Abstract
Purpose
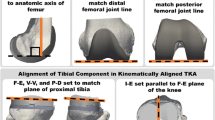
Gait analysis was used to evaluate knee kinematics in patients who underwent successful primary total knee arthroplasty (TKA) using two modern bi-cruciate substituting designs. The knee joint was balanced intraoperatively using real-time sensor technology, developed to provide dynamic feedback regarding stability and tibiofemoral load. The authors hypothesized that major differences exist in gait parameters between healthy controls and post-TKA patients.
Methods
Ten patients who underwent successful TKA using bi-cruciate substituting designs were evaluated at a minimum of 9 months postoperatively using three-dimensional knee kinematic analysis; a multi-camera optoelectronic system and a force platform were used. Sensor-extracted kinematic data included knee flexion angle at heel-strike (KFH), peak midstance knee flexion angle (MSKFA), maximum and minimum knee adduction angle (KAA) and knee rotational angle at heel-strike. Multiple gait analysis data from the study group were compared to a group of ten healthy controls who were matched by age, sex and BMI. Clinical outcome in the TKA group was also measured using the Knee injury and Osteoarthritis Outcome Score (KOOS).
Results
Clinically, at final follow-up, a statistically significant difference in pain, general symptoms, and activities of daily living was seen between the groups. From a gait analysis standpoint, TKA patients had significantly less rotation at heel strike (p = 0.04), lower late stance peak extension moments (p = 0.02), and less Knee Adduction Angle excursion during swing phase (p = 0.04) compared to the control group. No statistically significant difference was observed for knee flexion angle at heel strike, knee adduction moment, or peak knee flexion moment between the groups.
Conclusions
Modern bi-cruciate substituting TKA designs failed to reproduce normal knee kinematics. The lack of full knee extension during the stance phase, absence of the “screw-home mechanism” typical of an ACL functioning knee, and the reduced fluctuation in knee adduction angle during the swing phase still represent major proprioceptive and muscular recruitment differences between normal and replaced knees.
Similar content being viewed by others
Background
Total Knee Arthroplasty (TKA) remains a very successful surgical treatment for knee arthritis. Unfortunately, 20% of post-operative patients still report major limitations in activities of daily living (ADLs) [40] compared to their age-matched non-arthritic peers [42]. Subjective symptoms (e.g. instability, abnormal proprioception) and objective clinical findings [e.g. poor range of motion (ROM), chronic joint effusions, inability to use the stairs, inability to comfortably kneel or squat] are commonly reported elements of patient dissatisfaction.
In an effort to improve patient satisfaction, the design of modern TKA underwent major modifications by many orthopaedic medical device companies over the last 10–15 years. The aim of this “implant personalization” was to update geometry and conformity [22] to restore normal knee kinematics; it followed the theoretical dogma that reproducing normal anatomy would provide a more natural joint proprioception. To make further progress towards this goal, the industry has also introduced digitalized technologies such as robotics, computer navigation, and load−sensing intra−articular sensors. The true impact of these technologies on knee kinematics during ambulation is yet to be proven. Previous studies from the current authors’ Institution supported the evidence that strong differences in knee kinematic behavior exist when tested in the stance phase of gait (joint center of rotation is on the lateral side) [28] compared to the swing phases of gait, stair climbing, and mini−squatting activities (joint center of rotation is on the medial side) [27, 44]. Reproduction of the “dual pivoting” knee kinematics [38] is extremely challenging with arthroplasty because the anterior and posterior cruciate ligaments (ACL, PCL)—which are commonly removed during the procedure—play a major role in normal knee kinematics [2, 10, 20, 31].
