Abstract
Liraglutide is a glucagon-like peptide-1 (GLP-1) analog that has been utilized for the treatment of type 2 diabetes mellitus. Liraglutide at a higher dose also shows beneficial effects in weight loss, which prompted its widespread use as an anti-obesity drug. The potential of liraglutide to treat Alzheimer’s disease and cognitive impairment has also been suggested. Nevertheless, the pharmacokinetics of liraglutide, including its distribution to the brain, has not been fully characterized. Therefore, this study aimed to develop a simple and sensitive bioanalytical method using liquid chromatography–tandem mass spectrometry (LC–MS/MS) and determine the pharmacokinetics and brain distribution of liraglutide in rats. Liraglutide in the rat plasma and brain tissue homogenates was extracted by protein precipitation using methanol. A gradient elution profile was used for chromatographic separation with mobile phases comprising 0.3% formic acid in water and 0.3% formic acid in acetonitrile. The mass spectrometry was operated in the positive electrospray ionization with multiple reaction monitoring mode. The lower limit of quantification of the present LC–MS/MS was 1 ng/mL in the plasma and 2 ng/mL in the brain tissue. Following intravenous injection (0.05 mg/kg, n = 5), plasma concentrations of liraglutide decreased monoexponentially with an average half-life of 3.67 h. The estimated absolute bioavailability of liraglutide after subcutaneous injection was 13.16%. Brain distribution of liraglutide was not significant, with the tissue-to-plasma partition coefficient (Kp) of liraglutide less than 0.00031. However, the concentrations of liraglutide were significantly different in the different brain regions following IV injection. In the brain, liraglutide concentrations were the highest in the hypothalamus, followed by the cerebellum and cerebrum. The present LC–MS/MS assay and the pharmacokinetic results may be helpful to understand better the effect of liraglutide in the brain for further preclinical and clinical studies of liraglutide.
Similar content being viewed by others
Introduction
Glucagon-like peptide-1 (GLP-1) stimulates insulin secretion in response to blood glucose, thereby controlling blood glucose levels with a minimal adverse effect of hypoglycemia (Doyle and Egan 2007; Drucker and Nauck 2006). Nevertheless, its extremely short biological half-life of approximately 2 min hampers the clinical utility of intact GLP-1 for type 2 diabetes mellitus (T2DM) (Tahrani et al. 2010). Therefore, structural analogs of GLP-1 with extended biological half-life have been developed and become an emerging therapeutic class of drugs as an alternative to insulin drugs.
Liraglutide (Victoza®) is a GLP-1 analog with an extended half-life in which 16-carbon fatty acid is attached at Lys26, and Arg34 is replaced with Lys while maintaining the pharmacological activities comparable to native GLP-1 (Drucker and Nauck 2006; Chen et al. 2016). The structural modification protects liraglutide from metabolic degradation by dipeptidyl peptidase-4 (DPP-4), which is responsible for the rapid elimination of GLP-1 (Jacobsen et al. 2016). Moreover, liraglutide binds to serum albumin, which further reduces the metabolism possibly by preventing the enzyme binding, and decreases renal elimination (Jacobsen et al. 2016; Deacon 2009). Thus, liraglutide has a half-life of 10–14 h after subcutaneous injection in humans and is administered once daily for the treatment of T2DM (Drucker and Nauck 2006; Jacobsen et al. 2016).
In addition, liraglutide has extra benefits in weight loss, which motivates its use in treating obesity (Nuffer and Trujillo 2015). The mechanism by which liraglutide exerts weight loss is attributed to its combinatorial effects on the brain and the gut. While stimulating insulin and suppressing glucagon secretion, liraglutide inhibits gastric emptying as well as increases satiety and reduces appetite by binding to the GLP-1 receptors in the brain (Nuffer and Trujillo 2015; Shah and Vella 2014; Turton et al. 1996). Thus, high-dose liraglutide (Saxenda®) was approved for the treatment of obesity by the US Food and Drug Administration, which became the most widely prescribed anti-obesity drug in 2020 (Neeland et al. 2021).
