Abstract
Background
Self-medication with antibiotics has become an important factor driving antibiotic resistance and it masks the signs and symptoms of the underlying disease and hence complicates the problem, increasing drug resistance and delaying diagnosis. This study aimed to assess the extent of self-medication practice with antibiotics and its associated factors among adult patients attending outpatient departments (OPD) at selected public Hospitals, in Addis Ababa, Ethiopia.
Methods
Facility-based cross-sectional study was employed. A systematic random sampling technique was used to include the study participants. Self-administered with structured questionnaires were applied among patients who visited outpatient departments at selected public Hospitals, in Addis Ababa. Data were entered into Epi-data version 4.6 and analyzed using SPSS version 26. Descriptive statistics such as frequencies and percentages were used for the present categorical data. The data are presented in pie charts, tables, and bar graphs. Furthermore, bivariable and multivariable binary logistic regression analyses were used to identify significant associations. Statistical significance was declared at p value < 0.05.
Results
Out of 421 respondents interviewed, 403 (95.7%) participants completed questionnaires. Among the respondents, 71% had generally practiced self-medication. Among these, 48.3% had self-medication with antibiotics, while 51.7% had used other drugs. The most commonly cited indication for self-medication practice was abdominal pain 44.9%, followed by Sore throat 21% commonly used antibiotics are amoxicillin (57%), ciprofloxacin (13%), amoxicillin/clavulanic (10%), erythromycin (8%), cotrimoxazole (7%), and doxycycline (5%).
Conclusions
Self-medication with antibiotics was common among the study participants. The prevalence of general self-medication was 71%, whereas that of self-medication with antibiotics was 48.3%. In general, the potentially dangerous effects of SMP seem to be underestimated by patients with OPD patients.
Similar content being viewed by others
Introduction
Self-medication has traditionally been characterized as using medications, or home remedies on one’s own initiative or at the suggestion of another person without first contacting a medical professional [1]. The World Health Organization (WHO), defined self-medication as the selection and use of drugs to address self-identified diseases or symptoms. Self-medication is when a person obtains and consumes a medication without seeking medical assistance, whether for diagnosis, prescription, or monitoring of one’s own therapy or medication [2].
It usually involves over-the-counter (OTC) medications, but it can also include prescription-only medications (POM, purchasing drugs by reusing or resubmitting a previous prescription, taking medications on the advice of a relative or other, or eating leftover medications already on hand at home [3]. The FDA (2006) characterizes OTCs as a sedate item promoted for use by the buyer without the intercession of a well-being care proficient in arranging to get the item. With respect to the classification of drugs, it appears that individuals do not separate between medication and OTC drugs [4].
Prescription products are medications that require a doctor’s prescription [5]. Several studies conducted in indicated that self-medication with antibiotics is quite common, varies by community and social determinants of health, and is usually accompanied by the use of unsuitable drugs [6]. In developed countries, the use of antibiotics without prescription is the second highest prevalent next to antipain [7]. Antibiotics are not available over the counter, and they require a prescription before being dispensed. Over the counter products are also available at supermarkets and other community pharmacies in various countries, including Ethiopia [8].
Inappropriate self-medication waste resources raises the risk of drug resistance and leads to major health issues such adverse drug responses, treatment failure, prescription misuse, and drug addiction [9]. Despite this, self-medication may save money on health care and time spent waiting to visit a doctor for mild diseases.
Self-medication has several detrimental effects on one’s health. It may result in incorrect self-diagnosis and a delay in receiving urgent medical care. Moreover, it may lead to ineffective dosing, polypharmacy, and hazardous drug interactions [10]. This can lead to noncompliance with a drug regimen that can result in serious outcomes such as adverse drug reactions and reduction in the quality of treatment [10]. Moreover, currently, there is a worldwide concern about the emergence of antibiotic-resistant strains of micro-organisms, which might have been highly augmented by self-medication [11].
Self-medication has been reported to be on the rise around the world and has become a public health concern [9]. People in poor countries are self-medicating with not only non-prescription but also prescription medications without supervision. Although the WHO has stressed the importance of properly teaching and controlling self-medication, its use is nevertheless widespread [12].
