Abstract
Background
Despite appropriate treatment of epilepsy, the treatment outcome is poor in developing country. Therefore, the study was aimed to identify the magnitude and associated factors of epileptic patients at ambulatory clinic of south western Ethiopian hospital.
Methods
A hospital-based cross-sectional study was conducted on epileptic patients who had follow-up at Mettu Karl Comprehensive Specialized Hospital (MKCSH). Data collection was done through patient interview and medical charts review. The pharmaceutical care network Europe foundation classification system was used to assess the drug therapy problem and Naranjo algorithm of adverse drug reaction was employed to identify the probability of adverse drug reaction. The data were analyzed by SPSS version 23 after data were entered by Epidemiological Information (Epi Info) 7.2.1. The multivariable logistic regressions were utilized and P < 0.05 was used to declare association.
Results
Over the study period, more than half of the participants 172(57.7%) were males. The magnitude of drug-related problems was found to be 164(55.0%). Among epileptic patients about 323 drug-related problems (DRPs) were identified on average, 1.084 drug-related problems (DRPs) per patient. The widely occurred types of drug-related problems were needs additional drug therapy 72(22.29%), dose too low 52(16.09%) and dose to high which accounts 50(15.48%). Regarding the predictors of drug-related problems, being a female (AOR = 3.57, 95% CI:1.85–6.88, P ≤ 0.001), having frequent seizures (AOR = 2.47, 95% CI%:1.33–4.61, P = 0.004) and the presence of poly-pharmacy (AOR = 3.57, 95% CI: 1.49–8.5, P = 0.004) were predictors of drug-related problems.
Conclusion
More than half of the patients had a drug therapy problem. Number of medications taken by the patients, gender and the seizure frequency had a significant association with occurrence of drug therapy problems (DTPs). Therefore, the pharmaceutical care in general and drug information services in particular should be established to hinder any undesirable medication effects in our study area.
Similar content being viewed by others
Background
Epilepsy is one of the neurologic disorders that is manifested as a frequent attacks of the seizures affecting about 50 million people globally in which more than three-fourths of them residing in developing countries [1,2,3]. In Ethiopia the prevalence of epilepsy is 64 per 100,000 populations [2].
The goal of epilepsy treatment is to control seizures without drug-related problems (DRPs) [4]. The epilepsy drug therapy should be individualized to reduce any drug-related problems [1]. However, almost all of epileptic patients have no access to the appropriate treatment in low-resource countries [2]. In south western Ethiopia, about two-thirds of the epileptic patients had had uncontrolled seizures due to inappropriate therapy [5]. Therefore, the drug-related problems should be reduced to enhance the treatment outcome of epileptic patients [6].
Despite appropriate treatment of epilepsy, the treatment outcome is poor in developing country [7]. This could be due to the complexity of the pharmacokinetics profiles of AEDs and the probability of the drugs to inhibit/induce the most metabolizing enzymes that pose difficulty in delivering appropriate dose of the drugs [1].
Non-adherences to anti-epileptic drugs (AEDs) were the common drug therapy problems that hinder the treatment outcomes of the epileptic patients. Hence, the hindrances to patient’s adherence to their treatment should studied at large to reduce poor treatment outcomes [3].
Different factors were associated with the occurrence of drug-related problems (DRPs) in epileptic patients that includes presence of poly-pharmacy, the presence of comorbidity, female sex and history of hospital admission [8, 9].
The occurrences of medication-related problems might lead to unsuccessful control of the seizure, hospitalization, increased health care cost, decreased quality of life [3, 9, 10]. Besides, the mortality rate is increased secondary to medication therapy problems [10, 11].
In Ethiopia, about 70% of the epileptic patients had encountered at least one drug-related problems [12]. The previous study only reports the magnitudes of the drug-related problems and they primarily focused on the assessment of adherence, and there is a scanty of studies on the associated factors of medication-related problems. Therefore, the study aimed to identify the predictors of medication-related problems among epileptic patients at ambulatory care.
Patients and methods
Study area, design and period
A cross-sectional study was conducted at Mettu Karl Comprehensive Specialized Hospital (MKCSH) from February 12, 2020 to August 11, 2020. MKCSH is found in Mattu town, South West Oromia, Ethiopia which is found at 600 km from Finfinne. There are different wards and clinics within MKCSH; those include internal medicine ward, surgery ward, pediatric ward, gynecology and obstetrics ward, antenatal clinic, dental clinics, tuberculosis clinic, anti-retro viral therapy clinic and ophthalmic clinic.
