Abstract
Background
The 5A score including five components “Age, Activities of daily living, Arrest, Acidemia and Albumin” was developed as an easy-to-use screening tool for predicting in-hospital mortality among patients with accidental hypothermia. However, the external validity of the 5A score has not yet been evaluated. We aimed to perform an external validation of the 5A score model.
Method
This secondary analysis of the multicenter, prospective cohort Japanese Association for Acute Medicine-Hypothermia Study (2018–2019), which was conducted at 87 and 89 institutions throughout Japan, collected data from December 2018 to February 2019 and from December 2019 to February 2020. Adult accidental hypothermia patients whose body temperature was 35 °C or less were included in this analysis. The probability of in-hospital mortality was calculated using a logistic regression model of the 5A score. The albumin was not recorded in this database; thus, it was imputed by estimation. Predictions were compared with actual observations to evaluate the calibration of the model. Furthermore, decision-curve analysis was used to evaluate the clinical usefulness.
Results
Of the 1363 patients registered in the database, data of 1139 accidental hypothermia patients were included for analysis. The median [interquartile range] age was 79 [68–87] years, and there were 625 men (54.9%) in the study cohort. The predicted probability and actual observation by risk groups produced the following results: low 7% (5.4–8.6), mild 19.1% (17.4–20.8), moderate 33.2% (29.9–36.5), and high 61.9% (55.9–67.9) predicted risks, and the low 12.4% (60/483), mild 17.7% (59/334), moderate 32.6% (63/193), and high 69% (89/129) observed mortality. These results indicated that the model was well calibrated. Decision-curve analysis visually indicated the clinical utility of the 5A score model.
Conclusion
This study indicated that the 5A score model using estimated albumin value has external validity in a completely different dataset from that used for the 5A model development. The 5A score is potentially helpful to predict the mortality risk and may be one of the valuable information for discussing the treatment strategy with patients and their family members.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Accidental hypothermia is an emergency condition that is defined as an unintentional decrease in the body temperature to less than 35 °C, [1] and is associated with a high mortality risk due to life-threatening arrhythmias and multiorgan injury. Approximately half of patients with accidental hypothermia need intensive care unit (ICU) admission [1,2,3]. Furthermore, some of the accidental hypothermia patients require invasive rewarming techniques, such as extracorporeal membrane oxygenation for hemodynamic support [1,2,3]. On the other hand, in a super-aging society such as Japan, most cases of accidental hypothermia occur in residential settings, and the patients are older, frail, and face difficulties in independent living [2,3,4,5]. Some patients in such a population might wish the withdrawal of ICU admission and invasive treatment for avoiding undesirable life-sustaining therapy. In the process of considering treatment strategy, if physicians can provide the critical prognostic information to the patients or their family members, they will make the better clinical decisions considering their values, preference and goals of care [6]. Although some predictors or prediction models in patients with accidental hypothermia have been developed, the reproducibility or generalizability of their predictive performance has not been adequately evaluated [7,8,9,10,11,12,13]. Therefore, a valid and reliable prediction model that has been evaluated by an external validation study is needed for decision-making based on evidence-based predictions of prognosis.
The 5A score model developed by Okada et al. is an easily applied predictive tool that was derived from a logistic regression model (Table 1 and Additional file 1: eAppendix1) [7]. The 5A score includes five predictors with an initial “A” (Age, Activities of daily living, Arrest, Acidemia, and Albumin) and indicated high predictive performance for in-hospital mortality. However, in order to apply such a prediction model to clinical settings, generalizability should be evaluated through external validation using a totally different dataset from that used for developing the model [14, 15]. Although the 5A score was evaluated in external validation using a split sample from an original cohort [7], this method was insufficient to determine the feasibility of clinical application, and the 5A score has not been evaluated by external validation using a completely different dataset.
This study aimed to externally validate the 5A score model for predicting in-hospital mortality by using a dataset that is independent from the one used for the development of the 5A score.
Methods
This study was performed according to the reporting guideline in the Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis statement [16]. This study was approved by the Ethics Review Board of Teikyo University Hospital, Japan (Approval No: 17-090-2) and of each hospital listed in Additional file 1: eAppendix2. The requirement for informed consent was waived because this study is a secondary analysis of anonymized data provided by the Japan Association of Acute Medicine Heatstroke and Hypothermia Surveillance Committee.
