Abstract
Background
In out-of-hospital cardiac arrest (OHCA) patients with extracorporeal cardiopulmonary resuscitation (ECPR), the association between low-flow time and outcomes in accidental hypothermia (AH) patients compared to those of patients without AH has not been fully investigated.
Methods
This was a secondary analysis of the retrospective multicenter registry in Japan. We enrolled patients aged ≥ 18 years who had been admitted to the emergency department for OHCA and had undergone ECPR between January, 2013 and December, 2018. AH was defined as an arrival body temperature below 32 °C. The primary outcome was survival to discharge. Cubic spline analyses were performed to assess the non-linear associations between low-flow time and outcomes stratified by the presence of AH. We also analyzed the interaction between low-flow time and the presence of AH.
Results
Of 1252 eligible patients, 105 (8.4%) and 1147 (91.6%) were in the AH and non-AH groups, respectively. Median low-flow time was 60 (47–79) min in the AH group and 51 (42–62) min in the non-AH group. The survival discharge rates in the AH and non-AH groups were 44.8% and 25.4%, respectively. The cubic spline analyses showed that survival discharge rate remained constant regardless of low-flow time in the AH group. Conversely, a decreasing trend was identified in the survival discharge rate with longer low-flow time in the non-AH group. The interaction analysis revealed a significant interaction between low-flow time and AH in survival discharge rate (p for interaction = 0.048).
Conclusions
OHCA patients with arrival body temperature < 32 °C who had received ECPR had relatively good survival outcomes regardless of low-flow time, in contrast to those of patients without AH.
Similar content being viewed by others
Background
Accidental hypothermia (AH) is an involuntary drop in core body temperature to < 35 °C. At a core body temperature below 32 °C, there is a risk of cardiac arrest, and the risk becomes significantly elevated below 28 °C [1]. Previous nationwide and international studies of AH have reported mortality rates of 12.0–26.9% [2,3,4]. The incidence and mortality rates of AH are higher in geriatric patients, and the number of AH patients is predicted to rise in coming decades [5]. Therefore, AH treatment is a matter of medicine and public health.
Extracorporeal cardiopulmonary resuscitation (ECPR), which applies extracorporeal membrane oxygenation (ECMO) to patients with cardiac arrest refractory to conventional cardiopulmonary resuscitation (CPR), has been reported to improve outcomes for AH patients presenting with cardiac arrest or circulation instability [6,7,8,9]. Previous studies have also reported cases of prolonged cardiac arrest with hypothermia who received ECPR, in which the patients survived without neurologic impairment [10,11,12].
Previous studies have revealed that low-flow time, the duration between the initiation of conventional CPR and the implementation of ECPR, is associated with ECPR outcomes for cardiac arrest patients [13,14,15,16,17]. The guidelines from the European Resuscitation Council and the Extracorporeal Life Support Organization recommend initiating ECPR until 60 min of low-flow time [18, 19]. However, whether ECPR for cardiac arrest patients with AH results in good neurological outcomes even with prolonged low-flow time has not yet been fully investigated. Consequently, the present study aimed to assess the association between low-flow time and outcomes in AH patients and compared to those of patients without AH among a cohort of OHCA patients resuscitated using ECPR.
Methods
Study design and data
This study was a secondary analysis of the multicenter retrospective cohort study, the Study of Advanced life support for Ventricular fibrillation with Extracorporeal circulation in Japan II (SAVE-J II) in Japan. Thirty-six institutions in Japan participated in this registry. This multicenter study was pre-registered at the Japanese clinical trial registry (registration number: UMIN000036490) [20], and approved by the institutional review board of Kagawa University (approval number: 2018-110) and each participating institution. Owing to the retrospective study design, informed consent was not required. However, patients were given the opportunity to opt out of the study at any time by withdrawing permission to use their data. To ensure patients’ right to refuse participation, the methods of utilizing patient information were disclosed on the websites and notice boards of each participating institution.
