Abstract
Background
Advanced therapy medicinal products (ATMPs) represent an important cornerstone for innovation in healthcare. However, uncertainty on the value, the high average cost per patient and their one-shot nature has raised a debate on their assessment and appraisal process for pricing and reimbursement (P&R) purposes. This debate led experts providing for recommendations on this topic. Our primary objective is to investigate the ATMPs P&R process in the main five European countries and to understand if this process is consistent with published P&R expert recommendations. We also investigated the current ATMP pipelines to understand if future ATMPs will create challenges for their P&R process.
Methods
P&R framework for ATMPs in the European Major five (EU5) countries was investigated through a literature search on PubMed, institutional websites of National Health Authorities and grey literature. The ATMPs pipeline database was populated from a clinical trial database (clinicaltrials.gov), relying on inclusion and exclusion criteria retrieved from the literature.
Results
Reimbursement status of ATMPs is different across the EU5 countries, with the exception of CAR-Ts which are reimbursed in all countries. Standard P&R process in place for other medicinal products is extended to ATMPs, with the exception of some cases in Germany. List prices, where available, are high and, tend to be aligned across countries. Outcome-based Managed Entry Agreements (MEAs) have been extensively used for ATMPs. Extra-funds for hospitals managing ATMPs were provided only in Germany and, as additional fund per episode, in France. The accreditation process of hospitals for ATMPs management was in most countries managed by the national authorities. As far as ATMPs pipeline is concerned, ATMPs in development are mostly targeting non-rare diseases.
Conclusions
Expert recommendations for ATMPs P&R were partially applied: the role of outcome-based MEAs has increased and the selection process of the centres authorized to use these treatments has been enhanced; additional funding for ATMPs management to accredited centres has not been completely considered and annuity payment and broader perspective in cost considerations are far from being put in place. These recommendations should be considered for future P&R negotiations to pursue rational resource allocation and deal with budget constraints.
Similar content being viewed by others
Background
Advanced therapy medicinal products (ATMPs), defined by Directive 2001/83/EC, integrated by Regulation 1394/2007, include gene therapies, somatic-cell therapies, tissue-engineered medicines, and products containing one or more medical devices (combined ATMPs) [1].
ATMPs assessment and appraisal issues [2], in particular gene therapies [3,4,5,6], and implications on the Pricing and Reimbursement (P&R) process have been recently investigated.
ATMPs are often used to treat severe diseases associated with considerable societal costs [3, 4].
Clinical trials are characterized by small patient populations, short investigational duration and single-arm trial design. This is supportive in accelerated procedures granted to medicines for rare diseases with a high unmet need but creates problems for Health Technology Assessment (HTA) [3, 5]. ATMPs are one-shot costly therapies, whose benefits can only be appreciated in a longer-term perspective. The temporal misalignment between incremental and avoided costs represents a challenging issue for budget constraints; payers may focus on the short-term economic impact of medicines, disregarding saving in the long-run [6]. Despite the overall impact on budget being similar to that of a cheaper treatment for a larger patient population, the emotional impact of high prices is stronger and may undermine the principle of equity [4]. In addition, ATMP management and administration is complex and requires: (i) a clear definition of centres of excellence with high-quality equipment and expertise of health-care professionals; (ii) proper funding of the centres, and (iii) facilitated patient access to effective new therapies [6].
These issues have been widely discussed by the literature, driving various recommendations by experts on the assessment and appraisal of ATMPs. In general, experts have not supported a specific value framework for ATMP, but they have recommended to (i) collect more robust evidence [6]; (ii) increase awareness on the value of ATMPs in order to overcome prejudice or excessive unjustified optimism [6]; (iii) strengthen the early dialogue between HTA authorities, payers and other stakeholders, including patients [6]; (iv) conduct post-marketing assessment programmes (which may include registries or observational studies) with the purpose to gain additional information on the efficacy and safety profile of ATMPs [6]; (v) rely on outcome-based Managed Entry Agreements (MEAs) to manage uncertainty on benefits and on annuity payment to split treatment costs over time [6]; (vi) work on an early definition of the criteria for a proper identification of the centres of excellence [6]; and (vii) to adopt a societal perspective in the economic evaluation of ATMPs (or at least a double reference case approach) and face challenges posed by ATMPs to cost–effectiveness analysis, including discount rates and modelling [3, 5].
The primary objective of this paper is to investigate how the P&R of ATMPs has been managed in the European Major five (EU5) countries and whether it is consistent with published expert recommendations. We also compared the current ATMP pipelines with already marketed treatments with the aim of identifying the issues that may be challenging in the P&R process in the future.
