty acids (SCFAs), including propionate, acetate, and butyrate, that can be used by the gut epithelium to promote barrier integrity and enhance immune function [124,125,126]. This loss can promote systemic infection and dysregulated inflammation.
-
C)
Manipulation of the gut microbiome affects outcomes from infection and alters immune responses in some conditions.
Therapeutic manipulation of the gut microbiome via selective decontamination, fecal transplantation, or use of probiotics has been attempted in several conditions attributed to gut dysbiosis. This approach is supported by studies in animals [127,128,129,130,131,132,133]. A number of studies have documented that selective gut decontamination in both humans and animals reduced organ inflammation and dysfunction [134, 135]. Fecal transplantation has shown efficacy for severe recurrent diarrhea caused by antibiotic-resistant Clostridium difficile and has mixed results in inflammatory bowel disease, but its utility in critically ill patients has yet to be defined [136,137,138,139].
-
D)
What environmental factors could be manipulated to promote a healthy microbiome?
Although it may be difficult to forgo treatment with essential therapies such as antibiotics, other factors, such as diet, stress ulcer prophylaxis, and the use of immunosuppressive agents, are potentially amenable to interventions. Although some cannot be changed (e.g., host genome), understanding their impact on the host’s microbiome may eventually lead to personalized approaches to manipulating the host’s environment to promote a healthy microbiome.
-
E)
How do the microbiomes from different parts of the body determine outcomes?
Thus far, studies on how the changes in the microbiome affect critically ill patients have focused on the gut. However, critical illness and sepsis also cause changes in other microbiomes, such as the lung [105]. The importance of non-GI microbiomes in determining outcomes of sepsis has yet to be defined.
What is not known—gaps in our understanding—directions for future research
-
1.
How do specific approaches to the management of sepsis affect the host microbiome?
-
2.
Which of the factors noted in Table 1 promote gut dysbiosis? What are their specific effects? Are other factors are involved?
-
3.
Do changes in the microbiome directly lead to the development or exacerbation of sepsis/MODS? What specific components of the pathobiome are of particular interest?
-
4.
Does the conversion from a normal microbiome to a pathobiome cause/exacerbate sepsis MODS or is the change merely associated with sepsis/MODS?
-
5.
Does manipulation of the microbiome alter the incidence, severity, or outcomes of sepsis?
-
6.
Can the pathobiome be stably converted back to a normal microbiome? Is such a conversion beneficial?
-
7.
Does the presence/absence of SCFA affect the pathogenesis of sepsis? Does it affect organ dysfunction or sepsis outcomes? Does administration of SCFAs or the introduction of SCFA-producing bacteria alter sepsis pathogenesis and/or improve organ dysfunction and outcomes?
-
8.
What environmental factors could be manipulated to promote a healthy microbiome? Does manipulating diet, exercise, or immunosuppressive agents affect the development of sepsis/MODS? Does it alter outcomes?
-
9.
Can a better understanding of how host genomics interact with specific elements in the microbiome/pathobiome provide insight that can alter outcomes? Can this understanding be leveraged to provide personalized approaches to the promotion of a healthy microbiome?
-
10.
Are prebiotics or probiotics therapeutically beneficial? Is fecal transplantation beneficial?
Question 4: how do epigenetics influence the pathobiology of sepsis?
What is known
“Epigenetics” is a catch-all phrase used to describe alterations in gene expression that occur independent of changes in DNA sequence. It is increasingly evident that these alterations are essential determinants of human health and diseases [140]. Epigenetic alterations are dynamic, and under optimal conditions, serve beneficial functions. However, these changes can also contribute to the development of major diseases and disorders, as well as affecting outcomes in more subtle ways. Importantly, epigenetic changes can be heritable. Epigenetic changes may alter the host response to infection and injury, and therefore the ability to prevent or clear infection.
Epigenetic mechanisms include DNA methylation, histone modifications (methylation, acetylation, phosphorylation, ubiquitination, and glycation), and elaboration of microRNAs (miRNAs). All can lead to rapid, transient, and reversible modification of gene expression by inducing gene activation or silencing. Studies in humans and animals suggest that epigenetic modifications impact sepsis [140, 141].
-
A)
Sepsis and endotoxemia are associated with epigenetic alterations in myeloid cells and in modulation of inflammation.
DNA methylation, histone modifications, and altered levels of miRNAs have been observed in cells in endotoxemia and sepsis. The changes in gene expression associated with these modifications modulate responses that may lead to endotoxin tolerance, immunosuppression, and immunoparalysis and susceptibility to infections [142,143,144,145,146,147,148,149,150,151,152]. DNA and histone methylation can silence genes encoding inflammatory mediators, anti-oxidants, and other factors that contribute to systemic inflammation [146, 152, 153]. In contrast, DNA methylation at certain genes has been linked to excessive systemic inflammation [147, 149].
-
B)
Lung injury induces epigenetic modifications that promote vascular permeability.
Experimental lung injury induced modification of histone H3 and thus downregulation of angiopoietin 1, Tie2, and Vegfr2. These changes, in turn, have been implicated in the expression of genes encoding inflammatory mediators and in the development of excessive microvascular permeability [154].
-
C)
Histones and miRNAs circulate in sepsis and may contribute to organ dysfunction.
Animal and human studies have shown that histones circulate in sepsis and are associated with increased mortality rates [155, 156]. miRNAs have also been found to circulate in human sepsis [157,158,159,160]. In CLP mice, miRNAs that circulate in extracellular vesicles have been implicated in the development of inflammation [161].
-
D)
Epigenetic alterations are being explored as potential sepsis biomarkers and therapeutic targets.
Epigenetic alterations, including DNA methylation, histone modifications, and miRNAs, have been touted as diagnostic biomarkers, markers of disease severity, and therapeutic targets [155, 162,163,164]. Studies on utility, which has been demonstrated in cancers [165], are being explored in sepsis [163, 166,167,168,169,170,171,172].
What is not known—gaps in our understanding—directions for future research
-
1.
Are epigenetic changes such as DNA methylation, histone modifications, and miRNA expression important contributors to the development of sepsis?
-
2.
Do epigenetic changes contribute to sepsis-induced MODS or changes in immune function? Or are they merely epiphenomena?
-
3.
Can epigenetic changes be used as diagnostic and/or prognostic biomarkers?
-
4.
Are epigenetic alterations potential therapeutic targets in sepsis?
-
5.
Might existing drugs (e.g., HDAC modulators) be used or new drugs be designed to target epigenetic alterations in sepsis?
-
6.
How do epigenetic factors influence the microbiome, and vice versa, and what are the implications for sepsis?
Question 5: what mechanisms initiate, sustain, and terminate recovery after sepsis?
The phrase “recovery from sepsis” can have a broad meaning. On an organism, wide level recovery can mean survival, reversal of organ dysfunction, or resumption of premorbid activities. Control/elimination of the focus of infection is required but it is by no means sufficient. Indeed, organ dysfunction can persist for a prolonged period afterward; some sepsis-induced abnormalities may never fully resolve. Overall, recovery likely reflects reversal of a vast array of maladaptive cellular, subcellular, and biochemical changes that develop during sepsis. These alterations involve metabolism, dysfunction in organelles, in particular mitochondria, attenuation of intracellular signal transduction pathways, and decrement in the activity of WBCs, neuronal pathways, and endocrine responses that are responsible for the transfer information from one part of the organism to another.
Despite reports that describe the events occurring during recovery or lack of recovery, the specific mechanisms that initiate recovery are unknown. It is possible that recovery represents an extension of Darwinian theory: sepsis resolves and the fittest cells/patients survive by implementing general mechanisms of protection. Alternatively, it may be that specific molecules/processes/events directly promote recovery from sepsis. Or perhaps recovery represents a combination of both.
-
A)
What immunological processes contribute to recovery from sepsis?
In contrast to a substantial body of work describing the resolution of “normal” or “balanced” inflammation, much about the reversal of the unique inflammatory state present in sepsis is poorly understood. Perhaps the greatest hindrance lies in a limited ability to characterize that state. To some extent, sepsis resembles an exaggeration of normal inflammation, with expression of high levels of pro-inflammatory cytokines. Other aspects, such as white cell bacterial engulfment and bacterial killing, are impaired. However, the combination of immune excess and immure incompetence characteristic of sepsis is strikingly unusual. It is logical to assume that the resolution of sepsis will be similarly difficult to understand. Thus, the complexity of the issue is apparent and requires attention.