The aim of this study was to register knee kinematic parameters during normal gait (knee flexion–extension angle, adduction–abduction angle, internal–external tibial rotation, peak knee flexion moment, first peak knee adduction moment, and peak knee internal rotation moment) in patients who underwent successful bi−cruciate substituting TKA. Pressure sensors were used intra−operatively to obtain the desired articular stability. The acquired kinematic data was compared to match−paired healthy controls. The authors hypothesized that the kinematic parameters of TKA patients differ significantly from healthy controls because the proprioceptive role of the ACL and PCL is not replicated by modern posterior−stabilized TKA designs or by using a computer−assisted intraoperative strategy.
Materials and methods
This was a retrospective case–control study. Patients who underwent primary TKA because of severe unilateral knee osteoarthritis at two authors’ Institutions (PFI, MG) were included in this study. Inclusion criteria consisted of age greater than 40 years with clinically and radiographically diagnosed unilateral tricompartmental osteoarthritis. Preoperative exclusion criteria included pre-existing concurrent hip, ankle, and/or contralateral knee osteoarthritis, presence of a chronic inflammatory disease, body mass index (BMI) greater than 35 kg/m2, and/or prior joint replacement surgery. The treatment group was composed of ten patients who underwent a bi-cruciate substituting TKA; five patients had a Persona posterior-stabilized (PS) implant (Persona, Zimmer-Biomet, USA) and five patients had a Legion posterior-stabilized (PS) TKA design (Smith & Nephew, London, UK).
The authors decided to use a second-generation PS design (Legion, Smith & Nephew, London, UK) and a third-generation (Persona, Zimmer-Biomet, USA) in order to highlight any difference in the gait data as well as in the clinical outcome. Intraoperative joint balancing was obtained using the load pressure system VERASENSE™ (Orthosensor Inc., Dania Beach, FL, USA).
The load sensor utilized in this study consists of a digital trial insert that can detect intra-operative tibio-femoral loads during component trialing. This technology can quantify the intercompartmental pressure and is able to report data on a screen, delivering a real-time feedback to the surgical team. In addition, the wireless sensor can define the tibio-femoral contact points during passive range of motion testing, including measuring the femoral roll-back during high flexion. Intraoperative load measurements were systematically taken at 10°, 45°, and 90° of knee flexion [33]. The current authors considered the knee well-balanced when the medial compartment pressure was 50 ± 20 pounds, the lateral compartment pressure was 35 ± 20 pounds, and the intercompartmental difference was within 15 pounds. An identical surgical technique was used in all ten cases: this was a combination of gap-balancing in extension and measured resection in flexion with uniform removal of both the ACL and PCL. All patients followed an identical postoperative rehabilitation protocol that included weight-bearing as tolerated with crutch-assist on the first postoperative day.
All patients were followed clinically at the same time intervals: 3-months, 6-months, and 9-months postoperatively: this final timeframe was selected since it has been reported that the kinematic of the knee following TKA has plateaued at nine months from the surgery [27].
At 9 months of minimum follow-up (FU), the treatment group was matched by gender, age, BMI and operating surgeon, to 10 healthy controls. The major postoperative inclusion criteria in the TKA group was the demonstration of a high Knee Injury and Osteoarthritis Outcome Score (KOOS) at final FU [34].
Patients in both groups were matched by age (TKAs: 67.8 ± 6.8 years; Control Group 59.4 ± 7.9 years), sex (all males) and BMI (TKAs: 32.8 ± 5.9 kg/m2; Control group: 30.3 ± 4.6 kg/m2) (Table 1). All patients had to demonstrate full knee extension and at least 125° of active flexion prior to the gait analysis test.
