Abstract
Background
Medication-related problems (MRPs) contribute significantly to preventable patient harm and global healthcare expenditure. Vulnerable populations, including Indigenous Australians (please note that the use of the term ‘Indigenous’ in this paper includes all Aboriginal and Torres Strait Islander people and acknowledges their rich traditions and heterogenous cultures.) and people living with severe and persistent mental illness (SPMI), may be at increased risk of MRPs. Pharmacist-led medication reviews can identify MRPs for targeted action.
Objective
To characterize MRPs identified and recommendations made by community pharmacists during medication reviews conducted with Indigenous Australians and people living with SPMI.
Methods
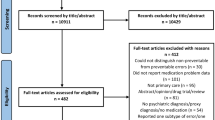
Participants were recruited through two Australian trials testing the feasibility and/or effectiveness of novel community pharmacist-led interventions, the Indigenous Medication Review Service (IMeRSe) feasibility study (June 2018–July 2019) and Bridging the Gap between Physical and Mental Illness in Community Pharmacy (PharMIbridge) randomized controlled trial (September 2020–December 2021). Trained community pharmacists conducted medication reviews responsive to the cultural and health needs of participants. MRPs, MRP severity and pharmacist recommendations were documented and classified using an established classification system (DOCUMENT). MRP severity was assessed by pharmacists and an independent assessor. Data were analysed descriptively, and paired t-tests were used to compare severity ratings.
Results
Pharmacists identified 795 MRPs with 411 participants across both trials (n = 255 IMeRSe, n = 156 PharMIbridge). Non-adherence to medication was the most common (n = 157, 25.1%) and second-most common (n = 25, 14.7%) MRP in IMeRSe and PharMIbridge, respectively. Undertreatment was the second-most common MRP in the sample of Indigenous Australians (n = 139, 22.2%), and reports of toxicity/adverse reactions were most common in people living with SPMI (n = 41, 24.1%). A change in pharmacotherapy was the most frequent recommendation made by pharmacists (40.2% and 55.0% in IMeRSe and PharMIbridge, respectively). Severity ratings varied, with the majority being ‘Mild’ or ‘Moderate’ in both groups. Significant differences were found in the severity rating assigned by trial pharmacists and the independent assessor.
Conclusions
Community pharmacists identified a range of MRPs experienced by two at-risk populations, most commonly non-adherence and toxicity or adverse reactions, when conducting medication reviews and proposed diverse strategies to manage these, frequently recommending a change in pharmacotherapy. These findings highlight the opportunity for more targeted approaches to identifying and managing MRPs in primary care and tailored community pharmacist-led interventions may be of value in this space.
Trail Registration: Australian and New Zealand Clinical Trial Registry records (IMeRSe ACTRN12618000188235 registered 06/02/2018 & PharMIbridge ACTRN12620000577910 registered 18/05/2020).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Medication (drug)-related problems (MRPs) contribute significantly to morbidity, hospitalization, and subsequent healthcare expenditure around the world [1]. MRPs have been defined as “an event or circumstance involving drug therapy that actually or potentially interferes with desired health outcomes” [2] and may occur at any stage of the medication-use process, from prescribing, to dispensing and use by consumers. Although definitions and classifications of MRPs vary, examples include adverse drug reactions, medication errors, and adverse drug events [3]. Factors such as polypharmacy, older age, or comorbid conditions contribute to risk of MRPs [4]. It is estimated that anywhere up to a median of 12.1% of all MRPs result in hospitalization [4] and contribute significantly to preventable patient harm [5]. In Australia alone, an estimated 250,000 hospital admissions annually are due to MRPs which costs the health care system (AUD) 1.4 billion dollars [6].
As medication experts, pharmacists have a critical role in the identification and management of MRPs [7]. Medication reviews, a structured evaluation of medications to optimize medication use and health outcomes [8], are an example of a pharmacist-led intervention with the intention of reducing the number and impact of MRPs experienced by consumers [8, 9]. Although outcomes of medication reviews have varied [10, 11], they form a routine part of community pharmacy practice in many countries [12,13,14,15]. In Australia, pharmacists can provide several government-funded medication reviews to eligible consumers. These include in-depth medication management reviews intended to be conducted in the consumer’s place of residence (Home Medicines Review and Residential Medication Management Review) and brief in-pharmacy medication reviews (Diabetes MedsCheck and MedsCheck) to eligible services [16,17,18].
Certain populations may also be at greater risk of experiencing MRPs which may result in negative health outcomes. For example, Indigenous AustraliansFootnote 1 may be at increased risk of experiencing MRPs [19]. Multimorbid illnesses, poor health literacy and lack of access to culturally appropriate information sources [20, 21] may contribute to the risk of unidentified MRPs. Furthermore, Indigenous Australians report barriers to accessing existing medication review services [22] and these services may not meet the health and cultural needs of this group. Another at-risk and underserved population are people living with severe and persistent mental illness (SPMI),Footnote 2 which includes conditions such as schizophrenia, bipolar disorder, and major depression [23]. People living with SPMI have been identified to have increased risk and high incidence rates of MRPs due to numerous reasons, including high prevalence of poorly managed physical illnesses and the adverse effects associated with psychotropic (e.g. antipsychotics) medication use [24,25,26]. Lack of training and confidence in caring for people with mental illness [27] as well as stigmatizing attitudes held by healthcare professionals towards this group [28] may generate barriers to access to, and provision of, existing medication review services.