Furthermore, liraglutide has shown promising effects in treating Alzheimer’s disease and cognitive impairments, which are also likely to be mediated by GLP-1 receptors in the brain. After peripheral injection, liraglutide reduced plaque formation, protected memory and synaptic plasticity, and decreased inflammation in the mouse model of Alzheimer’s disease (McClean et al. 2011). Improvement in spatial working memory and restoration of episodic memory was also observed (Vargas-Soria et al. 2021).
As the indication of liraglutide is being expanded, the side effects associated with liraglutide at higher as well as lower doses also need to be considered carefully. The most frequently observed adverse effects of liraglutide are gastrointestinal symptoms. Other side effects include increased levels of serum lipase and amylase, risk of acute pancreatitis, gallbladder or biliary disease, liver disease, and kidney disease (Seo 2021). Thus, it is important to determine the proper dosing regimen according to the pharmacokinetics as well as the patient’s condition.
Nevertheless, the pharmacokinetics of liraglutide, particularly its distribution to the brain, has not been fully characterized. So far, most pharmacokinetic studies of liraglutide, like those of other peptide and protein drugs, have relied on enzyme-linked immunosorbent assays (ELISA) (Jacobsen et al. 2016; Agerso et al. 2002). Despite the high sensitivity, ligand binding assays (LBA), including ELISA methods in general, have disadvantages in their application in pharmacokinetic studies (Dong et al. 2018; Meng et al. 2017; Pinho et al. 2019). Due to the failure to discern if the epitope is present in the parent or metabolite, as well as inherent cross-reactivity, ELISA may overestimate the concentrations of the parent drug. Moreover, ELISA is susceptible to a significant matrix effect, which makes it difficult to be applied to another biological matrix for tissue distribution studies. Potential penetration of liraglutide across the blood–brain barrier was indicated by the determination of the liraglutide content in the brain via ELISA after intraperitoneal injection in mice (Hunter and Holscher 2012). Nevertheless, ELISA assay only allowed relative comparison of brain levels of liraglutide after saline injection and liraglutide injection instead of measuring its actual concentrations in the brain (Hunter and Holscher 2012). Direct assessment of brain distribution of liraglutide by quantifying its exact concentration in the brain has never been pursued.
Moreover, a variety of research is ongoing toward the development of its analogs or other GLP-1 receptor agonists. The development of longer-acting and different types of dosage forms for liraglutide and other GLP-1 receptor analogs are of particular interest (Chen et al. 2016; Meng et al. 2017). For example, dissolving microneedle-assisted drug delivery system (Rabiei et al. 2021), longer-acting liraglutide precursor peptide (Ahmadi et al. 2022), and controlled release thermogel formulation of liraglutide (Chen et al. 2016) have been reported. The development of formulations with reduced frequency of injection and better patient compliance would further protract the therapeutic utility of liraglutide. For the research on new formulations and analogs of liraglutide, a robust bioanalytical method, as well as rigorous pharmacokinetic evaluation, is highly required.
Recently, liquid chromatography–tandem mass spectrometry (LC–MS/MS) assay has become a promising alternative to LBAs for the bioanalysis of peptides and protein drugs. LC–MS/MS has fundamental advantages, including high sensitivity, specificity, reproducibility, and high throughput, and serves as the most favorable bioanalytical technique for pharmacokinetic studies. Recent advances in LC–MS/MS have been overcoming its limitations of poor ionization, significant endogenous interference, and low sensitivity in the bioanalysis of peptides and proteins (Dong et al. 2018; Meng et al. 2017; Pinho et al. 2019; Ewles and Goodwin 2011). There are several LC–MS/MS methods available for the determination of liraglutide in the plasma (Dong et al. 2018; Meng et al. 2017; Sauter et al. 2019; Zhai et al. 2020). However, no LC–MS/MS methods have been reported to determine liraglutide concentrations in the tissues.
