Abstract
Purpose
Although most patellar dislocations are associated with medial patellofemoral ligament (MPFL) injury, many patients also sustain concomitant patellar osteochondral fractures following a patellar dislocation. Few prior studies have described or evaluated risk factors for patellar osteochondral fractures in pediatric patients. The purpose of the present study was to describe the incidenceand location of patellar osteochondral fractures following acute patellar dislocation in pediatric patients. In addition, we described risk factors for patellar osteochondral fractures in this population. We hypothesized that most fractures would occur at the inferomedial quadrant of the patella following a traumatic injury mechanism.
Methods
Following Institutional Review Board approval, the electronic medical record was queried to identify pediatric patients ≤ 18 years old who underwent MPFL reconstruction (MPFLR) or non-operative treatment for patellar instability between July 2016 and February 2020. Osteochondral fractures were defined as full-thickness chondral injuries with attached subchondral bone or purely osseous injuries measuring ≥ 3 mm (mm) in at least two magnetic resonance imaging (MRI) planes. Patients were included in the study if they had complete preoperative x-ray and MRI studies with minimum 6-month follow-up. Patients were excluded if they had incomplete imaging, isolated chondral fractures, or less than 6 months follow-up. Univariate analysis was used to identify patient factors associated with osteochondral fractures. Multivariate regression analysis was used to identify risk factors for osteochondral fractures.
Results
Sixty patients (63 knees) were included in the study, 15 (23.8%) of whom had a patellar osteochondral fracture. The majority of osteochondral fractures (87%) involved the inferomedial quadrant of the patella. Univariate analysis showed an association between male sex (p = 0.041), skeletal immaturity (p = 0.028), and decreased patellar tilt (p = 0.021) and patellar osteochondral fractures. Multivariate regression analysis identified male sex as an independent risk factor for osteochondral fractures (relative risk: 4.8, 95% confidence interval [CI]: 1.08–20.9, p = 0.039). No patients had recurrent dislocation at minimum 6-month follow-up. All patients with osteochondral fractures returned to sports at most recent follow up.
Conclusion
In this study, 23% of pediatric patients with acute patellar dislocations have a concomitant patellar osteochondral fracture. The majority of patellar osteochondral fractures involve the inferomedial quadrant of the patella. Male sex is an independent risk factor for patellar osteochondral fractures, and skeletal immaturity is associated with patellar osteochondral fractures in this population.
Level of evidence
Level III.
Similar content being viewed by others
Introduction
Acute patellar dislocations (APDs) are a common cause of knee pain in pediatric patients [3]. Twenty-nine per 100,000 children will sustain at least one patellar dislocation between the ages of 10 and 17 [6], with 35% of these patients experiencing recurrent patellar dislocations [8]. Well-established risk factors for APD include trochlear dysplasia, increased tibial tubercle-to-trochlear groove (TT-TG) distance, increased lateral patellofemoral tilt, torsional malalignment of the femur/tibia, and patella alta [19].
The majority (96–97%) of APDs are associated with injury to the medial patellofemoral ligament (MPFL [8, 24]), which functions as the primary soft tissue restraint to lateral patellar translation at 0–30 degrees of knee flexion [11]. Although MPFL injuries are a common sequela of APDs, concomitant pathologies, including chondral or osteochondral injuries of the patella, trochlea, or lateral femoral condyle, and medial collateral ligament injuries, are also frequently associated with these injuries [4, 32].
The incidence and characteristic patterns of concomitant patellar osteochondral fractures in adults with APDs are well-described. Eleven to 76% of adults sustain osteochondral fractures following patellar dislocation, the majority of which (42 – 63%) involve the patella [15, 29, 30]. Mochizuki et al. [12] found that 84% of patellar osteochondral fractures in adults with APD were at the inferomedial border of the patella, whereas the minority of patients (16%) sustained superomedial patellar osteochondral fractures. Other studies [4, 25, 27] have similarly found that the majority of patellar osteochondral fractures involve the medial margin or inferomedial facet of the patella in mixed cohorts of pediatric and adult patients.