Gait analysis
At a minimum of 9 months from TKA, 3-D knee kinematic analysis was performed using a multi-camera optoelectronic system (Qualisys AB, Gothenburg, Sweden) and a force platform (Bertec Corporation, Columbus, OH) embedded in the middle of a 10-m walkway. This technology was used to analyze and compare the gait of bi-cruciate substituting TKA patients and healthy controls. Video recording and force data were synchronized and collected at 120 Hz. Gait data was collected using a Point Cluster Technique (PCT) with markers placed at reproducible anatomic landmarks on the lower limbs: nine markers were placed on the thigh and six markers on the leg to track relative motion of the lower extremity. Static trial data was collected to obtain the appropriate reference frames and inverse dynamics were used to evaluate the kinematics of the knee (angles and moments) as previously described by the current authors [1]. The BioMove software (Stanford University, Stanford, CA) was used to monitor and measure normalized knee joint moments during the stance and swing phases of gait [13]. All subjects (healthy controls and post-TKA patients) performed three walking trials at their self-selected normal pace. Kinematic data including knee flexion angle at heel strike (KFH), peak midstance knee flexion angle (MSKFA), maximum and minimum knee adduction angle (KAA), and knee rotational angle at heel-strike was extracted by the bioengineers. Peak joint moments included the first peak knee adduction moment (KAM), peak knee flexion moment (KFM), and the peak internal knee rotational moment (KIRM). Particular attention was paid to the evaluation of the external moments, using a standard inverse dynamics approach that was normalized to percent bodyweight and height (%BW%Ht) to facilitate the final comparison between participants in different groups. Final data was averaged for the different walking trials. Clinical outcomes scores (KOOS) were collected prior to the gait test to ensure that gait data were acquired in a patient population which reported a satisfactory clinical outcome. Differences between the treatment group as a whole and the control group were also assessed using student’s t-tests: significance was set at P < 0.05, with trends P < 0.15. A post-hoc power analysis was performed since the number of patients included in the study was limited: the study incidence was set at 20% in the TKA group and at 80% in the control group.
Results
Patient demographics are presented in Table 1. There were no significant differences in BMI, sex, age, or clinical outcome score between TKA patients and healthy controls. The study population was divided into two groups: bi-cruciate substituting PS TKA and Healthy Controls.
Knee flexion angle at heel-strike (KFH)
No statistically significant difference in KFH was observed between the two groups. The average KFH was 5° in the TKA group and 4.5° in the control group. This finding was not surprising because studies from the current authors’ Institution previously demonstrated that, with aging, the tibia undergoes a more forward inclination, and the femur has less forward inclination accordingly [13, 15]. The evaluation of this parameter showed that an increased knee flexion at heel-strike might reflect a reduced capacity to extend the knee dynamically (Fig. 1).
Analysis of knee flexion during Gait Cycle. A Heel-strike: both groups (PS TKA and healthy controls) showed a slight flexion contracture at heel-strike. The difference between the two groups was not statistically significant. B Mid-stance flexion angle. There was a trend that the average mid-stance knee flexion angle in the bi-cruciate substituting PS TKA group (16.1°) was lower than the healthy controls group (20.7°) (P = 0.07)
Mid-stance knee flexion angle
The average mid-stance knee flexion angle in the bi-cruciate substituting PS TKA group (16.1°) trended lower than the control group (20.7°) but did not reach statistical significance (P = 0.07) (Table 1, Fig. 1). Interestingly, the degree of mid-stance knee flexion angle correlated with pain, as reported in the KOOS score (pain section), in both groups—patients with higher mid-stance knee flexion angles reported less pain and better functional outcomes (P = 0.02).
Tibial rotation at heel-strike
The bi-cruciate substituting PS TKA group showed significantly less rotation at heel strike (5.8°) compared to healthy controls (11.2°) (P = 0.04). This strong difference has been related to the fact that both cruciate ligaments have been removed during the surgical procedure.
Knee adduction angle (KAA) and Knee Adduction Moment (KAM)
Significantly less fluctuation in knee adduction angle was seen during swing phase in the bi-cruciate substituting PS TKA group compared to the controls; the TKA group showed less peak knee adduction angle excursion (0.2°) (peak-to-peak) compared to healthy controls (-5.1°) (Fig. 2). Interestingly, the KAA excursion during swing trended higher in the healthy control group but did not reach statistical significance (P = 0.07).
Analysis of the Knee Adduction Moment (KAM), defined by the authors as percent bodyweight and height (%BW%Ht), did not reach statistical significance between the two groups.