SAVE-J II included all patients aged ≥ 18 years who were admitted to the emergency department for OHCA and underwent ECPR between January 1, 2013 and December 31, 2018. In this registry, ECPR was defined as resuscitation for cardiac arrest using veno-arterial ECMO. The exclusion criteria were patients with in-hospital cardiac arrest and refusal to participate in the study communicated by the patients themselves, family, or others. The following data were collected: patient characteristics, prehospital information, information on hospital arrival, diagnosis, interventions, mechanical support information, time course, and outcomes [21].
Study population and data collection
We included all patients of the SAVE-J II study. The exclusion criteria of this secondary analysis were as follows: return of spontaneous circulation before ECMO pump on; transfer from another hospital; and missing data on outcomes (survival to hospital discharge and cerebral performance category [22] at hospital discharge), low-flow time, body temperature at hospital arrival, and covariates, as mentioned below.
The following patient data were used for this secondary analysis: age, sex, location of cardiac arrest (home, public space, or ambulance), witnessed cardiac arrest, bystander CPR, initial cardiac rhythm (shockable or unshockable) at the scene and at hospital arrival, body temperature at hospital arrival, the detailed time course of resuscitation, survival to hospital discharge, and cerebral performance category at hospital discharge. Initial shockable rhythm was defined as ventricular fibrillation, pulseless ventricular tachycardia, or rhythm for defibrillation in an automated external defibrillator used by emergency medical staff.
Variables of interest
The variables of interest were body temperature at hospital arrival and low-flow time. Body temperatures were measured at the body surface or core body temperature, which were not recorded in this registry. Following the previous studies on AH [9, 23], we defined AH as body temperatures < 32 °C.
Low-flow time was defined as follows: (i) the duration from cardiac arrest to the establishment of ECPR when the cardiac arrest occurred in the ambulance, (ii) the duration from the call for an ambulance to the establishment of ECPR when the cardiac arrest occurred before ambulance arrival with bystander CPR, or (iii) the duration from the arrival of emergency medical service to the establishment of ECPR when the cardiac arrest occurred before ambulance arrival without bystander CPR.
Outcomes
The primary outcome was survival at hospital discharge. The secondary outcome was favorable neurological outcome, defined as a cerebral performance category of 1 or 2 at hospital discharge.
Statistical analysis
Categorical variables were counted and presented as proportions. Continuous variables were expressed as medians and interquartile ranges.
First, we compared the baseline characteristics and outcomes using the Wilcoxon rank-sum test for continuous variables and the Chi-square test for categorical variables.
Next, we examined the non-linear associations between body temperature at hospital arrival and outcomes for all eligible patients using restricted cubic spline analyses [24]. We set four knots in the cubic splines, placed on the fifth, 35th, 65th, and 95th percentile of body temperature [25]. We adjusted for age, sex, the location of cardiac arrest, witnessed cardiac arrest, bystander CPR, the initial cardiac rhythm at the scene and upon hospital arrival and low-flow time. We calculated the adjusted outcomes and their 95% confidence intervals (CIs) for each value of body temperature.
Then, we examined the non-linear associations between low-flow time and outcomes using restricted cubic spline analyses stratified by the presence or absence of AH (hypothermia defined as body temperature below 32 °C). We set four knots in the cubic splines, placed on the fifth, 35th, 65th, and 95th percentiles of low-flow time. We adjusted for age, sex, location of cardiac arrest, witnessed cardiac arrest, bystander CPR, and the initial cardiac rhythm at the scene and upon hospital arrival. We calculated the adjusted outcomes and their 95% CIs for each value of low-flow time.
Finally, we stratified the patients into two groups according to the cut-off value of low-flow time. Since a method has not been universally accepted for determining the cut-off value, we defined a new method in this study to assess the association between low-flow time and outcomes in patients with AH and compared them with those of patients without AH. We defined the cut-off value based on the qualitative assessment of the appearance of the restricted cubic spline curves on the survival discharge rate. Then, we investigated whether the presence of AH had interactions on the association between low-flow time and outcomes by performing multivariable logistic regression analyses for the outcomes with the category of low-flow time (short or long), the presence of AH, their interaction term, and same covariates adjusted in the restricted cubic spline analyses. The odds ratios (ORs) and their 95% CIs on outcomes were calculated for each body temperature group with respect to the reference group with long low-flow time.