-
1.
Do anti-inflammatory cytokines contribute to recovery after sepsis? If so, how?
What is known
Resolution of sepsis-induced inflammation is an active process that likely involves the production of endogenous anti-inflammatory molecules. A number of anti-inflammatory cytokines are upregulated during the course of sepsis (e.g., IL-1RA, IL-4, IL-10, and TGF-β) [173,174,175]. Importantly, IL-4 alters the balance between pro-inflammatory and anti-inflammatory T lymphocyte phenotypes and participates in the regulation of proliferation, differentiation, and apoptosis in multiple cell types. These IL-4-mediated changes are important for resolution of nonseptic inflammation but may actually contribute to the pathobiology of sepsis [176]. IL-10, in turn, blocks synthesis of interferon-γ, IL-1, TNF-α, IL-12, and GM-CSF and enhances the endocytosis-mediated elimination of human leukocyte antigen (HLA)-DR for the surface of white cells [177]. Again, these activities contribute to the resolution of inflammation under normal circumstances but how they influence sepsis is unclear. Indeed, clinical trials of a number of “anti-inflammatory” mediators have not demonstrated benefit in patients with sepsis [178].
What is not known—gaps in knowledge
• How do cytokines (IL-1RA, IL-4, IL-10, and TGF-β) with known anti-inflammatory effects contribute to the resolution of sepsis? What other white cell mediators contribute?
• Does the activity of IL-1RA, IL-4, IL-10, and/or TGF-β contribute to sepsis-associated immunosuppression? What other mediators are involved?
• Is the balance between pro- and anti-inflammatory activities that mediate recovery from “normal” inflammation lost in the resolution of sepsis?
-
2.
What processes in immune cells other than cytokine elaboration and release contribute to the resolution of sepsis?
What is known
As mentioned, sepsis is associated with a poorly understood defect in bacterial engulfment and killing by leukocytes [27]. In normal inflammation, the endocytosis-mediated elimination of HLA-DR for the surface of white cells by IL-10 plays an important role [177]. Changes in lymphocyte expression of the inhibitory receptor programmed death 1 (PD-1) and changes of T cell receptor diversity occur during healthy recovery from nonseptic conditions. However, it is unclear whether a similar process in sepsis leads to a healthy resolution of inflammation or if it represents an additional manifestation of sepsis pathobiology. PD-1 has been implicated in sepsis-associated immune suppression in both animals and humans [179, 180]. PD-1 overexpression by circulating T cells has been detected in septic patients and correlates with worse outcomes [179]; further, normalization of PD-1 expression at day 7 was noted in septic shock survivors [180].
A number of processes are known to contribute to limitations in normal/balanced inflammation. For example, lipoxin A4 regulates MCP-1 and nonphlogistic monocyte recruitment and stops LTB4-stimulated PMN influx [181]. Similarly, maresins, protectins, and resolvins limit further PMN influx to the site and stimulate efferocytosis and the clearance of cellular debris by resolving macrophages [181]. Autophagy-related proteins that act as critical regulators of caspase-1 activation (e.g., beclin-1 and LC3B) in vitro and in vivo contribute to normal/balanced inflammation by preventing accumulation of physiologically abnormal mitochondria [182]. miRNAs, such as programmed miR-466l expression, are temporally and differentially expressed during the resolution of balanced inflammation [183]. Impairment of any of these processes might contribute to failed resolution of sepsis.
What is not known—gaps in our understanding—directions for future research
• Sepsis is associated with impairment in a number of processes that contribute to resolution of normal/balanced inflammation. Does resolution of this defect contribute to recovery from sepsis? Or, conversely, does recovery from sepsis lead to resolution of these abnormalities?
• Does the PD-1 pathway exacerbate sepsis pathobiology or does it enhance recovery?
• Do lipid mediators, autophagy, or miRNA, which contribute to resolution of balanced inflammation, also contribute to recovery from sepsis?
• Resolution of inflammation in states other than sepsis involves specific intracellular pathways and/or events in immune cells. Which of these events/intracellular pathways also contribute to resolution of sepsis? What pathways/events not involved in other states are important for resolution of inflammation in sepsis?
• What events in immune cells that contribute to resolution of nonseptic inflammation promote sepsis-induced immunosuppression, thereby delaying the resolution of sepsis?
-
B)
What processes related to metabolism and/or bioenergetics contribute to recovery from cellular and subcellular dysfunction?
What is known
The catabolic state produced by sepsis causes alterations in protein breakdown and is characterized by a reduction in body weight, lean body mass, skeletal muscle mass, and fat mass. Metabolism, in general, is impaired, but compensatory mechanisms such as endocrine activity and enhanced substrate availability mask these abnormalities. For example, while global hepatic glucose production is higher than that observed under nonseptic conditions, this increase reflects high levels of catecholamines, corticosteroids, and glucagon. The response of the liver in the absence of sepsis to equivalent levels of hormonal stimulation far exceeds that observed during sepsis [184]. Hepatic inefficiency at least in part reflects impairment of intracellular signal transduction pathways for hormones and other mediators [12, 21, 24, 185, 186]. Although it is likely that the recovery mechanisms that restore the balance between catabolism and anabolism differ from those that initiated the imbalance, the actual process is poorly described. Importantly, lean body mass may be depleted in sepsis but cell death is not a significant feature in most organs and functional recovery does not appear to be limited by the regenerative capacity of the tissue, perhaps because solid organ mass does not appear to be affected [187]. It is essential to note that metabolic changes during sepsis recovery may be linked to other subcellular mechanisms, including autophagy, apoptosis, and proteasome activity [182, 188,189,190].
Some aspects of metabolic recovery have been examined in experimental models, most often using the CLP model in rodents. Crowell et al. [190] studied the regulation of skeletal muscle protein balance during recovery from CLP in mice. These investigators noted (1) persistence of CLP-induced proteolysis persisted during the recovery phase, (2) a period of enhanced muscle protein synthesis that was mediated by activation of Akt-TSC2-mTORC1 signal transduction, and (3) apparent delay of complete restoration of muscle mass that was in part explained by continued stimulation of the ubiquitin-proteasome pathway-mediated proteolysis.
Although the erosion of lean body mass and skeletal muscle loss have been studied [190, 191], examination of sepsis-induced changes in fat mass and adipocyte biology has been less thorough. The same group also showed that white adipose tissue stimulated continued inflammation with activation of the inflammasome, the ubiquitin-proteasome pathway, and autophagy, even when the infectious source was excised. These changes overlapped with alterations in skeletal muscle. However, release of uncoupling protein 1 during recovery, suggesting a “browning” of this white adipose tissue, was associated with diminution of inflammasome activation and autophagy as well as limited lipolysis and lipogenesis [192]. Again, these findings suggest that sepsis-induced changes in substrate metabolism persist into the recovery phase but that distinct recovery mechanisms exist.
Some of the mechanisms that modulate the balance between protein breakdown and synthesis also contribute to control of autophagy, a process that facilitates the turnover of organelles and intracellular protein. Both skeletal muscle turnover and autophagy are tightly controlled by mTORC1 and adenosine monophosphate-activated protein kinase (AMPK) [193]. Recovery of AMPK activity following CLP was associated with reduced severity and less profound lung injury [194] as well as improved bacterial clearance [195].
As described under question 2, bioenergetics are also significantly altered by sepsis. Mitochondrial dysfunction has been demonstrated in human sepsis and in animal models, including CLP [33, 196,197,198,199,200]. Fink termed this block in oxidative phosphorylation “cytopathic hypoxia” [201]. In 2008, Carré and Singer [202] suggested a link between recovery from sepsis and mitochondrial biogenesis. This contention is supported by animal studies demonstrating that recovery was associated with a progressive increase in cytochrome and mitochondrial DNA, followed by recovery of oxygen consumption and resting energy expenditure [203]. Additional investigations using CLP demonstrated improved organ function with reversal or bypass of dysfunction in specific elements of the ETC [204,205,206,207,208,209]. Recovery in patients was associated with early production of new mitochondria (biogenesis) [210]. Glycolysis contributes substantially to ATP generation in the presence of sepsis-induced mitochondrial dysfunction [39, 45, 48, 56, 57, 198, 211,212,213]. However, the glycolytic process is complex. Studies in animals have suggested that it is highly dependent on substrate delivery, Na-K transport [214], stimulation by catecholamines [215], and the Warburg effect [49, 216,217,218].