Materials and methods
A literature review on the ATMPs P&R status and regulatory frameworks across EU5 was conducted using PubMed (as scientific literature source), the institutional websites of the National Health Authorities for each of the five EU countries [7,8,9,10,11,12,13,14], and grey literature (google and non-peer review journals) using as cut-off date July 2020. ATMPs reimbursement status was defined as “reimbursed ATMP”, “not reimbursed ATMP” or “ongoing evaluation” and was assessed searching the institutional websites.
For pipeline analysis interventional clinical trials on ATMPs were retrieved from the clinicaltrials.gov database (www.clinicaltrials.gov) with a temporal limitation from July 2017 to November 2019. Hanna et al. 2016 keywords were used for a preliminary screening of ATMPs trials (i.e. trials focused on ATMPs) [15]. This first screening was validated using Committee for Advanced Therapies (CAT) criteria [16]. Only trials that met inclusion and exclusion criteria described in Table 1 were considered.
Rarity of the targeted diseases in each trial was searched on the Orphanet website [17]. Based on the European Medicine Agency (EMA) definition [18], diseases were considered rare if their prevalence does not exceed 5 cases in 10,000 people. An Excel® 2010 extraction template (Microsoft Corporation) was created to include all data for each trial identified: ATMP, Completion Date, Diseases, Rarity of the disease, First Posted, Funded By, Interventions, Last Update Posted, Locations, NCT (Number of Clinical Trial), Outcome, Phases, Primary Completion Date, Results, Sponsor/Collaborators, Start Date, Status, Study Results, Study Type, Therapeutic area, Title, URL. Duplicates and trials on investigational products other than ATMPs were excluded and finally the database was analysed according to ATMPs type, trial status, funding origin, therapeutic area and disease rarity (Table 2).
Results
The following two sections describe the current P&R process for ATMPs in EU5 countries and the pipelines. Consistency of the former with the recommendations of the literature and problems posed by the latter to future P&R negotiations will be discussed afterwards.
P&R process for ATMPs in EU5 countries
At the time of the analysis (July 2020), 15 ATMPs achieved marketing authorization (MA) in the European Union (EU); of these, ten have received orphan designation, ten have an active MA (Holoclar, Imlygic, Strimvelis, Spherox, Alofisel, Kymriah, Yescarta, Luxturna, Zynteglo, and Zolgensma) and five had already been withdrawn from the market for commercial reasons (ChondroCelect, Glybera, Provenge, Maci, and Zalmoxis) [19,20,21,22,23,24,25,26,27,28,29,30,31,32,33]. Despite being recently withdrawn from the market a few years after obtaining MA, Zalmoxis was included in the analysis because of its P&R assessment by all EU5 countries. After MA is granted, the Marketing Authorisation Holder (MAH) has to submit a P&R request in each country to ensure patient access of a new ATMP.
The P&R request was not submitted for all ATMPs in each of the EU5 countries: (i) no request for Imlygic submission in France, Spain and Italy; (ii) no submission for Strimvelis in France; (iii) no submission for Spherox in Italy and France (Table 3).
All ATMPs were assessed as medicines and followed the “traditional” appraisal procedure in each country, except for Germany. In Germany, the Federal Joint Committee (G-BA) first categorizes the ATMP either as a medicine or a medical procedure. If the ATMP has pharmacologic properties and its clinical outcome is not dependent on the healthcare professional skills, it is categorized as a medicine and undergoes the benefit assessment procedure according to the AMNOG (Arzneimittelmarktneuordnungsgesetz, Medicine Market Reorganization Act), where discounts on list prices determined by the MAH are negotiated on the grounds of different variables, including the added therapeutic value. Otherwise, it is categorized as a medical procedure and is normally assessed by the PEI (Paul-Ehrlich-Institut) [34,35,36,37]. Spherox and Holoclar were evaluated via the medical procedure; all other ATMPs underwent the AMNOG process (Table 3).
In United Kingdom, the National Institute for Health and Care Excellence (NICE) evaluates ATMPs through two different HTA processes: the STA (Single Technology Appraisal) or the HSTP (Highly Specialised Technologies Programme). The STA is used for products targeting non-rare diseases and relies on cost–effectiveness analysis (CEA); the HSTP evaluates products for ultra-rare diseases, allowing a higher Incremental Cost–Effectiveness Ratio (ICER) threshold [38]. Among the most recently appraised ATMPs, Kymriah and Yescarta have been evaluated through STA, while Strimvelis and Luxturna by HSTP. Zynteglo and Zolgensma are currently under assessment through STA and HSTP, respectively. Alofisel received a negative recommendation.