In recognition of the health needs and access barriers experienced by these two populations, two novel community pharmacist-delivered interventions, which included medication review as a component of the intervention, were trialed in Australia. These interventions were the Indigenous Medication Review Service (IMeRSe), trialed in the IMeRSe feasibility study [29], and the Bridging the Gap between Physical and Mental Illness in Community Pharmacy (PharMIbridge) intervention, trialed in the PharMIbridge randomized controlled trial (RCT) [30].
Given the increased risk of MRPs and potentially unmet needs of these two populations, the primary aim of the current study was to examine these two populations as case studies to characterize the MRPs identified and subsequent recommendations made by community pharmacists during medication reviews (interventions) conducted as part of the IMeRSe feasibility study and the PharMIbridge RCT. A secondary aim was to examine the severity (clinical significance) rating of MRPs by trial pharmacists and an independent accredited pharmacist.
Methods
Data presented in this paper were collected as part of the IMeRSe feasibility study and the PharMIbridge RCT. Further information on the eligibility criteria, interventions, and methods can be obtained from the respective published protocols [29, 30] and the Australian and New Zealand Clinical Trial Registry records (ACTRN12618000188235 and ACTRN12620000577910, respectively). Other relevant findings arising from both trials will be published elsewhere.
Ethical approval
The IMeRSe feasibility study and PharMIbridge RCT received ethical approval from the Griffith University Human Research Ethics Committee (HREC/2018/251 and HREC/2019/473, respectively). Written informed consent was obtained from all consumer participants.
Study design and setting
IMeRSe feasibility study
The IMeRSe feasibility study developed and evaluated a culturally responsive medication management service, which was delivered by community pharmacists in collaboration with Aboriginal Health Service (AHS) staff. During the trial, 291 Aboriginal and Torres Strait Islander participants aged 18 years and over, with chronic conditions and at-risk of MRPs (full eligibility criteria available elsewhere [29]), were recruited from nine Aboriginal Health Services across three Australian jurisdictions (Northern Territory, Queensland and New South Wales). Pharmacists from 23 community pharmacies associated with the AHSs and AHS staff completed online modules and attended a one-day face-to-face training workshop prior to delivering the intervention. Pharmacists were also supported by mentors throughout the trial [31]. Training included two case studies with recorded vignettes which guided pharmacists through the trial procedures, including a strengths-based approach to medication review. Data from 255 consumer participants who had completed the baseline questionnaire and the intervention (called a Medicines Talk; see “IMeRSe feasibility study”) with a trained community pharmacist, were analysed.
PharMIbridge RCT
The PharMIbridge RCT was conducted in 51 community pharmacies across four Australian regions (Australian Capital Territory, Hunter New England, Northern Sydney, and regional Victoria). Recruited community pharmacies were randomized into the intervention (IG) or comparator group. Consumers aged 16 years of age and over, living with a self-reported SPMI and taking at least one antipsychotic or mood-stabilizer medication were recruited from IG community pharmacies (full eligibility criteria available elsewhere [30]). Pharmacists and pharmacy support staff from IG pharmacies attended a two-day face-to-face training workshop prior to delivering the intervention [32]. The training included a case study with recorded vignettes about a consumer experiencing MRPs as well as a presentation on psychopharmacology and other relevant topics including physical health issues and motivational interviewing. This paper reports on IG data only, from 156 consumer participants who completed the baseline survey and received the intervention (called Initial Health Review; see “PharMIbridge RCT”) within 25 community pharmacies.
Data collection
IMeRSe feasibility study
Data collection occurred from June 2018–July 2019. Consumer participants completed an electronic or paper baseline questionnaire with a study coordinator from the AHS and proceeded to the Medicines Talk during which the pharmacist reviewed current medications, identified potential MRPs and other issues of concern, and facilitated goal setting to improve their general health. The intervention was intended to be holistic and was based on the Stay Strong app [33], a resource culturally adapted for Indigenous people. An Aboriginal Health Worker (AHW) or other AHS staff coordinated the Medicines Talk and any follow-up services (at an interval determined by both parties). The Medicines Talk could include the participant, an AHW, and/or family members according to participant preference.
Demographic and health characteristics including age, gender, cultural identity, and chronic conditions were obtained. A research-specific module was developed in community pharmacy clinical practice software (GuildCare NG™) to collect and document the Medicines Talk, including information on current medications, MRPs and associated recommendations or pharmacist action/s. A Medicines Report was subsequently generated and made available to the nominated General Practitioner (GP) through the module for further review and action. Service coordination was conducted by the AHS staff member within this bespoke shared online module.
PharMIbridge RCT
Data collection occurred from September 2020–December 2021. Similar to IMeRSe, an electronic baseline survey was used to capture participant demographic details and responses to numerous validated instruments encompassing general health, medication adherence, mental wellbeing, physical wellbeing, and substance use, among others [30]. As part of the Initial Health Review, consumers worked with pharmacists to review key baseline survey results, identify any potentially relevant issues (including MRPs) and set corresponding goals to address these issues. Although the intervention was intended to be holistic, with medication review forming a component of the intervention, emphasis was placed on physical health and wellbeing. Further instruments were made available to pharmacists to help with issue identification, including the My Medicines and Me Questionnaire (M3Q) which can assist in the detection of side-effects from psychotropic medication use [34].