Patellar osteochondral fractures are a relatively common sequela of APD in children, with a reported incidence of 29% in first-time dislocation events [14]. A previous investigation demonstrated that the majority of chondral and osteochondral fractures associated with APD in pediatric patients involved the patella (versus the lateral femoral condyle), with the medial and inferomedial portions of the patella most commonly affected [10]. In addition, APDs associated with a traumatic mechanism were associated with a 42-time increased risk of chondral or osteochondral injury of the patella [10]. However, the aforementioned study did not separate grade IV chondral defects from true osteochondral fractures in their analyses. It is critical to evaluate outcomes following osteochondral injury in this patient population, as these injuries are often managed differently than pure chondral injuries. There is a paucity of information in the literature regarding the incidence and patterns of patellar osteochondral injuries following APD in pediatric patients. In addition, no prior studies have evaluated radiographic risk factors for patellar osteochondral fracture in pediatric patients with APD.
The primary aim of the present study was to describe the incidenceand location of patellar osteochondral fractures in pediatric patients with acute patellar dislocations. The secondary aim of the study was to describe risk factors for concomitant patellar osteochondral fracture, surgical management, and recurrent dislocation rate in this patient population at mid-term follow-up. The authors hypothesized that the majority of fractures would involve the inferomedial quadrant of the patella and occur more frequently following traumatic injury mechanisms.
Materials and methods
Patient selection
Institutional review board (IRB) approval was obtained at our institution prior to initiation of the study (IRB number: 2020–0203). We conducted a retrospective review of a consecutive series of pediatric patients treated for acute patellar dislocation at a single tertiary care center between July 2016 and February 2020. All surgical procedures were performed by a single pediatric orthopaedic sports medicine-trained orthopaedic surgeon (D.W.G.). Eligible patients were identified either by query of the electronic medical record by procedure type (MPFL reconstruction) and surgeon (D.W.G.) or ICD-10 code for patellar instability (M2200, M2201, M2202, M2210, M2211, M2212) from July 2016 to February 2020.
Patients were included in the study if they were ≤ 18 years old and underwent pre-operative anteroposterior, lateral, and Merchant view plain radiographs and standard magnetic resonance imaging (MRI) of the affected knee. Inclusion criteria also consisted of minimum 6-month postoperative follow-up for patients who underwent surgery or minimum 6-month clinical follow-up post-diagnosis if they elected to pursue non-operative treatment. Patients with incomplete imaging, isolated chondral fractures, or less than 6 months of postoperative/post-diagnosis clinical follow-up were excluded from analysis.
Surgical technique for skeletally immature patients
Hamstring autograft was used for all patients. A 2 cm posteromedial incision is made over the proximal tibia, and a tendon harvester is used for semitendinosus tendon harvest. The graft is prepared for double-bundle reconstruction, with a target final graft length of 60 mm, including 20 mm in the femoral socket. A 3 cm anteromedial incision is made over the patella, and the medial border of the patella is exposed. Two patellar sockets are drilled in the proximal half of the patella to a depth of 12-15 mm. A 2 cm incision is made over the femoral MPFL insertion site. A guidewire is placed at Schöttle’s point [23] in the epiphysis of the distal femur aimed from medial to lateral, 5-7 mm distal to the physis.
A femoral socket is drilled to a depth of 20 mm. The doubled end of the graft is placed into the femoral socket and secured with an interference screw. The graft is then passed between layers 2 and 3 of the knee, and the graft length is determined based on the appropriate tension at 30 degrees of knee flexion. The two free ends of the graft are secured to the patellar sockets with suture anchors. The knee is brought through full range of motion for a final check of graft isometry [26].
Surgical technique for skeletally mature patients
Like the skeletally immature patients, hamstring autograft was used for skeletally mature patients who had closed distal femoral physes on magnetic resonance imaging (MRI) using the same technique described above. The graft is prepared for double-bundle reconstruction, and the patellar sockets are prepared in the same fashion. A 2 cm incision is used at the MPFL insertion site on the femur, and a guidewire is placed at Schottle’s point [23]. However, unlike the skeletally immature patients, the guidewire is aimed proximally, from medial and distal to proximal and lateral, in the distal femur. A 40 mm femoral socket is drilled, and the guidewire is passed through the distal femur. The midportion of the graft is identified and secured to the patella with loaded suture anchors. The graft is passed between layers 2 and 3 of the knee, and the sutures at the free ends of the graft are passed through the femur following the guidewire. An interference screw is used to secure the graft in the femoral socket. The knee is brought through range of motion to check graft isometry.