As a sensitivity analysis, with the definition of AH as below 28 °C instead of below 32 °C, we examined the non-linear association between low-flow time and outcomes and investigated whether AH had interactions on the association between low-flow time and outcomes in the same way as in the main analysis. AH was defined as a body temperature below 28 °C because the risk of cardiac arrest increases substantially if the core temperature drops below 28 ℃ [1], and severe hypothermia is usually defined as a core temperature below 28 ℃ [26].
Statistical analyses were performed using STATA/BE 17.0 software (StataCorp, College Station, TX, USA) and R 4.3.1 software (R Foundation for Statistical Computing, Vienna, Austria).
Results
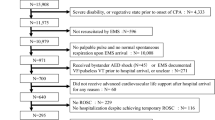
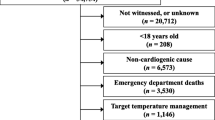
Of the 2,157 adult patients with OHCA who received ECPR, 1,252 were eligible in this analysis. Of these, 105 (8.4%) were in the AH group and 1,147 (91.6%) were in the non-AH group (Additional file 1: Figure S1).
Characteristics of patients at baseline and outcomes
As to the all eligible patients, the median age was 61 years, and 82.5% were male (Table 1). The median body temperature was 35.1 °C (34.0–35.8 °C), and the median low-flow time was 52 (42–63) min. The overall survival at hospital discharge and favorable neurological outcome were 27.0% and 13.9%, respectively. Patients in the AH group were older, more likely to be female, more likely to be unwitnessed, less likely to receive bystander CPR, and more likely to have initial unshockable rhythm. The median low-flow times, survival at hospital discharge, and favorable neurological outcomes of patients in the AH and non-AH groups were 60 (47–79) and 51 (42–62) min, 44.8% and 25.4%, and 25.7% and 12.8%, respectively (all p < 0.001). Only one patient in the AH group had serum potassium levels > 10 mmol/L at hospital arrival (Additional file 2: Table S1).
Association between body temperature and outcomes
The cubic spline analysis of survival discharge rate and favorable neurological outcomes of all eligible patients showed increased trend with lower body temperature below 32 °C, with little change between 32 °C and 36 °C (Fig. 1, Additional file 3: Figure S2).
Non-linear associations between arrival body temperature and survival discharge. Four body temperature points (26.7, 34.5, 35.5, and 36.7 °C) were used as the knots in the cubic splines. In the cubic spline analyses, we adjusted for age, sex, location of cardiac arrest, witnessed cardiac arrest, bystander cardiopulmonary resuscitation, the initial cardiac rhythm at the scene and upon hospital arrival, and low-flow time
Association between low-flow time and outcomes in the AH and non-AH groups
In the AH group, the cubic spline analysis showed that the survival discharge rate remained relatively unchanged irrespective of the low-flow time (Fig. 2). In the non-AH group, the cubic spline analysis showed decreased trend from 20 to 60 min, with little change above 60 min. The survival discharge rate was higher in the AH group between 50 to 90 min of low-flow time compared with that in the non-AH group. The cubic spline analysis on favorable neurological outcomes showed a similar trend (Additional file 4: Figure S3).
Non-linear associations between low-flow time and survival discharge stratified by the presence of accidental hypothermia. Four low-flow time points (28, 46, 57, and 88 min) were used as the knots in the cubic splines. In the cubic spline analyses, we adjusted for age, sex, location of cardiac arrest, witnessed cardiac arrest, bystander cardiopulmonary resuscitation, and the initial cardiac rhythm at the scene and upon hospital arrival
Based on the cubic spline curve between the low-flow time and survival outcomes (Fig. 2), patients were stratified into the short (1–50 min) and long (> 50 min) low-flow time groups. In the AH group, the survival discharge rate in the short and long low-flow time groups was 45.5% and 44.4%, respectively, with no statistically significant difference between the groups (OR, 1.05; 95% CI 0.40–2.79). In the non-AH group, the survival discharge rate in the short and long low-flow time groups was 32.1% and 19.2%, respectively, with statistically significant difference between the groups (OR, 0.54; 95% CI 0.40–0.73). The interaction analyses showed a statistically significant interaction between low-flow time and AH group in survival discharge rate (p for interaction = 0.048) (Table 2). For the favorable neurological outcome, there was not a significant interaction between low-flow time and the AH group (p for interaction = 0.058).