Peak Knee Flexion Moment (KFM) and Peak Knee Rotational Moment (KIRM)
The analysis of the Peak KFM did not demonstrate a statistically significant difference between the two groups (Fig. 3). Still, the bi-cruciate substituting PS TKA group showed smaller late stance peak extension moments compared to healthy controls (P = 0.02) (Fig. 3). No statistically significant differences were observed between the two groups in Peak KIRM. Interestingly, a statistically significant difference in the rotational moment was seen between the groups at heel strike: the bi-cruciate substituting PS TKA group had a significant loss of external rotation, a finding that is commonly associated with ACL-deficient knees (Fig. 4).
Analysis of the external tibial rotation during the stance phase of gait. The bi-cruciate substituting PS TKA group showed a significant loss of external rotation at heel strike, both in the prosthetic knee as well as in the contralateral knee. This paradox motion is typical of anterior cruciate ligament (ACL) deficient knees
The post-hoc power analysis of the study revealed a post-hoc power of 81.7%.
Discussion
The current study confirms that modern, third-generation, bi-cruciate substituting TKA failed to reproduce normal knee kinematics. Another major finding of this study was that the intraoperative use of a real-time sensor technology system, which has supported the surgeon in his/her intra-operative decisions, did not have a major impact on the final knee kinematic.
Despite the multiple different total knee arthroplasty designs that have been recently developed and recommended for the theoretical advantage of restoring normal knee kinematics and meeting the demands of active patients, as few as 7% of patients report that their knee feels “normal” after TKA [24, 32, 35]. While the exact cause/causes of this dissatisfaction has/have yet to be elucidated, it has been hypothesized that to improve patient satisfaction, the kinematic patterns of the implanted knee should be similar to those of a healthy knee [39]. Multiple studies have suggested that the evolution of component designs and introduction of new technologies does not always translate into restoration of native knee kinematics [12, 43].
Multiple authors have shown that the motion of the normal knee joint depends on the interaction between the shape of the articular surfaces and the ligaments crossing the knee joint [3, 39]. In the normal knee, the femoral condyles undergo a combination of rolling, sliding, and rotation on the tibial plateau during flexion. With increasing flexion, the posterior translation of the tibiofemoral contact point is greater on the lateral plateau compared to the medial plateau. This is due to the larger radius of curvature of the lateral femoral condyle. This well-established asymmetry in condylar motion during knee flexion imposes passive internal rotation of the tibia with flexion. The opposite rotational motion (“screw home” rotation) occurs when the tibia passively externally rotates during knee extension as the medial femoral condyle articular surface is wider than the lateral one [3].
Posterior stabilized knee designs have been thought to better reproduce femoral rollback and posterior translation of the femur; this is due to the engagement of the cam–post mechanism at 60° of flexion, preventing anterior femoral translation—well known as “paradoxical motion” [35]. The antero-posterior (AP) stability, normally guaranteed by the presence of an intact PCL, has been also reproduced by the use of ultra-congruent (UC) polyethylene inserts, characterized by the high conformity between the tibial and femoral articulating surfaces [4, 25].
In the current study, no statistically significant differences were found between the two groups in peak KFM during level walking. Interestingly, patients with designs that remove or substitute for the PCL tend to reduce their knee flexion moment and thus the resulting demand on the quadriceps. In PCL substituting TKAs, the lack of femoral rollback reduces the lever of the quadriceps and thus its mechanical efficiency. This reduction usually manifests at about 60° of knee flexion, the angle at which the greatest demands are placed on the quadriceps during stairclimbing. Consequently, the mechanism that patients use for the adaptation is a forward lean of the torso [3,4,5].
