Abstract
Background
The prognosis for acute exacerbation of idiopathic pulmonary fibrosis (AE-IPF) is poor, and there is no established treatment. Hence, we aimed to investigate the effectiveness of a polymyxin B-immobilised fibre column (PMX) for the treatment of AE-IPF.
Methods
Data were retrospectively collected from the Japanese Diagnosis Procedure Combination database from 1 July 2010 to 31 March 2018. We identified adult patients with idiopathic pulmonary fibrosis who received high-dose methylprednisolone (mPSL) therapy and mechanical ventilation upon admission. Eligible patients (n = 5616) were divided into those receiving PMX treatment combined with high-dose mPSL (PMX group, n = 199) and high-dose mPSL alone (mPSL alone group, n = 5417). To compare outcomes between the two groups, we applied a stabilised inverse probability of treatment weighting (IPTW) using propensity scores. The primary outcome was in-hospital mortality, and the secondary outcomes were 14- and 28-day mortality and length of hospital stay.
Results
The in-hospital mortality rates of the PMX and mPSL alone groups were 79.9% and 76.4%, respectively. The results did not significantly differ between the two groups after performing a stabilised IPTW. The odds ratio of the PMX group compared with the mPSL alone group was 1.56 (95% confidence interval 0.80–3.06; p = 0.19). The 14- and 28-day mortality and length of hospital stay (secondary outcomes) also did not significantly differ between the two groups.
Conclusions
In AE-IPF patients using mechanical ventilation, the treatment outcome was not significantly better for PMX combined with high-dose mPSL than for high-dose mPSL alone.
Similar content being viewed by others
Background
Idiopathic pulmonary fibrosis (IPF) is an interstitial lung disease characterised by chronic and progressive fibrosis, with a poor prognosis and an average survival time of 3–4 years [1]. Patients with IPF sometimes develop acute respiratory failure, known as acute exacerbation of IPF (AE-IPF), which is associated with a 90-day mortality rate of approximately 50% [2].
In AE-IPF, various inflammatory mediators are produced and alveolar epithelial damage is induced, resulting in respiratory failure and pathological lesions of diffuse alveolar damage [1,2,3,4]. Although there is no established treatment for AE-IPF, the therapeutic options in the Japanese and international guidelines include immunosuppressive agents and corticosteroids, such as high-dose methylprednisolone (mPSL) [3, 4]. A polymyxin B-immobilised fibre column (PMX) is a medical device originally developed for removing circulating endotoxin and is used for treating sepsis [5, 6]. However, randomised trials did not show an effect of PMX for patients with sepsis [7]. Several studies have shown that PMX was associated with reducing several other inflammatory mediators, such as high-mobility group box 1 and neutrophils [8, 9]. Additionally, some reports have shown that PMX potentially could be effective for ARDS, which is similar in pathophysiology to AE-IPF [10, 11]. Small observational studies have shown that PMX treatment was associated with better short-term prognosis of AE-IPF [12,13,14,15,16]. However, these were retrospective studies with small sample sizes and lacked adjustment for confounding factors. Moreover, the effectiveness of PMX treatment in patients with AE-IPF who develop severe respiratory failure remains unclear.
This study used data collected from a Japanese nationwide inpatient database and aimed to evaluate the effectiveness of PMX treatment in patients with AE-IPF who developed severe respiratory failure.
Methods
Data source
Inpatient data were extracted from the Japanese Diagnosis Procedure Combination database, the details of which have been reported elsewhere [17]. More than 1000 hospitals, representing approximately 50% of all discharges from acute care hospitals in Japan. We collected data that included sex and age; hospitalisation and discharge dates; weight and height; severity of dyspnoea based on the Hugh–Jones dyspnoea scale [18]; level of consciousness upon admission; smoking index; activities of daily living; frequency of hospitalisation; intensive care unit (ICU) admission during hospitalisation; main diagnoses, pre-existing comorbidities upon admission and complications after admission as recoded by the attending physicians based on the International Classification of Diseases, 10th revision (ICD-10) codes accompanied by text in Japanese; procedures and their dates; dates and doses of drugs administered during hospitalisation; and discharge status.