Inclusion criteria
Adult patients (age ≥ 18 years) with the diagnosis of the epilepsy who have been on regular follow- up for at least 2 years with complete registration charts who were on drug therapy or who need drug therapy during study period and with more than 48 h of length of stay were included.
Exclusion criteria
The epileptic patients who had not prescribed with anti-epileptic drugs, follow-up period of less than 2 years, seriously ill to complete the interview, refused to give consent, and those with incomplete medical records were excluded.
Study variables and outcome endpoints
Medication-related problem was the primary outcome. Adverse drug reaction (ADR) was assessed by using the Naranjo algorithm of the ADR probability scale [13]. Hill–Bone Compliance to High Blood Pressure Therapy Scale was used to measure medication adherence [14]. For this study purpose, we had used a 9-item medication-taking sub-scale. Each item is a four-point Likert-type scale (none of the time, some of the time, most of the time, and all the time). The median split was used and dichotomies into adherent and non-adherent to the treatment. The pharmaceutical care network Europe guideline was used to assess the presence of medication-related problems. The work has been reported in line with the strengthening the reporting of cohort studies in surgery (STROCSS) criteria [15].
Sample size and sampling technique
Single population proportion formula was used to calculate the required sample size by considering the magnitude of the problem P = 0.608 [5].
The sample size (n) was calculated as:
where n = the desired sample size, Z = level of significance at 95% confidence interval which is 1.96, P = magnitude of problem, q = 1-p, d = margin of error which is 0.05, \(n = \frac{ \left( {{1}.{96}} \right)^{{2}} \left( {0.{6}0{8}} \right)(0.{392})} {\left( {0.0{5}} \right)^{{2}}} = {366},\) \({\text{nf }} = \frac{n}{1 + n/N} = \frac{n \times N}{n+N},\) where nf = adjusted sample size, n = sample from infinite population, N = population size,
By adding 10% contingency, the final sample size becomes 298. A simple random sampling was used to include study participants.
Data collection process and management
A semi-structured data collection tool was prepared to collect the data. Laboratory results, current medications, co-morbidities, relevant previous medical and medication histories were collected using data abstraction format from medical chart review. Three medical doctors and two clinical pharmacists were recruited for data collection; one clinical pharmacist was assigned to supervise the data collection process. DRP registration format was used to identify and record different types of DRPs [16]. To assure the consistency of the data collection tool, it was pretested at nearby hospital called Bedele general hospital prior to normal data collection.
Data processing and analysis
The data were entered into a computer using Epidemiological Information (Epi Info) 7.2.1. The principal investigators had daily checked and clean the data. The data were then exported to statistical software for social sciences (SPSS) 24.0 for analysis. Multivariable logistic regression was used to analyze the variable by using crude odds ratio (COR) and adjusted odds ratio (AOR) with 95% CI. All variables associated with the drug-related problems at a P-value ≤ 0.25 on the bivariate analysis were entered into a multivariable logistic regression analysis to control for confounders. Finally, the predictors of drug-related problems were declared if a P value of ≤ 0.05.
Operational definitions
Drug-related problem: includes ADR, non-adherence, inappropriate indication and dose, and ineffective drug therapy [17] Poly-pharmacy: the daily consumption of 5 or more medications [17] Co-morbidity: patients diagnosed with two or more diseases [17] Prolonged hospital stay: if the patients stay ≥ 7 days [18] |
Results
Socio-demographic characteristics of participants
Over the study period, more than half of the participants 172(57.7%) were males. The median age of participants was 29 years and majorly distributed to age of 18–30 year class. Majority, 235(78.9%) of participants were single and 139 (46.6%) of were attended high school. With regard to their occupation, about two-thirds 100(33.6%) of them were students and one fourths 77(25.8%) of them were housewife. About two-thirds 100(33.6%) of them had a monthly income of greater than one thousand (Table 1).
Clinical characteristics of the epileptic patients
The most type of seizure was absence seizure 85(28.5%) and generalized tonic–clonic (GTC) which accounts 83 (27.9%). About half 138(46.5%) of them had a seizure frequency of greater than four whereas three-fourths 222(74.5%) of them had the epilepsy duration of less than 3 years. Nearly two-thirds 194(65.1) of the patients have no family history of epilepsy and 92(30.9%) had comorbidity (Table 2).