What is not known—gaps in our understanding—directions for future research
-
1.
Does reversal of sepsis-induced changes in metabolism/energetics promote recovery? Or is reversal of sepsis-induced changes simply an indicator that recovery is occurring/has occurred?
-
2.
What pathways both mediate sepsis-induced changes in metabolism and also effect recovery from sepsis? What pathways that modulate sepsis-induced changes in metabolism do NOT mediate recovery, and vice versa? Can any of these pathways be manipulated to initiate or enhance recovery from sepsis?
-
3.
Do unexplored or undiscovered pathways mediate both the development of sepsis-induced changes in metabolism and the recovery from these changes?
-
4.
Can the pathways that mediate recovery from sepsis-induced changes in both protein and fat metabolism be manipulated to initiate or enhance recovery from sepsis?
-
5.
Can the “browning” of fat be enhanced? Can manipulation of “browning” be used to enhance recovery from sepsis?
-
6.
Is the restoration of mitochondrial function necessary for recovery from sepsis?
-
7.
Do interventions that improve the function of individual aspects of mitochondrial function promote recovery from sepsis? Do interventions that have been found to be successful following CLP also enhance recovery from human sepsis?
-
8.
Recovery requires ATP utilization above basal levels. In addition to serving as a source of energy production during sepsis, does ATP production from lactate, that is, glycolysis, meaningfully contribute to recovery from sepsis? What mechanisms regulate sepsis-induced lactate production? Can these mechanisms be manipulated for therapeutic benefit?
-
C)
What endocrine and neuronal pathways contribute to recovery from sepsis?
What is known
Endocrine dysfunction is a key characteristic of sepsis; sepsis-induced abnormalities have been reported in the intracellular pathways mediating tissue responses to nearly every hormone [19, 20]. Dysfunction takes two forms. In the acute phase, tissues become hypo-responsive (“peripheral resistance”) and central mechanisms to increase hormone release are activated [19]. Ultimately, however, central secretion of hormones, for example, from the pituitary, decreases (“central suppression”). Restoration of both tissue responses and central elaboration/release have been described in recovery [19]. However, resolution of sepsis-induced defects in endocrine activity may simply be a result of recovery as opposed to a contributing factor.
Neuronal abnormalities are believed to contribute to sepsis pathobiology. For example, recent studies have demonstrated a role for dysfunction in the orexinergic pathway of the hypothalamus [27] and in the basal forebrain cholinergic system [28, 219]. Seminal work by Pavlov and Tracey [220] defined the “cholinergic anti-inflammatory pathway,” which downregulates inflammation in sepsis via activation of vagus nerve efferents, leading to sequential splenic release of norepinephrine and then acetylcholine which in turn downregulates activation of endothelial cells and promotes a pro-resolving phenotype in macrophages and monocytes. Importantly, the vagus-mediated anti-inflammatory pathway is impaired following CLP [220]. Stimulation of the vagus can reverse some elements of the CLP-induced inhibition of this reflex [221].
Cognitive defects that may be analogous to those present in patients with sepsis have been identified following CLP in rodents. These abnormalities have been attributed to a number of underlying causes, including neuroinflammation, a number of different brain regions, most notably the hippocampus and basal forebrain, and in some cases have been amenable to treatment [28, 168, 222,223,224,225,226,227,228,229,230,231]. However, the relevance of these abnormalities to human sepsis is unknown.
What is not known—gaps in our understanding—directions for future research
-
1.
Is reversal of sepsis-induced endocrine/neuronal defects a cause or an effect of recovery?
-
2.
What specific hormones and/or neuronal pathways contribute to recovery? Are there pathways that are not operative in the pathogenesis of sepsis that are involved in recovery?
-
3.
Do strategies that counteract or reverse endocrine or neuronal dysfunction contribute to recovery?
-
4.
What additional neuronal pathways contribute to the pathogenesis of sepsis?
-
5.
What neuronal abnormalities, pathways, and defects contribute to sepsis-induced short-term neurobehavioral abnormalities and long-term cognitive dysfunction?
Summary
This document expands upon topics in “Basic Science Research” that were specifically identified as priorities by the SSC Research Committee [2, 3]. The goal of the authors and the committee was to provide the critical care community with a detailed, well-balanced, and highly informative summary regarding topics specifically identified by the members of the SSC Research Committee as a whole. Our focus, and the focus of future publications, is on “what is known,” followed by enumeration of ongoing research priorities and questions that we believed are unanswered. Each of the basic research areas that we have focused on has high translational potential. We have called upon our collective insights as critical care practitioners and as investigators focusing on basic science research in sepsis. We have also included recommendations from other members of the SSC Research Committee that reflect long-term involvement in the critical care community as a whole.
We recognize that members of the critical care community have diverse backgrounds and interests and that many are more clinically focused. We therefore have attempted to provide a balanced and accessible review and perspective and to provide material that is useful to all involved in our specialty. Importantly, the process used to generate the topics discussed here is, by its nature, subjective. Members of the committee all have interests in/commitments to the study of specific topics. We have tried to limit the effects of personal interest/bias on the choice of topics. Similarly, some areas of interest to some readers, of necessity, will not be represented in this document. Undoubtably some seeming omissions will be addressed in future papers.
We are grateful to the leadership of the SSC, the ESICM, and the SCCM for providing the opportunity and for their continued commitment to critical care research.
References
Singer M, Deutschman CS, Seymour CW et al (2016) The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 315:801–810
Coopersmith CM, De Backer D, Deutschman CS et al (2018) Surviving sepsis campaign: Research priorities for sepsis and septic shock. Crit Care Med 46:1334–1356
Coopersmith CM, De Backer D, Deutschman CS et al (2018) Surviving sepsis campaign: research priorities for sepsis and septic shock. Intensive Care Med 44:1400–1426
Osuchowski MF, Ayala A, Bahrami S et al (2018) Minimum quality threshold in pre-clinical sepsis studies (MQTiPSS): an international expert consensus initiative for improvement of animal modeling in sepsis. Shock 50:377–380
Endo S, Sato N, Nakae H et al (2002) Surfactant protein A and D (SP-A, AP-D) levels in patients with septic ARDS. Res Commun Mol Pathol Pharmacol 111:245–251
Greene KE, Wright JR, Steinberg KP et al (1999) Serial changes in surfactant-associated proteins in lung and serum before and after onset of ARDS. Am J Respir Crit Care Med 160:1843–1850
Baker CS, Evans TW, Randle BJ et al (1999) Damage to surfactant-specific protein in acute respiratory distress syndrome. Lancet 353:1232–1237