Osteochondral fracture definition and radiographic analysis
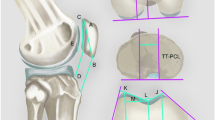
Patellar fractures were defined as either full-thickness chondral injuries with attached subchondral bone (osteochondral) or purely osseous injuries (without associated articular cartilage) measuring ≥ 3 mm in at least two MRI planes (sagittal, axial, or coronal). Patellar fractures without at least 3 mm of bone in two or more MRI planes were excluded from analysis. Patellar osteochondral fractures were categorized by location (Fig. 1). Patient demographic, perioperative, and post-operative clinical data were obtained via review of the electronic medical record. Traumatic injury mechanism was classified as an injury occurring after a fall or during a sporting event.
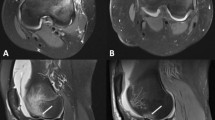
Patellar tilt was calculated as the angle between a line parallel to the articular surface of the patella and a line connecting the summits of the medial and lateral femoral condyles on Merchant view radiographs (Fig. 2) [13]. The Caton Deschamps Index (CDI) was calculated as the ratio of the distance between the articular surface of the tibia and the inferior-most aspect of the articular surface of the patella divided by the length of the articular surface of the patella on sagittal MRI, one to two slices lateral to the ACL insertion (Fig. 3) [18]. The tibial tubercle-trochlear groove (TT-TG) distance was calculated as the distance between the tibial tubercle and the deepest portion of the trochlear groove on axial MRI (Fig. 4) [17]. Measurements were performed by two blinded senior orthopaedic surgery residents (.,.). Each measurement was performed twice by each observer with a break of at least 2 weeks between measurements.
Statistical analysis
Descriptive statistics were used to evaluate patient and fracture characteristics. Means and standard deviations were used for continuous data, whereas categorical data was reported as frequencies and percentages. Data for age, TT-TG, CDI, and patellar tilt were normally distributed per the results of the Shapiro–Wilk test; therefore, unpaired t-tests were used for analysis. Data for BMI was not normally distributed based on Shapiro–Wilk test results, and Wilcoxon Rank-Sum test was used for analysis. Categorical data were analyzed with Fisher’s exact tests. Poisson regressions with robust error variance (multivariate analysis) were used to determine association between each patient characteristic and occurrence of a fracture. Two-way mixed inter- and intraclass correlation coefficients were calculated for each measurement. Data analysis was performed with STATA (Version 17.0, StataCorp). Statistical significance was determined at the α < 0.05 level.
Results
A total of 80 patients (84 knees) were identified, 60 of whom (63 knees) remained following application of exclusion criteria. Of the patients included in the study, the mean age was 14.2 ± 1.8 years, and mean BMI was 21.9 ± 7.8. Thirty-two patients (53.3%) were female, and 30 (47.6%) were right knees (Table 1). Thirty-six patients (60%) were first-time dislocators, 49 knees (77.8%) were skeletally immature, and 45 (76.3%) had a traumatic injury mechanism. Fifty-six knees (89.9%) underwent surgery, the majority of whom underwent MPFLR (47 patients, 84%). The average follow-up was 2.7 ± 1.5 years.
Fifteen knees (23.8%) sustained osteochondral fractures, and the majority of fractures involved the inferomedial quadrant (Zone IV, 13 fractures, 86.7%, Table 2). Thirteen of the 15 fractures (86.7%) were visible on merchant XR, whereas only half (n = 8/15, 53.5%) were visible on AP knee XR (Table 2). The majority (86.7%) of fractures involved articular cartilage (Table 2). There were two purely osseous fractures (no associated articular cartilage), both of which occurred in zone IV.