In France, medicinal products are assessed and appraised by the Transparency Committee (TC) of the Haute Autorité de Sante (HAS). If the Service Médical Rendu (SMR, absolute clinical value) of a drug is considered sufficient, the medicine can be granted reimbursement and then evaluated for its Amélioration du Service Médical Rendu (ASMR, additional clinical value). ASMR is a driver for price negotiation with the Comité Économique des Produits de Santé (CEPS, Committee for Healthcare Products). The ASMR rating, assigned by TC, ranges from I (maximum, revolutionary therapy) to V (minimum, no superiority versus standard of care) [39,40,41]. Patient access to a new product is possible also before MA with the Authorization for Temporary Use (ATU). To date, Kymriah, Yescarta, and Zolgensma obtained ATU; the ATU for Zolgensma is the only one currently active. During the ATU period, the MAH is allowed to set a launch price before the negotiation with the CEPS.
In Spain, the Agencia Española de Medicamentos y Productos Sanitarios (AEMPS) performs a clinical assessment of new medicinal products and then the General Directorate for Medicines of MoH (Dirección General de Cartera Básica de Servicios del Sistema Nacional de Salud y Farmacia, DGCBSF) prepares a price proposal. Negotiation of the proposal occurs between the Price Committee (Comisión Interministerial de Precios de Medicamentos y Productos Sanitarios, CIPM) and the MAH [42]. The final price is the maximum reimbursable price nationwide, subject to further reduction by hidden discounts negotiated by the Regions [43], due to the fact that the Spanish Healthcare System is decentralized and each Region has the authority to re-negotiate the prices.
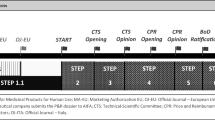
In Italy, the assessment and appraisal process is managed by the Italian Medicines Agency (Agenzia Italiana del Farmaco, AIFA), through its Scientific Technical Committee (Commissione Tecnico Scientifica, CTS) and its Price and Reimbursement Committee (Comitato Prezzi e Rimborso, CPR). The CTS evaluates the clinical added value, the place in therapy of the new medicine and possible price comparators. In the case of a positive opinion, the CPR negotiates with the MAH the price and any MEAs [44]. If the product is reimbursed and the price is negotiated at a national level, a request for inclusion in the regional and/or hospital therapeutic lists has to be submitted. The MAH may also ask for the recognition of the “innovative status” of the medicinal product. Innovativeness is appraised on the grounds of three criteria: unmet medical need, added therapeutic value and quality of available evidence and lasts maximum 3 years [45]. Innovative medicines benefit from dedicated funds and immediate access to regional lists, and they are not subject to temporary price reductions by law. Currently, only three ATMPs (Strimvelis, Kymriah, and Yescarta), have been granted this status (for Strimvelis the innovativeness status has expired).
Only Chimeric Antigen Receptor-T cells (CAR-Ts) therapies are reimbursed in all the EU5 while the decisions regarding other products are quite heterogeneous (Table 3).
List prices, on the other hand, are substantially aligned across all the EU5 (Table 3), despite in Italy, Spain and France they are negotiated together with the reimbursements status, whereas in Germany and England prices are freely determined by the relevant MAH, but indirectly regulated (in Germany a discount is negotiated after 1 year of marketing; in England a threshold range for the incremental cost–effectiveness is set, thus addressing pricing strategies by the pharmaceutical companies).
ATMPs were also quite disruptive for MEAs trends in almost all the EU5. Outcome-based agreements, in the form of performance-linked reimbursement, had never been signed centrally in Spain before a “payment at result” for the two CAR-Ts; in Italy, a similar agreement as the one above for the two CAR-Ts was signed, despite the outcome-based agreements being gradually substituted by simple discounts. An instalment plan, with 315,000 € paid up front and four additional annual payments only if the treatment continues to be effective, was applied for Zynteglo in Germany [46]. In England, NICE has created a Cancer Drug Fund (CDF), as a time-limited managed access agreement, which guarantees a faster and temporary reimbursement for cancer medicines, conditioned by evidence-based results which allow a routine appraisal. The two CAR-Ts were included in the CDF, due to the uncertainty of their benefit and cost–effectiveness profiles.
Germany and France adopted extra-cost coverage systems to support the management of ATMPs in hospitals. In Germany, when a medicine is used in a hospital setting and its price is not totally covered by an existing diagnosis-related group (DRG) fee, it is possible apply for an extra-budgetary reimbursement, the NUB (Neue Untersuchungs- und Behandlungsmethoden, new examination and treatment method). A status of NUB 1 is granted to a medicine or procedure which is new, innovative, for a low number of patients and which requires higher resource use (other than that covered by the DRG); this means that an extra-coverage can be negotiated by hospitals [47, 48]. In France, an additional 15,000€ (fixed) was added to the current DRG fee exclusively for Kymriah and Yescarta (Table 3).
