Abstract
Background
Revision anterior cruciate ligament (ACL) reconstruction requires a precise evaluation of previous tunnel locations and diameters. Enlargement of the tunnels, despite not usually affecting primary reconstruction outcomes, plays an important role in revision ACL management. Three dimensional (3D) computed tomography (CT) models are reported to be the most accurate method for identifying the tunnel position and possible conflicts with a revision tunnel placement. However, the ability of 3D CT to measure the tunnel size is still not proven. The goal of this study was to evaluate the ability of measuring the size of the bone tunnels in ACL reconstructed knees with 3D CT compared to the traditional two dimensional (2D) CT method.
Methods
Twenty-four patients had CT scans performed immediately following ACL reconstruction surgery. Their femoral tunnels size were measured by a standard 2D CT measurement and then compared with three novel 3D CT measuring methods: the best transverse section method, the best fit cylinder method and the wall thickness method. The drill size used during surgery was used as a control measure for the tunnel width. Intra-class correlation coefficients were obtained.
Results
The intra-class correlation coefficient and respective 95% confidence interval range (ICC [95%CI]) for the three methods compared with the drill sizes were 0.899 [0.811-0.947] for the best transverse section method, 0.745 [0.553-0.862] for the best fit cylinder method, −0.004 [−0.081 to −0.12] for the wall thickness method and 0.922 [0.713-0.97] for the 2D CT method. The mean differences compared to the drill size were 0.02 mm for the best fit transverse section method, 0.01 mm for the best fit cylinder diameter method, 3.34 mm for the wall thickness method and 0.29 mm for the 2D CT method. The intra-rater agreement (ICC [95%CI]) was excellent for the best transverse section method 0.999 [0.998-0.999] and the 2D CT method 0.969 [0.941-0.984].
Conclusions
The 3D best transverse section method presented a high correlation to the drill sizes and high intra-rater agreement, and was the best method for ACL tunnel evaluation in a 3D CT based model.
Similar content being viewed by others
Background
Tunnel enlargement after an anterior cruciate ligament (ACL) reconstruction is a well-known phenomenon, noticed first in the early 1990’s following allograft reconstruction [[1]], but is also seen with different graft techniques and fixation methods [[1]–[3]]. Although no significant correlation between tunnel enlargement and clinical outcomes has currently been reported [[4]–[9]], tunnel widening may have serious implications for patients requiring ACL revision surgery. Revision ACL rates range from 10-25% [[10]], and a reliable assessment of the tunnel width and position is crucial to surgical planning [[11]].
Different methods for measuring tunnel width have been described in the literature using two dimensional (2D) radiography, computed tomography (CT) and magnetic resonance imaging (MRI) [[12]–[16]]. The 2D CT has been reported to be the best method for identifying the tunnels, especially immediately after surgery [[12],[17]]. Other advantages of CT scans are that they eliminate the scaling issues present in plain radiographs and that they appear to be less affected by geometric factors that may influence the tunnel measurements due to knee positioning during image acquisition. Although providing the most accurate measurements, CT scans also have limitations. Interobserver and intraobserver reliability have been reported to be inconsistent [[12],[17]].
Three dimensional (3D) computed tomography models have been developed to create an accurate 3D model of the bones using imaging software. These models have been largely used to investigate tunnel position following cruciate ligament reconstruction and reportedly have increased intraobserver reliability [[18]–[20]]. Additionally, 3D CT models were reported to be the most reliable imaging method of showing conflict between pre-existing and desired femoral tunnel locations prior to ACL revision surgery [[21]]. However, to the authors’ knowledge, 3D CT methods for evaluating tunnel width have not been studied to date.
The purpose of this study was to evaluate the accuracy of three novel methods for measuring tunnel width based on the 3D CT bone model of ACL reconstructed knees. The novel methods were compared to the current clinical method of measuring tunnel width using 2D CT images. We hypothesized that the novel CT bone model methods would be more accurate for measuring tunnel width than the current standard methods.