Kim PK, Chen J, Andrejko KM et al (2000) Intraabdominal sepsis down-regulates transcription of sodium taurocholate cotransporter and multidrug resistance-associated protein in rats. Shock 14:176–181
Andrejko KM, Raj NR, Kim PK et al (2008) IL-6 modulates sepsis-induced decreases in transcription of hepatic organic anion and bile acid transporters. Shock 29:490–496
Wauters J, Mesotten D, Van Zwam K et al (2010) The impact of resuscitated fecal peritonitis on the expression of the hepatic bile salt transporters in a porcine model. Shock 34:508–516
Munoz C, Carlet J, Fitting C et al (1991) Dysregulation of in vitro cytokine production by monocytes during sepsis. J Clin Invest 88:1747–1754
Abcejo AS, Andrejko KM, Raj NR et al (2009) Failed interleukin-6 signal transduction in murine sepsis: Attenuation of hepatic glycoprotein 130 phosphorylation. Crit Care Med 37:1729–1734
Post EH, Kellum JA, Bellomo R et al (2017) Renal perfusion in sepsis: from macro- to microcirculation. Kidney Int 91:45–60
Gomez H, Ince C, De Backer D et al (2014) A unified theory of sepsis-induced acute kidney injury: inflammation, microcirculatory dysfunction, bioenergetics, and the tubular cell adaptation to injury. Shock 41:3–11
Arulkumaran N, Sixma ML, Jentho E et al (2017) Sequential analysis of a panel of biomarkers and pathologic findings in a resuscitated rat model of sepsis and recovery. Crit Care Med 45:e821–e830
Jenniskens M, Langouche L, Vanwijngaerden YM et al (2016) Cholestatic liver (dys)function during sepsis and other critical illnesses. Intensive Care Med 42:16–27
Sauer M, Haubner C, Richter G et al (2018) Impaired cell viability and functionality of hepatocytes after incubation with septic plasma-results of a second prospective biosensor study. Front Immunol 9:1448
De Backer D, Orbegozo Cortes D, Donadello K et al (2014) Pathophysiology of microcirculatory dysfunction and the pathogenesis of septic shock. Virulence 5:73–79
Ingels C, Gunst J, Van den Berghe G (2018) Endocrine and metabolic alterations in sepsis and implications for treatment. Crit Care Clin 34:81–96
Van den Berghe G (2002) Dynamic neuroendocrine responses to critical illness. Front Neuroendocrinol 23:370–391
Deutschman CS, De Maio A, Clemens MG (1995) Sepsis-induced attenuation of glucagon and 8-BrcAMP modulation of the phosphoenolpyruvate carboxykinase gene. Am J Physiol 269:R584–R591
Cariou A, Pinsky MR, Monchi M et al (2008) Is myocardial adrenergic responsiveness depressed in human septic shock? Intensive Care Med 34:917–922
Kakihana Y, Ito T, Nakahara M et al (2016) Sepsis-induced myocardial dysfunction: pathophysiology and management. J Intensive Care 4:22
Abraham MN, Jimenez DM, Fernandes TD et al (2018) Cecal ligation and puncture alters glucocorticoid receptor expression. Crit Care Med 46:e797–e804
Witt NJ, Zochodne DW, Bolton CF et al (1991) Peripheral nerve function in sepsis and multiple organ failure. Chest 99:176–184
Cankayali I, Dogan YH, Solak I et al (2007) Neuromuscular deterioration in the early stage of sepsis in rats. Crit Care 11:R1
Deutschman CS, Raj NR, McGuire EO et al (2013) Orexinergic activity modulates altered vital signs and pituitary hormone secretion in experimental sepsis. Crit Care Med 41:e368–e375
Zaghloul N, Addorisio ME, Silverman HA et al (2017) Forebrain cholinergic dysfunction and systemic and brain inflammation in murine sepsis survivors. Front Immunol 8:1673
Zrzavy T, Höftberger R, Berger T et al (2019) Pro-inflammatory activation of microglia in the brain of patients with sepsis. Neuropathol Appl Neurobiol 45:278–290
Santos-Junior NN, Catalão CHR, Costa LHA et al (2018) Experimental sepsis induces sustained inflammation and acetylcholinesterase activity impairment in the hypothalamus. J Neuroimmunol 324:143–148
Zanos TP, Silverman HA, Levy T et al (2018) Identification of cytokine-specific sensory neural signals by decoding murine vagus nerve activity. Proc Natl Acad Sci U S A 115:E4843–E4852
Gellerich FN, Trumbeckaite S, Hertel K et al (1999) Impaired energy metabolism in hearts of septic baboons: Diminished activities of complex I and complex II of the mitochondrial respiratory chain. Shock 11:336–341
Brealey D, Brand M, Hargreaves I et al (2002) Association between mitochondrial dysfunction and severity and outcome of septic shock. Lancet 360:219–223
Levy RJ, Deutschman CS (2007) Cytochrome c oxidase dysfunction in sepsis. Crit Care Med 35:S468–S475
Peruchi BB, Petronilho F, Rojas HA et al (2011) Skeletal muscle electron transport chain dysfunction after sepsis in rats. J Surg Res 167:e333–e338
Patil NK, Parajuli N, MacMillan-Crow LA et al (2014) Inactivation of renal mitochondrial respiratory complexes and manganese superoxide dismutase during sepsis: Mitochondria-targeted antioxidant mitigates injury. Am J Physiol Renal Physiol 306:F734–F743
Khakpour S, Wilhelmsen K, Hellman J (2015) Vascular endothelial cell toll-like receptor pathways in sepsis. Innate Immun 21:827–846
Lewis AJ, Billiar TR, Rosengart MR (2016) Biology and metabolism of sepsis: innate immunity, bioenergetics, and autophagy. Surg Infect (Larchmt) 17:286–293
Arulkumaran N, Deutschman CS, Pinsky MR et al (2016) ADQI XIV Workgroup: Mitochondrial function in sepsis. Shock 45:271–281
Kreymann G, Grosser S, Buggisch P et al (1993) Oxygen consumption and resting metabolic rate in sepsis, sepsis syndrome, and septic shock. Crit Care Med 21:1012–1019
Jacobs DO, Maris J, Fried R et al (1988) In vivo phosphorus 31 magnetic resonance spectroscopy of rat hind limb skeletal muscle during sepsis. Arch Surg 123:1425–1428
Chen HW, Hsu C, Lu TS et al (2003) Heat shock pretreatment prevents cardiac mitochondrial dysfunction during sepsis. Shock 20:274–279
Bougaki M, Searles RJ, Kida K et al (2010) Nos3 protects against systemic inflammation and myocardial dysfunction in murine polymicrobial sepsis. Shock 34:281–290
Eyenga P, Roussel D, Morel J et al (2018) Time course of liver mitochondrial function and intrinsic changes in oxidative phosphorylation in a rat model of sepsis. Intensive Care Med Exp 6:31
Brealey D, Karyampudi S, Jacques TS et al (2004) Mitochondrial dysfunction in a long-term rodent model of sepsis and organ failure. Am J Physiol Regul Integr Comp Physiol 286:R491–R497
Clemens MG, Chaudry IH, McDermott PH et al (1983) Regulation of glucose production from lactate in experimental sepsis. Am J Physiol 244:R794–R800
Schmoch T, Uhle F, Siegler BH et al (2017) The glyoxalase system and methylglyoxal-derived carbonyl stress in sepsis: Glycotoxic aspects of sepsis pathophysiology. Int J Mol Sci 18:657
Srivastava A, Mannam P (2015) Warburg revisited: lessons for innate immunity and sepsis. Front Physiol 6:70
Yang L, Xie M, Yang M et al (2014) PKM2 regulates the Warburg effect and promotes HMGB1 release in sepsis. Nat Commun 5:4436
Corrêa TD, Jeger V, Pereira AJ et al (2014) Angiotensin II in septic shock: effects on tissue perfusion, organ function, and mitochondrial respiration in a porcine model of fecal peritonitis. Crit Care Med 42:e550–e559
Potter M, Newport E, Morten KJ (2016) The Warburg effect: 80 years on. Biochem Soc Trans 44:1499–1505
Schumacker PT, Chandel N, Agusti AG (1993) Oxygen conformance of cellular respiration in hepatocytes. Am J Physiol 265:L395–L402
Boutilier RG (2001) Mechanisms of cell survival in hypoxia and hypothermia. J Exp Biol 204:3171–3181
Levy RJ (2007) Mitochondrial dysfunction, bioenergetic impairment, and metabolic down-regulation in sepsis. Shock 28:24–28
Cerra FB, Siegel JH, Border JR et al (1979) The hepatic failure of sepsis: Cellular versus substrate. Surgery 86:409–422