Patients with osteochondral fractures were more likely to be male (n = 11/15 versus 20/48, p = 0.041) and skeletally immature (n = 15/15 versus 34/48, Table 3, p = 0.028). There was no difference in age between patients with osteochondral fractures (average age 13.6 ± 1.7 years) compared to those without osteochondral fractures (average age 14.4 ± 1.8 years, Table 3). There were also no differences in average BMI (21.6 ± 3.8 versus 22.1 ± 5.1, respectively, p = 0.82), laterality (7/15 versus 23/49 right knees, respectively, p = 1.0), or average follow-up (2.5 ± 1.8 years versus 2.8 ± 1.4 years, respectively, p = 0.25) between the two groups. There were no differences between the two groups with regard to injury mechanism (traumatic versus atraumatic, p = 0.15) or history of prior dislocation (Table 3, p = 0.23). There was also no association between sex and skeletal maturity (p = 0.25) or sex and age (p = 0.34) in the entire cohort.
There were no differences in average CDI values (1.33 ± 0.2 versus 1.42 ± 0.2, respectively, p = 0.079) or TT-TG values between the two groups (15.7 ± 5.4 versus 17.8 ± 4.7, respectively, Table 3, p = 0.12). Patients without osteochondral fractures had increased patellar tilt (17.8 ± 6.8°) compared to those with osteochondral fractures (12.6 ± 5.9°, Table 3, p = 0.021).
The majority of patients with and without osteochondral fractures underwent surgical intervention (86.7% and 76.8%, respectively, p = 0.67). Among those with osteochondral fractures who underwent surgery (n = 13), 5 patients (38.5%) underwent MPFL reconstruction (MPFLR) with patellar open reduction and internal fixation (ORIF) and 8 (61.5%) underwent MPFLR only (Table 4). All of the patients who underwent MPFLR + ORIF had articular cartilage involvement (n = 5, 100%), whereas 62.5% (5 patients) of those who underwent MPFLR only had articular cartilage involvement (Table 4, p = 0.061). There were no recurrent patellar dislocations at most recent follow-up in either group. All patients with osteochondral fractures (n = 15) returned to sports at most recent follow up.
Multivariate regression analysis was also performed to control for patient factors. Statistically significant variables from univariate analysis were used as inputs to the model except for skeletal maturity, which was excluded from the model given that there were no occurrences in the reference group for this characteristic. Male sex was an independent risk factor for osteochondral fractures in our cohort (relative risk (RR) 4.8, 95% confidence interval [CI]: 1.08–20.9, p = 0.039), whereas patellar tilt was no longer significant following multivariate regression analysis (RR: 0.96, 95% CI: 0.90–1.01, p = 0.133, Table 5).
Two-way mixed intraclass correlation coefficient values were as follows: CDI: 0.75, TTTG: 0.90, patellar tilt: 0.81, osteochondral fracture location: 0.77. Two-way mixed interclass correlation coefficient values were as follows: CDI: 0.77, TTTG: 0.76, patellar tilt: 0.90, osteochondral fracture location: 0.77.
Discussion
We found that patellar osteochondral fractures occurred in 23% of pediatric patients with APD, and the majority of osteochondral fractures involved the inferomedial quadrant of the patella. Male sex was an independent risk factor for patellar osteochondral fractures, as males were 4.8 times more likely to sustain an osteochondral fracture than their female counterparts. In addition, skeletal immaturity was associated with osteochondral fractures in our cohort. No patients in either group had a recurrent dislocation at minimum 6-month follow-up.
Although there is a wide range of reported rates of associated osteochondral fractures in adults with APD reported in the literature (11–76%) [15, 29, 30], we found that 23% of pediatric patients with APD sustained a concomitant patellar osteochondral fracture in our cohort, similar to what has previously been described by Nietosvaara et al. in a pediatric population (29%) [14]. However, unlike Nietosvaara et al. [14], we found a higher rate of patellar osteochondral fracture after first-time dislocation (73% versus 29%).