Study setting and design
This study is a secondary analysis of the Japanese Association for Acute Medicine (JAAM)-Hypothermia 2018–2019 database. This national database is derived from a prospective, observational, multicenter cohort study conducted by the JAAM Heatstroke and Hypothermia Surveillance Committee and includes consecutive patients whose body temperature was 35 °C or less when measured at the scene by emergency medical services or at the emergency department (ED). This database recorded the data of accidental hypothermia patients between December 2018 and February 2019, and between December 2019 and February 2020 from 87 and 89 institutions in 2018 and 2019, respectively, participated nationwide in Japan. These data do not include the clinical data which were used to develop the 5A score model. A detailed description of this database has been previously reported and is included in Additional file 1: eAppendix2 [3].
Participants
This study included adult (age ≥ 18 years) accidental hypothermia patients whose body temperature was 35 °C or less at ED arrival. Patients whose body temperature data were missing or whose temperature was more than 35 °C at the ED were excluded from this study.
Data collection and outcomes
The following variables were collected as patient characteristics: age, sex, route to hospital, primary cause of accidental hypothermia, settings (indoor or outdoor), lifestyle, activities of daily living (ADL), vital signs, and results of blood test at hospital arrival. Furthermore, information about rewarming method were collected. Definition and details of these variables are provided in Additional file 1: eAppendix3. The outcome of interest was in-hospital mortality.
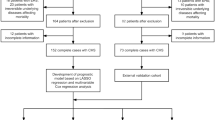
Prediction model of interest
The 5A score model is a prediction model of interest and is scored based on five predictors with an initial “A” on arrival at ED (Age, ADL, Arrest or hemodynamically unstable, Acidemia, and Albumin; Table 1) [7]. The formula for calculating the probability of in-hospital mortality is provided in a supplementary file (Additional file 1: eAppendix1). The details of developing process of 5A score are described in a previous study [7]. In short, the 5A score was originally derived using the J-point registry database which was a multicenter retrospective cohort study database that included accidental hypothermia patients between April 1, 2011, and March 31, 2016, and was conducted in 12 hospitals in the urban areas of the Kyoto, Osaka, and Shiga prefectures in Japan. This score was developed by a logistic model for predicting in-hospital mortality using the clinical information from six of the 12 hospitals in the J-point registry and its internal validity was assessed by bootstrapping. Further, it was evaluated for internal–external validation using data of the other six hospitals in the J-point registry which was different from the data used for the model development. In this study, based on the original definition in the original study of the 5A score model [7], ADL disturbance was defined as the requirement of partial or total assistance for daily activities, such as eating, dressing, taking a bath or shower, and using the toilet, before the event. Albumin was not recorded in the JAAM-Hypothermia 2018–2019 Study; thus, we imputed an estimated value for albumin by using a conversion formula (described in the next section and in Additional file 1: eAppendix4).
Sample size and missing data
With regard to the sample-size estimation, although there are no generally accepted approaches to estimate the sample size for validating prediction models, a previous study suggested that externally validating a prognostic model requires a minimum of 100 events [17]. Therefore, the present study had an adequate sample size with the number of in-hospital death more than 100. For cases with missing data, we described the frequency of the missing data in Additional file 1: eAppendix5. Missing data in the categorical variables of patient characteristics that are not included in the calculation of the 5A score were categorized as “Unknown”; otherwise, missing data were imputed by a multiple imputation technique using the “missForest” R-package [18]. As described above, the serum albumin value was not recorded in the study’s database, and was estimated from the total calcium value based on the previous reports which indicated that the serum albumin value is linearly correlated to the total calcium value [19,20,21,22,23]. Furthermore, sensitivity analysis confirmed the robustness of the results by using different estimating equations and worst-case scenarios. Details of the estimation of the albumin value and sensitivity analysis are described in Additional file 1: eAppendix4)
Statistical analysis
We described the patients’ characteristics using the median and interquartile range (IQR) for continuous variables and the number and percentages (%) for categorical variables. To evaluate the discriminative performance of the 5A score model, we calculated C-statistics with 95% confidence intervals (CI). Moreover, we calculated the probability of in-hospital mortality by using the formula (Additional file 1: eAppendix1) and the mean probability with 95% CI for each value of the 5A score. Furthermore, based on the definition in the original study [7], patients were categorized into risk groups as follows: low-risk, 0–3 points, mild risk, 4 points, moderate risk, 5 points, and high-risk, 6–9 points. To evaluate the calibration performance, we visually compared the observed outcome and mean probability of in-hospital mortality by using a calibration plot with locally weighted scatterplot smoothing by the score and a bar plot by the risk groups. Moreover, we calculated the other performances using the following indices: Nagelkerke R2 value, calibration slope, intercept, and Brier Score, which are indices of the accuracy of the prediction [14, 24]. Furthermore, we evaluated the clinical utility of the 5A score model by using net-benefit and decision-curve analysis compared to the reference as age, body temperature and “all treatment strategy” [25]. All treatment strategy is a concept of treatment policy in decision-curve analysis, which describes the net-benefit if all the patients are managed as test positive regardless of the prediction [25]. Statistical analyses were performed using R (version 4.1.2).