Stoner HB, Little RA, Frayn KN et al (1983) The effect of sepsis on the oxidation of carbohydrate and fat. Br J Surg 70:32–35
White RH, Frayn KN, Little RA et al (1987) Hormonal and metabolic responses to glucose infusion in sepsis studied by the hyperglycemic glucose clamp technique. JPEN J Parenter Enteral Nutr 11:345–353
Hobler SC, Tiao G, Fischer JE et al (1998) Sepsis-induced increase in muscle proteolysis is blocked by specific proteasome inhibitors. Am J Physiol 274:R30–R37
Berger MM, Shenkin A (2006) Update on clinical micronutrient supplementation studies in the critically ill. Curr Opin Clin Nutr Metab Care 9:711–716
Langouche L, Van den Berghe G (2006) The dynamic neuroendocrine response to critical illness. Endocrinol Metab Clin North Am 35:777–791 ix
Wei H, Cao X, Zeng Q et al (2015) Ghrelin inhibits proinflammatory responses and prevents cognitive impairment in septic rats. Crit Care Med 43:e143–e150
Tschöp J, Nogueiras R, Haas-Lockie S et al (2010) CNS leptin action modulates immune response and survival in sepsis. J Neurosci 30:6036–6047
Ng PY, Eikermann M (2017) The obesity conundrum in sepsis. BMC Anesthesiol 17:147
Wang S, Liu X, Chen Q et al (2017) The role of increased body mass index in outcomes of sepsis: A systematic review and meta-analysis. BMC Anesthesiol 17:118
Trivedi V, Bavishi C, Jean R (2015) Impact of obesity on sepsis mortality: a systematic review. J Crit Care 30:518–524
Ayalon I, Shen H, Williamson L et al (2018) Sepsis induces adipose tissue browning in nonobese mice but not in obese mice. Shock 50:557–564
Kaplan JM, Nowell M, Lahni P et al (2012) Short-term high fat feeding increases organ injury and mortality after polymicrobial sepsis. Obesity (Silver Spring) 20:1995–2002
Kaplan JM, Nowell M, Lahni P et al (2016) Obesity enhances sepsis-induced liver inflammation and injury in mice. Obesity (Silver Spring) 24:1480–1488
DeMartini T, Nowell M, James J et al (1863) High fat diet-induced obesity increases myocardial injury and alters cardiac STAT3 signaling in mice after polymicrobial sepsis. Biochim Biophys Acta Mol Basis Dis 2017:2654–2660
Lynch SV, Pedersen O (2016) The human intestinal microbiome in health and disease. N Engl J Med 375:2369–2379
Mar JS, LaMere BJ, Lin DL et al (2016) Disease severity and immune activity relate to distinct interkingdom gut microbiome states in ethnically distinct ulcerative colitis patients. MBio 7;e 1072–16
Sender R, Fuchs S, Milo R (2016) Are we really vastly outnumbered? Revisiting the ratio of bacterial to host cells in humans. Cell 164:337–340
Dickson RP (2016) The microbiome and critical illness. Lancet Respir Med 4:59–72
Sender R, Fuchs S, Milo R (2016) Revised estimates for the number of human and bacteria cells in the body. PLoS Biol 14:e1002533
Li J, Jia H, Cai X et al (2014) MetaHIT Consortium; MetaHIT Consortium: An integrated catalog of reference genes in the human gut microbiome. Nat Biotechnol 32:834–841
Lachar J, Bajaj JS (2016) Changes in the microbiome in cirrhosis and relationship to complications: hepatic encephalopathy, spontaneous bacterial peritonitis, and sepsis. Semin Liver Dis 36:327–330
Reinhardt C, Bergentall M, Greiner TU et al (2012) Tissue factor and PAR1 promote microbiota-induced intestinal vascular remodelling. Nature 483:627–631
Cho I, Yamanishi S, Cox L et al (2012) Antibiotics in early life alter the murine colonic microbiome and adiposity. Nature 488:621–626
Kamada N, Chen GY, Inohara N et al (2013) Control of pathogens and pathobionts by the gut microbiota. Nat Immunol 14:685–690
Fulde M, Hornef MW (2014) Maturation of the enteric mucosal innate immune system during the postnatal period. Immunol Rev 260:21–34
Canfora EE, Jocken JW, Blaak EE (2015) Short-chain fatty acids in control of body weight and insulin sensitivity. Nat Rev Endocrinol 11:577–591
Neuman H, Debelius JW, Knight R et al (2015) Microbial endocrinology: the interplay between the microbiota and the endocrine system. FEMS Microbiol Rev 39:509–521
Yano JM, Yu K, Donaldson GP et al (2015) Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell 161:264–276
Haiser HJ, Gootenberg DB, Chatman K et al (2013) Predicting and manipulating cardiac drug inactivation by the human gut bacterium Eggerthella lenta. Science 341:295–298
Turnbaugh PJ, Hamady M, Yatsunenko T et al (2009) A core gut microbiome in obese and lean twins. Nature 457:480–484
Wang Z, Klipfell E, Bennett BJ et al (2011) Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 472:57–63
Qin J, Li Y, Cai Z et al (2012) A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 490:55–60
Karlsson FH, Tremaroli V, Nookaew I et al (2013) Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature 498:99–103
Hsiao EY, McBride SW, Hsien S et al (2013) Microbiota modulate behavioral and physiological abnormalities associated with neurodevelopmental disorders. Cell 155:1451–1463
Koeth RA, Wang Z, Levison BS et al (2013) Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med 19:576–585
Arrieta MC, Stiemsma LT, Dimitriu PA et al (2015) CHILD study investigators: early infancy microbial and metabolic alterations affect risk of childhood asthma. Sci Transl Med 7:307ra152
Marshall JC, Christou NV, Horn R, et al: The microbiology of multiple organ failure. The proximal gastrointestinal tract as an occult reservoir of pathogens. Arch Surg 1988; 123:309–315
Johanson WG, Pierce AK, Sanford JP (1969) Changing pharyngeal bacterial flora of hospitalized patients. Emergence of gram-negative bacilli. N Engl J Med 281:1137–1140
Shimizu K, Ogura H, Hamasaki T et al (2011) Altered gut flora are associated with septic complications and death in critically ill patients with systemic inflammatory response syndrome. Dig Dis Sci 56:1171–1177
Alverdy JC, Krezalek MA (2017) Collapse of the microbiome, emergence of the pathobiome, and the immunopathology of sepsis. Crit Care Med 45:337–347
Krezalek MA, DeFazio J, Zaborina O et al (2016) The shift of an intestinal “Microbiome” to a “Pathobiome” governs the course and outcome of sepsis following surgical injury. Shock 45:475–482
Zaborina O, Lepine F, Xiao G et al (2007) Dynorphin activates quorum sensing quinolone signaling in Pseudomonas aeruginosa. PLoS Pathog 3:e35
Zaborin A, Gerdes S, Holbrook C et al (2012) Pseudomonas aeruginosa overrides the virulence inducing effect of opioids when it senses an abundance of phosphate. PLoS One 7:e34883
Romanowski K, Zaborin A, Valuckaite V et al (2012) Candida albicans isolates from the gut of critically ill patients respond to phosphate limitation by expressing filaments and a lethal phenotype. PLoS One 7:e30119
Zaborin A, Smith D, Garfield K et al (2014) Membership and behavior of ultra-low-diversity pathogen communities present in the gut of humans during prolonged critical illness. mBio 5:e01361–e01314
Kanazawa H, Nagino M, Kamiya S et al (2005) Synbiotics reduce postoperative infectious complications: a randomized controlled trial in biliary cancer patients undergoing hepatectomy. Langenbecks Arch Surg 390:104–113
Shimizu K, Ogura H, Goto M et al (2006) Altered gut flora and environment in patients with severe SIRS. J Trauma 60:126–133
Hayakawa M, Asahara T, Henzan N et al (2011) Dramatic changes of the gut flora immediately after severe and sudden insults. Dig Dis Sci 56:2361–2365
Rogers MB, Firek B, Shi M et al (2016) Disruption of the microbiota across multiple body sites in critically ill children. Microbiome 4:66
Dickson RP, Singer BH, Newstead MW et al (2016) Enrichment of the lung microbiome with gut bacteria in sepsis and the acute respiratory distress syndrome. Nat Microbiol 1:16113