Like Jungesblut et al. [10] and Mochizuki et al. [12], we found that the majority of osteochondral fractures of the patella involved the inferomedial quadrant. However, unlike Jungesblut et al., we did not find an association between traumatic injury mechanism and patellar osteochondral fractures, although we did find an association between male sex and skeletal immaturity with these fractures. The lack of association between traumatic injury mechanism and the presence of osteochondral fracture was a surprising finding in the present study, although patients with osteochondral fractures tended to be more likely to sustain their injuries via traumatic injury mechanism (93%) compared to patients without osteochondral fractures (71%). However, defining traumatic injury mechanism can pose a challenge, as there are inherent differences between a direct blow to the knee and a non-contact twisting injury during a sporting event. It was not possible to distinguish direct blows from non-contact twisting injuries during sports from the data available in our retrospective chart review, although future prospective studies may better evaluate the association between direct blow versus non-contact twisting injury mechanisms and the presence of patellar osteochondral fractures.
The present study builds on the existing literature by including a skeletally immature patients (average age 14.2 ± 1.8 years) who sustained patellar osteochondral fractures with articular cartilage involvement. Mochizuki et al. [12], by contrast, examined a group of older, skeletally mature patients (average age 18.5 years, 95% CI 16.1 – 20.9 years). It is important to consider skeletal maturity status when studying patellar instability in pediatric patients, as numerous prior studies have shown that skeletal immaturity is a risk factor for recurrent patellar dislocation [9, 22, 28]. Moreover, Mochizuki et al. excluded patients with isolated osteochondral fractures with articular involvement, yet articular cartilage involvement in common in patellar osteochondral fractures [21, 32].
Results of a previous histological study by Flachsmann et al. [7] may explain the higher rates of patellar osteochondral fractures in skeletally immature individuals in our cohort. Per Flachsmann et al. [7], uncalcified cartilage in skeletally immature patients weaves with subchondral bone, which renders the subchondral bone more susceptible to failure than the tidemark, which is weaker and thus more prone to failure in skeletally mature patients.
Males were 4.8 times more likely to sustain concomitant patellar osteochondral fractures than females in our cohort. This result is in line with Zheng et al. [32], who found that adolescent males were more likely to sustain a patellar chondral injury compared to adolescent females following APD. One possible explanation for this finding is that males are, on average, more skeletally immature than their female counterparts for a given chronological age [2]. In the present study, skeletal maturity was categorized as a categorical variable for the sake of statistical analysis, but in reality, skeletal maturity exists along a spectrum. Even though it is challenging to determine the degree of skeletal maturity without hand-for-bone-age XR, it is possible that the males in the present study were more skeletally immature or had a younger average skeletal age than their female counterparts, despite no differences in chronological age between these groups. Therefore, males may be more likely to sustain patellar osteochondral fractures following APD than females because they are more skeletally immature and thus have a weaker subchondral bone relative to the tidemark than females of similar chronological age.
With regard to radiographic parameters, patients without osteochondral fractures had increased patellar tilt compared to patients with osteochondral fractures. In addition, TT-TG and CDI values tended to be higher on average in the no fracture group compared to the fracture group, although this finding was not significant. Given that increased patellar tilt, CDI, and TT-TG are risk factors for patellar dislocations [1], it could be hypothesized that patients with the aforementioned risk factors could sustain a patellar dislocation via lower energy mechanisms and thus would be less likely to sustain a concomitant osteochondral fracture than those without risk factors for APD, who would likely require a greater amount of force in order to dislocate the patella.
There were two purely osseous fractures in our cohort, both of which occurred in zone IV. It is likely that these purely osseous zone IV fractures occurred as a result of a medial patellotibial ligament (MPTL) avulsion, as opposed to a medial patellofemoral ligament avulsion. The MPTL originates on the distal third of the medial border of the patella and inserts just medial to the patellar tendon insertion approximately 15 mm distal to the joint line [5]. Several prior studies have described the importance of the MPTL as a secondary restraint to lateral translation and rotation of the patella, particularly from 45° to 90° of knee flexion [16, 20], and combined MPFL and MPTL reconstruction has been shown to have good outcomes at mid-term follow up in patients with patellofemoral instability and patella alta [31].