Following the Initial Health Review, consumer participants could meet with pharmacists for Follow-Up services (at an interval determined by both parties) with a Final Health Review scheduled 6 months after the Initial Health Review. New and previously unidentified MRPs were documented during the Follow-Ups and Final Health Review. Issues and associated recommendations could be shared with a nominated healthcare professional (usually a GP) following any service. Similar to IMeRSe, documentation occurred in a bespoke PharMIbridge research module built into GuildCare NG™.
DOCUMENT framework and severity rating
When a MRP was identified, pharmacists in both trials were required to classify the MRP and the potential severity of the MRP using the validated Australian DOCUMENT framework [35]. Although other classification systems exist, including the Pharmaceutical Care Network Europe (PCNE) system [2], DOCUMENT (which was informed by the PCNE system [35]) was selected as it was designed in Australia and used in a previously funded Australian professional pharmacy service [36, 37]. The DOCUMENT framework broadly classifies MRPs into eight categories: ‘Drug selection’, ‘Over or underdose’, ‘Compliance’, ‘Undertreated’, ‘Monitoring’, ‘Education or information’, ‘Not classifiable’, and ‘Toxicity or adverse reaction’. All categories except ‘Not classifiable’, have further sub-classifications. Severity of the potential impact of the MRPs if not resolved (i.e. clinical significance) was classified using five categories, ranging from ‘Nil’ to ‘High’, coded from 0 to 4, respectively [35]. Full descriptors of each of the severity classifications are available in Additional file 1: Table S1. Free-text fields were available for pharmacists to describe MRPs and associated recommendations. In IMeRSe, free-text recommendations were coded into an adapted version of DOCUMENT by research team members, whereas PharMIbridge pharmacists were asked to self-select the appropriate recommendation codes using DOCUMENT. The adapted version used in IMeRSe included an additional category of ‘Lifestyle recommendation’ which was not included in the categories in PharMIbridge. The severity rating of MRPs was also not documented for a proportion of the MRPs (n = 271, 43.4%) in the IMeRSe feasibility study as the feature was not functional in the Medicines Talk module until February 2019.
Independent coding of severity rating
The severity of MRPs identified in IMeRSe and PharMIbridge were independently coded by one author who is an accredited consultant pharmacist in Australia with significant experience conducting medication reviews. The independent coder used notes and medication lists created by pharmacists during the medication review and other clinical documentation such as shared health summaries (where available) to independently assign a severity classification to each of the documented MRPs.
Data cleaning and analysis
Prior to analysis, data were exported to Microsoft Excel® (Microsoft Corp, Redmond, USA) for review. Data were screened by a member of the research team to ensure unrelated issues had not been incorrectly coded as MRPs by pharmacists. Where it was clear that an issue was not an MRP, such as those relating to exercise or interpersonal relationships, it was excluded from the analysis. A secondary sample (10%) was screened by another author as a quality check. Descriptive analyses were performed on participant characteristics and details of the identified MRPs including classifications, severity ratings as well as pharmacists’ recommendations. Results are presented separately for the two trial samples. Mean (standard deviation [SD]) and median (interquartile range [IQR]) were reported for continuous variables, whereas number (percentage) was reported for categorical variables. To compare the mean severity ratings from the community pharmacists and the independent coder, paired t-tests were used. The significance level was set at p-value less than 0.05 (two-sided).
Results
A total of 411 consumer participants (n = 255 IMeRSe, n = 156 PharMIbridge) were screened for MRPs by trained community pharmacists, with 795 MRPs identified and classified using DOCUMENT. The large majority (n = 625) of these MRPs were identified in the IMeRSe feasibility study (rate of 2.45 MRPs per consumer participant) as compared to 170 MRPs identified in the PharMIbridge RCT (rate of 1.09 MRPs per consumer participant). Non-MRPs made up the remaining 137 and 474 issues documented in IMeRSe and PharMIbridge, respectively and were not included in the analysis presented in this paper. No discrepancies were found between coders in the 10% quality check.
Participant characteristics
Consumer participant characteristics are outlined in Table 1. Compared to the PharMIbridge population, the consumer participants in IMeRSe were older (average age of 60.0 years vs. 48.1 years), more likely to identify as female (62.8% vs. 55.2%), more likely to reside in a rural/remote/non-metropolitan region (76.9% vs. 44.2%) and used a greater number of medications (median 7 vs. 6). Consumer participants in IMeRSe lived with a median of six self-reported chronic conditions (including mental illness diagnoses), whereas PharMIbridge consumer participants reported living with a median of one chronic condition in addition to their mental illness(es).
Classification of MRPs
Classification of the 795 MRPs identified in IMeRSe and PharMIbridge is shown in Table 2. Of the 625 MRPs experienced by 255 Indigenous Australians in IMeRSe, pharmacists commonly classified MRPs as ‘Compliance’ (Adherence) (25.1%) followed by ‘Undertreated’ (22.2%), with ‘Toxicity or adverse reaction’ being the least common (5.1%). In contrast, of the 170 MRPs identified from 156 people living with SPMI in PharMIbridge, pharmacists most frequently classified the MRPs as ‘Toxicity or adverse reaction’ (24.1%) followed by ‘Compliance’ (14.7%), with ‘Education or information’ being the least common (8.2%). Examples of MRPs from each of the DOCUMENT categories from both trials can be found in Additional file 1: Table S2.