Results
Participant characteristics
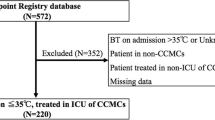
Among the 1363 patients registered in the database, 1139 patients with accidental hypothermia were included for the analysis (Fig. 1). The median [IQR] age was 79 [68–87] years, 625 (54.9%) participants were male. Almost half of the patients (54%, 610/1139) were admitted to the ICU. In-hospital mortality was reported for 271 (23.8%) participants. Other participant characteristics and in-hospital data are described in Table 2 and Additional file 1: eAppendix 6.
Model performance
To evaluate the discriminative performance of the 5A score using the estimated albumin value, we found that the C-statistic [95% CI] was 0.736 [0.699–0.772]. For calibration, the predicted probability and actual observation by score are illustrated (Fig. 2, left). Furthermore, the predicted probability [95% CI] and actual observation by risk groups were as follows: Predicted probability, low risk 7% (5.4–8.6), mild 19.1% (17.4–20.8), moderate 33.2% (29.9–36.5), and high risk 61.9% (55.9–67.9); observation, low risk 12.4% (60/483), mild 17.7% (59/334), moderate 32.6% (63/193), and high risk 69% (89/129), as shown in Fig. 2 (right panel). Although the prediction was slightly underestimated in the patients in the low-risk and high-risk groups, the model was well calibrated. Other details of model performance are specified in Additional file 1: eAppendix7, 8. In the decision-curve analysis (Fig. 3), the net-benefit of 5A score model is visually higher than that of age, BT, or all treatment strategy, which suggests the clinical utility of the 5A score model. In the sensitivity analysis, the robustness of the results was confirmed, which is described in Additional file 1: eAppendix9 and 10.
Decision-curve analysis. BT body temperature. The net-benefit of 5A score is higher than age, BT, “all treatment strategy” and “none” in almost all range of threshold probability. All treatment strategy is a concept of treatment policy in decision-curve analysis, which describes the net-benefit if all the patients are managed as test positive regardless of the prediction. None is also a treatment policy which describes the net-benefit if all the patients are managed as test negative regardless of the prediction
Discussion
Key findings
This multicenter observational study conducted the external validation of the 5A score for predicting the in-hospital mortality for the patients with accidental hypothermia. The results indicated that the 5A score using the estimated albumin value is well calibrated and has clinical utility. Thus, the 5A score could facilitate decision-making regarding the treatment strategy.
Strengths
The 5A score has several strengths. First, this 5A score is the first externally validated prediction model for use in patients with accidental hypothermia. Previously, some reports have indicated methods to predict the clinical outcome for the patients with accidental hypothermia. For example, the “ICE score” and the “HOPE score” were reported for predicting the prognosis of patients with cardiac arrest following accidental hypothermia [11, 12]. However, these scores were developed on the basis of a literature review of case reports and was affected by both publication and selection bias. Furthermore, another prediction model for accidental hypothermia using coagulopathy and the level of consciousness was reported as a prediction tool, but was derived from a small sample (192 patients with accidental hypothermia) and had a risk of overfitting and less reproducibility [9]. Moreover, these scores were not evaluated using bootstrapping for internal validation or with a separate dataset for external validation; therefore, there are serious concerns with regard to the applicability of the model in the real-world clinical settings. However, with regard to the 5A score, internal validation by a bootstrapping procedure and both internal–external validation have already been evaluated previously [7]. Moreover, this study undertook external validation using a completely different cohort from that used for the derivation data. Therefore, the predictive performance of the 5A score may have adequate reproducibility and generalizability to similar populations.