There are several limitations to the present study. Given the retrospective nature of this study, our results are limited by selection bias, as the type and timing of surgical management were not randomized. In addition, our small sample size renders our study susceptible to type II error, particularly for variables which approached significance, such as CDI. There was also heterogeneity in our study population, as more than one third of the patients included in our study had a history of at least two patellar dislocations. However, we argue that rate of recurrent patellar dislocations in our study population is representative of pediatric patients with APD. Moreover, given the underlying assumptions of Poisson regression model, we were unable to evaluate skeletal immaturity as a risk factor for osteochondral fractures, as there were no skeletally mature patients with osteochondral fractures in our cohort. However, skeletal maturity was associated with osteochondral fractures in univariate analysis, and there was no association between skeletal maturity and gender in univariate analysis. Finally, the present study only included short-term follow-up (minimum 6 months), and future studies can include longer-term follow-up.
In conclusion, male sex is an independent risk factor for patellar osteochondral fractures, and skeletal immaturity is associated with patellar osteochondral fractures in pediatric patients. The majority of patients have good outcomes, including a low recurrence rate, at short-term follow-up.
References
Askenberger M, Janarv PM, Finnbogason T, Arendt EA (2017) Morphology and anatomic patellar instability risk factors in first-time traumatic lateral patellar dislocations. Am J Sports Med 45(1):50–58
Cavallo F, Mohn A, Chiarelli F, Giannini C (2021) Evaluation of bone age in children: a mini-review. Front Pediatr 9:21
DeFroda SF, Gil JA, Boulos A, Cruz AI (2017) Diagnosis and management of traumatic patellar instability in the pediatric patient. Orthopedics 40(5):e749–e757
Elias DA, White LM, Fithian DC (2002) Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology 225(3):736–743
Felli L, Alessio-Mazzola M, Lovisolo S, Capello AG, Formica M, Maffulli N (2021) Anatomy and biomechanics of the medial patellotibial ligament: a systematic review. Surgeon 19(5):e168–e174
Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA, White LM (2004) Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 32(5):1114–1121
Flachsmann R, Broom ND, Hardy AE, Moltschaniwskyj G (2000) Why is the adolescent joint particularly susceptible to osteochondral shear fracture? Clin Orthop Relat Res 381:212–221
Höhne S, Gerlach K, Irlenbusch L, Schulz M, Kunze C, Finke R (2017) Patella dislocation in children and adolescents. Z Orthop Unfall 155(2):169–176
Jaquith BP, Parikh SN (2017) Predictors of recurrent patellar instability in children and adolescents after first-time dislocation. J Pediatr Orthop 37(7):484–490
Jungesblut W, Rupprecht M, Schroeder M, Krajewski KL, Stuecker R, Berger-Groch J, Strahl A, Hubert J, Jungesblut OD (2022) Localization and likelihood of chondral and osteochondral lesions after patellar dislocation in surgically treated children and adolescents. Orthop J Sports Med 10(12):23259671221134104
Krebs C, Tranovich M, Andrews K, Ebraheim N (2018) The medial patellofemoral ligament: review of the literature. J Orthop 15(2):596–599
Mochizuki T, Tanifuji O, Watanabe S, Katsumi R, Tomiyama Y, Sato T, Endo N (2020) The majority of patellar avulsion fractures in first-time acute patellar dislocations included the inferomedial patellar border that was different from the medial patellofemoral ligament attachment. Knee Surg Sports Traumatol Arthrosc 28(12):3942–3948
Murayama K, Nakayama H, Murakami T, Yoshiya S, Otsuki S, Tachibana T (2018) The effect of concomitant arthroscopic lateral retinacular release on postoperative patellar position and orientation in open wedge high tibial osteotomy. Knee Surg Relat Res 30(3):241–246
Nietosvaara Y, Aalto K, Kallio PE (1994) Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop 14(4):513–515
Nomura E, Inoue M, Kurimura M (2003) Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy 19(7):717–721