Wichterman KA, Baue AE, Chaudry IH (1980) Sepsis and septic shock–a review of laboratory models and a proposal. J Surg Res 29:189–201
Houlden A, Goldrick M, Brough D et al (2016) Brain injury induces specific changes in the caecal microbiota of mice via altered autonomic activity and mucoprotein production. Brain Behav Immun 57:10–20
Maurice CF, Haiser HJ, Turnbaugh PJ (2013) Xenobiotics shape the physiology and gene expression of the active human gut microbiome. Cell 152:39–50
Knights D, Silverberg MS, Weersma RK et al (2014) Complex host genetics influence the microbiome in inflammatory bowel disease. Genome Med 6:107
Fujimura KE, Demoor T, Rauch M et al (2014) House dust exposure mediates gut microbiome Lactobacillus enrichment and airway immune defense against allergens and virus infection. Proc Natl Acad Sci U S A 111:805–810
Goodrich JK, Waters JL, Poole AC et al (2014) Human genetics shape the gut microbiome. Cell 159:789–799
David LA, Maurice CF, Carmody RN et al (2014) Diet rapidly and reproducibly alters the human gut microbiome. Nature 505:559–563
Zhernakova A, Kurilshikov A, Bonder MJ et al (2016) LifeLines cohort study: Population-based metagenomics analysis reveals markers for gut microbiome composition and diversity. Science 352:565–569
Falony G, Joossens M, Vieira-Silva S et al (2016) Population-level analysis of gut microbiome variation. Science 352:560–564
Wang S, Charbonnier LM, Noval Rivas M et al (2015) MyD88 adaptor-dependent microbial sensing by regulatory T cells promotes mucosal tolerance and enforces commensalism. Immunity 43:289–303
Painter KL, Krishna A, Wigneshweraraj S et al (2014) What role does the quorum-sensing accessory gene regulator system play during Staphylococcus aureus bacteremia? Trends Microbiol 22:676–685
Wu B, Capilato J, Pham MP et al (2016) Lipoxin A4 augments host defense in sepsis and reduces Pseudomonas aeruginosa virulence through quorum sensing inhibition. FASEB J 30:2400–2410
Gilbert JA, Quinn RA, Debelius J et al (2016) Microbiome-wide association studies link dynamic microbial consortia to disease. Nature 535:94–103
Lyons JD, Coopersmith CM (2017) Pathophysiology of the gut and the microbiome in the host response. Pediatr Crit Care Med 18:S46–S49
Yu LC, Shih YA, Wu LL et al (2014) Enteric dysbiosis promotes antibiotic-resistant bacterial infection: systemic dissemination of resistant and commensal bacteria through epithelial transcytosis. Am J Physiol Gastrointest Liver Physiol 307:G824–G835
Schuijt TJ, Lankelma JM, Scicluna BP et al (2016) The gut microbiota plays a protective role in the host defence against pneumococcal pneumonia. Gut 65:575–583
Alhasson F, Das S, Seth R et al (2017) Altered gut microbiome in a mouse model of Gulf war illness causes neuroinflammation and intestinal injury via leaky gut and TLR4 activation. PLoS One 12:e0172914
Deplancke B, Gaskins HR (2001) Microbial modulation of innate defense: Goblet cells and the intestinal mucus layer. Am J Clin Nutr 73:1131S–1141S
Guarner F, Malagelada JR (2003) Gut flora in health and disease. Lancet 361:512–519
Cummings JH, Macfarlane GT (1991) The control and consequences of bacterial fermentation in the human colon. J Appl Bacteriol 70:443–459
Shapiro H, Thaiss CA, Levy M et al (2014) The cross talk between microbiota and the immune system: metabolites take center stage. Curr Opin Immunol 30:54–62
Matsumoto T, Ishikawa H, Tateda K et al (2008) Oral administration of Bifidobacterium longum prevents gut-derived Pseudomonas aeruginosa sepsis in mice. J Appl Microbiol 104:672–680
Khailova L, Frank DN, Dominguez JA et al (2013) Probiotic administration reduces mortality and improves intestinal epithelial homeostasis in experimental sepsis. Anesthesiology 119:166–177
Khailova L, Petrie B, Baird CH et al (2014) Lactobacillus rhamnosus GG and Bifidobacterium longum attenuate lung injury and inflammatory response in experimental sepsis. PLoS One 9:e97861
Gauguet S, D’Ortona S, Ahnger-Pier K et al (2015) Intestinal microbiota of mice influences resistance to Staphylococcus aureus pneumonia. Infect Immun 83:4003–4014
Argenta A, Satish L, Gallo P et al (2016) Local application of probiotic bacteria prophylaxes against sepsis and death resulting from burn wound infection. PLoS One 11:e0165294
Brown RL, Sequeira RP, Clarke TB (2017) The microbiota protects against respiratory infection via GM-CSF signaling. Nat Commun 8:1512
Panpetch W, Chancharoenthana W, Bootdee K et al (2018) Lactobacillus rhamnosus L34 attenuates gut translocation-induced bacterial sepsis in murine models of leaky gut. Infect Immun 86:e00700–e00717
Silvestri L, van Saene HK, Zandstra DF et al (2010) Impact of selective decontamination of the digestive tract on multiple organ dysfunction syndrome: Systematic review of randomized controlled trials. Crit Care Med 38:1370–1376
Silvestri L, de la Cal MA, van Saene HK (2012) Selective decontamination of the digestive tract: The mechanism of action is control of gut overgrowth. Intensive Care Med 38:1738–1750
Tian Z, Liu J, Liao M et al (2016) Beneficial effects of fecal microbiota transplantation on ulcerative colitis in mice. Dig Dis Sci 61:2262–2271
Imdad A, Nicholson MR, Tanner-Smith EE et al (2018) Fecal transplantation for treatment of inflammatory bowel disease. Cochrane Database Syst Rev 11:CD012774
Khan MY, Dirweesh A, Khurshid T et al (2018) Comparing fecal microbiota transplantation to standard-of-care treatment for recurrent Clostridium difficile infection: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol 30:1309–1317
Klingensmith NJ, Coopersmith CM (2016) Fecal microbiota transplantation for multiple organ dysfunction syndrome. Crit Care 20:398
Hassan FI, Didari T, Khan F et al (2018) The role of epigenetic alterations involved in sepsis: an overview. Curr Pharm Des 24:2862–2869
van der Poll T, van de Veerdonk FL, Scicluna BP et al (2017) The immunopathology of sepsis and potential therapeutic targets. Nat Rev Immunol 17:407–420
De AK, Laudanski K, Miller-Graziano CL (2003) Failure of monocytes of trauma patients to convert to immature dendritic cells is related to preferential macrophage-colony-stimulating factor-driven macrophage differentiation. J Immunol 170:6355–6362
Chan C, Li L, McCall CE et al (2005) Endotoxin tolerance disrupts chromatin remodeling and NF-kappaB transactivation at the IL-1beta promoter. J Immunol 175:461–468
Foster SL, Hargreaves DC, Medzhitov R (2007) Gene-specific control of inflammation by TLR-induced chromatin modifications. Nature 447:972–978
McCall CE, Yoza BK (2007) Gene silencing in severe systemic inflammation. Am J Respir Crit Care Med 175:763–767
El Gazzar M, Yoza BK, Chen X et al (2008) G9a and HP1 couple histone and DNA methylation to TNFalpha transcription silencing during endotoxin tolerance. J Biol Chem 283:32198–32208
George SJ (2008) Wnt pathway: A new role in regulation of inflammation. Arterioscler Thromb Vasc Biol 28:400–402
El Gazzar M, Yoza BK, Chen X et al (2009) Chromatin-specific remodeling by HMGB1 and linker histone H1 silences proinflammatory genes during endotoxin tolerance. Mol Cell Biol 29:1959–1971
Villar J, Cabrera NE, Casula M et al (2011) WNT/β-catenin signaling is modulated by mechanical ventilation in an experimental model of acute lung injury. Intensive Care Med 37:1201–1209
Kovalchuk I, Walz P, Thomas J et al (2013) The increased expression of proteins involved in proliferation, DNA repair and DNA methylation in spleen of mice exposed to E. coli O157:H7 lipopolysaccharide. Environ Mol Mutagen 54:421–428
Dhas DB, Ashmi AH, Bhat BV et al (2015) Comparison of genomic DNA methylation pattern among septic and non-septic newborns - an epigenome wide association study. Genom Data 3:36–40
