Abstract
Background
Measuring access to medicines has often been limited to assessing availability and affordability, while little is known regarding other dimensions of access including geographical accessibility. Our study aims to provide a systematic review of literature on the accessibility of medicines by studying the geographical distribution of pharmacies using Spatial Analytical methods.
Methods
As systematic review of scientific peer-reviewed literature between 2000 and 2018 was carried out using PubMed, Web of Science, Google Scholar, Google and the Preferred Reporting items for Systematic Reviews and Meta-Analyses (PRISMA). Data regarding pharmacy density, distance to pharmacies in relation of pharmacy to sociodemographic factors and pharmacy characteristics were extracted from studies that meet the inclusion criteria.
Findings
Twenty papers fulfilled our inclusion criteria, of which only three were from middle income countries and rest from high-income economies. Pharmacy density per population was reported in 15 studies. Although geographical information was utilized in all studies, only 14 studies reported distance to pharmacies represented as Euclidean (straight line) distance. Disparities in accessibility was reported according to population income and rural or urban location. Seven studies described additional pharmacy characteristics including opening hours, presence of a pharmacist and delivery services.
Conclusions
Geographical accessibility is a key dimension of access to medicines. Pharmacy density per population is a relevant indicator to assess geographical accessibility which should be complemented by an equity analysis using socio-demographic information and population perception of accessibility.
Similar content being viewed by others
Introduction
Medicines play an integral part of health system [1]. Target 3.8 of SDG 3 is: ‘to achieve universal health coverage, including financial risk protection, access to quality essential healthcare services and access to safe, effective, quality and affordable essential medicines and vaccines for all’ [2]. Access to medicines is essential to improve the health outcome and achieving universal health care coverage [1]. Lack of access to medicines can result in increased preventable morbidity and mortality, loss of economic income and increased poverty. One of the main access points of medicines are pharmacies and other private sector outlets [3]. Pharmacies not only provide medicines but often offer primary care services, advice and consultation regarding common ailments which helps to improve the overall health of the population [4].
Penchansky’s and Thomas’ [5] concept of access states availability, accessibility, accommodation, affordability and acceptability as the different dimensions of access. Measuring access has often been limited to two of these five dimensions, namely availability and affordability. For instance, Target 3.b of the SDGs is measured as the proportion of health facilities that have a core set of relevant essential medicines available and affordable on a sustainable basis [2]. However, equally important for achieving access is geographical accessibility, commonly measured as geographical distribution of pharmacies within a region and density of pharmacies per population [6]. This is also reflected by the fact that the geographical location of residency is a core dimension when measuring health equities [7].
With developing technologies, we can identify geographical distribution of pharmacies within a region, by mapping pharmacies using spatial methods to determine the areas of pharmacy deserts and the areas of high pharmacy density [6]. However, the literature on geographical distribution of pharmacies is sparse. An exception is the study of pharmacy density in Chicago and the relation between their distribution and socio-economic characteristics of the neighborhood [8]. Our study aims to provide a systematic review of literature on the evidences available for geographical distribution of pharmacies across countries and their relationship between pharmacy density and other sociodemographic factors. This study contributes to the existing body of knowledge of measuring geographical accessibility of medicines (Additional file 1).
Methods
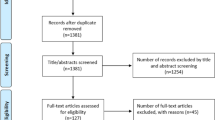
This study follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [9].
Data collection
Original studies describing the geographical distribution of pharmacies were included. We included articles from all countries regardless of the funding source of the study. The review timeline was restricted to 18 years (2000–2018) and only studies published in English.
A search strategy that combines key words “geographic distribution”,” spatial analysis”,” maps” and “pharmacy” was applied to PubMed and Web of Science (see Appendix 1 for the search terms). Additionally, we did open Google Scholar searches using the combination of terms outlined in Appendix 1. Duplicated articles were removed. We excluded articles that discussed the access to medicines but had no mention regarding the geographical distribution of pharmacies. Geographical distribution of pharmacies represented in any format (e.g.—maps and graphical representation) were included. Both qualitative and quantitative studies were included. The full text papers were assessed against the inclusion criteria by one researcher and those identified as relevant was checked again by another researcher.