Severity of MRPs
Pharmacists in IMeRSe commonly rated the 354 MRPs that underwent severity classification (post-February 2019) as ‘Moderate’ (39.6%) or ‘High’ (28.0%). PharMIbridge pharmacists most frequently rated the severity of 170 MRPs as ‘Mild’ (47.7%) and ‘Moderate’ (32.9%), with ‘High’ less frequently applied (8.8%). The distribution of ratings across categories can be seen in Table 3. Examples of MRPs from each of the severity rantings from both trials can be found in Additional file 1: Table S3.
The independent consultant pharmacist reviewed pharmacist documented MRPs with pharmacist severity ratings (n = 354). The independent pharmacist coded the MRPs (0 = lowest severity rating and 4 = highest severity rating) as less severe than the community pharmacists in the IMeRSe sample, with a mean rating of 2.1 (SD 1.0) vs 2.8 (SD 1.0) (t(353) = 11.4, p < 0.001), and coded MRPs as more severe than the community pharmacists in the PharMIbridge sample, with a mean rating of 2.6 (SD 0.7) vs. 2.4 (SD 0.8) (t(169) = 2.7, p = 0.008) (Table 3).
Pharmacist recommendations for identified MRPs
Pharmacists in both studies provided recommendation(s) to resolve or manage identified MRPs (see Tables 4, 5). A ‘Change in pharmacotherapy’ was the most common recommendation in both populations, making up 40.2% of 833 recommendations in IMeRSe and 55.0% of 278 in PharMIbridge, followed by ‘Monitoring’ in IMeRSe (19.3%) and ‘Referral to other services’ in PharMIbridge (27.7%). ‘No recommendation necessary’ was selected for three MRPs in PharMIbridge.
Discussion
The current study adds to the existing body of literature examining MRPs identified by pharmacists during medication reviews by presenting a parallel case study of two vulnerable and underserved populations. This work describes the numbers, types, and severity of MRPs identified in these populations using an established Australian classification system, as well as the recommendations made by pharmacists to address these MRPs. Adherence issues, undertreatment, and toxicity and adverse reactions were commonly identified in both populations, demonstrating priority areas to be addressed in these populations.
The DOCUMENT classification system was used to classify MRPs by IMeRSe and PharMIbridge pharmacists, enabling descriptive cross-comparison of the MRPs reported in two at-risk populations. ‘Compliance’ was the most and second-most common MRP identified during the medication reviews with IMeRSe and PharMIbridge consumer participants, respectively. Although there is insufficient evidence to demonstrate whether there is a significant difference in medication adherence between Indigenous Australians and the general population, healthcare professionals believe adherence is a significant issue for Indigenous Australians [38]. Furthermore, a recent review noted a lack of empirical evidence regarding medication-taking behaviours among Indigenous Australians [39]. Further work is required to explore contributing factors to adherence issues in this population, however, these may include previously identified challenges such as misconceptions regarding medications and lack of culturally appropriate information sources [20]. Barriers to accessing care have been acknowledged by policymakers, with system level strategies implemented to improve access to medicines and healthcare for Indigenous Australians [40]. Conversely, adherence issues with psychotropic medications is well documented in people living with SPMI, with many factors, including the adverse effects of psychotropic medications such as those reported as MRPs in this current study, contributing to poor adherence [41]. Moreover, polypharmacy is known to contribute to adherence issues; both population samples were taking a median of more than 5 medications (a commonly used definition for polypharmacy [42]), which may have influenced pharmacists flagging adherence as a potential issue.
There were also differences in MRPs between the two populations. For example, ‘Undertreated’ was the second-most common MRP identified in IMeRSe, reported twice as often as in PharMIbridge. This is consistent with the findings of a study conducted in remote Australia which found that 12% of elderly Indigenous participants were potentially under-prescribed medications [19]. This further emphasizes the continuing inequity in healthcare provision for Indigenous Australians, particularly those living in rural and remote areas [43, 44]. The least common MRPs identified in the IMeRSe sample, ‘Toxicity or adverse reaction’, was conversely the most common category in PharMIbridge, making up almost a quarter of all MRPs. This is not unexpected, given the significant adverse effect profile of medications used to manage SPMI and the incidence of high-dose psychotropics and psychotropic polypharmacy in this cohort [24, 45]. This finding further highlights the need for screening for, and managing, MRPs in this population. The inclusion of the M3Q tool [34], which is readily available for pharmacists to access [46], in the Initial Health Review may have facilitated further discussion with consumer participants about medication related adverse effects compared to other types of MRPs. Regardless, the identification of numerous MRPs, irrespective of type, across both populations indicates the importance of timely access to services which are tailored to the needs of individuals.
When comparing the collective study results to the PROMISe trials, which piloted, validated, and refined the DOCUMENT system in a general population, differences can be seen in the nature of the MRPs reported. In PROMISe, ‘Drug selection’ and ‘Education or information’ were the two most common categories identified (30.7% and 23.7%, respectively) out of 5948 identified MRPs [35]. This differs to the most common categories identified in IMeRSe and PharMIbridge, namely ‘Compliance’, ‘Undertreated’, and ‘Toxicity or adverse reaction’. This could be due to differences in trial populations, the interventions trialed, or the intended purpose. The DOCUMENT system was primarily used in the PROMISe trials to document clinical interventions made in response to dispensed prescriptions [35, 47], rather than being used to code MRPs identified during a medication review as used in IMeRSe and PharMIbridge. A study by Wang et al. which used DOCUMENT to classify MRPs identified during medication reviews with elderly ambulatory patients in China found ‘Drug selection’ and ‘Undertreated’ made up almost half of 1,188 MRPs [48]. This highlights that different populations may have specific needs and priorites and further work exploring these nuances could produce findings that are useful for clinicians and policymakers.