Dhas BB, Antony HA, Bhat V et al (2015) Global DNA methylation in neonatal sepsis. Indian J Pediatr 82:340–344
Riggs AD, Jones PA (1983) 5-methylcytosine, gene regulation, and cancer. Adv Cancer Res 40:1–30
Bomsztyk K, Mar D, An D et al (2015) Experimental acute lung injury induces multi-organ epigenetic modifications in key angiogenic genes implicated in sepsis-associated endothelial dysfunction. Crit Care 19:225
Ekaney ML, Otto GP, Sossdorf M et al (2014) Impact of plasma histones in human sepsis and their contribution to cellular injury and inflammation. Crit Care 18:543
Fattahi F, Grailer JJ, Jajou L et al (2015) Organ distribution of histones after intravenous infusion of FITC histones or after sepsis. Immunol Res 61:177–186
Roderburg C, Luedde M, Vargas Cardenas D et al (2013) Circulating microRNA-150 serum levels predict survival in patients with critical illness and sepsis. PLoS One 8:e54612
Wang X, Huang W, Yang Y et al (1842) Loss of duplexmiR-223 (5p and 3p) aggravates myocardial depression and mortality in polymicrobial sepsis. Biochim Biophys Acta 2014:701–711
Rahmel T, Schäfer ST, Frey UH et al (2018) Increased circulating microRNA-122 is a biomarker for discrimination and risk stratification in patients defined by sepsis-3 criteria. PLoS One 13:e0197637
Caserta S, Kern F, Cohen J et al (2016) Circulating plasma microRNAs can differentiate human sepsis and systemic inflammatory response syndrome (SIRS). Sci Rep 6:28006
Xu J, Feng Y, Jeyaram A et al (2018) Circulating plasma extracellular vesicles from septic mice induce inflammation via microRNA- and TLR7-dependent mechanisms. J Immunol 201:3392–3400
Abrams ST, Zhang N, Manson J et al (2013) Circulating histones are mediators of trauma-associated lung injury. Am J Respir Crit Care Med 187:160–169
Li Y, Liu Z, Liu B et al (2014) Citrullinated histone H3: a novel target for the treatment of sepsis. Surgery 156:229–234
Benz F, Roy S, Trautwein C et al (2016) Circulating microRNAs as biomarkers for sepsis. Int J Mol Sci 17:E78
Gore SD, Baylin S, Sugar E et al (2006) Combined DNA methyltransferase and histone deacetylase inhibition in the treatment of myeloid neoplasms. Cancer Res 66:6361–6369
Roger T, Lugrin J, Le Roy D et al (2011) Histone deacetylase inhibitors impair innate immune responses to toll-like receptor agonists and to infection. Blood 117:1205–1217
Ciarlo E, Savva A, Roger T (2013) Epigenetics in sepsis: targeting histone deacetylases. Int J Antimicrob Agents 42(Suppl):S8–S12
Fang J, Lian Y, Xie K et al (2014) Epigenetic modulation of neuronal apoptosis and cognitive functions in sepsis-associated encephalopathy. Neurol Sci 35:283–288
Stiehl T, Thamm K, Kaufmann J et al (2014) Lung-targeted RNA interference against angiopoietin-2 ameliorates multiple organ dysfunction and death in sepsis. Crit Care Med 42:e654–e662
Thangavel J, Samanta S, Rajasingh S et al (2015) Epigenetic modifiers reduce inflammation and modulate macrophage phenotype during endotoxemia-induced acute lung injury. J Cell Sci 128:3094–3105
Thangavel J, Malik AB, Elias HK et al (2014) Combinatorial therapy with acetylation and methylation modifiers attenuates lung vascular hyperpermeability in endotoxemia-induced mouse inflammatory lung injury. Am J Pathol 184:2237–2249
Kim SJ, Baek KS, Park HJ et al (2016) Compound 9a, a novel synthetic histone deacetylase inhibitor, protects against septic injury in mice by suppressing MAPK signalling. Br J Pharmacol 173:1045–1057
Li J, Li M, Su L et al (2015) Alterations of T helper lymphocyte subpopulations in sepsis, severe sepsis, and septic shock: a prospective observational study. Inflammation 38:995–1002
Nullens S, De Man J, Bridts C et al (2018) Identifying therapeutic targets for sepsis research: A characterization study of the inflammatory players in the cecal ligation and puncture model. Mediators Inflamm 2018:5130463
Potjo M, Theron AJ, Cockeran R et al (2019) Interleukin-10 and interleukin-1 receptor antagonist distinguish between patients with sepsis and the systemic inflammatory response syndrome (SIRS). Cytokine 120:227–233
Song Z, Zhang J, Zhang X et al (2015) Interleukin 4 deficiency reverses development of secondary Pseudomonas aeruginosa pneumonia during sepsis-associated immunosuppression. J Infect Dis 211:1616–1627
Schulte W, Bernhagen J, Bucala R (2013) Cytokines in sepsis: potent immunoregulators and potential therapeutic targets–an updated view. Mediators Inflamm 2013:165974
Freeman BD, Buchman TG (2001) Interleukin-1 receptor antagonist as therapy for inflammatory disorders. Expert Opin Biol Ther 1:301–308
Hotchkiss RS, Monneret G, Payen D (2013) Sepsis-induced immunosuppression: From cellular dysfunctions to immunotherapy. Nat Rev Immunol 13:862–874
Tomino A, Tsuda M, Aoki R et al (2017) Increased PD-1 expression and altered T cell repertoire diversity predict mortality in patients with septic shock: A preliminary study. PLoS One 12:e0169653
Buckley CD, Gilroy DW, Serhan CN (2014) Proresolving lipid mediators and mechanisms in the resolution of acute inflammation. Immunity 40:315–327
Nakahira K, Haspel JA, Rathinam VA et al (2011) Autophagy proteins regulate innate immune responses by inhibiting the release of mitochondrial DNA mediated by the NALP3 inflammasome. Nat Immunol 12:222–230
Li Y, Dalli J, Chiang N et al (2013) Plasticity of leukocytic exudates in resolving acute inflammation is regulated by microRNA and proresolving mediators. Immunity 39:885–898
Clemens MG, Chaudry IH, Daigneau N et al (1984) Insulin resistance and depressed gluconeogenic capability during early hyperglycemic sepsis. J Trauma 24:701–708
Hargrove DM, Lang CH, Bagby GJ et al (1989) Epinephrine-induced increase in glucose turnover is diminished during sepsis. Metabolism 38:1070–1076
Matsuda N, Hattori Y, Akaishi Y et al (2000) Impairment of cardiac beta-adrenoceptor cellular signaling by decreased expression of G(s alpha) in septic rabbits. Anesthesiology 93:1465–1473
Boomer JS, To K, Chang KC et al (2011) Immunosuppression in patients who die of sepsis and multiple organ failure. JAMA 306:2594–2605
Bellingan G (2007) Resolution of inflammation. In: Mechanisms of sepsis-induced organ dysfunction. Spinger, New York, NY
Bordon J, Aliberti S, Fernandez-Botran R et al (2013) Understanding the roles of cytokines and neutrophil activity and neutrophil apoptosis in the protective versus deleterious inflammatory response in pneumonia. Int J Infect Dis 17:e76–e83
Crowell KT, Soybel DI, Lang CH (2017) Restorative mechanisms regulating protein balance in skeletal muscle during recovery from sepsis. Shock 47:463–473
Bouglé A, Rocheteau P, Sharshar T et al (2016) Muscle regeneration after sepsis. Crit Care 20:131
Crowell KT, Soybel DI, Lang CH (2017) Inability to replete white adipose tissue during recovery phase of sepsis is associated with increased autophagy, apoptosis, and proteasome activity. Am J Physiol Regul Integr Comp Physiol 312:R388–R399
Kim J, Guan KL (2011) Regulation of the autophagy initiating kinase ULK1 by nutrients: Roles of mTORC1 and AMPK. Cell Cycle 10:1337–1338
Zhao X, Zmijewski JW, Lorne E et al (2008) Activation of AMPK attenuates neutrophil proinflammatory activity and decreases the severity of acute lung injury. Am J Physiol Lung Cell Mol Physiol 295:L497–L504
Park DW, Jiang S, Tadie JM et al (2013) Activation of AMPK enhances neutrophil chemotaxis and bacterial killing. Mol Med 19:387–398
Adrie C, Bachelet M, Vayssier-Taussat M et al (2001) Mitochondrial membrane potential and apoptosis peripheral blood monocytes in severe human sepsis. Am J Respir Crit Care Med 164:389–395