A number of researches on various elements of self-medication have been undertaken internationally, and the prevalence of self-medication among adult outpatients has been found to be high [13,14,15,16,17,18]. The prevalence of self-medication in Greece was 77.9% in [19], 98% in Palestine [20], 71% in India [21], and 76% in Pakistan [21]. The rates are similar in Africa: It is 99.4% in Nigeria [22], 56% in Malawi [23], 53.5% Kenya [24], 75.7% in Uganda [25] and 50% in Ethiopia [8]. Accordingly, individuals practiced self-medication for different purposes. Studies have reported that headache, fever, cough, gastrointestinal diseases, respiratory tract infections, maternal/menstrual, eye diseases, skin diseases, injury, and sexually transmitted diseases were common indications for self-medication practice [26].
A few studies have been undertaken in Ethiopia to investigate the usage of self-medication among the public and students, including medical students [27,28,29], and there are indications on the misuse of antibiotics by patients, even by health professionals [30]. However, there is no study conducted on self-medication practice with antibiotics of adult outpatients in Ethiopia. The findings of this study will fill the research and knowledge gap. In addition, this study will generate information that may be useful in policy development and review of policies on licensing of drugs. Furthermore, it can be used as a stepping stone for health professionals if there is any possibility of intervention. Finally, this research can be used as a base for other health professionals including pharmacists in understanding the situation of the case and extending their intervention or work to different institutions also the findings potentially assisting in the development of appropriate regulatory and administrative solutions in Ethiopian hospitals. As a result, this study aimed to assess self-medication practice with antibiotic-among adult patients in OPD at selected public hospitals in Addis Ababa, Ethiopia.
Materials and methods
Study design, setting and period
An institution-based cross-sectional study was conducted from February 2022 and March 2022, in selected public hospitals, Addis Ababa, Ethiopia. Addis Ababa is the capital city of Ethiopia, which contains 13 government hospitals (5 federals, 6 under Addis Ababa health bureau, one owned by the police force, and one owned by armed force) distributed throughout ten sub-cities. All Hospitals provide different OPD services. Four hospitals had been selected using simple random sampling by lottery method from the list of thirteen hospitals [31]. Tikur Anbessa specialized Hospital, St. Paul Hospital Millennium Medical College, Minillik II Hospital and St. Peter specialized hospital. Tikur Anbessa Specialized hospital and St. Paul’s Hospital both are the largest referral and teaching hospitals in Ethiopia and are operated under the ministry of health. St. Peter specialized Hospital is the other referral and teaching hospital among those operated under the federal ministry of health. However, Minillik II Hospital is among the six governmental referral hospitals that are managed under the Addis Ababa Administrative Health Office. Patients who attended outpatient clinics in the hospital were expected to provide information in respect to factors associated with SMA. The above selected hospitals outpatient clinics had a high volume of patients and this enabled the researcher to collect data from the subjects from the proposed sample size within the limited time of the survey. Patients visiting the hospital due to their illnesses may have had prior knowledge of SMA, unlike a person in the community who may not have experienced an illness.
Study participants and eligibility criteria
All adult patients seeking treatment in OPD in the selected public Hospital during the study period and fulfilled the inclusion criteria were included. addition, patients attending out patients in selected PHs who were above 18 years of age, and those who had taken informed consent were included, whereas, participants who were admitted in the ward, unconscious, unable to speak and hear, critically ill patients and who were not willing to participate in the study were excluded in this study.
Sample size determination and sampling techniques
Sample size (n) had been calculated on the basis of a single population proportion formula assuming that the prevalence of self-medication with antibiotics is taken from a previous similar study in Kenya to calculate the sample size 0.476 is taken [32]:
The assumptions used are: z value of 1.96 at 95% confidence interval (CI) and margin of error (d) is 5%, non-response rate 10%:
d marginal error of 5%; p proportion; n sample size.