In this study we also observed a significant loss of external rotation at heel strike and a trend toward a lower average mid-stance knee flexion angle in the PS group compared to the healthy controls. The current authors strongly believe this finding could be related to the absence of the ACL, which contributes to the external orientation of the tibia at full extension (“screw-home” mechanism in the normal knee). The role of the ACL is also to limit the anterior displacement of the tibia with respect to the femur in early to mid-flexion [39]. It has been established that ACL deficiency can cause the avoidance of quadriceps contraction during activities when the knee is near full extension. It appears that patients adapt to the absence of the ACL by minimizing the demand for quadriceps activation as the anterior pull of the patellar ligament is no longer stabilized by the ACL. Andriacchi et al. confirmed that patients with an ACL-deficient knee had a significantly lower than normal net quadriceps moment during the mid-portion of the stance phase of walking ("quadriceps avoidance" gait). In the normal knee, the quadriceps muscles control knee flexion to approximately 20° during midstance; the patients who underwent TKA in the current study did not flex the knee in the same manner [4, 6, 11]. In ACL deficient knees, quadriceps muscle strength deficit contributes to reduction of the knee angles and moments as a natural reaction to knee instability [19, 29]. These historical findings matched our results, which demonstrated a trend toward a lower mid-stance knee flexion angle in the PS TKA group (16.1°) as compared to the healthy control group (20.7°). Moreover, in our series, lower mid-stance knee flexion angle correlated with worse KOOS pain scores.
The recent use of polyethylene designs alternative to the classic PS designs, especially medially constrained, has recently increased with the hope of reproducing normal knee kinematics and to mimic the physiologic medial pivoting pattern with posterolateral femoral roll-back in flexion [14], This “kinematic advantage” was hoped to translate into improved knee proprioception by the patient. Despite successful clinical outcomes, greater patient satisfaction, and higher forgotten joint scores (FJSs) when compared to traditional PS designs, the kinematic patterns of these designs failed to be similar to those of normal knees [16, 18, 23, 37, 41].
In the current, the use of sensor-embedded tibial inserts did not reproduce a kinematic pattern similar to the normal knee during standard gait analysis: the authors’ interpretation of this finding was that the retention of the cruciate ligaments along with a reproduction of the articular geometry, could produce a more normal knee kinematics, greater stability, and decrease muscle forces leading to improved knee function. In a previous study, Meneghini et al. [30] reported higher satisfaction and better Knee Society Function scores when early flexion lateral pivot and late flexion medial pivot kinematic patterns were detected intraoperatively by sensor-embedded tibial inserts [30]: in our study, unfortunately, a correlation between the acquired kinematic data and the clinical results could not be done due to the small cohort analyzed, representing a major limitation of this study.
Bicruciate-retaining (BCR) TKA designs have been developed in the past to reproduce knee biomechanics through ACL preservation: the current literature on the use of BCR TKA designs is extremely controversial: a strong debate is still ongoing between supporters [21, 26, 36, 45] and opponents [7, 8, 19, 36, 39].
Few authors [9, 17] have recently reported excellent outcomes and near- normal gait characteristics when patients who received Bi-unicondylar arthroplasties (Bi-UKA) were matched with TKA subjects: the current authors agree that this technique could represent an interesting surgical strategy in modern total knee arthroplasty.
The main limitation of this study is the small cohort of patients which precludes from making a correlation between the kinematical analysis and the clinical results; however, considering that existing kinematic studies traditionally have relatively small numbers, the authors believe this work could provide useful information for future studies on kinematics following knee replacement. The post-hoc power of the study was 81.7%.
The authors also recognized that, in the gait analysis section of this study, more activities should be analyzed in addition to walking on level-ground: this will eventually help to get a better understanding of the actual knee kinematics.
Conclusion
Modern, bi-cruciate substituting TKA designs failed to reproduce normal knee kinematics despite the intra-operative use of sensor-embedded tibial inserts. The loss of rotation during heel strike, the lack of the “screw-home mechanism,” and the lower mid-stance knee flexion angle all represent major proprioceptive and biomechanical differences between normal and replaced knees. Implants that preserve both cruciate ligaments and allow the reproduction of normal articular geometry in association with robotic-assisted personalized alignment should be studied to detect how far we are from reproducing a closer-to-normal knee kinematics.