Methods
Sample selection
Prior to initiation, the study protocol was approved by the Institutional Review Board of the (Regional Committee for Medical Research Ethics) and a signed informed consent for release of scans was received from all participants. The patients’ selection criteria were: age between 18 and 40 years, 3 months of rehabilitation prior to the surgical procedure and a complete ACL tear verified by history, physical examination and confirmed by an arthroscopic procedure. Patients were excluded from the study if they presented with ACL revision reconstruction, ACL lesion of the contralateral knee, concomitant PCL, lateral or medial instability at the time of the surgery, established osteoarthritis with Kellgren-Lawrence classification grades 3 or 4 or hamstring grafts unable to have a minimum diameter of 5 mm for each bundle. The 24 patients enrolled into the study were randomized to single-bundle (SB) or double-bundle (DB) ACL reconstruction, with 12 patients in each group.
Imaging protocol and 3D modeling
The CT scanner used was a Philips Brilliance 16-slice scanner, and the imaging specifications used for all patients included 1.5 mm slice thickness, 0.75 mm slice increment, 120 kV, 250 mAs, 500 mm field of view, 512 × 512 resolution. All patients had CT scans performed during the initial two days following surgery with their knee positioned in full extension. The high resolution images were evaluated by an independent investigator who was not involved in the surgical procedure or patient care.
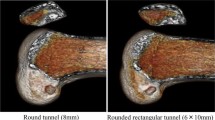
The CT images were exported to an image analysis software (Mimics v1.6, Materialise, Leuven, Belgium) and a manual segmentation of the bone structures, bone tunnels and cortical buttons was performed. The segmentation process relies on using bone-soft tissue density variation on CT images, adjusting a density range to highlight bone anatomy on CT scan images. Manual revision of the CT images was performed to correct errors, and assure that the outline of the bone and tunnels were appropriately filled. This allowed for the creation of a patient-specific 3D bone model of the knee joint, with the tunnels appearing as empty spaces (Figures 1 and 2). This process has previously been validated, and has demonstrated high intraobserver and interobserver reliability and accuracy [[22],[23]].
Measurement methods
Using the 3D model of each patient’s knee, three different techniques for measuring tunnel width were evaluated: best fit cylinder, overall wall thickness and transverse section diameter. The best fit cylinder method consisted of creating an analytical best fit cylinder to the entire tunnel length (Figure 3). The wall thickness method consisted of an internal software function (Mimics, Materialise, Leuven, Belgium) that measured the perpendicular distance from each triangle that formed the 3D model to the opposite side of the model (Figure 4). The best fit transverse section method was performed by fitting a center axis to the entire tunnel length and then fitting a circle to the tunnel walls at its mid-length (Figure 5).
Best transverse section method. The segmented tunnel (A) was used as a guide for the automated centerline drawing made by the Mimics® software. Centerline half-way distances were measured and the best fit diameter on this points was evaluated (B). Image of the tunnel model with the measurements on its surface (C).
The traditional method for measuring tunnel width in a 2D CT scan was also evaluated. The tunnel diameter was measured at the tunnel mid-point in all three image planes (axial, sagittal, and coronal) using a straight line drawing tool (Figure 6). The mean value of the measurements from the three image planes was used for comparison.
The 2D CT measurements and the best fit transverse section method measurements were repeated after one month to determine the intra-observer reliability of the method. The best fit cylinder and wall thickness methods were entirely automated by the software, having a complete agreement between the two consecutive measurements. An orthopedic surgeon (B.C.) trained by a musculoskeletal radiologist performed all measurements.
Surgical technique
All procedures were performed by one surgeon (S.J.). The reconstructions relied on ACL anatomical landmarks, with the SB reconstruction targeting to have the tunnel in a central position of the ACL footprint, and the DB reconstruction aimed to place the tunnels in the center of each ACL bundle, as previously described by Muller et al. [[24]]. The drilling was performed through an accessory anteromedial portal with the knee in hyperflexion for both techniques, following a technique as described by Brown et al. [[25]]. The gracilis and semitendinosus tendons were harvested and doubled or tripled according to their size and length. The tunnel sizes were defined based on the graft diameters in a 0.5 mm increase graft ruler scale (Smith and Nephew, Andover, MA, USA), and the drill size was selected to match the graft diameter. A suspension device was used for femoral fixation (EndoButton - Smith and Nephew, Andover, MA, USA) and an interference screw (Biosure PK - Smith and Nephew, Andover, MA, USA), was used for tibial fixation.