Therefore, the purpose of this study was to develop a simple and sensitive LC–MS/MS analysis for the quantification of liraglutide in the plasma as well as in the brain tissue. The LC–MS/MS analysis was fully validated in two different biological matrices and allowed to evaluate the pharmacokinetics and brain distribution of liraglutide in rats. The developed bioanalysis and its pharmacokinetic information may be helpful in better understanding its action for further preclinical and clinical studies.
Materials and methods
Materials
Liraglutide (99.2%) was purchased from Chengdu Shengnuo Biopharm Co., Ltd (Chengdu, China). Semaglutide (98%), which was used as the internal standard (IS), was purchased from Zhejiang Peptites Biotech Co., Ltd (Hangzhou, China). Formic acid was a product of Sigma-Aldrich Co. (St. Louis, MO). Other reagents, including methanol, acetonitrile, and distilled water, were all high-performance liquid chromatography (HPLC)-grade and purchased from J.T. Baker, Inc. (Phillipsburg, NJ).
Stock solutions, calibration standards, and quality control samples
The stock solution of liraglutide (1 mg/mL) was prepared by dissolving 5 mg of liraglutide in 5 mL of methanol. The stock solution of liraglutide was serially diluted with methanol, yielding standard working solutions of 1000, 500, 100, 50, 10, 5, 2, and 1 ng/mL for plasma and 200, 100, 50, 20, 10, 5, and 2 ng/mL for brain tissue homogenates. Similarly, IS working solution at 50 ng/mL was prepared by diluting the IS stock solution (1 mg/mL) with methanol.
To prepare calibration samples of liraglutide in the plasma, 50 µL of the rat blank plasma was spiked with 50 µL of the liraglutide standard working solution, and 50 µL of the IS working solution (50 ng/mL) in a 1.5 mL Protein LoBind Tubes® (Eppendorf, Hamburg, Germany). To prepare calibration samples in the brain tissue, 50 µL of the rat brain tissue homogenate was spiked with 50 µL of the liraglutide standard working solution and 50 µL of the IS working solution (50 ng/mL). Following the addition of 150 µL of methanol as a precipitation solvent, the mixture was mixed on a vortex mixer for 1 min and centrifuged at 15,000 × g for 10 min. An aliquot of 10 µL of the supernatant was injected onto the LC–MS/MS.
Quality control (QC) samples were prepared to provide four concentration levels, i.e., high, medium, low, and the lower limit of quantification (LLOQ), of liraglutide based on the calibration standard ranges for each biological matrix by using the same procedure as the calibration standards. QC concentration levels were 800, 80, 4, and 1 ng/mL for the plasma matrix, and 160, 40, 8, and 2 ng/mL for the brain tissue homogenates.
Sample preparation
An aliquot of 50 µL of biological samples, i.e., rat plasma or brain tissue homogenates, was mixed with 50 µL of IS working solution (50 ng/mL) and 200 µL of methanol. After vortexing for 1 min, the mixture was centrifuged at 15,000 × g for 10 min. An aliquot of 10 µL of the supernatant was injected onto the LC–MS/MS for analysis.
LC–MS/MS
The LC–MS/MS analysis of liraglutide was performed on an LC–MS/MS system consisting of Agilent 1260 HPLC (Agilent Technologies, Santa Clara, CA) and Agilent 6490 mass spectrometer (Agilent Technologies). Chromatographic separation was performed on a bioZen™ 2.6 µm Peptide XB-C18 (100 × 2.1 mm, Phenomenex, Torrence, CA) by using gradient elution. The mobile phase consisted of 0.3% formic acid in distilled water (MP-A) and 0.3% formic acid in acetonitrile (MP-B). The gradient elution profile and flow rate are shown in Table 1. The total run time was 15 min, and the column oven temperature was set at 50 °C.