As far as other polices that affect patients access to ATMPs, in most cases, the accreditation criteria for centre selection are established by the National Authorities, usually through the JACIE (Joint Accreditation Committee ISCT-Europe and EBMT) accreditation process and with the involvement of multidisciplinary medical teams [49,50,51,52,53]. In England, the National Health Service has been working with the JACIE and life sciences companies to get centres up and running. In Spain, for CAR-T, a group of experts for the definition of criteria for designation of centres was established. In Italy, the accreditation process is usually managed by the regional governments, regulated by the minimum criteria for centres' selection drawn up by AIFA for ATMPs.
Pipeline analysis
According to the previously mentioned inclusion and exclusion criteria, 6,982 trials were identified. After the exclusion of duplicates and all studies not targeting ATMPs, 249 clinical trials were included in the final analysis.
Out of these, 181 (73%) are conducted on cell therapies (CAR-Ts included), 59 (24%) on gene therapies, and 9 (4%) on tissue engineering products. One hundred and twenty-two (49%) trials are actively ongoing and recruiting, 76 (31%) not yet recruiting, and 51 (20%) have been completed (Fig. 1).
Clinical trial analysis according to type (a) and status (b). The current ATMP pipeline analysed retrieved clinical trials on ATMPs from the clinicaltrials.gov database and selecting with the following inclusion criteria: interventional studies, phase II/, II/III and III studies, ongoing or completed studies, 1/07/2017–1/7/2019 as temporal limitation, and Directive 2001/83/EC plus Committee for Advanced Therapies algorithm used as definition of “ATMP”. Of 249 clinical trials included in the final analysis (after exclusion of duplicates and those not targeting ATMPs), 181 (73%) were conducted on cell therapies (CAR-Ts included), 59 (24%) on gene therapies, and 9 (4%) on tissue engineering products (figure a), while 122 (49%) were actively ongoing and recruiting, 76 (31%) not yet recruiting, and 51 (20%) completed (figure b)
Ninety-three trials (37%) were funded by companies, 114 (46%) through other sources, and 42 (17%) were co-funded by companies and other organizations (Fig. 2).
Funding of clinical trials with ATMPs. The current ATMP pipeline analysed retrieved clinical trials on ATMPs from the clinicaltrials.gov database and selecting with the following inclusion criteria: interventional studies, phase II/, II/III and III studies, ongoing or completed studies, 1/07/2017–1/7/2019 as temporal limitation, and Directive 2001/83/EC plus Committee for Advanced Therapies algorithm used as definition of “ATMP”. Of 249 clinical trials included in the final analysis (after exclusion of duplicates and those not targeting ATMPs), 93 (37%) were funded by companies, 114 (46%) through other sources, and 42 (17%) were co-funded by companies and others
The main target of ATMPs under development are oncological and onco-haematological diseases (110; 44%), followed by cardiovascular (35; 14%) and immunological (17; 7%) diseases.
The study target was a rare disease in only 114 (46%) trials, while the target disease was not rare in the remaining 135 (54%) (Fig. 3).
Therapeutic area (a) and disease rarity (b) of ATMPs clinical trials. The current ATMP pipeline analysed retrieved clinical trials on ATMPs from the clinicaltrials.gov database and selecting with the following inclusion criteria: interventional studies, phase II/, II/III and III studies, ongoing or completed studies, 1/07/2017–1/7/2019 as temporal limitation, and Directive 2001/83/EC plus Committee for Advanced Therapies algorithm used as definition of “ATMP”. Of 249 clinical trials included in the final analysis (after exclusion of duplicates and those not targeting ATMPs), 110 (44%) were on oncological and onco-haematological diseases, 35 (14%) on cardiovascular diseases and 17 (7%) on immunological diseases (figure a), while 114 (46%) on a rare disease, and the remaining 135 (54%) on not rare one (figure b)
Discussion
This paper aimed at comparing assessment, appraisal and P&R process for ATMPs in the main European countries and whether this process is consistent with the expert recommendations currently available.
This study shows similar common patterns. ATMPs follow the same procedure already in place for other medicinal products in all countries, with the exception of Germany. Since the medicines P&R process is different across countries, this makes the reimbursement status of ATMPs heterogenous, with the exception of CAR-T therapies, which have been granted reimbursement in all countries due to the high expectations of their clinical benefits. Furthermore, for some ATMPs, request for P&R was not submitted in all countries. List prices tend to remain aligned in order to avoid cross-reference pricing. Our results also indicate that outcome-based MEAs and discounts are extensively used due to the uncertainty on the risk–benefit profile of ATMPs and their sustainability over time, respectively. This makes net prices divergent from list prices. Comparison of discounts on net prices is not possible as they are not published in any of the EU5 countries, with the exception of Germany. Additional funding for managing ATMPs was provided only in Germany (through the ordinary process of NUB classification) and in France (15,000 € for each DRG) for CAR-Ts alone.