Patient selection
This study used data collected from 1 July 2010 to 31 March 2018. The inclusion criteria were patients aged ≥ 15 years, those diagnosed with interstitial pneumonia (ICD-10 codes J84.1, J84.8 and J84.9), those who underwent computed tomography scan within 1 day after admission and those who received treatment with intravenous mPSL at a dose of 500–1000 mg/day for 3 days, which was started within 4 days after admission [19, 20]. Patients with IPF were selected as follows. Firstly, we excluded patients with any of the following diagnoses of idiopathic interstitial pneumonias other than IPF recorded in Japanese text: idiopathic nonspecific interstitial pneumonia, respiratory bronchiolitis-associated interstitial lung disease, cryptogenic organising pneumonia, acute interstitial pneumonia, desquamative interstitial pneumonia, lymphoid interstitial pneumonia, idiopathic pleuroparenchymal fibroelastosis and unclassifiable idiopathic interstitial pneumonia. Secondly, we excluded patients with secondary interstitial lung diseases identified using ICD-10 codes (hypersensitivity pneumonitis [J67], connective tissue disease associated with interstitial lung disease [M05, M06 and M30–35], sarcoidosis [D86], amyloidosis [E85], drug-induced lung disease [J70], radiation pneumonitis [J70], Pneumocystis jirovecii pneumonia [B59], pneumoconiosis [J60–65], pulmonary alveolar proteinosis [J84.0)] eosinophilic pneumonia [J82], Langerhans cell histiocytosis [C96] and lymphangioleiomyomatosis [D21.9]); those receiving medications, including carperitide and tolvaptan for acute heart failure, within 1 day after admission; and those who received intra-aortic balloon pumping during hospitalisation [19, 20]. The remaining patients were assumed to have AE-IPF. Then, we also excluded patients with missing data about the level of consciousness, age and treatment year; patients who died within 6 days after admission to prevent immortal time bias; patients with sepsis (ICD-10 codes A40 and A41) and those without mechanical ventilation. In this study, we included only AE-IPF patients with mechanical ventilation under intubation and we did not count the use of non-invasive positive pressure ventilation as an inclusion criterion. Eligible patients were divided into two groups: those who received PMX treatment for ≥ 1 day, which was started within 6 days after admission, combined with high-dose mPSL (PMX group) and those who received high-dose mPSL alone (mPSL alone group).
Characteristics of patients
The characteristics of patients evaluated in this study were sex, age, treatment year, body mass index, Hugh–Jones dyspnoea scale scores upon admission, level of consciousness upon admission, Charlson Comorbidity Index, smoking index, activities of daily living scale (Barthel Index) upon admission, history of previous hospitalisation (0, 1–2 or ≥ 3), type of hospital (academic or non-academic hospital), ICU admission and comorbidities. The Charlson Comorbidity Index scores were calculated according to the previous study (Additional file 1) [21]. The Charlson Comorbidity Index scores were classified into four categories (0, 1, 2 and ≥ 3). Further, we examined data on procedures and treatments, including haemodialysis, high-flow nasal cannula oxygen therapy and use of antibiotics and medications for IPF within 3 days after admission. We identified the use of hydrocortisone, as well as noradrenaline, as a treatment for shock, because shock is a complication indicating the severity in patients with AE-IPF. The Japan Coma Scale was used to evaluate the level of consciousness upon admission [22, 23], which is widely used in Japan and well correlated with the Glasgow Coma Scale score [24]. The ICD-10 codes were used to identify the following comorbidities (Additional file 2: Table S1) bronchial asthma, chronic obstructive pulmonary disease, pneumonia, pulmonary embolism, bronchiectasis, pneumothorax, lung and other types of cancer, disseminated intravascular coagulation, chronic heart failure, acute coronary syndrome, diabetes mellitus, stroke, renal failure, liver dysfunction, gastroesophageal reflux disease and urinary tract infection.
Outcome
The primary outcome was all-cause in-hospital mortality. The secondary outcomes were 14- and 28-day mortality and length of hospital stay.