The electrospray ionization (ESI) source was operated in the positive mode. The mass spectrometer was conducted in the multiple reaction monitoring (MRM) mode with a dwell time of 200 ms per MRM channel. For MRM analysis, the MS parameters were set as follows: gas temperature, 350 °C; gas flow, 17 L/min; nebulizer gas pressure, 40 psi. The transition m/z ions for MRM analysis were selected as follows: 938.5 → 1063.7 for liraglutide and 1029.4 → 1302.9 for semaglutide. The fragment voltage was 380 V for both liraglutide and IS. The collision energy was set at 24 eV for liraglutide and 38 eV for IS. MassHunter Quantitative Analysis (Agilent Technologies) was used to process the mass spectrometric data.
Assay validation
The assay was validated following the guidance published by US FDA (US FDA 2018) to demonstrate the specificity, sensitivity, linearity, accuracy, precision, extraction recovery, and stability. Specificity was evaluated by comparing the blank biological matrix, i.e., rat plasma and brain tissue homogenates, spiked with the liraglutide and IS to the blank biological matrix. The linearity of the method was evaluated over the concentration ranges of 1–1000 ng/mL in the rat blank plasma and 2–200 ng/mL in the brain tissue homogenates. The calibration curve for each biological matrix was constructed from the peak area ratios of liraglutide to IS versus theoretical concentration via the weighted regression method (1/x).
Accuracy and precision were determined by assaying the three replicates of matrix-matched QC samples on the same day (intra-day) and three consecutive days (inter-day). Accuracy was calculated as the percentage of the mean back-calculated concentration compared to the nominal concentration. Precision was defined as the coefficient of variance for each concentration. The extraction recovery was calculated by comparing the peak responses of liraglutide and IS in the biological matrices spiked before and after the extraction. The stability was examined under four different conditions as follows: short-term, 4 h at room temperature; long-term, 7 days at − 70 °C; autosampler, 24 h in the autosampler; freeze/thaw, 3 freeze/thaw cycles. All stability data were expressed as the percentage of the mean response of the QC samples for stability tests vs. those of the freshly prepared samples.
Application to in vivo studies
The animal study protocol was approved by the Ethics Committee for the Treatment of Laboratory Animals at Sungkyunkwan University (SKKUIACUC2021-09-01-2) and conducted in accordance with the standard operating procedures (SOPs).
Pharmacokinetic studies
Male Sprague–Dawley rats (7 weeks, 194–238 g; DBL, Eumseong, Korea) were fasted overnight before drug administration. Liraglutide dissolved in normal saline was administered by intravenous (IV) injection via penile vein at 0.05 mg/kg (n = 5) or subcutaneous (SC) injection at 1 mg/kg (n = 5). The injection volume was 0.5 mL/kg and 1 mL/kg for IV and SC injection, respectively. Approximately 0.3 mL of the venous blood samples was collected at 0.25, 0.5, 1, 1.5, 2, 3, 4, 6, 8, 12, 24, and 36 h after drug administration directly from the jugular vein. Plasma samples were obtained by centrifugation of the blood samples at 15,000 × g for 10 min. The obtained plasma samples were immediately frozen and stored at − 70 °C until analysis.
Brain distribution studies
For brain distribution studies, liraglutide (1 mL/kg) was administered via IV injection at 5 mg/kg or SC injection at 500 mg/kg. Brain tissues were excised at 1 h after IV injection or 12 h after SC injection of liraglutide (n = 6, each). From the excised brain, parts of the brain, i.e., cerebrum, cerebellum, and hypothalamus, were separated, accurately weighed, and homogenized (Tissue Tearor, Biospec Products Inc., Bartlesville, OK) with appropriate volumes of isotonic saline. The tissue homogenates were stored at − 70 °C until analysis.