Most MRPs were rated as having a severity of either ‘Mild’ or ‘Moderate’ (Additional file 1: Supplementary table i), together making up 61.9% and 80.6% of severity ratings in IMeRSe and PharMIbridge, respectively. This indicates that pharmacists identified MRPs that, when addressed, would have improved compliance, or alleviated a minor symptom, or prevented a doctor visit. Wang et al. similarly classified 86% of MRPs identified among elderly ambulatory patients in these categories [48]. However, pharmacists in IMeRSe rated more than a quarter of MRPs as ‘High’ severity, indicating that they believed addressing the MRP prevented a hospital visit or referred participants to hospital. These findings highlight that identified MRPs could have potentially had a range of clinical outcomes if not identified and that there is room for new opportunities in primary care to identify and manage MRPs in these populations, to minimize serious sequelae.
In addition to examining the types and severity of MRPs, it is necessary to consider the implementation and use of the DOCUMENT classification system itself. During the validation process of DOCUMENT, a “moderate” level of agreement was found between raters, indicating that there was some inconsistency in classification of MRPs [35]. Similarly, differences between raters have been found in the classification of MRPs identified in medication reviews in a Norwegian study using a different classification system [49]. The potential for disagreement or misclassification must be considered when interpreting the results of the current study as independent coding and review of the assigned categories was not performed except for severity. Similar to IMeRSe, severity ratings made by pharmacists in the PROMISe trials were potentially over-stated [35]. However, the differences in severity ratings between the study pharmacists and the independent coder in the current study could possibly be attributed to various factors, including the information available to each at the time of coding, familiarity with the consumer and their medical and social history, and overall experience in conducting medication reviews and considering potential clinical significance of MRPs. Further training and consideration of pharmacists’ understanding of the clinical significance of MRPs should be considered. The quality of documentation of MRPs must be considered, not only to ensure accurate and clear clinical notes, but to also ensure meaningful communication regarding MRPs with other healthcare professionals, such as the prescriber. This is particularly important as referral to another professional or service was commonly recommended by pharmacists. It is essential to ensure that pharmacists are trained in clear and accurate clinical documentation.
Strengths and limitations
The current study is strengthened by classifying the identified MRPs using an established and validated classification system designed for the Australian practice setting. Key strengths of both the IMeRSe and PharMIbridge interventions included ongoing follow-ups, which may facilitate the working relationship between consumers and community pharmacists. Although the two studies are heterogenous in design and direct comparisons between the two populations cannot be made, this study highlights the needs of the two underserved and vulnerable populations which may inform the implementation of targeted training and/or services. Furthermore, eligibility criteria for consumer participants in both studies included being at-risk of MRPs; this may have resulted in increased rates of MRPs identified in these two samples. It is unknown how generalizable these two samples are to the broader populations of Indigenous Australians and people living with SPMI. The physical health focus of the PharMIbridge intervention, may have resulted in comparatively less MRPs being identified out of all the issues due to the focus of training and overall design.
It is likely that trial pharmacists had varying degrees of experience conducting medication reviews and using the DOCUMENT classification system; this may have impacted how pharmacists conducted the reviews and classified MRPs. Some pharmacists had undergone additional training to become accredited pharmacists (i.e. able to conduct Home Medicines Reviews) which may also have impacted how they conducted the medication reviews in the two studies. It is also important to acknowledge that the independent coding was conducted by a single accredited pharmacist and a panel approach to classification may have yielded different results. Lastly, outcomes for individual MRPs, such as GP acceptance rates, further healthcare use due to MRPs, and resolution of MRPs, were unable to be tracked.
Conclusion
Community pharmacists identified a range of MRPs with varying levels of severity experienced by two at-risk and underserved populations, namely Indigenous Australians and people living with SPMI, when conducting novel interventions which included medication review. Non-adherence to medication and the presence of toxicity or adverse reactions were among the most reported MRPs. Pharmacists proposed a variety of strategies to address the MRPs, most often involving a proposed change to pharmacotherapy. These findings highlight specific needs of the two populations and emphasize that there is room for more targeted approaches to identifying and managing MRPs in primary care and tailored community pharmacist-led interventions may be of value in this space.
Availability of data and materials
The datasets generated and analysed for this study are not publicly available as consent from participants was not sought to share the data more widely than for the purpose of this study. Data are not publicly available as consent for data sharing was not obtained from participants.
Notes
Please note that the use of the term ‘Indigenous’ in this paper includes all Aboriginal and Torres Strait Islander people and acknowledges their rich traditions and heterogenous cultures.
It is acknowledged that Aboriginal and Torres Strait Islander people may also live with SPMI and the authors are not suggesting these are two discrete populations. Some participants in IMeRSe lived with SPMI and some participants in PharMIbridge identified as Aboriginal or Torres Strait Islander.