Statistical analysis
Dichotomous and categorical variables were presented as numbers with percentages and continuous variables as the median and interquartile range (IQR). To account for differences in baseline characteristics between the two groups, we conducted stabilised inverse probability of treatment weighting (IPTW) analyses using propensity scores. Stabilised IPTW uses propensity scores and adjusts for measured potential confounders while preserving sample size [25]. To control covariate imbalance, the specific stabilised weights were generated using propensity scores, which can predict the probability of receiving PMX treatment combined with high-dose mPSL therapy. To estimate the propensity score, a logistic regression model for receiving high-dose mPSL alone therapy was used with the following independent variables: sex, age, treatment year, body mass index, Hugh–Jones dyspnoea scale score, level of consciousness upon admission, Charlson Comorbidity Index, smoking index, Barthel Index upon admission, frequency of hospitalisation, type of hospital, ICU hospitalisation within 3 days after admission, comorbidities and procedures (haemodialysis and high-flow nasal cannula oxygen therapy), antibiotics (ampicillin/sulbactam, tazobactam/piperacillin, third-generation cephalosporin, fourth-generation cephalosporin, carbapenem, fluoroquinolone and anti-methicillin-resistant Staphylococcus aureus drug) and drugs (noradrenaline, hydrocortisone, cyclophosphamide, tacrolimus, pirfenidone, nintedanib and furosemide). A standardised mean difference was used to assess covariate balance. A value of < 20% indicated an acceptable balancing of covariates between the two groups. Stabilised IPTW analyses can preserve sample size and appropriately estimate average treatment effects over the marginal distribution of measured covariates in a study cohort.
We used generalised linear models with cluster-robust standard errors, treating each hospital as a cluster, to compare the primary and secondary outcomes. Logistic regression analyses of in-hospital mortality and 14- and 28-day mortality were performed. Then, odds ratios and their 95% confidence intervals (CIs) were calculated. The lengths of hospital stay between the two groups were compared via Poisson regression analysis, and the incidence rate ratios and their 95% CIs were calculated. To address competing outcomes, the lengths of hospital stay was evaluated among the survivors alone and all patients.
We performed sensitivity analysis 1 for patients who received PMX treatment and/or high-dose mPSL therapy at an earlier stage after admission. We included patients diagnosed with interstitial pneumonia who received treatment with intravenous mPSL at a dose of 500–1000 mg/day for 3 days, which was started within 2 days after admission. Then, we divided the patients into two groups: those who received PMX treatment for ≥ 1 day, which was started within 4 days after admission, combined with high-dose mPSL (PMX_S1 group) and those who received high-dose mPSL alone (mPSL alone_S1 group). We excluded patients who died within 4 days after admission. Other inclusion and exclusion criteria were the same as in the main analysis. Furthermore, we conducted sensitivity analysis 2 which included only patients aged 51 years or older, because IPF develops predominantly in the elderly. We used the same inclusion and exclusion criteria as in the main analysis except for age, and divided patients into two groups: those who received PMX treatment combined with high-dose mPSL (PMX_S2 group) and those who received high-dose mPSL alone (mPSL alone_S2 group). We examined the same outcomes in sensitivity analysis 1 and 2 as in the main analysis.
A two-tailed significance level of 0.05 was used in all statistical analyses. STATA/MP version 16 software (STATA Corp., College Station, TX, USA) was used to perform all tests.
Results
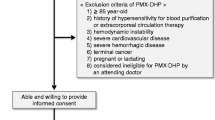
Figure 1 shows the process of patient selection. During the study period, 37781 patients underwent computed tomography scan within 1 day and received high-dose mPSL corticosteroid therapy within 4 days after admission. Among them, 5616 patients were eligible for this study. The patients were divided into the PMX group (n = 199) and the mPSL alone group (n = 5417). None of the patients in our cohort had undergone veno-venous extracorporeal membrane oxygenation or lung transplantation.
Flow chart of patient selection. *idiopathic nonspecific interstitial pneumonia, respiratory bronchiolitis-associated interstitial lung disease, cryptogenic organising pneumonia, acute interstitial pneumonia, desquamative interstitial pneumonia, lymphoid interstitial pneumonia, idiopathic pleuroparenchymal fibroelastosis and unclassifiable idiopathic interstitial pneumonia. IP, interstitial pneumonia; CT, computed tomography; IPF, idiopathic pulmonary fibrosis; mPSL, methylprednisolone; PMX, polymyxin B-immobilised fibre column
Table 1 shows the baseline patient characteristics, and Table 2 provides comorbidities and treatments before and after stabilised IPTW. The proportion of patients aged ≥ 80 years was higher in the mPSL alone group than in the PMX group. Moreover, the percentages of patients with BMI of < 23 kg/m2 and a higher Hugh–Jones dyspnoea scale scores were higher in the mPSL alone group than in the PMX group. A higher percentage of patients in the PMX (46.2%) group were admitted to the ICU. The percentage of patients with renal failure or receiving haemodialysis was higher in the PMX group than in the mPSL alone group. The frequency of some antibiotics use was not balanced between the two groups. After the stabilised IPTW using propensity scores, the baseline characteristics of the patients were well balanced between the two groups.