Data extraction
Data from the included studies were then extracted into an excel database under the following headings: author, title, year and location of the study, objective of the study, type of pharmacy described- whether public or private, sampling and study design, pharmacy data collection source, pharmacy census validation, pharmacy density per 10,000 population, distance to pharmacies on relation to population, description of pharmacies based on urban/rural regions, ethnicity, socio-economic status and description of pharmacy characteristics. We classified study countries based on income according to World Bank Country classification [10]. If a study did not provide sufficient information to assess bias (e.g. no data on sampling and pharmacy data sources) it was excluded. Type of pharmacy was described as public if it was run by the government and private if it was run by an independent or chain pharmacy. Studies were classified as ‘national’ and ‘local’ depending on the region of data presented. If the data was presented for the entire country, we considered them as ‘national’ and if the data was presented for a state/city in a country, we considered it to be ‘local’. Data sources for pharmacies and population were identified and listed. We considered the pharmacy census to be validated if the data obtained were cross-checked by either visiting pharmacies in person or making phone call to certain pharmacy to check the accuracy of the data obtained from the sources. Ethnicity was described in some studies based on the population of pharmacy’s neighborhood. Socio-economic status was accounted for as described by each study using the countries deprivation indices and registries. Pharmacy characteristics such as hours of operation, presence of pharmacists, prescription medication delivery services, in-store medication availability and medicines price described were extracted and synthesized.
Data analysis
While the units of pharmacy density varied across studies, we retrieved and converted them to per 10,000 population to compare results across studies. Distance to pharmacies were described as mentioned in original studies, due to different units in which they were reported aggregation and comparison between studies was not feasible. While some studies measured distance to pharmacies based on population, some studies measured distance between two pharmacies. Studies that further described differences in distribution of pharmacies according to urban–rural regions, ethnicity and socio-economic status was identified. Key emergent themes recurring across the data were analyzed and a narrative review was conducted.
Results
Pubmed database search resulted in 3528 papers and Web of Science resulted in 2806 papers, which was narrowed to 4676 after removing duplicates. 176 articles were selected on the basis of title screen, 20 articles were identified based on the inclusion criteria. Only 3 of those studies are from lower middle- and upper middle-income countries (Brazil, India and South Africa) [6, 11, 12], the rest are from high income countries. Data from high income economies are available from countries namely New Zealand [13], England[14, 15], Scotland [16], Italy [17], Portugal[18], Canada [19, 20] and United States [8, 21,22,23,24,25,26,27,28]. Studies reported the geographical distribution of pharmacies, in terms of population density, rural and urban areas, characteristics and policy guidelines in the region.
The characteristics of studies included in the review are presented in Table 1. While the majority (n = 18) of the studies were observation, using census pharmacy data with geographical mapping, two studies [12, 16] did a cross-sectional survey to map the distribution of pharmacies in Scottish Highlands and India respectively. Except two studies from United States before 2010, most studies (n = 17) were conducted after 2010 making use of more developed geographical information systems. The term community pharmacies was employed in most of the papers. Table 1 stratifies the community pharmacies into public and private pharmacies.
Table 2 outlines the methodology and results described in papers. Data reported were available both at national (n = 5) and local (n = 15) levels. While some studies (n = 11) obtained pharmacy data from the country’s department of health, studies from England used Fuse Geo-Health Care Access Database, studies from Canada used college of pharmacist’s data, two studies [12, 21] conducted cross-sectional surveys to identify pharmacies, two studies [16, 22] conducted surveys after obtaining data from a data-base. Ikram et al. [23] did not report the data source of pharmacy in their paper. Six studies conducted validation of pharmacy data and one study [24] used an internally validated database.
With respect to population, all studies (n = 20) utilized the latest available country’s population census. Pharmacy density data was reported in 15 studies. While Qato et al. [25] reported the density of pharmacies per square mile and Qato et al. [8] reported the density of pharmacies per census tract, other studies (n = 13) reported data based on population. Comparatively high pharmacy density per 10,000 population in Lisbon [18], Nova Scotia [19] and Ontario [20] respectively.
Geographical Information System (e.g. Arc GIS Software) was used for any necessary geo-processing in all the studies [29]. However, distance to pharmacies was reported only in 14 studies. The rest of the studies [6, 11, 14, 15], [26], [27] did not report the pharmacy distance even while using GIS software. While majority studies reported distance to pharmacies based on population accessibility, the study from India [12] reported data based on pharmacy distance from health care providers, the study from the UK [8, 14] reported pharmacy distance between two pharmacies. Studies that measured the distance of pharmacies in relation to population represented the data in Euclidean distance (straight line distance) from the center of the measured radius containing the population. Hot spot analysis, which is a spatial analysis technique used to identify clusters of high and low value, was used by one study [28] to measure accurate distance of pharmacies using their address and population address.
Studies (n = 11) differentiated the pharmacy density based on urban and rural areas according to country census classification. All studies concluded urban population have better access to pharmacies and shorter distances to travel. The study conducted in Lisbon [18], Portugal, found pharmacy deserts even in parts of urbanized corridors of Lisbon.