Second, the 5A score constitutes a simple and easy system that may be helpful to rapidly predict the in-hospital mortality in the ED. For critically ill patients, some scores to evaluate multiorgan injury such as the Sequential Organ Failure Assessment Score (SOFA) and Acute Physiology and Chronic Health Evaluation (APACHE) 2 scores are widely accepted and are used to assess the severity. Especially, the SOFA score was utilized in the assessment of patients with accidental hypothermia [8, 10]. However, these scores comprise multiple factors of organ injury as well as many predictive variables, and some of these parameters are unavailable in the ED after hospital arrival. Thus, the above-mentioned scores may be unsuitable for predicting mortality in the ED. Furthermore, when using APACHE2 score or other risk-assessment tools, the predicted mortality cannot be calculated without using a complicated equation. In contrast, physicians in the ED can easily and rapidly use the 5A score to predict mortality.
Third, this study suggested the clinical utility of the 5A score model using decision-curve analysis. The clinical utility of the prediction model is described as the net-benefit, which is the difference between the number of correctly predicted cases and wrongly predicted cases, weighted by the values [27]. For evaluating the prediction model, not only predictive performance, but also clinical utility should be assessed [28]. However, the clinical utility has not been evaluated for the previously reported prediction models used for accidental hypothermia [11, 12, 26]. In contrast, in this study, we evaluated the clinical utility using the decision-curve analysis, which indicated that the 5A score may have a higher net-benefit than BT and age. Based on these strong points, we believe that the 5A score model is an easy-to-use valuable tool in the ED for predicting mortality and facilitating decision-making, with high reproducibility and generalizability.
Clinical implication
We believe that the 5A score can enable clinicians to rapidly predict the in-hospital mortality risk of patients with accidental hypothermia, and thus provide patients and their families with information about their prognosis to enable the selection of the appropriate treatment strategy based on their values. In urban areas, most accidental hypothermia patients are older adults, and we do not think that all of the patients would want to avail invasive and aggressive life-sustaining treatment. If there is no established prognosis prediction model, physicians would be apprehensive about their therapeutic decision-making with regard to the treatment. Furthermore, in some cases, the above-mentioned deficit might lead to an unfavorable situation wherein an older adult patient who is facing imminent death might be treated too invasively, or patients with good survival prospects might undergo early withdrawal of treatment. If an option for the prediction of the prognosis is available, this can be valuable for discussing the treatment strategy with the patients or their family. For example, for patients in the low-risk group (≤ 3 points) who are expected to survive, aggressive treatment might be acceptable even if the patient is an older adult. On the other hand, for individuals in the severe-risk group (≥ 6 points), prediction of prognosis can be an important information to discuss about treatment strategy with the patient’s relatives. Therefore, the 5A score can provide valuable information to facilitate rational decision-making considering preference and values.
Limitation
This study had several limitations. First, the serum albumin value, a component of the 5A score, was not measured in this database and it was imputed by estimated value. Even though the robustness of the main results was confirmed through the sensitivity analysis and weight of albumin value in 5A score was not so high (one-nineth), the lack of an objectively measured albumin level is the most important limitation of this study; thus, it should be considered while interpreting the results. Second, although clinical information was prospectively collected in this database, inaccurate data collection or missing data might confer a risk of bias. Especially, in some of the patients, body temperature was measured at the axilla, and it might not exactly reflect the core body temperature in some circumstances. Further, assessing the ADL was not completely objective and it might also contribute towards the risk of a measurement bias. Third, the treatment for the patients was decided by the physician in charge and it may be based on the clinical information including age, ADL and so on, which might be a self-fulfilling prophecy bias. Fourth, the prediction was slightly underestimated among patients in the low-risk and high-risk groups, which may have been caused by overfitting of the model. Fifth, this database was compiled from data derived from more than 89 hospitals nationwide, and generalizability of the results to Japan may be confirmed; however, it is unclear whether this model would be applicable to other settings and in other countries. Lastly, the extent to which this score clinically influences the treatment strategy and actual patient outcomes remains unclear. Especially, it is not appropriate to jump to conclusion of withdrawal of intensive care only based on the 5A score, because even for the patients in the high-risk group, some of the patients (31%) were able to obtain survival discharge in this study. We believe that treatment strategy should be decided comprehensively, not only based on the 5A score, but also based on other clinical information, medical resources, and values of the patients. To eliminate such limitations, further research or updating the model would be necessary.