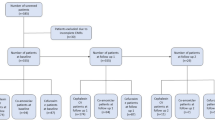
By adding 10% for incomplete and non-responses, the total sample size required for this study was found to be 421. From 13 governmental Hospitals in Addis Ababa, Tikur Anbessa, St. Paul, Minillik II, St. Peter hospitals and St. Paul’s Hospital Millennium Medical College were selected randomly using a lottery method. To select 421 participants from adult medical and surgical OPD from a total of four selected PHs, first, all selected hospitals were listed down with their respective number of OPD patients per month. A stratified sampling method was performed with the strata being outpatient department, surgical, and medical outpatient clinics. Data were taken from each hospital with of monthly OPD patients report, and then, the number of OPD patients in each hospital was proportionally allocated for sample size, and then, finally the study participants for each hospital were selected and interviewed with a systematic random sampling method in every kth interval of each respective hospital until the required sample size was achieved (Fig. 1).
From the past 3-monthly report from November, 2021 to January 2022 of each hospital indicate that the average number of adult OPD cases at Tikur Anbessa specialized hospital, Minillik II, St. Peter hospitals and St. Paul’s Hospital Millennium Medical College, were 1200, 950, 862 and 1450, respectively.
The total sample size (421) was allocated proportionally for the four public hospitals based on the number of OPD patients seeking treatment in a month of each hospital was: \({{n}_{j}}=\frac{{n}\times{N}_{j}}{N}\) and interval size; \({{k}_{j}}=\frac{Nj}{n}\)
where nj was the sample size of the jth hospital;
Nj was population size of the jth hospital;
n = nTASH + nSPMMC + n Minillik H + NSPSH was the total sample size (421);
N = NTASH + NSPMMC + NMinelikH + NSPSH was the total population size of hospitals
= 1200 + 1450 + 950 + 862 = 4462;
nTASH = 421 * 1200/4462 = 113; k = 1200/113 = 11, SPMMC = 421 * 1450/4462 = 137; k = 1450/137 = 11, Minillik II Hospital = 421 * 950/4462 = 90; k = 950/90 = 11, SPSH = 421 * 862/4462 = 81; k = 862/81 = 11.
Therefore, the initial sample was selected using the lottery metho; then, every 11th participant was selected until the calculated sample size was attained within the data collection period’s time frame.
Variables of the study
Socio-demographic factors were age, sex, education, marital status, religion, and occupation. Behavioral and social factors such as: mild illness, prior experience, emergency use, stressful conditions, chronic illness, advice from others, laws controlling, policy factors, insurance, and knowledge on risks of use. Health facility factors are the availability of antibiotics, diagnosis, healthcare costs, ease of access, prescription, queues, and save time and attitudes, such as attitudes, distance, queues, policy factors, and laws. The dependent variable was self-medication practice with antibiotics. This was determined as the report of taking drugs without a prescription among adult outpatients.
Data collection and procedures
The questionnaire was first prepared in the English language and translated into Amharic by a language expert for interviews. To check the accuracy and its consistency, the questionnaire was pretested on 21 participants (5% of the sample size) in one hospital in Addis Ababa, and this facility was excluded from the actual study before the start of the actual data collection period. Data were collected using structured and pretested questionnaires. Three BSc pharmacists participated in the data collection after 1 day of training were given on the objective, the relevance of the study, the confidentiality of information, respondent’s right, and informed consent. Frequent checks were made on the data collection process to ensure the completeness of principal investigators and supervisor.
Data quality assurance
Data collectors were trained intensively by the principal investigator on the contents of the questionnaire, data collection methods, and ethical concerns. The filled questionnaire was checked daily for completeness by the principal investigator for uniformity and understandability of the checklist after which modification for its appropriateness and suitability was performed. Data collectors had trained on strict use of study criteria, an explanation of study objective, getting verbal consent from study participants, uniform interpretation of questions, and the collected data confidentiality.
Data processing and analysis
After checking the collected data for its completeness and accuracy, codes were given to the questionnaire; then, the data were entered using Epi data 4.6 statistical software and analyzed using the SPSS version 26 statistical package. Binary logistic regression was used to determine the association between the explanatory and outcome variables, and multivariable logistic regressions were used to determine the association between dependent and independent variables, P value < 0.05 was considered as statistically significant.