Some studies [21, 23, 24, 28] (n = 4) differentiated pharmacy density based on ethnicity. Interestingly the reports from these studies contrast each other. While Ikram et al. [23] and Pednekar et al. [28] found pharmacy deserts in areas with higher white population, Qato et al. [25] and Chisholm-Burns et al. [21] reported pharmacy deserts in areas of segregated black and Hispanic community.
Studies (n = 8) also differentiated pharmacy densities based on their socio-economic status. The majority of studies identified pharmacy deserts among population of lower socio-economic status. Conversely, two studies [13, 28] identified higher income communities within pharmacy deserts.
Several studies [12, 14,15,, 21, 22, 25, 27, 28] described pharmacy characteristics along with accessibility. Interestingly, two of them [21, 27] also surveyed the pricing information of medications and reported the data. Pharmacy characteristics described are hours of operation, pharmacists available, prescription medication delivery services, in-store medication availability and affordability. Appendix 3 describes the details of pharmacy characteristics.
Four studies [21, 22, 27, 28] described hours of operation in the pharmacies. They reported that the least populated area typically reported fewer hours per week. Although the study from India [12] and one study conducted in the US [21] described the availability of pharmacists in a pharmacy, the findings related to socioeconomic level of the population were not significant to arrive at a conclusion. Three studies from the US [21, 22, 28] reported data on prescription delivery services. It is important to note that all articles were representing different regions in United States and such services were not described in any middle-income economies. Two of these studies [12, 28] also described details on medication availability. While Sabde et al. [12] identified no difference in availability in urban and rural pharmacies, Pednekar et al. [28] reported 15% of pharmacies had at least one item out of stock. Two studies [21, 27] in the US collected data on affordability. However, it was hard to synthesize the data across studies due to different methods of measuring prices.
Discussion
This systematic review fills an important gap in our knowledge on geographical accessibility of pharmacies and contributes to develop measures for access to medicine. While the majority of the studies are from high income economies, pharmacy accessibility is particularly relevant in low- and middle- income countries since transportation can be expensive and difficult to access. The absence of studies from low- and middle-income countries could possibly be attributed to the challenges of maintaining an up-to-date pharmacy census with limited resources in these nations. The study team in India [12] addressed the challenge of the lack of a census by walking through a geographically defined area and identifying pharmacies, whichis a resource intensive method.
The majority of the studies measured the distance based on the ‘centroid’ approach, which considers the center of the geospatial unit (e.g., zip code, census block) and measures the straight line (also known as Euclidean distance) distance to the nearest pharmacy. As outlined by Pednekar et al. [28], this may lead to errors in measurement as the actual distance required to travel to pharmacy might be less or more depending on the geography of the surrounding land. Although Ikram et al. [23] explains that distance measured in ArcGIS software is an underestimate compared to Google Maps and the data can be correlated, with improving access to Google Maps technology and hot spot analysis, we recommend further studies to determine the actual distance instead of using the centroid approach. Some studies measure pharmacy distance to assess density in terms of population and other studies measure distance between two pharmacies. Standardized measure of representation of pharmacy density such as pharmacy per 10,000 people would allow for uniformity and comparability.
Perception is another important factor to assess accessibility. However, only one study analyzed perception of distance. Rushworth et al. [16] found that those in the most remote areas and those who prescribed five or more regular medicines were more likely to report inconvenience of access to prescribed medicines. While only 63.7% found traveling to pharmacy to be easy, 84.3% found access to pharmacies convenient. This shows that people’s perception of easy access to pharmacies also depends on other factors like number of prescribed medicines, mobility and reliance on others.
Finally, it would be important to correlate the different access dimensions including geographical distribution to measure access to medicines more comprehensively. As mentioned by Penchansky and Thomas, access is multi-dimensional. Higher density of pharmacy is found in urban areas and increased pharmacy density is associated with increased access to medicines. High income areas were noted to have increased access to pharmacies except for two studies [13, 28], which noted pharmacy deserts in higher median income regions. Amitslavski et al. [27] found significant difference and very limited stock and hours of operation of pharmacies in poor communities compared to those of wealthier communities. They also explained that higher odds of common medications being out of stock in poorer communities might be due to high poverty and low rates of prescription insurance coverage. Home medication delivery services, as mentioned by Chisholm-Burns et al. [21], would be a feasible option to explore in areas where access is limited. Overall, access to pharmacy appears sparse in low income and rural regions and measures to expand pharmacy access based on actual distance in those populations would be beneficial.