Sensitivity analyses changing threshold of AH to below 28 °C
When patients were stratified according to the body temperature (below and above 28 °C), 72 (5.8%) and 1,180 (94.2%) were included in the AH and non-AH groups, respectively (Additional file 5: Table S2). The cubic spline curve of outcomes and low-flow time was similar to the main results (Additional file 6: Figure S4, Additional file 7: Figure S5). Statistically significant interaction between low-flow time and body temperature was observed for the survival discharge rate (p for interaction = 0.027), but not for favorable neurological outcome (p for interaction = 0.14) (Additional file 8: Table S3).
Discussion
This study of adult patients with OHCA who had undergone ECPR revealed an increasing trend in the survival discharge and favorable neurological outcome associated with a lower body temperature at arrival below 32 °C. Moreover, the survival outcome for AH patients with a temperature lower than 32 °C remained constant regardless of low-flow time, and there was a significant interaction of their association with patients without AH.
Previous case reports have shown that even with prolonged low-flow time, hypothermia patients with cardiac arrest who undergo ECPR may survive without neurological impairment [10,11,12]. However, this is the first observational study to investigate the association between low-flow time and outcomes of cardiac arrest patients with AH who received ECPR. The main cause of death of the patients resuscitated from OHCA is hypoxic–ischemic brain injury [27]. Hypothermia has protective effect toward cerebral cell death caused by circulation insufficiency with decreasing cerebral metabolic activity and oxygen consumption [28,29,30]. Therefore, it may be pathophysiologically plausible that OHCA patients with AH who received ECPR have good survival outcomes, even with prolonged low-flow time, in contrast to those without AH.
The guidelines from European Resuscitation Council and Extracorporeal Life Support Organization recommend establishing ECPR within 60 min of cardiac arrest without AH [18, 19]. However, this study’s results suggest that different criteria would be applied in the selection of ECPR indications for low-flow time in patients with a body temperature below 32 °C compared to those applicable to patients without hypothermia. In this study, many AH patients had good prognosis when undergoing ECPR, even if the low-flow time to ECPR was as long as 120 min. Therefore, based on our findings, introducing ECPR for AH patients may be reasonable, even if the low-flow time is longer. Further studies are needed to validate our findings.
This study has several limitations. First, although we adjusted the variables as extensively as possible, the large differences in patient characteristics may limit the comparability of the groups because of potential unmeasured confounders, including no-flow time, whether the AH was primary or secondary and the underlying diseases, and whether cardiac arrest preceded the body temperature drop. Concerning the presence of preceding cardiac arrest, serum potassium levels > 10 or 12 mmol/L are considered a marker of existence of hypoxia before body core temperature drop [1]. In this study, only one patient in the AH group had serum potassium levels > 10 mmol/L. Therefore, most AH patients are presumed to have been cooled before cardiac arrest. Second, the methods of temperature measurement were not recorded in this registry; therefore, arrival body temperatures of some patients may be skin temperatures, not core body temperature. In a cold environment, the core body temperature drops slower than skin temperature does [31]. Therefore, we might have misclassified some patients without AH as having AH. However, the survival outcome of non-AH patients was poorer than that of AH patients, and this misclassification caused a bias toward the null hypothesis. Therefore, our results remain robust against this possible bias. Furthermore, an additional questionnaire was administered to examine the details of temperature management in the participating institutions [32]. The questionnaire revealed that > 90% of the institutions monitored the core body temperature. Therefore, the bias due to the absence of a record of the body temperature measurement method in this study was negligible. Third, we approximated low-flow time by calculating the duration from the ambulance call to the initiation of ECPR in cases where cardiac arrest occurred at home or in a public space, and bystander CPR was administered, but this definition did not accurately capture the low-flow time. In cases where telecommunicator CPR was performed, a time lag existed between the emergency call and the initiation of CPR. Therefore, the actual low-flow time might have been longer than the estimated values in these cases. Fourth, the timing of body temperature measurements was not recorded in the registry, and the body temperatures of several patients may have been affected by heat exchangers. However, the measurement of body temperature does not require much time, and the implementation of a heat exchanger is usually performed after admission to the intensive care unit. Therefore, it is reasonable to assume that body temperature was minimally affected by the heat exchanger.