Assessment and appraisal for P&R are partially aligned with the expert recommendations. Payers show a higher availability to draw up outcome-based MEAs, centrally or locally. On the other hand, other expert recommendations have not been applied systematically: ad hoc additional coverage for ATMP administration and patient management was provided only in France, with limited funding. The two delayed payments at results MEAs in Spain and Italy differ from each other both in terms of payment schemes as well as evaluated overall outcome. To date, no country has applied annuity payments, apart from Germany (and one product). We did not find concrete evidence of anticipated early dialogue among stakeholders or a more holistic evaluation of the social impact of these diseases considering the avoided productivity loss.
Pipeline analysis showed that the role of ATMP-based therapy is rapidly evolving from a niche-based setting in rare diseases to a vaster application in diseases which involve larger target populations. In this potential scenario of aiding a larger population, the impact on budget will be higher, if unitary prices remain very high as they are for current ATMPs.
Conclusions
The P&R process for ATMPs in the largest European countries is similar to the one adopted for other medicines. This is aligned to what experts have recommended, i.e. not creating an “ad hoc” framework for P&R of ATMPs, but adapting the assessment and appraisal processes for medicines to ATMPs.
However, some recommendations have not been sufficiently pursued, by domestic payers, including the suggestion of: (i) promoting early dialogue among HTA bodies, payers, the industry, and other stakeholders; (ii) considering, more than for other medicines, the long-term impact and using societal perspective in determining value for money and impact on budget; (iii) introducing annuity payment schemes, which would mean to actually turn the current expenditure into investment.
For the future, since many new ATMPs are going to be launched for non-rare diseases, it is important (i) evaluating in advance the organizational impact of ATMPs and providing health-care centres with the necessary resources; (ii) estimating the budget impact of ATMPs through an appropriate horizon scanning activity; and (iii) implementing a price/volume trade-off strategy or prioritizing patients who can benefit more from treatment according to clinical data.
Availability of data and materials
Not applicable.
Abbreviations
- AEMPS:
-
Agencia Española de Medicamentos y Productos Sanitarios
- AIFA:
-
Agenzia Italiana del Farmaco
- AMNOG:
-
Arzneimittelmarktneuordnungsgesetz
- ASMR:
-
Amélioration du Service Médical Rendu
- ATMPs:
-
Advanced Therapy Medicinal Products
- ATU:
-
Authorization for Temporary Use
- CAR-T:
-
Chimeric Antigen Receptor-T cell
- CAT:
-
Committee for Advanced Therapies
- CDF:
-
Cancer Drugs Fund
- CEA:
-
Cost-Effectiveness Analysis
- CEPS:
-
Comité économique des produits de santé
- CIPM:
-
Comisión Interministerial de Precios de Medicamentos y Productos Sanitario
- CPR:
-
Comitato Prezzi e Rimborso
- CTS:
-
Commissione Tecnico Scientifica
- DGCBSF:
-
Dirección General de Cartera Básica de Servicios del Sistema Nacional de Salud y Farmacia
- DRG:
-
Diagnosis-Related Group
- EMA:
-
European Medicine Agency
- EU:
-
European Union
- EU5:
-
European Major five (Germany, United Kingdom, France, Spain, Italy)
- HAS:
-
Haute Autorité de Sante
- HSTP:
-
Highly Specialised Technologies Programme
- HTA :
-
Health Technology Assessment
- ICER:
-
Incremental Cost–Effectiveness Ratio
- IPT:
-
Informe de Posicionamiento Terapéutico
- JACIE:
-
Joint Accreditation Committee ISCT-Europe and EBMT
- MA:
-
Marketing Authorization
- MAH:
-
Marketing Authorisation Holder
- MEA:
-
Managed Entry Agreement
- MoH:
-
Ministry of Health
- NICE:
-
National Institute for Health and Care Excellence
- NUB:
-
Neue Untersuchungs—und Behandlungsmethoden
- P&R:
-
Pricing and Reimbursement
- PEI:
-
Paul-Ehrlich-Institut
- SMR:
-
Service Médical Rendu
- STA:
-
Single Technology Appraisal
- TC:
-
Transparency Committee
References
Official Journal of the European Union. Regulation (EC) No 1394/2007 of the European Parliament and of the Council of 13 November 2007 on advanced therapy medicinal products and amending Directive 2001/83/EC and Regulation (EC) No 726/2004. https://ec.europa.eu/health//sites/health/files/files/eudralex/vol-1/reg_2007_1394/reg_2007_1394_en.pdf. Accessed Oct 2019.