Limitations
Literature searches were restricted to PubMed, Web of Science and Google Scholar and did not use other search engines. Although comprehensive search terminology was used, there might be some articles that were missed. Literature was searched only in English language. While attempts to draw conclusion was made with regards to the distance and geographical distribution of pharmacies in various countries, heterogeneity in reporting on this measure reduced the ability to summarize trends and establish patterns. Studies were conducted in different countries with differences in cultures and health care system which affects consumer perception.
Conclusion
Geographical accessibility of pharmacies is one of the key dimensions of access to medicines. Disparities between rural and urban populations is an important challenge. The literature is scarce on studies assessing accessibility of medicines in particular in low- and middle- income countries. Expanding our knowledge on geographical access of pharmacies will enable us to provide better access to medicines, moving a step closer towards providing universal health coverage.
Availability of data and materials
All data for analysis in this review is in the public domain.
References
Wirtz VJ, Hogerzeil HV, Gray AL, Bigdeli M, de Joncheere CP, Ewen MA, et al. Essential medicines for universal health coverage. Lancet. 2016;389(10067):403–76.
Pacific WHORO for the W. Sustainable development goals (SDGs) : Goal 3. Target 3.8 : Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines [Internet]. Manila : WHO Regional Office for the Western Pacific; 2016. http://iris.wpro.who.int/handle/10665.1/12880
Silverman R, Madan Keller J, Glassman A, Chalkidou K. Tackling the Triple Transition in Global Health Procurement. Final report of CGD’s working group on the future of global health procurement. 2019. https://www.cgdev.org/sites/default/files/better-health-procurement-tackling-triple-transition.pdf
Joint FIP/WHO Guidelines on Good Pharmacy Practice. Standards for Quality of Pharmacy Services. WHO Tech Rep Ser. 2011;No. 961(Annex 8):20.
Penchansky R, Thomas JW. The Concept of Access: Definition and Relationship to Consumer Satisfaction. Med Care. 1981;19(2):127–40. http://www.jstor.org/stable/3764310
Ward K, Sanders D, Leng H, Pollock AM. Assessing equity in the geographical distribution of community pharmacies in South Africa in preparation for a national health insurance scheme. Bull World Health Organ. 2014;92(7):482–9. http://www.who.int/entity/bulletin/volumes/92/7/13-130005.pdf
Hosseinpoor AR, Bergen N, Magar V. Monitoring inequality: An emerging priority for health post-2015. Bull World Health Organ. 2015;93(9):591A.
Qato DM, Daviglus ML, Wilder J, Lee T, Qato D, Lambert B. “Pharmacy deserts” are prevalent in Chicago’s predominantly minority communities, raising medication access concerns. Health Aff. 2014;33(11):1958–65. https://doi.org/10.1377/hlthaff.2013.1397.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. http://www.bmj.com/content/339/bmj.b2535.abstract
World Bank Country and Lending Groups – World Bank Data Help Desk. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Accessed 17 May 2020
Emmerick ICM, Nascimento JM, Pereira MA, Luiza VL, Ross-Degnan D. Farmácia Popular Program: changes in geographic accessibility of medicines during ten years of a medicine subsidy policy in Brazil. J Pharm policy Pract. 2015;8(1):10. https://doi.org/10.1186/s40545-015-0030-x.
Sabde YD, Diwan V, Saraf VS, Mahadik VK, Diwan VK, De Costa A. Mapping private pharmacies and their characteristics in Ujjain district, Central India. BMC Health Serv Res. 2011;11(1):351. https://doi.org/10.1186/1472-6963-11-351.
Norris P, Horsburgh S, Sides G, Ram S, Fraser J. Geographical access to community pharmacies in New Zealand. Heal Place. 2014;12:65.
Todd A, Copeland A, Husband A, Kasim A, Bambra C. Access all areas? An area-level analysis of accessibility to general practice and community pharmacy services in England by urbanity and social deprivation. BMJ Open. 2015;5(5):e007328. https://doi.org/10.1136/bmjopen-2014-007328.
Todd A, Thomson K, Kasim A, Bambra C. Cutting care clusters: the creation of an inverse pharmacy care law? An area-level analysis exploring the clustering of community pharmacies in England. BMJ Open. 2018;8(7):e022109. https://doi.org/10.1136/bmjopen-2018-022109.
Rushworth GF, Cunningham S, Pfleger S, Hall J, Stewart D. A cross-sectional survey of the access of older people in the Scottish Highlands to general medical practices, community pharmacies and prescription medicines. Res Soc Adm Pharm. 2018;12:88.