Data analysis
The plasma concentration vs. time data were analyzed by a non-compartmental method to obtain the pharmacokinetic parameters of liraglutide. The bioavailability was calculated as the ratio of dose-normalized area under the plasma concentration–time curve (AUCinf) after SC injection and IV injection, i.e., Bioavailability = (AUCsc/Dosesc)/(AUCiv/Doseiv). The tissue-to-plasma partition coefficient (Kp) was calculated by the ratio of liraglutide concentration in the brain tissue homogenates to that in the plasma.
Statistical analysis
Statistical analyses were performed using one-way ANOVA. Comparisons among different groups were followed using Tukey post hoc analysis. Differences with p < 0.05 were denoted as statistically significant.
Results and discussion
An LC–MS/MS assay was developed and validated for quantifying liraglutide concentrations in rat plasma as well as brain tissue. The application of the LC–MS/MS method was demonstrated through in vivo pharmacokinetic studies to characterize the pharmacokinetics and brain distribution of liraglutide after IV and SC injections in rats.
Sample preparation
Liraglutide, like other peptides, is susceptible to adsorption to plastic or glass wares, which provides one of the major challenges for the development of bioanalytical method. Since adsorption is mostly unpredictable or more prominent at the lower concentrations, peptide adsorption results in unreliable and unreproducible results in the analysis (Verbeke et al. 2020). The linearity of the working standard solutions of liraglutide in the biological matrix is often poor due to the strong peptide adsorption (Dong et al. 2018). Thus, we utilized Protein LoBind Tubes® (Eppendorf) during the sample preparation and optimized the subsequent analytical procedures to minimize the peptide adsorption. By using the low adsorption tubes, the impact of nonspecific adsorption of liraglutide could be minimized.
To extract liraglutide from the plasma samples, simple protein precipitation with methanol was used. Compared to solid-phase extraction which has been applied in previous studies (Meng et al. 2017; Shah et al. 2017), protein precipitation is advantageous because it is rapid, simple, less labor-intensive, and economically favorable. Initially, acetonitrile was tested as a precipitation solvent from the rat biological samples for liraglutide. However, the use of acetonitrile resulted in poor sensitivity and recovery, likely due to the coprecipitation of liraglutide with plasma and tissue proteins (Dong et al. 2018). Thus, methanol was selected as a precipitation solvent, resulting in over 92.17% recovery for liraglutide and over 92.61% for IS from the rat plasma and brain homogenates.
LC–MS/MS conditions
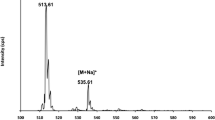
As the molecular weight of liraglutide is large (m.w. = 3751.2), multiply charged precursor ions are often selected for MRM analysis (Dong et al. 2018; Meng et al. 2017; Sauter et al. 2019; Zhai et al. 2020). In the present study, the most abundant precursor ion in the positive Q1 mass scan spectrum was [M + 4H]4+ at m/z 938.5 for liraglutide and [M + 4H]4+ at m/z 1029.4 for IS (semaglutide). Figure 1 shows the product ion mass spectra of protonated liraglutide and IS. The most prominent fragment ion was m/z 1063.7 of the protonated liraglutide, and m/z 1302.9 for protonated IS. The m/z 1063.7 fragment of [M + 4H]4+ at m/z 938.5 for liraglutide has been suggested as the doubly charged C-terminal fragment after cleavage of the peptide bond between positions 15 and 16 (Sauter et al. 2019). Therefore, the MRM transitions of m/z 938.5 → 1063.7 for liraglutide and m/z 1029.4 → 1302.9 for IS were monitored. The selected MRM transition of liraglutide is consistent with literature reports (Meng et al. 2017; Sauter et al. 2019).