Jonsson B, et al. Advanced therapy medicinal products and health technology assessment principles and practices for value-based and sustainable healthcare. Eur J Health Econ. 2019;20(3):427–38.
Drummond MF, et al. Analytic considerations in applying a general economic evaluation reference case to gene therapy. Value Health. 2019;22(6):661–8.
Garrison LP, et al. Value-based pricing for emerging gene therapies: the economic case for a higher cost-effectiveness threshold. J Manag Care Spec Pharm. 2019;25(7):793–9.
Hettle R, et al. The assessment and appraisal of regenerative medicines and cell therapy products: an exploration of methods for review, economic evaluation and appraisal. Health Technol Assess. 2017;21(7):1–204.
Marsden G, Towse A, Pearson SD, et al. Gene therapy: understanding the science, assessing the evidence, and paying for value. Research Paper, OHE&ICER March 2017. https://www.ohe.org/publications/gene-therapy-understanding-science-assessing-evidence-and-paying-value. Accessed Oct 2019.
Gemeinsamer Bundesausschuss. https://www.g-ba.de/. Accessed Dec 2019.
National Institute for Health and Care Excellence – NICE. https://www.nice.org.uk//. Accessed Dec 2019.
Haute Autorité de santé—HAS. https://www.has-sante.fr//. Accessed Dec 2019.
Agence Nationale de Sécurité du Médicament et des Produits de Santé—ANSM. https://www.ansm.sante.fr/Recherche/. Accessed Dec 2019.
Legifrance, le service public de la diffusion du droit par l'Internet. https://www.legifrance.gouv.fr/. Accessed Dec 2019.
Agencia Española de Medicamentos y Productos Sanitarios - AEMPS. https://www.aemps.gob.es//. Accessed Dec 2019.
Agenzia Italiana del Farmaco—AIFA. https://www.aifa.gov.it/archivio?strutture=96918/. Accessed Dec 2019.
Gazzetta Ufficiale. https://www.gazzettaufficiale.it//. Accessed Dec 2019.
Hanna E, et al. Advanced therapy medicinal products: current and future perspectives. J Mark Access Health Policy. 2016. https://doi.org/10.3402/jmahp.v4.31036.
Committee for Advanced Therapies (CAT)—Reflection paper on classification of advanced therapy medicinal products. 2015. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2015/06/WC500187744.pdf. Accessed Dec 2019.
Orphanet. The portal for rare diseases and orphan drugs. https://www.orpha.net/consor/cgi-bin/index.php?lng=EN. Accessed Jul 2020.
European Medicine Agency (EMA)—Development of medicines for rare diseases. https://www.ema.europa.eu/en/news/development-medicines-rare-diseases. Accessed Dec 2019.
Holoclar (ex vivo expanded autologous human corneal epithelial cells containing stem cells). European public assessment report (EPAR). EMA https://www.ema.europa.eu/en/medicines/human/EPAR/holoclar. Accessed Jul 2020.
Imlygic (talimogene laherparepvec). European public assessment report (EPAR). EMA. https://www.ema.europa.eu/en/medicines/human/EPAR/imlygic. Accessed Jul 2020.
Strimvelis (autologous CD34+ enriched cell fraction that contains CD34+ cells transduced with retroviral vector that encodes for the human ADA cDNA sequence). European public assessment report (EPAR). EMA. https://www.ema.europa.eu/en/medicines/human/EPAR/strimvelis. Accessed Jul 2020.
Spherox (spheroids of human autologous matrix-associated chondrocytes). European public assessment report (EPAR). EMA. https://www.ema.europa.eu/en/medicines/human/EPAR/spherox. Accessed Jul 2020.
Alofisel (darvadstrocel). European public assessment report (EPAR). EMA. https://www.ema.europa.eu/en/medicines/human/EPAR/alofisel. Accessed Jul 2020.
Kymriah (tisagenlecleucel). European public assessment report (EPAR). EMA. https://www.ema.europa.eu/en/medicines/human/EPAR/kymriah. Accessed Jul 2020.
Yescarta (axicabtagene ciloleucel). European public assessment report (EPAR). EMA. https://www.ema.europa.eu/en/medicines/human/EPAR/yescarta. Accessed Jul 2020.
Luxturna (voretigene neparvovec). European public assessment report (EPAR). EMA. https://www.ema.europa.eu/en/medicines/human/EPAR/luxturna. Accessed Jul 2020.