Availability of data and materials
Data are available upon request to the corresponding author.
Abbreviations
- TKA:
-
Total knee arthroplasty
- MC:
-
Medially-congruent
- PS:
-
Posterior-stabilized
- KFH:
-
Knee flexion angle at heel-strike
- MSKFA:
-
Peak midstance knee flexion angle
- KAA:
-
Knee adduction angle
- KAM:
-
Knee adduction moment
- KFK:
-
Peak knee flexion moment
- KRM:
-
Knee rotational moment
References
Andriacchi TP, Alexander EJ, Toney MK, Dyrby C, Sum J (1998) A point cluster method for in vivo motion analysis: applied to a study of knee kinematics. J Biomech Eng 120:743–749
Andriacchi TP, Dyrby CO (2005) Interactions between kinematics and loading during walking for the normal and ACL deficient knee. J Biomech 38:293–298
Andriacchi TP, Stanwyck TS, Galante JO (1986) Knee biomechanics and total knee replacement. J Arthroplasty 1:211–219
Andriacchi TP (1993) Functional analysis of pre and post-knee surgery: total knee arthroplasty and ACL reconstruction. J Biomech Eng 115:575–581
Andriacchi TP, Galante JO (1988) Retention of the posterior cruciate in total knee arthroplasty. J Arthroplasty 3(Suppl):S13-19
Andriacchi TP (1990) Dynamics of pathological motion: applied to the anterior cruciate deficient knee. J Biomech 23 Suppl 1:99–105
Arauz P, Klemt C, Limmahakhun S, An S, Kwon YM (2019) Stair climbing and high knee flexion activities in bi-cruciate retaining total knee arthroplasty. In vivo kinematics and articular contact analysis. J Arthroplasty 34:570–576
Arauz P, Peng Y, Kwon YM (2018) Knee motion symmetry was not restored in patients with unilateral bi-cruciate retaining total knee arthroplasty-in vivo three-dimensional kinematic analysis. Int Orthop 42:2817–2823
Banger MS, Johnston WD, Razii N, Doonan J, Rowe PJ, Jones BG, MacLean AD, Blyth MJG (2020) Robotic arm-assisted bi-unicompartmental knee arthroplasty maintains natural knee joint anatomy compared with total knee arthroplasty: a prospective randomized controlled trial. Bone Joint J 102-B:1511–1518
Berchuck M, Andriacchi TP, Bach BR, Reider B (1990) Gait adaptations by patients who have a deficient anterior cruciate ligament. J Bone Joint Surg Am 72:871–877
Branch TP, Hunter R, Donath M (1989) Dynamic EMG analysis of anterior cruciate deficient legs with and without bracing during cutting. Am J Sports Med 17:35–41
Cates HE, Komistek RD, Mahfouz MR, Schmidt MA, Anderle M (2008) In vivo comparison of knee kinematics for subjects having either a posterior stabilized or cruciate retaining high-flexion total knee arthroplasty. J Arthroplasty 23:1057–1067
Chehab EF, Andriacchi TP, Favre J (2017) Speed, age, sex, and body mass index provide a rigorous basis for comparing the kinematic and kinetic profiles of the lower extremity during walking. J Biomech 58:11–20
Cochetti A, Ghirardelli S, Iannotti F, Giardini P, Risitano S, Indelli PF (2020) Sensor-guided technology helps to reproduce medial pivot kinematics in total knee arthroplasty. J Orthop Surg (Hong Kong) 28:2309499020966133. https://doi.org/10.1177/2309499020966133
Favre J, Erhart-Hledik JC, Andriacchi TP (2014) Age-related differences in sagittal-plane knee function at heel-strike of walking are increased in osteoarthritic patients. Osteoarthritis Cartilage 22:464–471
Frye BM, Patton C, Kinney JA, Murphy TR, Klein AE, Dietz MJ (2021) A medial congruent polyethylene offers satisfactory early outcomes and patient [2021]satisfaction in total knee arthroplasty. Arthroplast Today 7:243–249