Prevalence and types of DRPs
The prevalence of actual or potential DTPs among subjects put on at least a single drug was found to be 164(55.0%). A total of 323 DRPs were identified on average, 1.084 DRPs per patient. Poly-pharmacy was reported among 70(23.5%) of the epileptic patients. The three-leading category of drug-related problems found to be a culprit among the sample were needs additional drug therapy 72(22.29%), dose too low 52(16.09%) and dose to high which accounts 50(15.48%) (Table 3).
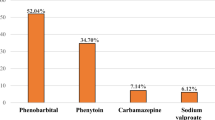
The individual drugs involved in DRPs
The most anti-epileptic drug (AED) associated with drug therapy problems were phenobarbitone 66(30.0%), carbamazepine 58(26.36%), and valproic acid 53(24.09%) (Table 4).
Determinants of medication-related problems among epileptic patients
The output of the multivariable logistic regression showed that a significant association was observed between the sex, frequency of the seizure, and poly-pharmacy with the presence of DRPs. Being a female were 3.57 times more likely to had at least one drug therapy problems than males (AOR = 3.57, 95% CI:1.85–6.88, P ≤ 0.001). Patients having frequent seizures were 2.74 more likely to have drug-related problems (AOR = 2.47, 95% CI:1.33–4.61, P = 0.004). Lastly, patients who have prescribed 5 or more drugs (poly-pharmacy) were 3.57 times more likely to have DRPs than patients prescribed with less than 5 drugs (AOR = 3.57, 95% CI: 1.49–8.5, P = 0.004) (Table 5).
The comparisons of the pattern medication-related problems among different settings of Ethiopian hospitals revealed that the prevalence of medication-related problem was lower than the study of Tikur Anbessa Specialized Hospital (TASH) and Jimma University Medical Center (JUMC). Phenobarbitone was the commonly prescribed AEDs in all hospitals of TASH, University of Gondar Referral Hospital (UOGRH) and JUMC. The presences of medication were predictors of medication-related problem in all hospitals of TASH, UOGRH and JUMC (Table 6).
Discussion
The occurrence of DRPs among epileptic patients could be influenced by different factors like the number of drugs (taking ≥ 5), types of medical conditions, poly-pharmacy, female sex and history of admission to the hospital [9]. Therefore, this study tried to identify the magnitudes and determinants of this DRP among epileptic patients on chronic follow-up.
The prevalence of DRP in our study patients was 164(55.0%) which was lower than the study done in Wollega university referral hospital (71.51%) [19] and Tikur anbessa specialized hospital 70.4% [1]. The difference in magnitudes of medication-related problem observed across different settings might be due to a variation in medication therapy management classifications and study settings. Despite this difference observed, the interventions should be done to resolve DRPs to improve patient’s treatment outcomes and future researchers should use similar DRPs classification systems to generate evidence-based recommendations.
The most commonly occurred drug therapy problems was needs additional drug therapy 72(22.29%) in our study area which was different from the study of Tikur anbessa specialized hospital in which adverse drug reaction was mostly reported [1]. Similar finding was obtained from Wollega university referral hospital [19]. The variety of reports might be due to the differences in the classification of drug-related problems in different settings.
Identifying factors contributing to drug therapy problems is crucial for the reduction of unwanted effects of DRPs in epileptic patients [19]. In our study being a female were 3.57 times more likely to had at least one drug therapy problems than males. This was contrary to the study of India and Tikur Anbessa Specialized Hospital, [1, 20]. This might be due to the non-adherences of female patients towards AEDs due to fear of harm to their fetus.
The presence of comorbidity was a predictor of drug-related problem in the study of Belayneh et al. [21]. Despite this, we could not find any association between drug-related problem and the presence of comorbidity in our study area.
Patients having frequent seizures were 2.74 more likely to have drug-related problems. This was in line with the reports of University of Gondar referral hospital [22]. This finding strongly suggests that patients having frequent seizure attacks were less adherent to their medications possibly by decreasing the patients belief on medication effectiveness.
Lastly, patients who have prescribed 5 or more drugs (poly-pharmacy) were 3.57 times more likely to have DRPs than patients prescribed with less than 5. This was similar with the reports of University of Gondar referral hospital and Tikur Anbessa Specialized Hospital and Jimma university medical center [1, 22, 23]. This might be patients prescribed a poly-pharmacy could have a drug–drug interactions with other medications that result in suboptimal dosages.