The in-hospital mortality rates before the stabilised IPTW in the PMX and mPSL alone groups were 79.9% (159/199) and 76.4% (4137/5417), respectively (Tables 3). Tables 3 and 4 presents the outcomes after the stabilised IPTW. The in-hospital mortality rates of the PMX and mPSL alone groups were 83.7% (164/196) and 76.4% (4151/5435), respectively. The results did not significantly differ between the two groups, and the odds ratio of the PMX group was 1.56 (95% CI 0.80–3.06; p = 0.19). Similarly, the odds ratios of 14- and 28-day mortality in the PMX group were 1.16 (95% CI 0.58–2.31; p = 0.67) and 1.38 (95% CI 0.86–2.20; p = 0.18), respectively. In the PMX group, the incidence rate ratio of length of hospital stay was 0.94 (95% CI 0.78–1.13; p = 0.52) compared with that of the mPSL alone group, and the same results were obtained in the analysis of survivors alone.
The results of sensitivity analysis 1 restricted to patients who received PMX treatment and/or high-dose mPSL therapy at an earlier stage after admission were comparable to those of the main analyses (Additional file 3: Table S2, Additional file 4: Table S3, Additional file 5: Table S4, Additional file 6: Table S5). Similarly, the results of sensitivity analysis 2 for patients aged 51 years and older were consistent with those of the main analyses (Additional file 7: Table S6, Additional file 8: Table S7, Additional file 9: Table S8, Additional file 10: Table S9).
Discussion
We used data from a nationwide database in Japan to investigate the effectiveness of PMX treatment combined with high-dose mPSL therapy in patients with AE-IPF. The results showed no significant difference in the in-hospital mortality between the PMX and mPSL alone groups. Similarly, the 14- and 28-day mortality and length of hospital stay did not remarkably differ between the two groups. The results of the sensitivity analyses supported these findings.
Several limited studies from Japan and Korea reported that PMX treatment improved the prognosis of AE-IPF [12,13,14,15,16]. Theoretically, PMX adsorbs inflammatory mediators, such as high mobility group box 1, neutrophils and interleukin-6 that cause respiratory failure in AE-IPF [8, 9, 26]. However, previous studies have been conducted only in a very small number of participating institutions and patients, and some studies lacked a control group [12,13,14,15,16]. Moreover, publication bias might also be a concern because there have been no studies of large populations since the first study showing the effectiveness of PMX treatment in AE-IPF was published in 2006 [11]. Using a national database, we examined the effectiveness of PMX treatment in a much larger number of IPF patients with respiratory failure than in previous studies and showed that no significant benefit was obtained from PMX with high-dose mPSL therapy compared with high-dose mPSL therapy alone.
When PMX treatment is administered to treat AE-IPF, it reportedly is more effective if started early after AE-IPF onset. Oishi et al. showed that prognosis was better for patients administered PMX treatment within 48 h of high-dose mPSL therapy than for those administered PMX treatment 48 h after high-dose mPSL therapy [27]. In our study, we included IPF patients who received treatment with high-dose mPSL, which was started within 2 days after admission for the sensitivity analysis 1. Patients in the PMX_S1 group were enrolled who received PMX treatment within 4 days after admission. However, the sensitivity analysis 1 also did not show significant effectiveness of PMX treatment for AE-IPF. However, our study was retrospective and included only AE-IPF patients with mechanical ventilation. Further studies are required to evaluate which populations of AE-IPF patients may benefit from PMX.
The mortality rate was higher in both groups in the current study than in previous ones [12,13,14,15,16] because our study included only AE-IPF patients with mechanical ventilation to reduce differences in disease severity between the two groups. Although the international guidelines for the diagnosis and management of IPF had a weak recommendation against the use of mechanical ventilation for IPF patients with respiratory failure [4], we often use mechanical ventilation for those patients in real-world clinical practice. Large-scale studies of AE-IPF patients with preserved respiratory condition who do not need mechanical ventilation are also needed in the future.