References
Ernst FR, Grizzle AJ. Drug-related morbidity and mortality: updating the cost-of-illness model. J Am Pharm Assoc. 2001;41(2):192–9. https://doi.org/10.1016/s1086-5802(16)31229-3.
van Mil F, Horvat N, Westerlund T, Richling I. PCNE Classification for drug related problems V9.1 Zuidlaren: PCNE; 2020 [cited: 18 January 2023]. Available from: https://www.pcne.org/upload/files/417_PCNE_classification_V9-1_final.pdf.
Strand LM, Morley PC, Cipolle RJ, Ramsey R, Lamsam GD. Drug-related problems: their structure and function. DICP. 1990;24(11):1093–7. https://doi.org/10.1177/106002809002401114.
Al Hamid A, Ghaleb M, Aljadhey H, Aslanpour Z. A systematic review of hospitalization resulting from medicine-related problems in adult patients. BIt J Clin Pharmacol. 2014;78(2):202–17. https://doi.org/10.1111/bcp.12293.
Panagioti M, Khan K, Keers RN, Abuzour A, Phipps D, Kontopantelis E, et al. Prevalence, severity, and nature of preventable patient harm across medical care settings: systematic review and meta-analysis. BMJ. 2019;366: l4185. https://doi.org/10.1136/bmj.l4185.
Lim R, Ellett LMK, Semple S, Roughead EE. The extent of medication-related hospital admissions in Australia: a review from 1988 to 2021. Drug Saf. 2022;45(3):249–57. https://doi.org/10.1007/s40264-021-01144-1.
Dalton K, Byrne S. Role of the pharmacist in reducing healthcare costs: current insights. Integr Pharm Res Pract. 2017;6:37–46. https://doi.org/10.2147/iprp.S108047.
Griese-Mammen N, Hersberger KE, Messerli M, Leikola S, Horvat N, van Mil JWF, et al. PCNE definition of medication review: reaching agreement. Int J Clin Pharm. 2018;40(5):1199–208. https://doi.org/10.1007/s11096-018-0696-7.
Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47(3):533–43. https://doi.org/10.1093/ajhp/47.3.533.
Al-babtain B, Cheema E, Hadi MA. Impact of community-pharmacist-led medication review programmes on patient outcomes: a systematic review and meta-analysis of randomised controlled trials. Res Social Adm Pharm. 2021;18(4):2559–68. https://doi.org/10.1016/j.sapharm.2021.04.022.
Jokanovic N, Tan EC, Sudhakaran S, Kirkpatrick CM, Dooley MJ, Ryan-Atwood TE, et al. Pharmacist-led medication review in community settings: an overview of systematic reviews. Res Social Adm Pharm. 2017;13(4):661–85. https://doi.org/10.1016/j.sapharm.2016.08.005.
Bulajeva A, Labberton L, Leikola S, Pohjanoksa-Mäntylä M, Geurts M, De Gier J, et al. Medication review practices in European countries. Res Social Adm Pharm. 2014;10(5):731–40. https://doi.org/10.1016/j.sapharm.2014.02.005.
Ontario Ministry of Health. MedsCheck General Information Toronto: Ontario Ministry of Health; 2022 [cited: 1 October 2022]. Available from: https://www.health.gov.on.ca/en/pro/programs/drugs/medscheck/faq_original.aspx#30.
Stewart D, Whittlesea C, Dhital R, Newbould L, McCambridge J. Community pharmacist led medication reviews in the UK: a scoping review of the medicines use review and the new medicine service literatures. Res Social Adm Pharm. 2020;16(2):111–22. https://doi.org/10.1016/j.sapharm.2019.04.010.
Viswanathan M, Kahwati LC, Golin CE, Blalock SJ, Coker-Schwimmer E, Posey R, et al. Medication therapy management interventions in outpatient settings: a systematic review and meta-analysis. JAMA Intern Med. 2015;175(1):76–87. https://doi.org/10.1001/jamainternmed.2014.5841.
Pharmacy Programs Administrator. MedsCheck and Diabetes MedsCheck. Melbourne: Pharmacy Programs Administrator; 2022 [cited: 13 January 2023]. Available from: https://www.ppaonline.com.au/programs/medication-management-programs/medscheck-and-diabetes-medscheck.
Pharmacy Programs Administrator. Home Medicines Review Melbourne: Pharmacy Programs Administrator; 2022 [cited: 18 January 2023]. Available from: https://www.ppaonline.com.au/programs/medication-management-programs/home-medicines-review.
Pharmacy Programs Administrator. Residential Medication Management Review and Quality Use of Medicines Melbourne: Pharmacy Programs Administrator; 2022 [cited: 18 January 2023]. Available from: https://www.ppaonline.com.au/programs/medication-management-programs/residential-medication-management-review-and-quality-use-of-medicines.
Page A, Hyde Z, Smith K, Etherton-Beer C, Atkinson DN, Flicker L, et al. Potentially suboptimal prescribing of medicines for older Aboriginal Australians in remote areas. Med J Aust. 2019;211(3):119–25. https://doi.org/10.5694/mja2.50226.
Hamrosi K, Taylor SJ, Aslani P. Issues with prescribed medications in Aboriginal communities: aboriginal health workers’ perspectives. Rural Remote Health. 2006;6(2):1–13. https://doi.org/10.22605/RRH557.
Kowanko I, Crespigny Cd, Murray H, Groenkjaer M, Emden C. Better medication management for Aboriginal people with mental health disorders: a survey of providers. Aust J Rural Health. 2004;12(6):253–7. https://doi.org/10.1111/j.1440-1854.2004.00625.x.