Operational definition
Self-medication: getting and using conventional medications for disease diagnosis, treatment, or prevention without a doctor’s prescription.
Antibiotics: this is a drug used in the treatment and prevention of bacterial infection.
Adverse reaction: this is an unwanted effect caused by administrating a drug.
Outpatient: patient who attends for treatment in an outpatient clinic without staying there overnight.
Outpatient department: is part of a hospital designed for treating outpatients for whom they have health problems but do not require a bed or to be admitted for overnight care.
Over the counter/non-prescribed drugs: are those drugs that can be legally purchased from a drug retail outlet without having a prescription from a licensed healthcare provider.
Self-medication practice: a person is said to practice self-medication if he/she self-medicated at least once [32].
Ethical consideration
Ethical clearance was obtained from the Institutional Review Board RVU college of Health science and a support letter obtained from Addis Ababa health bureau administration for each Hospital. The objective and importance of the study was explained to the study participants; then, data were collected only after full informed verbal and written consent was obtained. The confidentiality of the information was maintained by excluding the participants’ name in the interview questionnaire.
Results
Among 421 respondents approached for the study, 403 (95.7%) were included in the final analysis. Around two-third (69%) the respondents were females. The mean (± SD) age of the participants was 33 (± 21) years. More than one-third of the (36.7%) participants was between 25 and 34 years. The majority of the respondents (62.5%) were not employed, while those who were formally employed were 24.8%. Around three-fourth (73%) of the respondents had no medical insurance scheme (Table 1).
Education levels of the respondents
Education levels were categorized into four: those who had not gone to school, primary, secondary, and college/university. The respondents who had College/University were 6% (24), secondary education was 51.1% (206), those with primary education were 29.1% (117), and those who had not gone to school were 13.8% (56) (Fig. 2).
Prevalence of self-medication
General prevalence of self-medication
The participants were asked whether they had ever taken any drug without prescription. Among the total respondents, majority of them (71%), the respondents had generally practiced self-medication (Fig. 3).
Prevalence of self-medication with antibiotics
The respondents were required to determine whether they had ever taken any antibiotic without prescription. Around half of the participants (48.3%) had used antibiotics, while 51.7% had used other drugs (Table 2).
Number of times respondents self-medicated
More than half of the respondents, 59 (42.8%) had used antibiotics above five times in the past year, 34 (24.6%) three times, 26 (18.8%) twice, 12 (8.7%) four times, and 7 (5.1%) once (Fig. 4).
Factors associated with self-medication
The age of the respondents was categorized in groups ranging from 18 to 24 years, 25 to 34 years, 35 to 44 years, and those above 45 years. Age and medical insurance scheme were significantly associated with self-medication (P < 0.05) in the Chi-square test (Table 3).
Independent predictors of self-medication
In the multivariable regression model, participants who had College and university students were 1.6 times likely to practice self-medication compared with those who never went to school or illiterate [AOR = 1.65, 95% CI (1.3–2.4), P = 0.004]. The lack of medical insurance was also significantly associated with self-medication with antibiotics [AOR = 1.632, 95% CI (1.21–2.63), P = 0.033] (Table 4).
Reasons for indulging in self-medication
The majority of those who practiced self-medication with antibiotics (53.6%) gave reasons for the practice as to reduce medical cost, 26.2% said that there are long delays in health facility, while 11.6% did so because of a busy day’s program (Table 5).
Indication for SMP
Various respondents gave their complaints for taking antibiotics as follows: abdominal pain 44.9%, sore throat 21%, cough 16.7%, diarrhea and vomiting 8.0%, toothache 6.5%, and wound 2.9% (Fig. 5).
Patients who were advised on self-medication with antibiotics
Few participants (21.1%) had been advised to take medication without prescription, while 78.9% were advised but did not self-medicate. Advice had no significant association with self-medication (P > 0.05) (Table 6).
Respondents’ sources of advice for self-medication
Those advised to take an antibiotic the majority of the respondents (47.4%) said their source of advice was from a colleague, 28% from health workers, 12.3% from a relative (Table 7).