In the present study, we excluded patients with ICD-10 codes for sepsis. However, because our study included patients with AE-IPF who developed severe respiratory failure, we probably included patients with AE-IPF complicated by sepsis. To account for patients with sepsis, we compared outcomes of the two groups after balancing according to their treatments for severe infection. Furthermore, since our cohort included only patients with AE-IPF and the proportion of patients with sepsis was adjusted between the two groups, under the premise that PMX has no effect on sepsis, the effect of PMX may likely be on AE-IPF.
This study had several limitations. First, because the database did not include data about laboratory examinations, pulmonary function test results, performance status, the use of home oxygen therapy and radiological findings, the severity of IPF at AE onset could not be accurately evaluated. We only included patients who received mechanical ventilation to equalise the severity of AE-IPF between the two groups. In addition, baseline characteristics and treatments were well balanced between the two groups according to the stabilised IPTW. Second, although the IPF diagnosis was made by a physician, it was not confirmed by radiological and pathological examinations. Recently, multidisciplinary discussion (MDD) by physicians, radiologists and pathologists is recommended for the diagnosis of IPF [28]. In fact, however, it has been reported that not many facilities are able to perform MDD, and there is no established worldwide standardisation of the MDD or how to ensure its accuracy [29]. To accurately classify IPF, the diagnoses in the Japanese or ICD-10 codes were used to exclude all patients with idiopathic interstitial pneumonias other than IPF and secondary interstitial pneumonia because the specificity of respiratory disease diagnoses in the database is generally high [30, 31]. The strength of this study lies in the fact that we were able to accumulate a large number of cases, which would not have been feasible in a prospective study, and to evaluate the effectiveness of PMX using statistical methods. Third, although we included only AE-IPF patients who received mechanical ventilation, less than half of the original cohort were hospitalised in the ICU within 3 days after admission. The management of critical respiratory failure is multifaceted, and patient care outside the ICU may differ considerably from that inside the ICU. This divergence may reflect the unique situation in Japan. We conducted IPTW using propensity scores and balanced the frequency of ICU hospitalisation between the two groups.
Conclusions
For the treatment of patients with AE-IPF who developed severe respiratory failure, PMX treatment combined with high-dose mPSL was not associated with better in-hospital mortality. Additional studies are required to evaluate the treatment of AE-IPF with PMX treatment.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AE:
-
Acute exacerbation
- CI:
-
Confidence interval
- DIC:
-
Disseminated intravascular coagulation
- ICD-10:
-
International Classification of Diseases, 10th revision
- ICU:
-
Intensive care unit
- IPF:
-
Idiopathic pulmonary fibrosis
- IPTW:
-
Inverse probability of treatment weighting
- IQR:
-
Interquartile range
- MDD:
-
Multidisciplinary discussion
- mPSL:
-
Methylprednisolone
- PMX:
-
Polymyxin B-immobilised fibre column
References
Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824.
Natsuizaka M, Chiba H, Kuronuma K, Otsuka M, Kudo K, Mori M, et al. Epidemiologic survey of Japanese patients with idiopathic pulmonary fibrosis and investigation of ethnic differences. Am J Respir Crit Care Med. 2014;190:773–9.
Homma S, Bando M, Azuma A, Sakamoto S, Sugino K, Ishii Y, et al. Japanese guideline for the treatment of idiopathic pulmonary fibrosis. Respir Investig. 2018;56:268–91.
Collard HR, Ryerson CJ, Corte TJ, Jenkins G, Kondoh Y, Lederer DJ, et al. Acute exacerbation of idiopathic pulmonary fibrosis. An international working group report. Am J Respir Crit Care Med. 2016;194:265–75.
Kushi H, Nakahara J, Miki T, Okamoto K, Saito T, Tanjo K. Hemoperfusion with an immobilized polymyxin B fiber column inhibits activation of vascular endothelial cells. Ther Apher Dial. 2005;9:303–7.
Kushi H, Miki T, Nakahara J, Okamoto K, Saito T, Tanjoh K. Hemoperfusion with an immobilized polymyxin B column reduces the blood level of neutrophil elastase. Blood Purif. 2006;24:212–7.