Statistical analysis
Because the tibia interference screw fixation method produced an intra-operative tunnel widening, and the tunnel size could be significantly different from the original drill size, the tibial tunnels were not used for comparison of methods. The measurements of the femoral ACL reconstruction tunnels were obtained by using the different techniques and were compared to the drill size used to prepare the respective tunnel. Mean (±SD) differences between measurement and drill size are reported. Intra- and inter-method agreement were assessed using the two-way random, single measures, absolute agreement form of the intra-class correlation coefficient (ICC). ICC values were classified as excellent (>0.75), fair to good (0.40 - 0.75) or poor (<0.40) [[26]–[28]]. All statistical calculations were performed using IBM SPSS Statistics, Version 20 (Armonk, NY, USA). Histograms of all measurements and differences from drill size were inspected and found to be reasonably normally distributed, prompting the use of parametric statistical tools.
Results
Tunnel size
The drill size range used for the ACL reconstructions in this study was from 5.0 to 9.0 mm and the difference between the average of the drill sizes and the measurements means and respective standard deviation were 0.29 ± 0.4 mm for the 2D CT method, 0.02 ± 0.6 mm for the best fit transverse section method, 0.01 ± 0.8 mm for the best fit cylinder diameter method and 3.34 ± 2.1 mm for the wall thickness method (Figure 7).
The intraclass correlation coefficient and respective 95% confidence interval range (ICC [95%CI]) comparing the measurements to the drill sizes was 0.922 [0.713-0.97] for the 2D CT method, 0.899 [0.811-0.947] for the best fit transverse section method, 0.745 [0.553-0.862] for the best fit cylinder method and −0.004 [−0.081-0.12] for the wall thickness (Table 1).
Evaluating the measurements obtained on the original 2D CT scans, and comparing the measurements on each image plane (coronal, axial and sagittal) with the average of the drill sizes, there was an ICC [95%CI] of 0.922 [0.713-0.97] for the mean and 0.876 [0.711-0.942] for the measurements obtained on the coronal view, 0.907 [0.548-0.968] for the axial view and 0.876 [0.759-0.936] for the sagittal view (Table 2).
Intra-rater ICCs
The intra-rater agreement (ICC [95%CI]) was excellent for the best-fit circle 0.999 [0.998-0.999] and the 2D CT method 0.969 [0.941-0.984]. The best fit cylinder and the wall thickness methods were totally automated, with total agreement (ICC of 1.00) between measurements.
Discussion
The most important finding of our study was that the 3D best fit transverse section method presented excellent accuracy for measuring tunnel width and excellent intraobserver reliability. Of all the 3D model methods, the best fit cylinder method was the closest to the mean drill size. However, it had a higher standard deviation and lower accuracy, evaluated by the ICC, compared to the transverse section method. The wall thickness method produced significant smaller values than the mean drill size. Additionally, the 2D CT measurement method presented a high correlation to the drill sizes used to ream the tunnels and a high intraobserver reliability.
Several studies evaluated enlargement by comparing late post-operative CT images and the drill sizes used during the procedure. Comparing immediate postoperative images to the drill size diameters, we could access the accuracy of CT based methods. As expected, we obtained a high correlation between the drill diameter and the 2D CT measurements, validating the use of the drill size as the immediate postoperative diameter for the ACL femoral tunnels.
Although the 2D CT method for tunnel enlargement evaluation is commonly used, its limitations regarding alignment between CT plane cuts and limb/tunnel orientation have been previously described [[17]]. The ACL reconstruction technique has lately changed to a more anatomic graft placement with more oblique tunnels related to the femoral axis [[29]], and this technique change can theoretically increase the tunnel-CT axis orientation mismatch [[14]] attempted to minimize this factor by reorienting the images to align the tunnel axis, a step that has to be done for every tunnel and can be susceptible to error, especially in the presence of major enlargements, when the tunnel axis is less clear. In this study, the use of the average of all three 2D CT plane measurements improved the 2D method agreement when compared to the measurement in one single image plane (Table 2). However this strategy was time consuming compared to the 3D methods, once the 3D model is available, and hence not commonly used in clinical practice. Additionally, the tunnel enlargement does not seem to be an organized symmetric expansion of the tunnel, and Fink et al. [[9]] described that the tunnel enlargement differed according to the CT views used for the measurement, a 30.6% enlargement of the tibial tunnel, in the sagittal plane, against a 16.4% coronal plane enlargement was reported 2 years after surgery. All these issues can be potentially eliminated by the use of 3D model methods, because they portray the entire shape of the tunnel and thereby address the 3D geometry of the tunnel.