Commonly used antibiotics in SMA
The respondents were asked to mention the antibiotics that they had used without prescription. A list of antibiotics was provided to help the patients recall. The commonly used antibiotics are amoxicillin (57%), ciprofloxacin (13%), amoxicillin/clavulanic (10%), erythromycin (8%), cotrimoxazole (7%), and doxycycline (5%) (Fig. 6).
Sources of antibiotics
From Table 8, the majority of respondents who practiced self-medication with antibiotics got the drugs from community pharmacy (84.8%), others got drugs from health workers (8.7%), while 6.5% got the drugs from friends (Table 8).
How respondents knew the dosage
As shown in the table above, it shows that 81.9% had enquired the dosage from the seller, while 15.9% used a previous prescription to know the dosage of the drug for self-medication (Table 9).
Discussion
Patients who attended outpatient clinics were surveyed over the course of a month and a half. The prevalence of SMP was found to be 48.3% in the survey. Amoxicillin was the most widely used antibiotic for self-medication. Antibiotics were primarily obtained from local or community pharmacies. The primary motivation for using SMA was to save money. This study focused solely on antibiotic self-medication. Other drug classifications were excluded from the poll. The findings were still valid despite this constraint. To decrease the recall bias, a list of antibiotics was employed.
The majority of the respondents in this study were aged between 25 and 34 years at 31.1%. This was comparable with a study by Charles Kiragu Ngigi in Kenya, which had 27.7% of the respondents with the same age who practiced self-medication with antibiotics [32] and nearly also comparable with the study conducted in India, which found that 39% of respondents of the same age used antibiotics for self-medication [33]. According to this study, females account for 68.0% of practiced self-medication. In contrast [34], found that 44% of respondents in research in Saudi Arabia were female.
Self-medication with antibiotics was found to be 48.3%, which is lower than prior studies in Northern Nigeria, which found 56.8% and 50.3%, respectively [35, 36]. Self-medication with antibiotics was reported by 41.8% of respondents aged 18–24, which is comparable to data from [37] in Nigeria, who found 44% of respondents in the same age range. SMA and education had no meaningful relationship. Around half (46.7)% of those who self-medicate with antibiotics are divorced and 38.3% of those with secondary education. In this study, respondents who had not “gone to school” accounted for 25% of the total, implying that educated people accounted for 75% of the total, which is close to a study by Widayati et al. [38] that linked self-medication to a high percentage of education (78%). Other similar study reported in Nigeria, with just 14% of uneducated individuals self-medicating [39]. This link between self-medication and education could be due to the ease with which information can be obtained from various sources, including the internet.
Those who practiced self-medication with antibiotics had a smaller number of unemployed people (31%). This contradicts a study conducted by Askarian et al. [40], which revealed that 7.4% of the population was unemployed. SMA was practiced by 39.8% of persons who did not have health insurance, which was lower than the 46.3 percent reported by Askarian et al. [40] in Southern Iran. Self-medication with antibiotics is significantly connected with a lack of medical insurance.
Amoxicillin was the most often used antibiotic, with 79 (57%) of respondents using it. This was supported by studies conducted by Donkor et al. [41] in Accra, Ghana, and [42] in the United Arab Emirates, where amoxicillin had a high prevalence rate of 46% in both countries. According to a study conducted in Europe by Ali et al. [43], Greece has one of the highest outpatient antibiotic usage rates in Europe, with cephalosporins and macrolides being the most commonly prescribed antibiotics. The argument for the regular use of Amoxicillin was reinforced by the drug’s low cost around the world and its widespread prescription by healthcare practitioners, suggesting that it is well-known to the general people.
The antibiotics were obtained by a majority of responders (84.8%) from community pharmacy. This was contracted with a study conducted in Sudan, which found that 68.8% of the medications were obtained from a community pharmacy [44]. It is similar with other studies in India, with 79.5% of respondents getting their medications from pharmacies [45]. Other investigations in Palestine [20], Egypt [32], and other similar results [46]. The majority of respondents in all of these studies got their antibiotics from community pharmacies rather than through friends, health workers, or stores.