Dellinger RP, Bagshaw SM, Antonelli M, Foster DM, Klein DJ, Marshall JC, et al. Effect of targeted polymyxin B hemoperfusion on 28-day mortality in patients with septic shock and elevated endotoxin level: the EUPHRATES randomized clinical trial. JAMA. 2018;320:1455–63.
Abe S, Hayashi H, Seo Y, Matsuda K, Kamio K, Saito Y, et al. Reduction in serum high mobility group box-1 level by polymyxin b-immobilized fiber column in patients with idiopathic pulmonary fibrosis with acute exacerbation. Blood Purif. 2011;32:310–6.
Enomoto N, Mikamo M, Oyama Y, Kono M, Hashimoto D, Fujisawa T, et al. Treatment of acute exacerbation of idiopathic pulmonary fibrosis with direct hemoperfusion using a polymyxin B-immobilized fiber column improves survival. BMC Pulm Med. 2015;15:15.
Nakamura T, Kawagoe Y, Matsuda T, Shoji H, Ueda Y, Tamura N, et al. Effect of polymyxin B-immobilized fiber on blood metalloproteinase-9 and tissue inhibitor of metalloproteinase-1 levels in acute respiratory distress syndrome patients. Blood Purif. 2004;22:256–60.
Ohashi K, Ito R, Koda R, Iino N, Takada T. Serum cytokine changes induced by direct hemoperfusion with polymyxin B-immobilized fiber in patients with acute respiratory failure. Respir Investig. 2022;60:585–94.
Seo Y, Abe S, Kurahara M, Okada D, Saito Y, Usuki J, et al. Beneficial effect of polymyxin B-immobilized fiber column (PMX-DHP) hemoperfusion treatment on acute exacerbation of idiopathic pulmonary fibrosis. Results of a pilot study. Intern Med. 2006;45:1033–8.
Enomoto N, Suda T, Uto T, Kato M, Kaida Y, Ozawa Y, et al. Possible therapeutic effect of direct hemoperfusion with a polymyxin B immobilized fibre column (PMX-DHP) on pulmonary oxygenation in acute exacerbation of interstitial pneumonia. Respirology. 2008;13:452–60.
Hara S, Ishimoto H, Sakamoto N, Mukae H, Kakugawa T, Ishimatsu Y, et al. Direct hemoperfusion using immobilised polymyxin B in patients with rapidly progressive interstitial pneumonias: a retrospective study. Respiration. 2011;81:107–17.
Furusawa H, Sugiura M, Mitaka C, Inase N. Direct hemoperfusion with polymyxin B-immobilized fibre treatment for acute exacerbation of interstitial pneumonia. Respirology. 2017;22:1357–62.
Lee JH, Park JH, Kim HJ, Kim HK, Jang JH, Kim YK, et al. The effects of direct hemoperfusion with polymyxin B-immobilized fiber in patients with acute exacerbation of interstitial lung disease. Acute Crit Care. 2021;36:126–32.
Yasunaga H. Real world data in Japan: chapter II the diagnosis procedure combination database. Ann Clin Epidemiol. 2019;1:76–9.
Hugh-Jones P, Lambert AV. A simple standard exercise test and its use for measuring exertion dyspnoea. Br Med J. 1952;1:65–71.
Aso S, Matsui H, Fushimi K, Yasunaga H. Effect of cyclosporine A on mortality after acute exacerbation of idiopathic pulmonary fibrosis. J Thorac Dis. 2018;10:5275–82.
Awano N, Jo T, Yasunaga H, Inomata M, Kuse N, Tone M, et al. Body mass index and in-hospital mortality in patients with acute exacerbation of idiopathic pulmonary fibrosis. ERJ Open Res. 2021;7:00037.
Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173:676–82.
Ohta T, Waga S, Handa W, Saito I, Takeuchi K. New grading of level of disordered consciousness (author’s translation). No Shinkei Geka. 1974;2:623–7.
Shigematsu K, Nakano H, Watanabe Y. The eye response test alone is sufficient to predict stroke outcome reintroduction of Japan Coma Scale: a cohort study. BMJ Open. 2013;3: e002736.
Ono K, Wada K, Takahara T, Shirotani T. Indications for computed tomography in patients with mild head injury. Neurol Med Chir. 2007;47:291–7.