The best fit transverse section method presented an excellent agreement to the drill sizes (0.899 of ICC) and a mean difference of 0.07 mm to the drill sizes, comparable to 2D CT method with a 0.9222 ICC and 0.33 mm mean difference to the drill size. The intra-rater agreement was excellent (0.999 of ICC) because of the semi-automated nature of the measurement that only varied according to the position of the measurement. The ability of using the 3D image avoids the possible bias of the image cut selection and the tunnel-images mismatch present on 2D measurements. This method preserves the 2D CT method ability of evaluating the enlargement in different portions of the tunnel length. The best fit cylinder method presented a good agreement to the drill size (0.745 of ICC), and the closest mean difference to the drill size 0.04 mm. It has the advantage of evaluating the entire tunnel at once and was automated. The wall thickness method presented a poor agreement to the drill size and had a mean difference compared to the drill sizes of 3.38 mm due to variability in orientation of the triangles that composed the 3D model shape, downsizing the overall measurement.
A high intraobserver agreement value was obtained for the 2D CT method in our study. Previous papers reported much lower intraobserver agreement rates when using this method with ICC rates from 0.44 to 0.74 [[5],[17],[30]] This difference may be because our patients were evaluated immediately after surgery, when the tunnel remains cylindrical and has not enlarged. Measurement of an enlarged and misshaped tunnel on the 2D CT method would be more difficult, because it would greatly depend on how the enlargement was positioned within the CT field of view, if it was visible in the image planes and in which image the observer choose to perform the measurement. This could lead to a reduced reliability of the method.
3D CT scan is an important adjuvant in a clinical setting, and it has been validated to be the best method for tunnel placement evaluation and for planning a revision cruciate ligament surgery [[18]–[20]]. Many CT scanners currently have internal capacity of creating a 3D reconstruction of the bones and software to perform 3D measurements. Additionally this study demonstrated that with simple measurement tools an accurate measurement that addresses the 3D architecture of the tunnels was easily obtained.
This study has some limitations related to a small sample size, and the fact that one investigator performed all the measurements and an inter-observer evaluation was therefore not performed. The images were obtained in the immediate post operative and the effects of an asymmetrical enlargement in methods accuracy could not be evaluated. Additionally, the 2D CT measurements were collected in the original scan images, and the tunnels were not always well aligned to the images axis. However, this is the most usual measurement method on clinical practice, and no standardization for tunnel measurement is available in the literature.
Conclusions
The 3D CT based best-fit transverse section measurement method demonstrated excellent accuracy and reliability for the ACL reconstruction tunnel measurement in immediate post-operative patients. This method was found to be the method of choice for tunnel measurement in 3D models. The best fit cylinder method also presented a high correlation to the drill size, and could be very helpful in revision ACL surgery planning by optimizing the new tunnel size to fit the previous tunnel. The wall thickness method presented poor results in evaluating the tunnels in the 3D model, and would not be recommended.
Abbreviations
- ACL:
-
Anterior cruciate ligament:
- 2D:
-
Two dimensional:
- CT:
-
Computed tomography:
- 3D:
-
Three dimensional:
- SB:
-
Single-bundle:
- DB:
-
Double-bundle:
- SD:
-
Standard deviation:
- ICC:
-
Intraclass correlation coefficient:
- CI:
-
Confidence interval:
References
Roberts TS, Drez D Jr, McCarthy W, Paine R: Anterior cruciate ligament reconstruction using freeze-dried, ethylene oxide-sterilized, bone-patellar tendon-bone allografts Two year results in thirty-six patients. Am J Sports Med 1991,19(1):35–41. 10.1177/036354659101900106
Peyrache MD, Djian P, Christel P, Witvoet J: Tibial tunnel enlargement after anterior cruciate ligament reconstruction by autogenous bone-patellar tendon-bone graft. Knee Surg Sports Traumatol Arthrosc 1996,4(1):2–8. 10.1007/BF01565989
Webster KE, Feller JA, Hameister KA: Bone tunnel enlargement following anterior cruciate ligament reconstruction: a randomised comparison of hamstring and patellar tendon grafts with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc 2001,9(2):86–91. 10.1007/s001670100191
Klein JP, Lintner DM, Downs D, Vavrenka K: The incidence and significance of femoral tunnel widening after quadrupled hamstring anterior cruciate ligament reconstruction using femoral cross Pin fixation. Arthroscopy 2003,19(5):470–476. 10.1053/jars.2003.50106
Webster KE, Chiu JJ, Feller JA: Impact of measurement error in the analysis of bone tunnel enlargement after anterior cruciate ligament reconstruction. Am J Sports Med 2005,33(11):1680–1687. 10.1177/0363546505275489
Clatworthy MG, Annear P, Bulow JU, Bartlett RJ: Tunnel widening in anterior cruciate ligament reconstruction: a prospective evaluation of hamstring and patella tendon grafts. Knee Surg Sports Traumatol Arthrosc 1999,7(3):138–145. 10.1007/s001670050138
Dyer CR, Elrod BF: Tibial and femoral bone tunnel enlargement following allograft replacement of the anterior cruciate ligament. Arthroscopy 1995, 11: 353–354.