Chromatographic conditions were optimized to achieve the best chromatographic resolution of liraglutide with minimum matrix interference. BioZen™ 2.6 µm Peptide XB-C18 (100 × 2.1 mm, Phenomenex) column with a mobile phase consisting of 0.3% formic acid in distilled water and 0.3% formic acid in acetonitrile was finally selected, which led to a symmetric and sharp peak shape and less endogenous interference. However, significant carryover was observed with the isocratic elution, probably due to the adsorption of liraglutide to the parts of the LC–MS/MS system. The gradient elution profile was therefore employed and optimized to prevent inconsistent carryover (Table 1). The gradient profile in which the gradual increase of the organic phase for 9 min followed by a quick return to the initial condition led to reproducible peak response. Representative MRM chromatograms of liraglutide and IS in the biological matrices are shown in Fig. 2. The retention times of liraglutide and IS in the rat plasma were 6.0 min and 5.5 min, respectively, in both plasma and brain tissue.
Representative chromatograms of liraglutide (left) and IS (right) obtained from A blank plasma, B blank brain tissue, C LLOQ concentration of liraglutide and IS in the plasma, D LLOQ concentration of liraglutide and IS in the brain tissue, E ULOQ concentration of liraglutide and IS in the plasma, and F ULOQ concentration of liraglutide and IS in the brain tissue
Method validation
Specificity, linearity, and sensitivity
Examination of the blank matrix and blank matrix spiked with liraglutide at LLOQ and upper limit of quantification (ULOQ) indicated no interfering endogenous or exogenous peaks at the retention times corresponding to liraglutide and IS (Fig. 2). The calibration curve of liraglutide was linear over the calibration standard concentration range from 1 to 1000 ng/mL in the plasma and 2–200 ng/mL in the brain tissue homogenates with a correlation coefficient > 0.999. The LLOQ of liraglutide was 1 ng/mL in the plasma and 2 ng/mL in the brain tissue homogenates, which were defined as the lowest concentration in the calibration range. The sensitivity of liraglutide in the rat plasma in this study is compatible with previous studies with LLOQ of 1 ng/mL (Meng et al. 2017; Zhai et al. 2020) or 0.5 ng/mL (Dong et al. 2018). The present method provided sufficient sensitivity to evaluate the pharmacokinetics and tissue distribution of liraglutide in rats.
Accuracy and precision
Table 2 shows the accuracy and precision determined by using matrix-matched QC samples at four different concentration levels for rat plasma and brain tissue homogenates. The intra- and inter-day accuracies were 92.09–106.36% in the plasma and 91.91–105.19% in the brain tissue. The intra- and inter-day precisions were within 10.99% and 12.52% in the plasma and brain tissue, respectively. The obtained accuracy and precision of the current assay satisfied the FDA guidance on bioanalytical methods validation (US FDA 2018).
Extraction recovery
The extraction recovery was calculated as the ratio of the average peak area obtained from three replicates of standard solutions at each QC concentration level spiked in pre-extraction to those in post-extraction. Table 3 summarizes the calculated extraction recovery of liraglutide and IS in the rat plasma and brain tissue. The extraction recovery in the plasma was 92.17–104.59% for liraglutide and 92.61% for IS. The extraction recovery in the brain tissue was 94.09–99.76% for liraglutide and 95.76% for IS. These extraction recoveries indicated that the extraction of liraglutide in the rat plasma was efficient and reproducible.
Stability
The stability evaluation of liraglutide determined under four different storage conditions, i.e., short-term, long-term, autosampler, and freeze/thaw cycles, is summarized in Table 4. The average stability of liraglutide was 96.93–111.61% in the plasma and 86.60–109.38% in the brain tissue, with no significant deviations in all the tested conditions. These data demonstrated that liraglutide was stable for application in the routine analysis.
Pharmacokinetics of liraglutide in rats
The developed LC–MS/MS assay was applied to in vivo pharmacokinetic studies of liraglutide to assess the pharmacokinetics and bioavailability of liraglutide in rats. Figure 3 shows the obtained plasma concentration vs. time profiles following IV and SC injections of liraglutide in rats. The non-compartmental pharmacokinetic parameters of liraglutide are summarized in Table 5.