Conclusions
Adult OHCA patients with arrival body temperature lower than 32 °C who received ECPR had relatively good survival outcome regardless of low-flow time, in contrast to those without AH. In adult OHCA patients with AH, implementing ECPR may be considered even with a prolonged low-flow time.
Availability of data and materials
Please contact the author for data and requests.
Abbreviations
- AH:
-
Accidental hypothermia
- CI:
-
Confidence intervals
- CPR:
-
Cardiopulmonary resuscitation
- ECMO:
-
Extracorporeal membrane oxygenation
- ECPR:
-
Extracorporeal cardiopulmonary resuscitation
- OHCA:
-
Out-of-hospital cardiac arrest
- OR:
-
Odds ratio
References
Brown DJ, Brugger H, Boyd J, Paal P. Accidental hypothermia. N Engl J Med. 2012;367:1930–8.
Silfvast T, Pettilä V. Outcome from severe accidental hypothermia in Southern Finland–a 10-year review. Resuscitation. 2003;59:285–90.
Takauji S, Hifumi T, Saijo Y, Yokobori S, Kanda J, Kondo Y, et al. Accidental hypothermia: characteristics, outcomes, and prognostic factors-a nationwide observational study in Japan (Hypothermia study 2018 and 2019). Acute Med Surg. 2021;8: e694.
Walpoth BH, Maeder MB, Courvoisier DS, Meyer M, Cools E, Darocha T, et al. Hypothermic Cardiac Arrest - Retrospective cohort study from the International Hypothermia Registry. Resuscitation. 2021;167:58–65.
Paal P, Pasquier M, Darocha T, Lechner R, Kosinski S, Wallner B, et al. Accidental hypothermia: 2021 update. Int J Environ Res Public Health. 2022;19:501.
Dunne B, Christou E, Duff O, Merry C. Extracorporeal-assisted rewarming in the management of accidental deep hypothermic cardiac arrest: a systematic review of the literature. Heart Lung Circ. 2014;23:1029–35.
Ohbe H, Isogai S, Jo T, Matsui H, Fushimi K, Yasunaga H. Extracorporeal membrane oxygenation improves outcomes of accidental hypothermia without vital signs: a nationwide observational study. Resuscitation. 2019;144:27–32.
Prekker ME, Rischall M, Carlson M, Driver BE, Touroutoutoudis M, Boland J, et al. Extracorporeal membrane oxygenation versus conventional rewarming for severe hypothermia in an urban emergency department. Acad Emerg Med. 2023;30:6–15.
Takauji S, Hayakawa M, Yamada D, Tian T, Minowa K, Inoue A, et al. Outcome of extracorporeal membrane oxygenation use in severe accidental hypothermia with cardiac arrest and circulatory instability: a multicentre, prospective, observational study in Japan (ICE-CRASH study). Resuscitation. 2023;182: 109663.
Husby P, Andersen KS, Owen-Falkenberg A, Steien E, Solheim J. Accidental hypothermia with cardiac arrest: complete recovery after prolonged resuscitation and rewarming by extracorporeal circulation. Intensive Care Med. 1990;16:69–72.
Boue Y, Lavolaine J, Bouzat P, Matraxia S, Chavanon O, Payen JF. Neurologic recovery from profound accidental hypothermia after 5 hours of cardiopulmonary resuscitation. Crit Care Med. 2014;42:e167–70.