Graham DJ, Reichman ME, Wernecke M, Hsueh YH, Izem R, Southworth MR, et al. Stroke, bleeding, and mortality risks in elderly medicare beneficiaries treated with dabigatran or rivaroxaban for nonvalvular atrial fibrillation. JAMA Intern Med. 2016;176:1662–71.
Oishi K, Mimura-Kimura Y, Miyasho T, Aoe K, Ogata Y, et al. Association between cytokine removal by polymyxin B hemoperfusion and improved pulmonary oxygenation in patients with acute exacerbation of idiopathic pulmonary fibrosis. Cytokine. 2013;61:84–9.
Oishi K, Azuma A, Abe S, Murata Y, Sakamoto K, Mimura Y, et al. Improved prognostic prediction by combination of early initiation of polymyxin b hemoperfusion with modified gender-age-physiology index in acute exacerbation of idiopathic pulmonary fibrosis. Blood Purif. 2022;51:485–91.
Travis WD, Costabel U, Hansell DM, King TE Jr, Lynch DA, Nicholson AG, et al. An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188:733–48.
Glenn LM, Troy LK, Corte TJ. Diagnosing interstitial lung disease by multidisciplinary discussion: a review. Front Med (Lausanne). 2022;9:1017501.
Yamana H, Moriwaki M, Horiguchi H, Kodan M, Fushimi K, Yasunaga H. Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J Epidemiol. 2017;27:476–82.
Awano N, Urushiyama H, Yamana H, Yokoyama A, Ando T, Izumo T, et al. Validity of diagnoses of respiratory diseases recorded in a Japanese administrative database. Respir Investig. 2023;61:314–20.
Acknowledgements
Not applicable.
Funding
This study was supported by grants from the Ministry of Health, Labour and Welfare, Japan (21AA2007 and 20AA2005) and a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology, Japan (20H03907). The funding bodies had no role in the study design; data collection, analysis, or interpretation of the data; or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
NA and TJ designed the study, analysed and interpreted the data and prepared the manuscript. TI, MI, YI, HU and TN interpreted the data. KM collected and interpreted the data. HM and KF collected the data. HY analysed and interpreted the data and prepared the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the institutional review board of The University of Tokyo (Approval number: 3501). The need for informed consent was waived because anonymised data were used.
Consent for publication
Not applicable.
Competing interests
HY reports receiving grants from the Ministry of Health, Labour and Welfare, Japan and the Ministry of Education, Culture, Sports, Science and Technology, Japan during the conduct of the study. All other authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
The methodology for calculating the Charlson Comorbidity Index score.
Additional file 2: Table S1.
List of ICD-10 codes used to identify comorbidities.
Additional file 3: Table S2.
Baseline characteristics of the patients before and after the stabilised IPTW using propensity scores in the sensitivity analyses 1.
Additional file 4: Table S3.
Comorbidities and treatments before and after the stabilised IPTW using propensity scores in the sensitivity analyses 1.
Additional file 5: Table S4.
Outcomes in the PMX_S1 and mPSL alone_S1 groups before and after the stabilised IPTW in the sensitivity analyses 1.
Additional file 6: Table S5.
Comparison of outcomes between the PMX_S1 and mPSL alone_S1 groups after the stabilised IPTW in the sensitivity analyses 1.
Additional file 7: Table S6.
Baseline characteristics of the patients before and after the stabilised IPTW using propensity scores in the sensitivity analyses 2.
Additional file 8: Table S7.
Comorbidities and treatments before and after the stabilised IPTW using propensity scores in the sensitivity analyses 2.
Additional file 9: Table S8.
Outcomes in the PMX_S2 and mPSL alone_S2 groups before and after the stabilised IPTW in the sensitivity analyses 2.
Additional file 10: Table S9.
Comparison of outcomes between the PMX_S2 and mPSL alone_S2 groups after the stabilised IPTW in the sensitivity analyses 2.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Awano, N., Jo, T., Izumo, T. et al. Polymyxin B-immobilised fibre column treatment for acute exacerbation of idiopathic pulmonary fibrosis patients with mechanical ventilation: a nationwide observational study. j intensive care 11, 45 (2023). https://doi.org/10.1186/s40560-023-00693-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40560-023-00693-0