Strength and limitations
As strength, the DTPs were identified based on Cipolle DTPs classification system and Micromedex® was used as drug interaction checker and optimal sample size was obtained. As limitation, the result of the study may not be generalizable to all hospitals because it was a single-center study and the causal effect relationship was not assessed due to the retrospective nature of the study.
Conclusion
In conclusion, absence seizure was the commonest seizure type and phenobarbitone was the most prescribed AEDs. More than half of the patients had a drug therapy problem. Needs additional drug therapy was the top ranking DTP followed by dose too low. Number of medications taken by the patients, gender and the seizure frequency had a significant association with occurrence of DTPs. Therefore, the pharmaceutical care in general and drug information services in particular should be established to tackle any undesirable medication effects in our study area. Besides this, the prescriber should check on the possibility of drug interaction with different AEDs and unnecessary combination therapy should be avoided while a mono-therapy was preferred in our study settings.
Availability of data and materials
The materials used while conducting this study are obtained from the corresponding author on reasonable request.
Abbreviations
- ADR:
-
Adverse drug reaction
- AED:
-
Antiepileptic drug
- AOR:
-
Adjusted odds ratio
- COR:
-
Crude odds ratio
- DRP:
-
Drug-related problem
- DTP:
-
Drug therapy problem
- JUMC:
-
Jimma University Medical Center
- MKSCH:
-
Mettu Karl Comprehensive Specialized Hospital
- TASH:
-
Tikur Anbessa Specialized Hospital
- UOGRH:
-
University of Gondar Referral Hospital
References
Nasir BB, Berha AB, Gebrewold MA, Yifru YM, Engidawork E, Woldu MA. Drug therapy problems and treatment satisfaction among ambulatory patients with epilepsy in a specialized hospital in Ethiopia. PLoS ONE. 2020;15(1): e0227359. https://doi.org/10.1371/journal.pone.0227359.
Birru EM, Shafi M, Geta M. Drug therapy of epileptic seizures among adult epileptic outpatients of University of Gondar Referral and Teaching Hospital, Gondar, North West Ethiopia. Neuropsychiatr Dis Treat. 2016;12:3213.
Ejeliogu EU, Courage A. Prevalence and factors associated with non-adherence to antiepileptic drugs among children with epilepsy in Jos, Nigeria. Niger J Paediatr. 2020;47(3):240–5.
Mroueh L, Al-Hajje A, Salameh P, Preux PM, Boumediene F, Ratsimbazafy V, Jost J. Management of epilepsy in Lebanon: Medication reviews and drug-related problems. Pharmacoepidemiol Drug Saf. 2022;31(5):583–91.
Zewudie A, Mamo Y, Feyissa D, Yimam M, Mekonen G, Abdela A. Epilepsy treatment outcome and its predictors among ambulatory patients with epilepsy at Mizan-Tepi University Teaching Hospital, southwest Ethiopia. Neurol Res Int. 2020;8:2020.
Bekele F, Gezimu W. Treatment outcome and associated factors among epileptic patients at ambulatory clinic of Mettu Karl Comprehensive Specialized Hospital: a cross-sectional study. SAGE Open Medicine. 2022;10:20503121221125148.
Niriayo YL, Mamo A, Kassa TD, Asgedom SW, Atey TM, Gidey K, Demoz GT, Ibrahim S. Treatment outcome and associated factors among patients with epilepsy. Sci Rep. 2018;8(1):1–9.
Ayele Y, Tesfaye ZT. Drug-related problems in Ethiopian public healthcare settings: Systematic review and meta-analysis. SAGE open medicine. 2021;9:20503121211009730.
Adem F, Abdela J, Edessa D, Hagos B, Nigussie A, Mohammed MA. Drug-related problems and associated factors in Ethiopia: a systematic review and meta-analysis. Journal of Pharmaceutical Policy and Practice. 2021;14(1):1–24.
Ahmed I, Tesema AA, and Demeke T. Medication adherence and associated factors among patients with epilepsy at follow up clinics of Jimma town public hospitals, Jimma, South West, Ethiopia, 2019. J Pharmacol Clin Res 2020:8(1) JPCR.MS.ID.555735
Ayalew MB, Megersa TN, Mengistu YT. Drug-related problems in medical wards of Tikur Anbessa specialized hospital, Ethiopia. J Res Pharm Pract. 2015;4(4):216.