Antibiotics can be obtained from various sources: they are legally available over the counter, antibiotics originally prescribed by physicians can be saved and used without medical consultation, antibiotics can be obtained from friends or relatives, and they can be obtained via different sources.
Limitations of the study
The research was done in a limited duration of 1 month. Patients who continued to practice the self-medication at home and did not visit the hospital during the period of study were not sampled. The identification of the actual antibiotic taken may not have been accurately recalled. The study was restricted to the practice of self-medication among adult patients, and patients below 18 years were excluded from the study. A list of antibiotics was provided to the patients to help them recall the drugs used.
Recommendations
-
For policy makers
-
Health education initiatives on antibiotic self-medication should be directed at persons per age, gender, educational levels, and the public at large.
-
Interventions aimed at minimizing antibiotic self-medication should focus on limiting access to antibiotics obtained without a prescription.
-
Antibiotics will not be sold over the counter without a prescription at community pharmacies.
-
The involvement of community pharmacists in reducing the prevalence of SMP should be significant.
-
-
For further researchers
More research is needed:
-
To determine whether widely self-medicated medications cause microorganisms to develop antibiotic resistance.
-
To determine the prevalence of antibiotic self-medication in children under the age of 18.
-
To investigate the public awareness and perceptions of antibiotic self-medication
-
Conclusion
Antibiotic self-medication was prevalent among the study participants. Self-medication with antibiotics was 48.3 percent of the time, whereas general self-medication was 71%. Antibiotic self-medication is significantly associated with age, being a college or university student, and lack of health insurance. Self-medication with antibiotics is more common among adults aged 25–34 than in other age groups. The antibiotic amoxicillin was the most commonly self-medicated, followed by ciprofloxacin. Community pharmacies are a common source of antibiotics for self-medication. Self-medication with antibiotics, primarily amoxicillin and ciprofloxacin, was used to alleviate cough, abdominal pain, diarrhea, and vomiting. The majority of these drugs were gotten from a community pharmacy. In general, OPD patients appear to underestimate the possible hazardous effects of SMP. As a result, health officials should make an effort. As a result, health authorities such as the Drug and Therapeutic Committee, the Drug Regulatory Authority, hospital management, and other stakeholders should work together to ensure that antibiotics are used safely.
Availability of data and materials
Upon request to the corresponding author, all available supplementary information, including the data sets supporting the conclusions of this article, is made available.
Abbreviations
- FDA:
-
Food and Drug Administration
- FIP:
-
Federation International Pharmaceutics
- MOH:
-
Ministry of Health
- MOPC:
-
Medical out-patient clinic
- OPD:
-
Outpatient department
- OTC:
-
Over the counter
- PHs:
-
Public Hospitals
- RVU:
-
Rift Valley University
- SM:
-
Self-medication
- SMA:
-
Self-medication with antibiotics
- SMP:
-
Self-medication practice
- SOPC:
-
Surgical outpatient clinic
- SP:
-
Sulfadoxine/pyrimethamine
- SPHMMC:
-
St. Paul’s Hospital Millennium Medical College
- SPSH:
-
St. Peter Specialized Hospital
- TASH:
-
Tikur Anbessa Specialized Hospital
- WHO:
-
World Health Organization
- WSMI:
-
World Self-Medication Industry
References
Hernandez-Juyol M, Job-Quesada J. Dentistry and self-medication: a current challenge. Medicina oral: organo oficial de la Sociedad Espanola de Medicina Oral y de la Academia Iberoamericana de Patologia y Medicina Bucal. 2002;7(5):344–7.
Mekuria AB, et al. Prevalence and predictors of self-medication practice among teachers’ education training college students in Amhara region, Ethiopia: a cross-sectional study. Front Pharmacol. 2021;11:2457.
Helal R, Abou-ElWafa H. Self-medication in university students from the city of Mansoura, Egypt. J Environ Public Health. 2017. https://doi.org/10.1155/2017/9145193.
Björnsdóttir I, Almarsdóttir AB, Traulsen JM. The lay public’s explicit and implicit definitions of drugs. Res Social Adm Pharm. 2009;5(1):40–50.