Levy RJ, Piel DA, Acton PD et al (2005) Evidence of myocardial hibernation in the septic heart. Crit Care Med 33:2752–2756
Fredriksson K, Hammarqvist F, Strigård K et al (2006) Derangements in mitochondrial metabolism in intercostal and leg muscle of critically ill patients with sepsis-induced multiple organ failure. Am J Physiol Endocrinol Metab 291:E1044–E1050
Jarkovska D, Markova M, Horak J et al (2018) Cellular mechanisms of myocardial depression in porcine septic shock. Front Physiol 9:726
Comim CM, Rezin GT, Scaini G et al (2008) Mitochondrial respiratory chain and creatine kinase activities in rat brain after sepsis induced by cecal ligation and perforation. Mitochondrion 8:313–318
Fink MP (2002) Bench-to-bedside review: Cytopathic hypoxia. Crit Care 6:491–499
Carré JE, Singer M (1777) Cellular energetic metabolism in sepsis: The need for a systems approach. Biochim Biophys Acta 2008:763–771
Haden DW, Suliman HB, Carraway MS et al (2007) Mitochondrial biogenesis restores oxidative metabolism during Staphylococcus aureus sepsis. Am J Respir Crit Care Med 176:768–777
Zolfaghari PS, Carré JE, Parker N et al (2015) Skeletal muscle dysfunction is associated with derangements in mitochondrial bioenergetics (but not UCP3) in a rodent model of sepsis. Am J Physiol Endocrinol Metab 308:E713–E725
Verma R, Huang Z, Deutschman CS et al (2009) Caffeine restores myocardial cytochrome oxidase activity and improves cardiac function during sepsis. Crit Care Med 37:1397–1402
Piel DA, Deutschman CS, Levy RJ (2008) Exogenous cytochrome C restores myocardial cytochrome oxidase activity into the late phase of sepsis. Shock 29:612–616
Park DW, Zmijewski JW (2017) Mitochondrial dysfunction and immune cell metabolism in sepsis. Infect Chemother 49:10–21
Doerrier C, García JA, Volt H et al (2015) Identification of mitochondrial deficits and melatonin targets in liver of septic mice by high-resolution respirometry. Life Sci 121:158–165
Arulkumaran N, Pollen S, Greco E et al (2018) Renal tubular cell mitochondrial dysfunction occurs despite preserved renal oxygen delivery in experimental septic acute kidney injury. Crit Care Med 46:e318–e325
Carré JE, Orban JC, Re L et al (2010) Survival in critical illness is associated with early activation of mitochondrial biogenesis. Am J Respir Crit Care Med 182:745–751
Giovannini I, Boldrini G, Castagneto M et al (1983) Respiratory quotient and patterns of substrate utilization in human sepsis and trauma. JPEN J Parenter Enteral Nutr 7:226–230
Orsi A, Rees D, Beltran B: Physiological regulation and pathological inhibition of tissue respiration by nitric oxide in vivo. In: The Biology of Nitric Oxide, Part 7. Moncada S, Gustafsson LE, Wiklund NP, et al (Eds). London, United Kingdom, Portland Press, 2000, pp 35
Singer M, De Santis V, Vitale D et al (2004) Multiorgan failure is an adaptive, endocrine-mediated, metabolic response to overwhelming systemic inflammation. Lancet 364:545–548
James JH, Fang CH, Schrantz SJ et al (1996) Linkage of aerobic glycolysis to sodium-potassium transport in rat skeletal muscle. Implications for increased muscle lactate production in sepsis. J Clin Invest 98:2388–2397
Levy B, Desebbe O, Montemont C et al (2008) Increased aerobic glycolysis through beta2 stimulation is a common mechanism involved in lactate formation during shock states. Shock 30:417–421
Garcia-Alvarez M, Marik P, Bellomo R (2014) Sepsis-associated hyperlactatemia. Crit Care 18:503
Um JH, Yun J (2017) Emerging role of mitophagy in human diseases and physiology. BMB Rep 50:299–307
Pickles S, Vigie P, Youle RJ (2018) Mitophagy and quality control mechanisms in mitochondrial maintenance. Curr Biol 28:R170–R185
Rosas-Ballina M, Valdés-Ferrer SI, Dancho ME et al (2015) Xanomeline suppresses excessive pro-inflammatory cytokine responses through neural signal-mediated pathways and improves survival in lethal inflammation. Brain Behav Immun 44:19–27
Pavlov VA, Tracey KJ (2012) The vagus nerve and the inflammatory reflex—linking immunity and metabolism. Nat Rev Endocrinol 8:743–754
Rana M, Fei-Bloom Y, Son M et al (2018) Constitutive vagus nerve activation modulates immune suppression in sepsis survivors. Front Immunol 9:2032
Chavan SS, Huerta PT, Robbiati S et al (2012) HMGB1 mediates cognitive impairment in sepsis survivors. Mol Med 18:930–937
Comim CM, Cassol OJ Jr, Abreu I et al (2012) Erythropoietin reverts cognitive impairment and alters the oxidative parameters and energetic metabolism in sepsis animal model. J Neural Transm (Vienna) 119:1267–1274
Hu Y, Huang M, Wang P et al (2013) Ucf-101 protects against cerebral oxidative injury and cognitive impairment in septic rat. Int Immunopharmacol 16:108–113
Zhang S, Wang X, Ai S et al (2017) Sepsis-induced selective loss of NMDA receptors modulates hippocampal neuropathology in surviving septic mice. PLoS One 12:e0188273
Gasparotto J, Girardi CS, Somensi N et al (2018) Receptor for advanced glycation end products mediates sepsis-triggered amyloid-β accumulation, Tau phosphorylation, and cognitive impairment. J Biol Chem 293:226–244
Zarbato GF, de Souza Goldim MP, Giustina AD et al (2018) Dimethyl fumarate limits neuroinflammation and oxidative stress and improves cognitive impairment after polymicrobial sepsis. Neurotox Res 34:418–430
Assis MS, Soares AC, Sousa DN et al (2018) Effects of caffeine on behavioural and cognitive deficits in rats. Basic Clin Pharmacol Toxicol 123:435–442
Della Giustina A, Goldim MP, Danielski LG et al (2020) Fish oil-rich lipid emulsion modulates neuroinflammation and prevents long-term cognitive dysfunction after sepsis. Nutrition 70:110417
Yang Y, Liang S, Li Y et al (2019) Effects of early administration of insulin-like growth factor-1 on cognitive function in septic encephalopathy. Neuropsychiatr Dis Treat 15:323–337
Zong MM, Zhou ZQ, Ji MH et al (2019) Activation of β2-Adrenoceptor attenuates sepsis-induced hippocampus-dependent cognitive impairments by reversing neuroinflammation and synaptic abnormalities. Front Cell Neurosci 13:293
Funding
Dr. Coopersmith’s institution received funding from the National Institutes of Health.
Author information
Authors and Affiliations
Consortia
Contributions
The author (s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is being simultaneously published in Critical Care Medicine (https://doi.org/10.1097/CCM.0000000000004408) and Intensive Care Medicine Experimental (https://doi.org/10.1186/s40635-020-00312-4).
Appendix
Appendix
Members of the Surviving Sepsis Campaign Research Committee: Craig M. Coopersmith, MD, MCCM, Co-chair (Atlanta, GA); Daniel De Backer, MD, Co-chair (Brussels, Belgium); Massimo Antonelli, MD (Rome, Italy); Clifford S. Deutschman, MS, MD, MCCM (Manhasset, NY); Laura Evans, MD, MSc, FCCM (Seattle, WA—Consultant); Ricard Ferrer-Roca, MD, PhD (Barcelona, Spain); Judith Hellman, MD (San Francisco, CA); Sameer Jog, MD; Jozef Kesecioglu, MD, PhD (Utrecht, The Netherlands); Ishaq Lat, PharmD (Chicago, IL); Mitchell M. Levy, MD, MCCM (Providence, RI); Flavia Machado, MD, PhD (Sao Paulo, Brazil); Greg Martin, MD, MSc, FCCM (Atlanta, GA); Ignacio Martin-Loeches, MD, PhD, FJFICMI; Mark E. Nunnally, MD, FCCM (New York, NY); and Andrew Rhodes, MBChB, FRCP, FRCA, FFICM (London, United Kingdom—Consultant).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Deutschman, C.S., Hellman, J., Roca, R.F. et al. The surviving sepsis campaign: basic/translational science research priorities. ICMx 8, 31 (2020). https://doi.org/10.1186/s40635-020-00312-4
Published:
DOI: https://doi.org/10.1186/s40635-020-00312-4