Fahey M, Indelicato PA: Bone tunnel enlargement after anterior cruciate ligament replacement. Am J Sports Med 1994,22(3):410–414. 10.1177/036354659402200318
Fink C, Zapp M, Benedetto KP, Hackl W, Hoser C, Rieger M: Tibial tunnel enlargement following anterior cruciate ligament reconstruction with patellar tendon autograft. Arthroscopy 2001,17(2):138–143. 10.1053/jars.2001.21509
Höher J, Möller HD, Fu FH: Bone tunnel enlargement after anterior cruciate ligament reconstruction: fact or fiction? Knee Surg Sports Traumatol Arthrosc 1998,6(4):231–240. 10.1007/s001670050105
Hofbauer M, Muller B, Murawski CD, Baraga M, van Eck CF, Fu FH: Strategies for revision surgery after primary double-bundle Anterior Cruciate Ligament (ACL) reconstruction. Knee Surg Sports Traumatol Arthrosc 2013,21(9):2072–2080. 10.1007/s00167-013-2470-7
Webster KE, Feller JA, Elliott J, Hutchison A, Payne R: A comparison of bone tunnel measurements made using computed tomography and digital plain radiography after anterior cruciate ligament reconstruction. Arthroscopy 2004,20(9):946–950. 10.1016/j.arthro.2004.06.037
Kawaguchi Y, Kondo E, Kitamura N, Kai S, Inoue M, Yasuda K: Comparisons of femoral tunnel enlargement in 169 patients between single-bundle and anatomic double-bundle anterior cruciate ligament reconstructions with hamstring tendon grafts. Knee Surg Sports Traumatol Arthrosc 2011,19(8):1249–1257. 10.1007/s00167-011-1455-7
Siebold R, Cafaltzis K: Differentiation between intraoperative and postoperative bone tunnel widening and communication in double-bundle anterior cruciate ligament reconstruction: a prospective study. Arthroscopy 2010,26(8):1066–1073. 10.1016/j.arthro.2009.12.019
Choi NH, Oh JS, Jung SH, Victoroff BN: Tibial tunnel widening after hamstring anterior cruciate ligament reconstructions: comparison between rigidfix and Bio- TransFix. The Knee 2013,20(1):31–35. 10.1016/j.knee.2012.05.009
Vadalà A, Iorio R, De Carli A, Argento G, Di Sanzo V, Conteduca F, Ferretti A: The effect of accelerated, brace free, rehabilitation on bone tunnel enlargement after ACL reconstruction using hamstring tendons: a CT study. Knee Surg Sports Traumatol Arthrosc 2007,15(4):365–371. 10.1007/s00167-006-0219-2
Marchant MH Jr, Willimon SC, Vinson E, Pietrobon R, Garrett WE, Higgins LD: Comparison of plain radiography, computed tomography, and magnetic resonance imaging in the evaluation of bone tunnel widening after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2010,18(8):1059–1064. 10.1007/s00167-009-0952-4
Kopf S, Forsythe B, Wong AK, Tashman S, Irrgang JJ, Fu FH: Transtibial ACL reconstruction technique fails to position drill tunnels anatomically in vivo 3D CT study. Knee Surg Sports Traumatol Arthrosc 2012,20(11):2200–2227. 10.1007/s00167-011-1851-z
Meuffels DE, Potters JW, Koning AH, Brown CH Jr, Verhaar JA, Reijman M: Visualization of postoperative anterior cruciate ligament reconstruction bone tunnels: reliability of standard radiographs, CT scans, and 3D virtual reality images. Acta Orthop 2011,82(6):699–703. 10.3109/17453674.2011.623566
Youm YS, Cho SD, Eo J, Lee KJ, Jung KH, Cha JR: 3D CT analysis of femoral and tibial tunnel positions after modified transtibial single bundle ACL reconstruction with varus and internal rotation of the Tibia. Knee 2012,20(4):272–276. 10.1016/j.knee.2012.10.024