Garner AJ, Dandridge OW, Amis AA, Cobb JP, van Arkel RJ (2021) Bi-unicondylar arthroplasty : a biomechanics and clinical outcomes study. Bone Joint Res 10:723–733
Ghirardelli S, Asay JL, Leonardi EA, Amoroso T, Andriacchi TP, Indelli PF (2021) Kinematic comparison between medially congruent and posterior-stabilized third-generation TKA designs. J Funct Morphol Kinesiol 6(1):27
Hamada D, Wada K, Takasago T, Goto T, Nitta A, Higashino K, Fukui Y, Sairyo K (2018) Native rotational knee kinematics are lost in bicruciate-retaining total knee arthroplasty when the tibial component is replaced. Knee Surg Sports Traumatol Arthrosc 26:3249–3256
Harman MK, Bonin SJ, Leslie CJ, Banks SA, Hodge WA (2014) Total knee arthroplasty designed to accommodate the presence or absence of the posterior cruciate ligament. Adv Orthop 2014:178156
Heyse TJ, Slane J, Peersman G, Dirckx M, van de Vyver A, Dworschak P, Fuchs-Winkelmann S, Scheys L (2017) Kinematics of a bicruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:1784–1791
Indelli PF, Risitano S, Hall KE, Leonardi E, Migliore E (2019) Effect of polyethylene conformity on total knee arthroplasty early clinical outcomes. Knee Surg Sports Traumatol Arthrosc 27:1028–1034
Indelli PF, Morello F, Ghirardelli S, Fidanza A, Iannotti F, Ferrini A (2020) No clinical differences at the 2-year follow-up between single radius and j-curve medial pivot total knee arthroplasty in the treatment of neutral or varus knees. Knee Surg Sports Traumatol Arthrosc 28:3949–3954
Johnson AJ, Howell SM, Costa CR, Mont MA (2013) The ACL in the arthritic knee: how often is it present and can preoperative tests predict its presence? Clin Orthop Relat Res 471:181–188
Kim TW, Lee SM, Seong SC, Lee S, Jang J, Lee MC (2016) Different intraoperative kinematics with comparable clinical outcomes of ultracongruent and posterior stabilized mobile-bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24:3036–3043
Koh YG, Son J, Kwon SK, Kim HJ, Kwon OR, Kang KT (2017) Preservation of kinematics with posterior cruciate-, bicruciate- and patient-specific bicruciate-retaining prostheses in total knee arthroplasty by using computational simulation with normal knee model. Bone Joint Res 6:557–565
Koo S, Andriacchi TP (2008) The knee joint center of rotation is predominantly on the lateral side during normal walking. J Biomech 41:1269–1273
Kozanek M, Hosseini A, Liu F, Van de Velde SK, Gill TJ, Rubash HE, Li G (2009) Tibiofemoral kinematics and condylar motion during the stance phase of gait. J Biomech 42:1877–1884
Lewek M, Rudolph K, Axe M, Snyder-Mackler L (2002) The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon) 17:56–63
Meneghini RM, Deckard ER, Ishmael MK, Ziemba-Davis MA (2017) Dual-pivot pattern simulating native knee kinematics optimizes functional outcomes after total knee arthroplasty. J Arthroplasty 32:3009–3015
Mikashima Y, Tomatsu T, Horikoshi M, Nakatani T, Saito S, Momohara S, Banks SA (2010) In vivo deep-flexion kinematics in patients with posterior-cruciate retaining and anterior-cruciate substituting total knee arthroplasty. Clin Biomech (Bristol, Avon) 25:83–87
Noble PC, Gordon MJ, Weiss JM, Reddix RN, Conditt MA, Mathis KB (2005) Does total knee replacement restore normal knee function? Clin Orthop Relat Res 431:157–165
Risitano S, Karamian B, Indelli PF (2017) Intraoperative load-sensing drives the level of constraint in primary total knee arthroplasty: surgical technique and review of the literature. J Clin Orthop Trauma 8:265–269
Roos EM, Toksvig-Larsen S (2003) Knee injury and Osteoarthritis Outcome Score (KOOS) - validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes 25:1–17