Following IV injection, plasma concentrations of liraglutide showed a mono-exponential decline with an average half-life of 3.67 ± 0.40 h. After SC injection, liraglutide plasma concentration gradually increased and reached its peak concentration at 2.00–6.00 h, then decreased with an average half-life of 3.55 ± 0.51 h. The obtained half-life of liraglutide is well comparable with the literature-reported half-life of liraglutide in rats, i.e., 3.95–4.01 h (Dong et al. 2018; Zhai et al. 2020). In humans, the slow absorption with Tmax of about 12 h and extended half-life (approximately 13 h) of liraglutide were more recognizable (Jacobsen et al. 2016), which is compatible in beagle dogs (Sauter et al. 2019). Finally, the absolute bioavailability of liraglutide after SC injection was 13.16% in rats.
Brain distribution of liraglutide in rats
It has been suggested that the benefits of liraglutide for weight loss and Alzheimer’s disease are associated with GLP-1 receptors in the brain (McClean et al. 2011; Farr et al. 2016; Adams et al. 2018; Lee and Kim 2020). However, there is limited information regarding the distribution of liraglutide to the brain. Although it has been reported that liraglutide crosses the blood–brain barrier, but to a lesser extent than lixisenatide (Hunter and Holscher 2012), the brain distribution of liraglutide has never been directly evaluated by measuring its exact concentration in the brain.
Therefore, the potential utility of this LC–MS/MS assay to evaluate the brain distribution of liraglutide has been demonstrated by in vivo tissue distribution studies. As the literature suggested (Hunter and Holscher 2012), brain concentration of liraglutide was only detectable after high doses of liraglutide either by IV (5 mg/kg) or SC (500 mg/kg) injections. Table 6 and Fig. 4 show the liraglutide concentration in the different brain regions at 1 h after IV (5 mg/kg) or 12 h after SC (500 mg/kg) injections in rats. The tissue concentrations are presented in ng/g tissue, which was calculated as the measured concentration in the tissue homogenate by LC–MS/MS (ng/mL) divided by the density of tissue homogenate (g tissue/mL) (Song et al. 2022). The corresponding plasma concentration was 102,801.74 ± 6627.17 ng/mL and 181,525.94 ± 8838.02 ng/mL after IV and SC injections, respectively.
Brain distribution of liraglutide in rats represented by A brain concentration and B tissue-to-plasma partition coefficient (Kp) following intravenous (IV) injection and C brain concentration, and D Kp following subcutaneous (SC) injection in rats (mean ± SD, n = 6). †p < 0.05 versus cerebrum; *p < 0.05 versus cerebrum and cerebellum
Following either IV or SC injection, the brain tissue-to-plasma partition coefficient (Kp) of liraglutide was estimated as less than 0.00031, indicating the insignificant distribution of liraglutide to the brain. On the other hand, the concentrations of liraglutide were different in the different regions of the brain. In the brain, liraglutide concentrations were the highest in the hypothalamus, followed by the cerebellum and cerebrum. Significant distribution of liraglutide to the hypothalamus compared to other brain regions is consistent with the previous studies using labeled liraglutide in mice (Secher et al. 2014; Gabery et al. 2020). Following peripheral injection of labeled liraglutide, i.e., liraglutideVT750, the signal intensity of liraglutideVT750 had distributed primarily to circumventricular organs and parts of the hypothalamus (Secher et al. 2014; Gabery et al. 2020).