Forti A, Brugnaro P, Rauch S, Crucitti M, Brugger H, Cipollotti G, et al. Hypothermic cardiac arrest with full neurologic recovery after approximately nine hours of cardiopulmonary resuscitation: management and possible complications. Ann Emerg Med. 2019;73:52–7.
Wengenmayer T, Rombach S, Ramshorn F, Biever P, Bode C, Duerschmied D, et al. Influence of low-flow time on survival after extracorporeal cardiopulmonary resuscitation (eCPR). Crit Care. 2017;21:157.
Otani T, Sawano H, Natsukawa T, Nakashima T, Oku H, Gon C, et al. Low-flow time is associated with a favorable neurological outcome in out-of-hospital cardiac arrest patients resuscitated with extracorporeal cardiopulmonary resuscitation. J Crit Care. 2018;48:15–20.
Park JH, Song KJ, Shin SD, Ro YS, Hong KJ. Time from arrest to extracorporeal cardiopulmonary resuscitation and survival after out-of-hospital cardiac arrest. Emerg Med Australas. 2019;31:1073–81.
Matsuyama T, Irisawa T, Yamada T, Hayakawa K, Yoshiya K, Noguchi K, et al. Impact of low-flow duration on favorable neurological outcomes of extracorporeal cardiopulmonary resuscitation after out-of-hospital cardiac arrest: a multicenter prospective study. Circulation. 2020;141:1031–3.
Shoji K, Ohbe H, Kudo D, Tanikawa A, Kobayashi M, Aoki M, et al. Low-flow time and outcomes in out-of-hospital cardiac arrest patients treated with extracorporeal cardiopulmonary resuscitation. Am J Emerg Med. 2023;75:37–41.
Soar J, Böttiger BW, Carli P, Couper K, Deakin CD, Djärv T, et al. European Resuscitation Council Guidelines 2021: adult advanced life support. Resuscitation. 2021;161:115–51.
Richardson ASC, Tonna JE, Nanjayya V, Nixon P, Abrams DC, Raman L, et al. Extracorporeal cardiopulmonary resuscitation in adults. Interim guideline consensus statement from the Extracorporeal Life Support Organization. ASAIO J. 2021;67:221–8.
Study of advanced cardiac life support for ventricular fibrillation with extracorporeal circulation in Japan. https://center6.umin.ac.jp/cgi-open-bin/ctr/ctr_view.cgi?recptno=R000041577. Accessed 23 Dec 2023.
SAVE-J II study. http://square.umin.ac.jp/save-j2/en/. Accessed 23 Dec 2023.
Cummins RO, Chamberlain DA, Abramson NS, Allen M, Baskett PJ, Becker L, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein style. A statement for health professionals from a task force of the American Heart Association, the European resuscitation council, the Heart and Stroke Foundation of Canada, and the Australian resuscitation council. Circulation. 1991;84:960–75.
Grin N, Rousson V, Darocha T, Hugli O, Carron PN, Zingg T, et al. Hypothermia outcome prediction after extracorporeal life support for hypothermic cardiac arrest patients: assessing the performance of the HOPE score in case reports from the literature. Int J Environ Res Public Health. 2021;18:11896.
Greenland S. Dose-response and trend analysis in epidemiology: alternatives to categorical analysis. Epidemiology. 1995;6:356–65.
Gauthier J, Wu QV, Gooley TA. Cubic splines to model relationships between continuous variables and outcomes: a guide for clinicians. Bone Marrow Transplant. 2020;55:675–80.
Paal P, Gordon L, Strapazzon G, Brodmann Maeder M, Putzer G, Walpoth B, et al. Accidental hypothermia-an update: the content of this review is endorsed by the International Commission for Mountain Emergency Medicine (ICAR MEDCOM). Scand J Trauma Resusc Emerg Med. 2016;24:111.
Lemiale V, Dumas F, Mongardon N, Giovanetti O, Charpentier J, Chiche JD, et al. Intensive care unit mortality after cardiac arrest: the relative contribution of shock and brain injury in a large cohort. Intensive Care Med. 2013;39:1972–80.