Domnich A, Arata L, Amicizia D, Signori A, Gasparini R, Panatto D. Assessing spatial inequalities in accessing community pharmacies: a mixed geographically weighted approach. Geospat Health. 2016;11:3. http://geospatialhealth.net/index.php/gh/article/view/457
Padeiro M. Geographical accessibility to community pharmacies by the elderly in metropolitan Lisbon. Res Soc Adm Pharm. 2018;8:78.
Law MR, Heard D, Fisher J, Douillard J, Muzika G, Sketris IS. The geographic accessibility of pharmacies in Nova Scotia. Can Pharm J. 2013;146:39.
Law MR, Dijkstra A, Douillard JA, Morgan SG. Geographic accessibility of community pharmacies in ontario. Healthc Policy. 2011;6(3):36–46.
Chisholm-Burns MA, Spivey CA, Gatwood J, Wiss A, Hohmeier K, Erickson SR. Evaluation of racial and socioeconomic disparities in medication pricing and pharmacy access and services. Am J Heal Pharm. 2017;74(10):653–68. https://academic.oup.com/ajhp/article/74/10/653/5102533
Casey MM, Klingner J, Moscovice I. Pharmacy services in rural areas: is the problem geographic access or financial access? J Rural Health. 2002;18(3):467–77.
Ikram SZ, Hu Y, Wang F. Disparities in Spatial Accessibility of Pharmacies in Baton Rouge. Louisiana Geogr Rev. 2015;105(4):492–510. https://doi.org/10.1111/j.1931-0846.2015.12087.x.
Qato DM, Zenk S, Wilder J, Harrington R, Gaskin D, Alexander GC. The availability of pharmacies in the United States: 2007–2015. PLoS One. 2017;12(8):e0183172. https://doi.org/10.1371/journal.pone.0183172.
Qato DM, Wilder J, Zenk S, Davis A, Makelarski J, Lindau ST. Pharmacy accessibility and cost-related underuse of prescription medications in low-income Black and Hispanic urban communities. J Am Pharm Assoc. 2017;57(2):162-169.e1.
Lin S-J. Access to community pharmacies by the elderly in Illinois: a geographic information systems analysis. J Med Syst. 2004;28(3):301–9.
Amstislavski P, Matthews A, Sheffield S, Maroko AR, Weedon J. Medication deserts: survey of neighborhood disparities in availability of prescription medications. Int J Health Geogr. 2012;11(1):48. https://doi.org/10.1186/1476-072X-11-48.
Pednekar P, Peterson A. Mapping pharmacy deserts and determining accessibility to community pharmacy services for elderly enrolled in a State Pharmaceutical Assistance Program. PLoS One. 2018;13(6):e0198173. https://doi.org/10.1371/journal.pone.0198173.
Scott LM, Janikas MV. Spatial Statistics in ArcGIS. Handbook of Applied Spatial Analysis. Berlin: Springer; 2010. p. 27–41.
Acknowledgements
None.
Funding
This study did not receive any funding.
Author information
Authors and Affiliations
Contributions
VJW conceived the idea for the review. CTJ conducted the retrieval and data extraction under supervision of VJW. CTJ and VJW drafted the manuscript and revised it. Both authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
We declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
PRISMA Flow Diagram on Review Process.
Appendices
Appendix
Appendix 1: Search terms
GIS (AND) access (AND) medicines.
GIS (AND) Pharmacies.
Mapping (AND) medicines (AND) access (AND) Low- and middle-income countries.
Mapping (AND) pharmacies (AND) Low- and middle-income countries.
Mapping (AND) access (AND) medicines.
Mapping (AND) pharmacies (AND) developing countries.
Mapping (AND) pharmacy deserts.
geographic distribution of pharmacies.
geographic mapping of pharmacies.
geographic distribution (AND) access to medicines (AND) developing countries.
medicine access (AND) developing countries.
spatial analysis (AND) pharmacies.
spatial analysis (AND) pharmacies (AND) Low and middle income countries.
spatial analysis (AND) access to medicines.
spatial analysis (AND) access (AND) pharmacies.
maps (AND) medicine access.
Appendix 2: Inclusion criteria
-
Article published between 2000–2019
-
Available in PubMed, Web of Science and Google Scholar
-
Should represent geographical distribution of pharmacies in any format – maps, graphical representation
-
From any country
-
Qualitative or quantitative studies
Appendix 3: Pharmacy characteristics table
See Table
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tharumia Jagadeesan, C., Wirtz, V.J. Geographical accessibility of medicines: a systematic literature review of pharmacy mapping. J of Pharm Policy and Pract 14, 28 (2021). https://doi.org/10.1186/s40545-020-00291-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40545-020-00291-7