Sweileh MW. Self-medication and over-the-counter practices: a study in Palestine. Al-Aqsa Univ J (Nat Sci Ser). 2004;8(1):1–9.
Ocan M, et al. Household antimicrobial self-medication: a systematic review and meta-analysis of the burden, risk factors and outcomes in developing countries. MC Public Health. 2015;15:1–11.
González-López JR, Rodríguez-Gázquez MDLÁ, Lomas-Campos MDLM. Self-medication in adult Latin American immigrants in Seville. Acta Paulista de Enfermagem. 2012;25:75–81.
Andaulem T, Gebre-Mariam T. Self-medication practices in Addis Ababa: a prospective study. Ethiop J Health Sci. 2004;14(1):1–11.
Fuentes Albarrán K, Villa Zapata L. Analysis and quantification of self-medication patterns of customers in community pharmacies in southern Chile. Pharm World Sci. 2008;30(6):863–8.
Ruiz ME. Risks of self-medication practices. Curr Drug Saf. 2010;5(4):315–23.
Mihretie TM. Self-medication practices with antibiotics among urban dwellers of Bahir Dar town, north west Ethiopia. Addis Ababa: Addis Ababa University; 2014.
World Health Organization. Guidelines for the regulatory assessment of medicinal products for use in self-medication. Geneva: World Health Organization; 2000.
Sharif SI, Bugaighis LM, Sharif RS. Self-medication practice among pharmacists in UAE. Pharmacol Pharm. 2015;6(09):428.
Shankar P, Partha P, Shenoy N. Self-medication and non-doctor prescription practices in Pokhara valley, Western Nepal: a questionnaire-based study. BMC Fam Pract. 2002;3(1):1–7.
Shoaib MH, et al. Survey based study on the use of non-prescription drugs among pharmacists and non-pharmacists. Afr J Pharm Pharmacol. 2013;7(38):2652–6.
Mahardika AB, Suryawati S, Aji R. Intervensi CBIA untuk Meningkatkan Pengetahuan, Sikap, dan Perilaku Penggunaan Antibiotik yang Rasional pada Anggota Bina Keluarga Balita. Jurnal Kedokteran Brawijaya. 2016;29(2):165–9.
Jassim UT, Ebrahim SM. Self-medication among nurses working in Basra teaching hospitals, Iraq. Turk J Physiother Rehabil. 2021;32:3.
Kasulkar AA, Gupta M. Self medication practices among medical students of a private institute. Indian J Pharm Sci. 2015;77(2):178.
Skliros E, et al. Self-medication with antibiotics in rural population in Greece: a cross-sectional multicenter study. BMC Fam Pract. 2010;11(1):1–3.
Sawalha AF. A descriptive study of self-medication practices among Palestinian medical and nonmedical university students. Res Soc Adm Pharm. 2008;4(2):164–72.
Balamurugan E, Ganesh K. Prevalence and pattern of self medication use in coastal regions of South India. Br J Med Pract. 2011;4(3): a428.
Gbagbo FY, Nkrumah J. Self-medication among pregnant women in two municipalities in the Central Region of Ghana. Health Care Women Int. 2021;42(4–6):547–62.
Bradley C, Blenkinsopp A. Over the counter drugs: the future for self medication. BMJ. 1996;312(7034):835–7.
Nyambega JO. Antibiotic use and misuse among adults in Magwagwa Ward, Nyamira County in Kenya. Age. 2017;18(25):26–35.
Ocan M, et al. Patterns and predictors of self-medication in northern Uganda. PLoS ONE. 2014;9(3): e92323.
Parakh R, et al. Selfmedication practice among engineering students in an engineering college in North India. J Phytopharm. 2013;2:30–6.
Abay S, Amelo W. Assessment of Self-medication practices among medical, pharmacy, health science students in Gondar university. Ethiop J Young Pharm. 2010;2(3):306–10.
Gutema GB, et al. Self-medication practices among health sciences students: the case of Mekelle university. J Appl Pharm Sci. 2011;1(10):183.