Swain LS, Barclay L. Exploration of aboriginal and Torres Strait islander perspectives of Home medicines review. Rural Remote Health. 2015;15(1):64–76. https://doi.org/10.22605/RRH3009.
World Health Organization. Management of physical health conditions in adults with severe mental disorders (WHO Guidelines) Geneva: World Health Organization; 2018 [cited: 30 March 2022]. Available from: https://www.who.int/publications/i/item/978-92-4-155038-3.
Pillinger T, McCutcheon RA, Vano L, Mizuno Y, Arumuham A, Hindley G, et al. Comparative effects of 18 antipsychotics on metabolic function in patients with schizophrenia, predictors of metabolic dysregulation, and association with psychopathology: a systematic review and network meta-analysis. Lancet Psychiatry. 2020;7(1):64–77. https://doi.org/10.1016/s2215-0366(19)30416-x.
Bell SJ, Whitehead P, Aslani P, McLachlan AJ, Chen TF. Drug-related problems in the community setting. Clin Drug Invest. 2006;26(7):415–25. https://doi.org/10.2165/00044011-200626070-00003.
National Mental Health Commission. Equally Well Consensus Statement: Improving the physical health and wellbeing of people living with mental illness in Australia Sydney: National Mental Health Commission; 2016 [cited: 20 October 2022]. Available from: https://www.equallywell.org.au/wp-content/uploads/2018/12/Equally-Well-National-Consensus-Booklet-47537.pdf.
Wheeler A, Mey A, Kelly F, Hattingh L, Davey A. Education and training for community pharmacists in mental health practice: how to equip this workforce for the future. J Mental Health Training Educ Pract. 2014;9(3). https://doi.org/10.1108/JMHTEP-09-2013-0030.
O’Reilly C, Bell S, Kelly P, Chen T. Exploring the relationship between mental health stigma, knowledge and provision of pharmacy services for consumers with schizophrenia. Res Social Adm Pharm. 2015;11(3):e101–9. https://doi.org/10.1016/j.sapharm.2013.04.006.
Wheeler AJ, Spinks J, Kelly F, Ware RS, Vowles E, Stephens M, et al. Protocol for a feasibility study of an Indigenous Medication Review Service (IMeRSe) in Australia. BMJ Open. 2018;8(11): e026462. https://doi.org/10.1136/bmjopen-2018-026462.
Wheeler AJ, O’Reilly CL, El-Den S, Byrnes J, Ware RS, McMillan SS. Bridging the gap between physical and mental illness in community pharmacy (PharMIbridge): protocol for an Australian cluster randomised controlled trial. BMJ Open. 2020;10(7): e039983. https://doi.org/10.1136/bmjopen-2020-039983.
Wheeler AJ, Hu J, Tadakamadla SK, Hall K, Miller A, Kelly F. Development and feasibility testing of a training programme for community pharmacists to deliver a culturally responsive medication review intervention. Pilot Feasibility Stud. 2022;8(1):51. https://doi.org/10.1186/s40814-022-01006-2.
McMillan SS, El-Den S, O’Reilly CL, Roennfeldt H, Theodorus T, Chapman J, et al. A training programme for community pharmacists to support people living with severe and persistent mental illness: intervention mapping in the context of a pandemic. Health Educ J. 2022. https://doi.org/10.1177/00178969221130461.
Dingwall KM, Puszka S, Sweet M, Nagel T. “like drawing into sand”: acceptability, feasibility, and appropriateness of a new e-mental health resource for service providers working with Aboriginal and Torres Strait Islander people. Aust Psychol. 2015;50(1):60–9. https://doi.org/10.1111/ap.12100.
Ashoorian DM, Davidson RM, Rock DJ, Dragovic M, Clifford RM. Construction and validation of the My Medicines and Me Questionnaire for assessment of the self-reported side effects of psychotropic medication. Int Clin Psychopharmacol. 2015;30(4):224–9. https://doi.org/10.1097/yic.0000000000000072.
Williams M, Peterson GM, Tenni PC, Bindoff IK, Stafford AC. DOCUMENT: a system for classifying drug-related problems in community pharmacy. Int J Clin Pharm. 2012;34(1):43–52. https://doi.org/10.1007/s11096-011-9583-1.
Pharmaceutical Society of Australia. Guidelines for pharmacists performing clinical interventions. Canberra; 2018.
Pharmacy Programs Administrator. Clinical interventions program ceasing Melbourne: Pharmacy Programs Administrator; 2022 [cited: 20 January 2023]. Available from: https://www.ppaonline.com.au/ci-program-ceasing#:~:text=Under%20the%20newly%20signed%20Seventh,cease%20from%201%20July%202020.
de Dassel JL, Ralph AP, Cass A. A systematic review of adherence in Indigenous Australians: an opportunity to improve chronic condition management. BMC Health Serv Res. 2017;17(1):845. https://doi.org/10.1186/s12913-017-2794-y.
Walke E, Barclay L, Longman J. Scoping review—what do we know about Aboriginal peoples’ use of dose administration aids? Health Promot J Aust. 2022;33(S1):117–27. https://doi.org/10.1002/hpja.577.
Saxby K, Byrnes J, de New SC, Nghiem S, Petrie D. Does affirmative action reduce disparities in healthcare use by Indigenous peoples? Evidence from Australia’s Indigenous Practice Incentives Program. Health Econ. 2023. https://doi.org/10.1002/hec.4645.