Beyene YB, Daba FB, Goro KK, Senbeta BS. Drug therapy problems and predicting factors among ambulatory epileptic patients in Jimma Medical Center, Southwest Ethiopia. PLoS ONE. 2022;17(4): e0267673.
Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, Janecek E, Domecq C, Greenblatt DJ. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239–45.
Kim MT, Hill MN, Bone LR, Levine DM. Development and testing of the hill-bone compliance to high blood pressure therapy scale. Prog Cardiovasc Dis. 2000;15(3):90–6. https://doi.org/10.1111/j.1751-7117.2000.tb00211.x.
Agha R, Mathew G. STROCSS 2021: Strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int J Surg (London, England). 2021;10:106165.
Cipolle RJ, Strand LM, Morley PC. Pharmaceutical care practice: the patient-centered approach to medication management. McGraw Hill Professional; 2012.
Bekele F, Tsegaye T, Negash E, Fekadu G. Magnitude and determinants of drug related problems among patients admitted to medical wards of southwestern Ethiopian hospitals: A multicenter prospective observational study. PLoS ONE. 2021;16(3):e0248575. https://doi.org/10.1371/journal.pone.0248575.
Bekele F, Bereda G, Tamirat L, Geleta BA, Jabessa D. “Childrens are not just “little adults”. The rate of medication related problems and its predictors among patients admitted to pediatric ward of southwestern Ethiopian hospital: a prospective observational study. Ann Med Surg. 2021;70:102827.
Bekele F, Fekadu G, Bekele K, Dugassa D, Sori J. Drug-related problems among patients with infectious disease admitted to medical wards of Wollega University Referral Hospital: prospective observational study. SAGE open medicine. 2021;9:2050312121989625.
Gurumurthy R, Chanda K, Sarma GR. An evaluation of factors affecting adherence to antiepileptic drugs in patients with epilepsy: a cross-sectional study. Singapore Med J. 2017;58(2):98.
Belayneh Z, Mekuriaw B. A systematic review and meta-analysis of anti-epileptic medication non-adherence among people with epilepsy in Ethiopia. Arch Public Health. 2020. https://doi.org/10.1186/s13690-020-00405-2.
Ayalew MB, Muche EA. Patient reported adverse events among epileptic patients taking antiepileptic drugs. SAGE Open Med. 2018;3(6):2050312118772471.
Garedow AW, Mulisa Bobasa E, Desalegn Wolide A, Kerga Dibaba F, Gashe Fufa F, Idilu Tufa B, Debalke S, Kumela GK. Drug-related problems and associated factors among patients admitted with chronic kidney Disease at Jimma University Medical Center, Jimma Zone, Jimma, Southwest Ethiopia: a hospital-based prospective observational study. Int J Nephrol. 2019;20:2019.
Acknowledgements
We thank Mattu University for logistic support. We are grateful to staff members and health care professionals of MKCSH, data collectors, and study participants for their cooperation in the success of this study.
Funding
None.
Author information
Authors and Affiliations
Contributions
FB and TM contributed to the proposal preparation, study design, analysis and writes up the manuscript. GF contributed to the design of the study, and the manuscript write-up. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent-to-participate
Ethical approval was obtained from the Research Ethics Review Committee (RERC) of the Mattu University with reference no CHS/RERC/89/2020. The study protocol was performed in accordance with the Declaration of Helsinki. Permission was given from the administrators and medical directors of MKCSH to conduct the study. The pros and cons of the study were explained to the patients participated in the study and written informed consent was obtained from patients. The name of patients and prescribers were not written on the tool to ensure confidentiality. The study was registered researchregistry.com with a unique reference number of “researchregistry7589”.
Competing interests
No competing interests exist.
Consent for publication
Not applicable. No individual person’s personal details, images, or videos are being used in this study.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bekele, F., Mamo, T. & Fekadu, G. Prevalence and associated factors of medication-related problems among epileptic patients at ambulatory clinic of Mettu Karl Comprehensive Specialized Hospital: a cross-sectional study. J of Pharm Policy and Pract 15, 71 (2022). https://doi.org/10.1186/s40545-022-00468-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40545-022-00468-2