Zynteglo (betibeglogene autotemcel). European public assessment report (EPAR). EMA. https://www.ema.europa.eu/en/medicines/human/EPAR/zynteglo. Accessed Jul 2020.
Zolgensma (onasemnogene abeparvovec). European public assessment report (EPAR). EMA. https://www.ema.europa.eu/en/medicines/human/EPAR/zolgensma. Accessed Jul 2020.
ChondroCelect (characterised viable autologous cartilage cells expanded ex vivo expressing specific marker proteins). European public assessment report (EPAR). EMA. https://www.ema.europa.eu/en/medicines/human/EPAR/chondrocelect. Accessed Jul 2020.
Glybera (alipogene tiparvovec). European public assessment report (EPAR). EMA. https://www.ema.europa.eu/en/medicines/human/EPAR/glybera. Accessed Jul 2020.
Provenge (autologous peripheral-blood mononuclear cells activated with prostatic acid phosphatase granulocyte-macrophage colony-stimulating factor (sipuleucel-T)). European public assessment report (EPAR). EMA. https://www.ema.europa.eu/en/medicines/human/EPAR/provenge. Accessed Jul 2020.
Maci (matrix-applied characterised autologous cultured chondrocytes). European public assessment report (EPAR). EMA. https://www.ema.europa.eu/en/medicines/human/EPAR/maci. Accessed Jul 2020.
Zalmoxis (allogeneic T cells genetically modified with a retroviral vector encoding for a truncated form of the human low affinity nerve growth factor receptor (ΔLNGFR) and the herpes simplex I virus thymidine kinase (HSV-TK Mut2)). European public assessment report (EPAR). EMA. https://www.ema.europa.eu/en/medicines/human/EPAR/zalmoxis. Accessed Jul 2020.
Hecken J. ATMP im G‐BA zwischen AMNOG und Methodenbewertung 2018. https://www.mdk-wl.de/fileadmin/MDK-Westfalen-Lippe/user_upload/Hecken_atmp_im_g-ba.pdf. Accessed Oct 2019.
Cassel D, Ulrich V. AMNOG-Daten 2018 - Funktionsweise und Ergebnisse der Preisregulierung für neue Arzneimittel in Deutschland: Bundesverband der Pharmazeutischen Industrie e. V. (BPI); 2018. https://www.bpi.de/fileadmin/user_upload/Downloads/Publikationen/AMNOG-Daten/AMNOG-Daten-2018.pdf. Accessed Oct 2019.
Theidel U, von der Schulenburg JM. Benefit assessment in Germany: implications for price discounts. Health Econ Rev. 2016;6(1):33.
GKV-Spitzenverband. Rahmenvereinbarung nach § 130b Abs. 9 SGB V 2016. [cited 2019 October]; Available from: https://www.gkv-spitzenverband.de/media/dokumente/krankenversicherung_1/arzneimittel/rahmenvertraege/pharmazeutische_unternehmer/Rahmenvereinbarung_130b_Abs9__SGB_V_2016.pdf. Accessed Oct 2019.
Brockis E, Marsden G, Cole A, Devlin N. A review of NICE methods across health technology assessment programmes: differences, justifications and implications. Office of Health Economics. April 2016. https://www.ohe.org/system/files/private/publications/NICE%20HTA%20methods%20RP%20FINAL_0.pdf. Accessed Oct 2019.
Remuzat C, et al. Market access pathways for cell therapies in France. J Mark Access Health Policy. 2015. https://doi.org/10.3402/jmahp.v3.29094.
Chevreul K, et al. France: health system review. Health Syst Transit. 2015;17(3):1–218, xvii.
Cour des comptes -Sécurité sociale 2017 – Chapitre 3: La fixation du prix des médicaments des résultats significatifs, des enjeux toujours majeurs d’efficience et de soutenabilité, un cadre d’action à fortement rééquilibrer. https://www.ccomptes.fr/sites/default/files/2017-09/20170920-rapport-securite-sociale-2017-fixation-prix-medicaments.pdf. Accessed Oct 2019.
AEMPS. Propuesta de colaboración para la elaboración de los informes de posicionamiento terapéutico de los medicamentos. https://www.aemps.gob.es/medicamentosUsoHumano/informesPublicos/docs/propuesta-colaboracion-informes-posicionamiento-terapeutico.pdf. Accessed Oct 2019.
Miniserio de Sanidad C y BS. Comisión Interministerial de precios de medicamentos y productos sanitarios. https://www.mscbs.gob.es/profesionales/farmacia/CIPMyPS.htm. Accessed Oct 2019.
Jommi C, Minghetti P. Pharmaceutical pricing policies in Italy. In: Babar ZUD, editor. Pharmaceutical prices in the 21st century. Cham: Adis; 2015.