Conclusion
In this study, the 5A score model using estimated albumin value was externally validated in a completely independent dataset from that used for the model development. The 5A score is potentially helpful to predict the mortality risk and may be one of the valuable information for discussing the treatment strategy with patients and their family members.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available because it is not approved by the Ethics Committee. Editors are available from the corresponding author on reasonable request.
Change history
09 June 2022
A Correction to this paper has been published: https://doi.org/10.1186/s40560-022-00617-4
Abbreviations
- ED:
-
Emergency department
- BT:
-
Body temperature
- ADL:
-
Activities of daily living
- JAAM:
-
Japanese Association for Acute Medicine
- SOFA score:
-
Sequential Organ Failure Assessment Score
- APACHE2 score:
-
Acute Physiology and Chronic Health Evaluation 2 Scores
References
Brown DJ, Brugger H, Boyd J, Paal P. Accidental hypothermia. N Engl J Med. 2012;367(20):1930–8.
Matsuyama T, Morita S, Ehara N, Miyamae N, Okada Y, Jo T, Sumida Y, Okada N, Watanabe M, Nozawa M, et al. Characteristics and outcomes of accidental hypothermia in Japan: the J-Point registry. Emerg Med J. 2018;35(11):659–66.
Takauji S, Hifumi T, Saijo Y, Yokobori S, Kanda J, Kondo Y, Hayashida K, Shimazaki J, Moriya T, Yagi M, et al. Accidental hypothermia: characteristics, outcomes, and prognostic factors—a nationwide observational study in Japan (Hypothermia study 2018 and 2019). Acute Med Surg. 2021;8(1):e694.
Fujimoto Y, Matsuyama T, Morita S, Ehara N, Miyamae N, Okada Y, Jo T, Sumida Y, Okada N, Watanabe M. Indoor versus outdoor occurrence in mortality of accidental hypothermia in Japan: The J-Point Registry. Therap Hypothermia Temp Manag. 2019. https://doi.org/10.1089/ther.2019.0017.
Morita S, Matsuyama T, Ehara N, Miyamae N, Okada Y, Jo T, Sumida Y, Okada N, Watanabe M, Nozawa M, et al. Prevalence and outcomes of accidental hypothermia among elderly patients in Japan: data from the J-Point registry. Geriatr Gerontol Int. 2018;18(10):1427–32.
Gill TM. The central role of prognosis in clinical decision making. JAMA. 2012;307(2):199–200.
Okada Y, Matsuyama T, Morita S, Ehara N, Miyamae N, Jo T, Sumida Y, Okada N, Watanabe M, Nozawa M, et al. The development and validation of a “5A” severity scale for predicting in-hospital mortality after accidental hypothermia from J-point registry data. J Intensive Care. 2019;7:27.
Okada Y, Matsuyama T, Morita S, Ehara N, Miyamae N, Jo T, Sumida Y, Okada N, Watanabe M, Nozawa M, et al. Machine learning-based prediction models for accidental hypothermia patients. J Intensive Care. 2021;9(1):6.
Uemura T, Kimura A, Matsuda W, Sasaki R, Kobayashi K. Derivation of a model to predict mortality in urban patients with accidental hypothermia: a retrospective observational study. Acute Med Surg. 2019;7(1):e478–e478.
Kandori K, Okada Y, Matsuyama T, Morita S, Ehara N, Miyamae N, Jo T, Sumida Y, Okada N, Watanabe M, et al. Prognostic ability of the sequential organ failure assessment score in accidental hypothermia: a multi-institutional retrospective cohort study. Scand J Trauma Resusc Emerg Med. 2019;27(1):103.
Pasquier M, Hugli O, Paal P, Darocha T, Blancher M, Husby P, Silfvast T, Carron PN, Rousson V. Hypothermia outcome prediction after extracorporeal life support for hypothermic cardiac arrest patients: The HOPE score. Resuscitation. 2018;126:58–64.
Saczkowski RS, Brown DJA, Abu-Laban RB, Fradet G, Schulze CJ, Kuzak ND. Prediction and risk stratification of survival in accidental hypothermia requiring extracorporeal life support: an individual patient data meta-analysis. Resuscitation. 2018;127:51–7.