Semahegn A, Torpey K, Manu A, Assefa N, Tesfaye G, Ankomah A. Psychotropic medication non-adherence and its associated factors among patients with major psychiatric disorders: a systematic review and meta-analysis. Syst Rev. 2020;9(1):17. https://doi.org/10.1186/s13643-020-1274-3.
Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):1–10. https://doi.org/10.1186/s12877-017-0621-2.
Zhao Y, You J, Wright J, Guthridge SL, Lee AH. Health inequity in the Northern Territory, Australia. Int J Equity Health. 2013;12(1):79. https://doi.org/10.1186/1475-9276-12-79.
Australian Institute of Health and Welfare. Aboriginal and Torres Strait Islander Health Performance Framework: summary report 2023 Canberra: AIHW; 2023 [cited: February 14, 2023]. Available from: https://www.indigenoushpf.gov.au/getattachment/d396ed0d-9347-4de6-8b41-ff56bf3dfa18/2023-ihpf-summary-report.pdf.
Hu J, McMillan SS, Theodoros T, Collins JC, El-Den S, O’Reilly CL, et al. Psychotropic medication use in people living with severe and persistent mental illness in the Australian community: a cross-sectional study. BMC Psychiatry. 2022;22(1):705. https://doi.org/10.1186/s12888-022-04324-0.
Ashoorian D. My Medicines & Me Questionnaire (M3Q): A side effect questionnaire for mental health medications 2014 [cited: 27 January 2023]. Available from: https://www.chiefpsychiatrist.wa.gov.au/wp-content/uploads/2016/10/M3Q_Fillable.pdf.
Williams M, Peterson GM, Tenni PC, Bindoff IK, Curtain C, Hughes J, et al. Drug-related problems detected in Australian community pharmacies: the PROMISe Trial. Ann Pharmacother. 2011;45(9):1067–76. https://doi.org/10.1345/aph.1Q138.
Wang X, Yang J, Yu X, Wang Z, Wang H, Liu L. Characterization of drug-related problems and associated factors in ambulatory patients in China. J Clin Pharm Ther. 2020;45(5):1058–65. https://doi.org/10.1111/jcpt.13161.
Granas AG, Berg C, Hjellvik V, Haukereid C, Kronstad A, Blix HS, et al. Evaluating categorisation and clinical relevance of drug-related problems in medication reviews. Pharm World Sci. 2010;32(3):394–403. https://doi.org/10.1007/s11096-010-9385-x.
Hugo Centre for Population and Migration Studies. Pharmacy accessibility in Australia Adelaide: The University of Adelaide; 2018 [cited: 27 January 2023]. Available from: https://able.adelaide.edu.au/hugo-centre/news/list/2018/10/23/pharmacy-accessibility-in-australia.
Australian Government Department of Health and Aged Care. Modified Monash Model: Australian Government; 2021 [cited: 20 January 2023]. Available from: https://www.health.gov.au/health-topics/rural-health-workforce/classifications/mmm.
Acknowledgements
The authors wish to acknowledge the Indigenous communities, consumer participants, Aboriginal Health Service staff, and community pharmacists who participated in this research. We thank all members of the project teams and the Expert Panels for their contributions. The IMeRSe study was developed in partnership with The Pharmacy Guild of Australia, the National Aboriginal Community Controlled Health Organisation (NACCHO) and Griffith University. The PharMIbridge RCT was developed in partnership with The Pharmacy Guild of Australia, the Pharmaceutical Society of Australia, Griffith University, and The University of Sydney.
Funding
The IMeRSe feasibility study and PharMIbridge RCT received funding from the Australian Government Department of Health and Aged Care (formerly the Department of Health). The researchers were independent from the funder. This article contains the opinions of the authors and does not in any way reflect the views of the Department of Health and Aged Care or the Australian Government. The funding provided must not be taken as an endorsement of the contents of this paper.
Author information
Authors and Affiliations
Contributions
Conceptualization: JC, JH, SM, COR, SED, FK, JS, AW; data curation: JC, JH, JS; formal analysis: JC, JH, SM, FK, JS, TR, AW; funding acquisition: SM, COR, SED, FK, JS, AW; investigation: JC, JH, SM, COR, SED, FK, JS, AW; methodology: JC, JH, SM, COR, SED, FK, JS, AW; writing—original draft: JC, JH; writing—review and editing: JC, JH, SM, COR, SED, FK, JS, TR, AW.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The IMeRSe feasibility study and PharMIbridge RCT received ethical approval from the Griffith University Human Research Ethics Committee (HREC/2018/251 and HREC/2019/473, respectively). Written informed consent was obtained from all consumer participants.
Consent for publication
Not applicable.
Competing interests
None to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The use of the term ‘Indigenous’ in this paper includes all Aboriginal and Torres Strait Islander people and acknowledges their rich traditions and heterogenous cultures.
Supplementary Information
Additional file 1: Table S1
. Severity descriptors as used in the PROMISe trials. Table S2. Examples of MRPs documented by pharmacists using the DOCUMENT framework. Table S3. Examples of MRPs documented by pharmacists for each of the severity classifications.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Collins, J.C., Hu, J., McMillan, S.S. et al. Medication-related problems identified by community pharmacists: a descriptive case study of two Australian populations. J of Pharm Policy and Pract 16, 133 (2023). https://doi.org/10.1186/s40545-023-00637-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40545-023-00637-x