Scavone C, Capuano A, Rossi F. New criteria of Italian Medicine Agency for the attribution of therapeutic innovation: viewpoint of the pharmacologist. Giornale Italiano di Farmacoeconomia e Farmacoutilizzazione. 2017;9(3):5–12.
TIF. Bluebird puts €1.58m price on gene therapy Zynteglo. https://thalassaemia.org.cy/it/news/bluebird-puts-e1-57m-price-on-gene-therapy-zynteglo/. Accessed Jul 2020.
GKV-Spitzenverband. Neue Untersuchungs- und Behandlungsmethoden (NUB) 2019. https://www.gkv-spitzenverband.de/krankenversicherung/krankenhaeuser/drg_system/neue_untersuchungs_und_behandlungsmethoden_nub/neue_untersuchungs_und_behandlungsmethoden_nub.jsp. Accessed Oct 2019.
Institut für das Entgeltsystem im Krankenhaus (InEK GmbH). Neue Untersuchungs- und Behandlungsmethoden (NUB) 2019. https://www.g-drg.de/G-DRG-System_2019/Neue_Untersuchungs-_und_Behandlungsmethoden_NUB. Accessed Oct 2019.
legifrance.gouv.fr. JORF n°0085 du 10 avril 2019. texte n° 21.Arrêté du 28 mars 2019 limitant l'utilisation de médicament de thérapie innovante à base de lymphocytes T génétiquement modifiés dits CAR-T Cells autologues indiqués dans le traitement de la leucémie aiguë lymphoblastique à cellules B et/ou du lymphome à grande cellule B, à certains établissements de santé en application des dispositions de l'article L. 1151–1 du code de la santé publique. https://www.legifrance.gouv.fr/eli/arrete/2019/3/28/SSAH1909328A/jo/texte. Accessed Oct 2019.
Ministerio de Sanidad C y BS. Criterios y estándares para la designación de centros para utilización de CAR-T en Linfoma Difuso de Células B grandes recidivante o refractario y en Leucemia linfoblástica aguda de células B refractaria en el sistema nacional de salud. https://www.mscbs.gob.es/profesionales/farmacia/pdf/20190304_Criterios_Estandares_Desig_Centros_CAR_T.pdf. Accessed Oct 2019.
Osservatorio Terapie Avanzate. CAR-T: arrivano i nomi dei primi centri accreditati in Italia. 11 Ottobre 2019. https://www.osservatorioterapieavanzate.it/regolatorio/car-t-arrivano-i-nomi-dei-primi-centri-accreditati-in-italia. Accessed Oct 2019.
DETERMINA 7 agosto 2019. Regime di rimborsabilita' e prezzo del medicinale per uso umano «Kymriah». (Determina n. 1264/2019). (19A05147) (GU Serie Generale n.188 del 12–08–2019). https://www.gazzettaufficiale.it/eli/id/2019/08/12/19A05147/SG. Accessed Oct 2019.
NHS—CAR-T Therapy. https://www.england.nhs.uk/cancer/cdf/car-t-therapy/. Accessed Nov 2019.
Acknowledgements
The authors would like to thank Gilead Sciences, Inc. for providing an unrestricted grant for this study. The authors thank Dr. Ulrike Kuchenbecker, Dr. Paul Miller, Dr. Francis Fagnani, and Dr. Xavier Badia for the contribution to get information about Germany, United Kingdom, France, and Spain, respectively.
Funding
Meetings to elaborate and discuss the manuscript were organized by MAP Provider Srl that received consultation fee from Gilead Sciences, Inc.
Author information
Authors and Affiliations
Contributions
VR, MD, EL, PLC, CJ contributed equally to this work. All authors participated in the research setting, carried out the reaseach, analyzed the results, and contributed to the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable
Competing interests
The authors Prof. P.L. Canonico and Prof. C. Jommi declare no conflict of interest on the topics covered by the present paper. The authors Dr. V. Ronco, Dr. Myriam Dilecce, and Dr. E. Lanati and declare that they have no direct relationship with Gilead Sciences, Inc. which has provided an unconditional contribution to this paper realization. However, they highlight that Gilead Sciences, Inc. has existing consultancy relationships with MA Provider Srl, which provides services for the pharmaceutical and healthcare sector, where the undersigned hold the role of Managing Director and Senior Pricing Manager respectively.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ronco, V., Dilecce, M., Lanati, E. et al. Price and reimbursement of advanced therapeutic medicinal products in Europe: are assessment and appraisal diverging from expert recommendations?. J of Pharm Policy and Pract 14, 30 (2021). https://doi.org/10.1186/s40545-021-00311-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40545-021-00311-0