Okada Y, Kiguchi T, Irisawa T, Yoshiya K, Yamada T, Hayakawa K, Noguchi K, Nishimura T, Ishibe T, Yagi Y, et al. Predictive accuracy of biomarkers for survival among cardiac arrest patients with hypothermia: a prospective observational cohort study in Japan. Scand J Trauma Resusc Emerg Med. 2020;28(1):75.
Steyerberg EW. Clinical prediction models: a practical approach to development, validation, and updating. hardcover. New York: Springer; 2009.
Ramspek CL, Jager KJ, Dekker FW, Zoccali C, van Diepen M. External validation of prognostic models: what, why, how, when and where? Clin Kidney J. 2021;14(1):49–58.
Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ. 2015;350:g7594.
Collins GS, Ogundimu EO, Altman DG. Sample size considerations for the external validation of a multivariable prognostic model: a resampling study. Stat Med. 2016;35(2):214–26.
Stekhoven DJ, Bühlmann P. MissForest—non-parametric missing value imputation for mixed-type data. Bioinformatics. 2012;28(1):112–8.
James MT, Zhang J, Lyon AW, Hemmelgarn BR. Derivation and internal validation of an equation for albumin-adjusted calcium. BMC Clin Pathol. 2008;8:12–12.
Thambiah S-C. Derivation and Internal Validation of an Equation for Albumin-adjusted Calcium at a Tertiary Hospital in Selangor, Malaysia. Malays J Med Health Sci. 2020:16–25.
Davies SL, Hill C, Bailey LM, Davison AS, Milan AM. The impact of calcium assay change on a local adjusted calcium equation. Ann Clin Biochem. 2015;53(2):292–4.
Pawade YR, Ghangale SS, Dahake HS. Albumin-adjusted calcium: Are previously published regression equations reliable for your laboratory?—A pilot study. Int J Med Sci Public Health. 2013;2:217.
Ariffin ZAM, Jamaluddin FA. Albumin adjusted calcium: study in a tertiary care hospital. Malays J Pathol. 2020;42(3):395–400.
Harrell JFE. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis, vol. pbk. New York: Springer; 2010.
Vickers AJ, Van Calster B, Steyerberg EW. Net benefit approaches to the evaluation of prediction models, molecular markers, and diagnostic tests. BMJ. 2016;352:i6.
Uemura T, Kimura A, Matsuda W, Sasaki R, Kobayashi K. Derivation of a model to predict mortality in urban patients with accidental hypothermia: a retrospective observational study. Acute Med Surg. 2020;7(1):e478.
Vickers AJ, van Calster B, Steyerberg EW. A simple, step-by-step guide to interpreting decision curve analysis. Diagn Progn Res. 2019;3(1):18.
Steyerberg EW, Vergouwe Y. Towards better clinical prediction models: seven steps for development and an ABCD for validation. Eur Heart J. 2014;35(29):1925–31.
Acknowledgements
We appreciate the members of the participating hospitals for data collection.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceptualization: YO. Data curation: ST, TM, JK, SY. Formal analysis: YO. Writing—original draft: YO. Writing—review and editing: ST, TM, JK, SY. Supervision: SY. All authors interpreted the data, critically revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Review Board of Teikyo University Hospital, Japan (Approval No: 17-090-2), and the ethics boards of each participating hospital listed in Additional file 1: eAppendix2. The requirement for informed consent was waived because this study was a secondary analysis of anonymized data provided by the Japan Association of Acute Medicine Heatstroke and Hypothermia Surveillance Committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: the Figure 2 was updated.
Supplementary Information
Additional file 1
: eAppendix1. 5A score model. eAppendix2. List of hospitals participating in the database. eAppendix3. Detail of the variables. eAppendix4. Estimation of the Albumin value and sensitivity analysis. eAppendix5. Missing of the variables. eAppendix6. Other details of patient characteristics. eAppendix7. Performance of 5A score model. eAppendix8. Predicted and Observed probability. eAppendix9. Results of sensitivity Analysis. eAppendix10. Results of Sensitivity Analysis using worst-case scenario.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Okada, Y., Matsuyama, T., Hayashida, K. et al. External validation of 5A score model for predicting in-hospital mortality among the accidental hypothermia patients: JAAM-Hypothermia study 2018–2019 secondary analysis. j intensive care 10, 24 (2022). https://doi.org/10.1186/s40560-022-00616-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40560-022-00616-5