Panagiotopoulos E, Strzelczyk P, Herrmann M, Scuderi G (2006) Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 14(1):7–12
Pandit S, Frampton C, Stoddart J, Lynskey T (2011) Magnetic resonance imaging assessment of tibial tuberosity-trochlear groove distance: Normal values for males and females. Int Orthop 35(12):1799–1803
Paul RW, Brutico JM, Wright ML, Erickson BJ, Tjoumakaris FP, Freedman KB, Bishop ME (2021) Strong agreement between magnetic resonance imaging and radiographs for caton-deschamps index in patients with patellofemoral instability. Arthrosc Sports Med Rehabil 3(6):e1621–e1628
Pauyo T, Park JP, Bozzo I, Bernstein M (2022) Patellofemoral instability part i: evaluation and nonsurgical treatment. J Am Acad Orthop Surg 30(22):E1431–E1442
Philippot R, Boyer B, Testa R, Farizon F, Moyen B (2012) The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc 20(2):331–336
Salonen EE, Magga T, Sillanpää PJ, Kiekara T, Mäenpää H, Mattila VM (2017) Traumatic patellar dislocation and cartilage injury: a follow-up study of long-term cartilage deterioration. Am J Sports Med 45(6):1376–1382
Sanders TL, Pareek A, Hewett TE, Stuart MJ, Dahm DL, Krych AJ (2018) High rate of recurrent patellar dislocation in skeletally immature patients: a long-term population-based study. Knee Surg Sports Traumatol Arthrosc 26(4):1037–1043
Schöttle PB, Schmeling A, Rosenstiel N, Weiler A (2007) Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med 35(5):801–804
Seeley MA, Knesek M, Vanderhave KL (2013) Osteochondral injury after acute patellar dislocation in children and adolescents. Journal of Pediatric Orthopaedics 33(5):511–518
Shtarker H, Assaf M, Deltoff MN (2018) A new minimally invasive surgical technique for medial retinaculum repair following traumatic patellar dislocation. Eur J Orthop Surg Traumatol 28(5):811
Sidharthan S, Wang G, Schlichte LM, Fulkerson JP, Green DW (2020) Medial patellofemoral ligament reconstruction in skeletally immature patients. JBJS Essent Surg Tech 10(1):e0110
Song SY, Kim TS, Seo YJ (2020) Initial conservative treatment of osteochondral fracture of the patella following first-time patellar dislocation. BMC Musculoskelet Disord 21(1):1–8
Twomey KD, Fornari ED, Kirschner N, Sever R, Hanstein R (2019) Risk factors for recurrent patellar instability in children and adolescents. Pediatrics 144(2_MeetingAbstract):764
Uimonen M, Ponkilainen V, Paloneva J, Mattila VM, Nurmi H, Repo JP (2021) Characteristics of osteochondral fractures caused by patellar dislocation. Orthop J Sports Med 9(1):2325967120974649
Virolainen H, Visuri T, Kuusela T (1993) Acute dislocation of the patella: MR findings. Radiology 189(1):243–246
Yang Y, Zhang Q (2019) Reconstruction of the medial patellofemoral ligament and reinforcement of the medial patellotibial ligament is an effective treatment for patellofemoral instability with patella alta. Knee Surg Sports Traumatol Arthrosc 27(8):2599–2607
Zheng L, Ding H, Feng Y, Sun B, Zhu L, Zhang G (2021) Gender-related differences in concomitant articular injuries after acute lateral patellar dislocation. Injury 52(6):1549–1555
Acknowledgements
None.
Informed consent
Not required for this study, as it was retrospective.
Funding
None.
Author information
Authors and Affiliations
Contributions
JSR, TJU, DEC, and DWG developed the methodology of this protocol. JSR, TJU, DEC, and DWG drafted the manuscript. PB provided all statistical analyses and calculations. JSR, TJU, DEC, PB, and DWG edited and approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was reviewed and approved by the Hospital for Special Surgery Institutional Review Board.
Competing interests
JSR, TJU, DEC, and PB have no conflicts of interest to disclose. DWG is a consultant for Arthrex Inc. and receives royalties for Arthrex Inc. and Pega Medical.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Retzky, J.S., Uppstrom, T.J., Chipman, D.E. et al. Male sex is an independent risk factor for patellar osteochondral fractures following acute patellar dislocation in pediatric patients. J EXP ORTOP 10, 87 (2023). https://doi.org/10.1186/s40634-023-00646-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-023-00646-4