Norwood WI, Norwood CR, Castaneda AR. Cerebral anoxia: effect of deep hypothermia and pH. Surgery. 1979;86:203–9.
Wood SC. Interactions between hypoxia and hypothermia. Annu Rev Physiol. 1991;53:71–85.
Mezrow CK, Midulla PS, Sadeghi AM, Gandsas A, Wang W, Dapunt OE, et al. Evaluation of cerebral metabolism and quantitative electroencephalography after hypothermic circulatory arrest and low-flow cardiopulmonary bypass at different temperatures. J Thorac Cardiovasc Surg. 1994;107:1006–19.
Strapazzon G, Procter E, Paal P, Brugger H. Pre-hospital core temperature measurement in accidental and therapeutic hypothermia. High Alt Med Biol. 2014;15:104–11.
Hifumi T, Inoue A, Otani T, Otani N, Kushimoto S, Sakamoto T, et al. Details of targeted temperature management methods for patients who had out-of-hospital cardiac arrest receiving extracorporeal cardiopulmonary resuscitation: a questionnaire survey. Ther Hypothermia Temp Manag. 2022;12:215–22.
Acknowledgements
The authors would like to thank all members of the SAVE-J II study group who participated in this study: Hirotaka Sawano, M.D., Ph.D. (Osaka Saiseikai Senri Hospital), Yuko Egawa, M.D., Shunichi Kato, M.D. (Saitama Red Cross Hospital), Kazuhiro Sugiyama M.D. (Tokyo Metropolitan Bokutoh Hospital), Naofumi Bunya, M.D., Takehiko Kasai, M.D. (Sapporo Medical University), Shinichi Ijuin, M.D., Shinichi Nakayama, M.D., Ph.D. (Hyogo Emergency Medical Center), Jun Kanda, M.D., Ph.D., Seiya Kanou, M.D. (Teikyo University Hospital), Toru Takiguchi, M.D., Shoji Yokobori, M.D., Ph.D. (Nippon Medical School), Hiroaki Takada, M.D., Kazushige Inoue, M.D. (National Hospital Organization Disaster Medical Center), Ichiro Takeuchi, M.D., Ph.D., Hiroshi Honzawa, M.D. (Yokohama City University Medical Center), Makoto Kobayashi, M.D., Ph.D., Tomohiro Hamagami, M.D. (Toyooka Public Hospital), Wataru Takayama, M.D., Yasuhiro Otomo, M.D., Ph.D. (Tokyo Medical and Dental University Hospital of Medicine), Kunihiko Maekawa, M.D. (Hokkaido University Hospital), Takafumi Shimizu, M.D., Satoshi Nara, M.D. (Teine Keijinkai Hospital), Michitaka Nasu, M.D., Kuniko Takahashi, M.D. (Urasoe General Hospital), Yoshihiro Hagiwara, M.D., M.P.H. (Imperial Foundation Saiseikai, Utsunomiya Hospital), Reo Fukuda, M.D. (Nippon Medical School Tama Nagayama Hospital), Takayuki Ogura, M.D., Ph.D. (Japan Red Cross Maebashi Hospital), Shinichiro Shiraishi, M.D. (Aizu Central Hospital), Ryosuke Zushi, M.D. (Osaka Mishima Emergency Critical Care Center), Norio Otani, M.D. (St. Luke’s International Hospital), Migaku Kikuchi, M.D., Ph.D. (Dokkyo Medical University), Kazuhiro Watanabe, M.D. (Nihon University Hospital), Takuo Nakagami, M.D. (Omihachiman Community Medical Center), Tomohisa Shoko, M.D., Ph.D. (Tokyo Women’s Medical University Medical Center East), Nobuya Kitamura, M.D., Ph.D. (Kimitsu Chuo Hospital), Takayuki Otani, M.D. (Hiroshima City Hiroshima Citizens Hospital), Yoshinori Matsuoka, M.D., Ph.D. (Kobe City Medical Center General Hospital), Masaaki Sakuraya, M.D., M.P.H. (JA Hiroshima General Hospital Hiroshima), Hideki Arimoto, M.D. (Osaka City General Hospital), Koichiro Homma, M.D., Ph.D. (Keio University School of Medicine), Hiromichi Naito, M.D., Ph.D. (Okayama University Hospital), Shunichiro Nakao, M.D., Ph.D. (Osaka University Graduate School of Medicine), Tomoya Okazaki, M.D., Ph.D. (Kagawa University Hospital), Yoshio Tahara, M.D., Ph.D. (National Cerebral and Cardiovascular Center), Hiroshi Okamoto, M.D, M.P.H. (St. Luke’s International Hospital), Jun Kunikata, M.D., Ph.D., and Hideto Yokoi, M.D., Ph.D. (Kagawa University Hospital).