Bekele SA, Argaw MD, Yalew AW. Magnitude and factors associated with self-medication practices among university students: the case of Arsi University, College of Health Science, Asella, Ethiopia: cross-sectional survey based study. Open Access Libr J. 2016;3(6):1–15.
Kassa T, et al. Antibiotics self-medication practices among health care professionals in selected public hospitals of Addis Ababa, Ethiopia. Heliyon. 2022;8: e08825.
Negera TT. Determinants of adherence to anti-retroviral therapy (ART): protocols in public hospitals in Addis Ababa, Ethiopia (Doctoral dissertation). 2020.
Ngigi CK, Mwagiru P, Wala J. Self-medication with antibiotics prior to seeking treatment among adult patients attending outpatient department at Gatundu sub-county hospital, Kiambu County. Kenya Imp J Interdiscip Res. 2016;2(8):41–4.
Venkat MU, Nagesh A, Venkat MK. Community based survey of self-medication usage in Andhra Pradesh.
Alghanim S. Self-medication practice among patients in a public health care system. East Mediterr Health J. 2011;17(5):409–16.
Olayemi O, Olayinka B, Musa A. Evaluation of antibiotic self-medication pattern amongst undergraduate students of Ahmadu Bello university (main campus) Zaria. Res J Appl Sci Eng Technol. 2010;2(1):35–8.
Fadare JO, Tamuno I. Antibiotic self-medication among university medical undergraduates in northern Nigeria. J Public Health Epidemiol. 2011;3(5):217–20.
Osemene K, Lamikanra A. A study of the prevalence of self-medication practice among university students in southwestern Nigeria. Trop J Pharm Res. 2012;11(4):683–9.
Widayati A, et al. Self medication with antibiotics in Yogyakarta City Indonesia: a cross sectional population-based survey. BMC Res Notes. 2011;4(1):1–8.
Omolase C, et al. Self medication amongst general outpatients in a Nigerian community hospital. Ann Ibadan Postgrad Med. 2007;5(2):64–7.
Askarian M, et al. A study of antibiotics self-medication at primary health care centers in Shiraz, Southern Iran. J Health Sci Surveill Syst. 2013;1(1):1–5.
Donkor ES, et al. Self-medication practices with antibiotics among tertiary level students in Accra, Ghana: a cross-sectional study. Int J Environ Res Public Health. 2012;9(10):3519–29.
Sajith M, et al. Self-medication practices among health care professional students in a tertiary care hospital, Pune. Open Public Health J. 2017;10(1):63–8.
Ali AN, et al. Self-medication practices among health care professionals in a Private University, Malaysia. Int Curr Pharm J. 2012;1(10):302–10.
Awad A, Al-Rabiy S, Abahussain E. Self-medication practices among diabetic patients in Kuwait. Med Princ Pract. 2008;17(4):315–20.
Adhikary M, et al. Study of self-medication practices and its determinant among college students of Delhi University North Campus, New Delhi, India. Int J Med Sci Public Health. 2014;3(4):406–9.
Ibrahim NK, et al. Self-medication with analgesics among medical students and interns in King Abdulaziz University, Jeddah, Saudi Arabia. Pak J Med Sci. 2015;31(1):14.
Acknowledgements
We would like to acknowledge the data collectors and the study participants supporting us during conducting this study.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
YBT contributed to the conception, project administration, formal analysis, investigation, methodology, data curation, resources, writing of the original draft of the manuscript, reviewing, and editing. ATK contributed to the supervision, formal analysis, methodology, data curation, validation, review, and editing of the final manuscript. EAB contributed to the formal analysis, methodology, data curation, validation, review, and editing of the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Institutional Review Board RVU college of Health science and a support letter obtained from Addis Ababa health bureau administration for each Hospital. The objective and importance of the study were explained to the study participants; then, data were collected only after full informed verbal and written consent was obtained. The confidentiality of the information was maintained by excluding the participants’ name in the interview questionnaire.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tadesse, Y.B., Kassaw, A.T. & Belachew, E.A. Evaluating self-medication practices in Ethiopia. J of Pharm Policy and Pract 16, 47 (2023). https://doi.org/10.1186/s40545-023-00553-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40545-023-00553-0