Tscholl PM, Biedert RM, Gal I: Radiological evaluation for conflict of the femoral tunnel entrance area prior to anterior cruciate ligament revision surgery. Int Orthop 2013. ahead of printI
Bryce CD, Pennypacker JL, Kulkarni N, Paul EM, Hollenbeak CS, Mosher TJ, Armstrong AD: Validation of three-dimensional models of in situ scapulae. J Shoulder Elbow Surg 2008,17(5):825–832. 10.1016/j.jse.2008.01.141
Moro-oka TA, Hamai S, Miura H, Shimoto T, Higaki H, Fregly BJ, Iwamoto Y, Banks SA: Can magnetic resonance imaging–derived bone models Be used for accurate motion measurement with single-plane three-dimensional shape registration? J Orthop Res 2007,25(7):867–872. 10.1002/jor.20355
Muller B, Hofbauer M, Wongcharoenwatana J, Fu F: Indications and contraindications for double-bundle ACL reconstruction. International Orthopaedics (SICOT) 2012, 37: 239–246. 10.1007/s00264-012-1683-6
Brown CH Jr, Spalding T, Robb C: Medial portal technique for single-bundle anatomical anterior cruciate ligament reconstruction. International Orthopaedics (SICOT) 2013, 37: 253–269. 10.1007/s00264-012-1772-6
Chicchetti D, Bronen R, Spencer S, Haut S, Berg A, Oliver P, Tyrer P: Rating scales, scales of measurement, issues of reliability. J Nerv Ment Dis 2006,194(8):557–564. 10.1097/01.nmd.0000230392.83607.c5
Shrout PE, Fleiss JL: Intraclass correlations: uses in assessing rater reliab. Psychol Bulletin 1979, 86: 420–428. 10.1037/0033-2909.86.2.420
Landis JR, Koch GC: The measurement of observer agreement for categorical data. Biometrics 1977, 33: 159–174. 10.2307/2529310
Illingworth KD, Hensler D, Working ZM, Macalena JA, Tashman S, Fu FH: A simple evaluation of anterior cruciate ligament femoral tunnel position: the inclination angle and femoral tunnel angle. Am J Sports Med 2011,39(12):2611–2618. 10.1177/0363546511420128
Järvelä T: Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomize clinical study. Knee Surg Sports Traumatol Arthrosc 2007,15(5):500–507. 10.1007/s00167-006-0254-z
Acknowledgements
We thank Grant Dornan, MSc, for his contribution of statistical expertise to the analysis of this study. We also thank Steinar Johansen (S.J.), M.D. for performing the surgical procedure and allowing the evaluation of his patients. The orthopedic department of the Oslo University Hospital is gratefully acknowledged for providing the imaging resources. The project was supported by Oslo Sports Trauma Research Center and Steadman Philippon Research Institute.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
One or more authors receive scientific support from Smith and Nephew, which provided donation of surgical supplies for this study.
Authors’ contributions
BC, CA, KJW, SP, RFL, LE and CAW have made significant contributions to the conception, design, and were involved in acquisition, analysis and interpretation of the data. BC, CA, KJW, SP, RFL, LE and CAW have worked on drafting the manuscript and approved the final version of the manuscript to be published.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Crespo, B., Aga, C., Wilson, K.J. et al. Measurements of bone tunnel size in anterior cruciate ligament reconstruction: 2D versus 3D computed tomography model. J EXP ORTOP 1, 2 (2014). https://doi.org/10.1186/s40634-014-0002-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-014-0002-0