Roberti di Sarsina T, Alesi D, Di Paolo S, Zinno R, Pizza N, MarcheggianiMuccioli GM, Zaffagnini S, Bragonzoni L (2022) In vivo kinematic comparison between an ultra-congruent and a posterior-stabilized total knee arthroplasty design by RSA. Knee Surg Sports Traumatol Arthrosc 30(8):2753–2758
Sabatini L, Barberis L, Camazzola D, Centola M, Capella M, Bistolfi A, Schiraldi M, Massè A (2021) Bicruciate-retaining total knee arthroplasty: what’s new? World J Orthop 12:732–742
Sabatini L, Risitano S, Parisi G, Tosto F, Indelli PF, Atzori F, Massè A (2018) Medial pivot in total knee arthroplasty: literature review and our first experience. Clin Med Insights Arthritis Musculoskelet Disord 11:1179544117751431
Sandberg R, Deckard ER, Ziemba-Davis M, Banks SA, Meneghini RM (2019) Dual-pivot bearings improve ambulation and promote increased activity levels in total knee arthroplasty: a match-controlled retrospective study. Knee 26:1243–1249
Smith LA, Nachtrab J, LaCour M, Cates H, Freeman MG, Komistek RD (2021) In vivo knee kinematics: how important are the roles of femoral geometry and the cruciate ligaments? J Arthroplasty 36:1445–1454
Tolk J, van der Steen M, Janssen R, Reijman M (2017) Total knee arthroplasty: what to expect? a survey of the members of the dutch knee society on long-term recovery after total knee arthroplasty. J Knee Surg 30:612–616
Tso R, Smith J, Doma K, Grant A, McEwen P (2021) Clinical and patient-reported outcomes of medial stabilized versus non-medial stabilized prostheses in total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty 36:767–776
Varadarajan KMM, Zumbrunn T, Rubash HE, Malchau H, Li G, Muratoglu OK (2015) Cruciate retaining implant with biomimetic articular surface to reproduce activity dependent kinematics of the normal knee. J Arthroplasty 30:2149–2153
Walker PS, Sussman-Fort JM, Yildirim G, Boyer J (2009) Design features of total knees for achieving normal knee motion characteristics. J Arthroplasty 24:475–483
Yamaguchi S, Gamada K, Sasho T, Kato H, Sonoda M, Banks SA (2009) In vivo kinematics of anterior cruciate ligament deficient knees during pivot and squat activities. Clin Biomech 24:71–76
Zhou C, Peng Y, An S, Bedair H, Li G (2021) Does Contemporary bicruciate retaining total knee arthroplasty restore the native knee kinematics? A descriptive literature review. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-04116-3
Funding
This study was partially funded by Zimmer-Biomet (Warsaw, Indiana, USA).
Author information
Authors and Affiliations
Contributions
FI, PFI, MG Study design, manuscript editing, interpretation of findings, manuscript writing. SG Study design, manuscript writing, literature review. MG, PFI, FI Data collection, statistical analysis, interpretation of findings, figures and manuscript editing. FI Literature review and manuscript writing. KZ, RV Manuscript editing, interpretation of findings. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
IRB approval was obtained (Stanford University IRB 4947).
All patients provided informed consent for the participation in the study and the use of their data and images for research purposes.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Indelli, P.F., Giuntoli, M., Zepeda, K. et al. Native knee kinematics is not reproduced after sensor guided cruciates substituting total knee arthroplasty. J EXP ORTOP 10, 17 (2023). https://doi.org/10.1186/s40634-023-00567-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-023-00567-2