Funding
This study did not receive specific grants from public, commercial, or non-profit funding agencies.
Author information
Authors and Affiliations
Consortia
Contributions
KS and HO were responsible for the conception of analysis. KS, HO, and TM were responsible for data analysis and data implementation. All authors have drafted the work and substantively revised it. All authors read and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the institutional review board of Kagawa University (approval number: 2018–110) and each participating institution. The requirement for patient consent was waived at all participating institutions because of the retrospective nature of this study.
Consent for publication
Not applicable.
Competing interests
The author declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Patient flowchart. AH, accidental hypothermia; ECMO, extracorporeal membrane oxygenation; ECPR, extracorporeal cardiopulmonary resuscitation; ROSC, return of spontaneous circulation.
Additional file 2: Table S1.
Serum potassium levels at hospital arrival of patients in the AH group.
Additional file 3: Figure S2.
Non-linear associations between arrival body temperature and favorable neurological outcome. Four body temperature points (26.7, 34.5, 35.5, and 36.7 °C) were used as the knots in the cubic splines. In the cubic spline analyses, we adjusted for age, sex, location of cardiac arrest, witnessed cardiac arrest, bystander cardiopulmonary resuscitation, the initial cardiac rhythm at the scene and upon hospital arrival, and low-flow time.
Additional file 4: Figure S3.
Non-linear associations between low-flow time and favorable neurological outcome stratified by the presence of accidental hypothermia. Four low-flow time points (28, 46, 57, and 88 min) were used as the knots in the cubic splines. In the cubic spline analyses, we adjusted for age, sex, location of cardiac arrest, witnessed cardiac arrest, bystander cardiopulmonary resuscitation, and the initial cardiac rhythm at the scene and upon hospital arrival.
Additional file 5: Table S2.
Patient characteristics and outcomes of the patients with arrival body temperature below and above 28 °C.
Additional file 6: Figure S4.
Non-linear associations between low-flow time and survival discharge stratified by the body temperature below and above 28 °C. Four low-flow time points (28, 46, 57, and 88 min) were used as the knots in the cubic splines. In the cubic spline analyses, we adjusted for age, sex, location of cardiac arrest, witnessed cardiac arrest, bystander cardiopulmonary resuscitation, and the initial cardiac rhythm at the scene and upon hospital arrival.
Additional file 7: Figure S5.
Non-linear associations between low-flow time and favorable neurological outcome stratified by the body temperature below and above 28 °C. Four low-flow time points (28, 46, 57, and 88 min) were used as the knots in the cubic splines. In the cubic spline analyses, we adjusted for age, sex, location of cardiac arrest, witnessed cardiac arrest, bystander cardiopulmonary resuscitation, and the initial cardiac rhythm at the scene and upon hospital arrival.
Additional file 8: Table S3.
Outcomes of patients with arrival body temperature below and above 28 °C with different low-flow times.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shoji, K., Ohbe, H., Matsuyama, T. et al. Low-flow time and outcomes in hypothermic cardiac arrest patients treated with extracorporeal cardiopulmonary resuscitation: a secondary analysis of a multi-center retrospective cohort study. j intensive care 12, 22 (2024). https://doi.org/10.1186/s40560-024-00735-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40560-024-00735-1