Conclusions
Although LBAs have been widely used for the bioanalysis of therapeutic peptides and proteins, a more robust analytical method is highly encouraging for pharmacokinetic studies. Due to the intrinsic high selectivity and specificity, LC–MS/MS has been recognized as a promising alternative for analyzing peptide and protein drugs. This study provides a simple and selective LC–MS/MS assay for the quantification of a therapeutic peptide, liraglutide, in the plasma as well as brain. By applying simple protein precipitation and chromatographic optimization, this assay resulted in sufficient sensitivity for in vivo pharmacokinetic studies. The absolute bioavailability of liraglutide was 13.16% following SC injections in rats. Although the distribution of liraglutide to the brain was not significant, the concentrations of liraglutide were different among different parts of the brain in rats. The concentration of liraglutide in the hypothalamus was the highest compared to other brain regions. To the best of our knowledge, this is the first report of direct assessment of brain distribution of liraglutide, which may help better understand its action in the brain. We believe the present LC–MS/MS assay and the pharmacokinetic information of liraglutide may be helpful for the preclinical and clinical studies.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
References
Adams JM, Pei H, Sandoval DA, Seeley RJ, Chang RB, Liberles SD, et al. Liraglutide modulates appetite and body weight through glucagon-like peptide 1 receptor-expressing glutamatergic neurons. Diabetes. 2018;67(8):1538–48.
Agerso H, Jensen LB, Elbrond B, Rolan P, Zdravkovic M. The pharmacokinetics, pharmacodynamics, safety and tolerability of NN2211, a new long-acting GLP-1 derivative, in healthy men. Diabetologia. 2002;45(2):195–202.
Ahmadi S, Shahsavani MB, Tavaf Z, Albaghlany RM, Kumar A, Moosavi-Movahedi AA, et al. A novel strategy for production of liraglutide precursor peptide and development of a new long-acting incretin mimic. PLOS ONE. 2022;17(5):e0266833.
Chen Y, Li Y, Shen W, Li K, Yu L, Chen Q, et al. Controlled release of liraglutide using thermogelling polymers in treatment of diabetes. Sci Rep. 2016;6(1):31593.
Deacon CF. Potential of liraglutide in the treatment of patients with type 2 diabetes. Vasc Health Risk Manag. 2009;5(1):199–211.
Dong S, Gu Y, Wei G, Si D, Liu C. Determination of liraglutide in rat plasma by a selective liquid chromatography-tandem mass spectrometry method: application to a pharmacokinetics study. J Chromatogr B Analyt Technol Biomed Life Sci. 2018;1091:29–35.
Doyle ME, Egan JM. Mechanisms of action of glucagon-like peptide 1 in the pancreas. Pharmacol Ther. 2007;113(3):546–93.
Drucker DJ, Nauck MA. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet. 2006;368(9548):1696–705.
Ewles M, Goodwin L. Bioanalytical approaches to analyzing peptides and proteins by LC–MS/MS. Bioanalysis. 2011;3(12):1379–97.
Farr OM, Sofopoulos M, Tsoukas MA, Dincer F, Thakkar B, Sahin-Efe A, et al. GLP-1 receptors exist in the parietal cortex, hypothalamus and medulla of human brains and the GLP-1 analogue liraglutide alters brain activity related to highly desirable food cues in individuals with diabetes: a crossover, randomised, placebo-controlled trial. Diabetologia. 2016;59(5):954–65.
Gabery S, Salinas CG, Paulsen SJ, Ahnfelt-Ronne J, Alanentalo T, Baquero AF, et al. Semaglutide lowers body weight in rodents via distributed neural pathways. JCI Insight. 2020;5(6).
Hunter K, Holscher C. Drugs developed to treat diabetes, liraglutide and lixisenatide, cross the blood brain barrier and enhance neurogenesis. BMC Neurosci. 2012;13:33.
Jacobsen LV, Flint A, Olsen AK, Ingwersen SH. Liraglutide in type 2 diabetes mellitus: clinical pharmacokinetics and pharmacodynamics. Clin Pharmacokinet. 2016;55(6):657–72.
Lee H, Kim E. Repositioning medication for cardiovascular and cerebrovascular disease to delay the onset and prevent progression of Alzheimer’s disease. Arch Pharm Res. 2020;43(9):932–60.
McClean PL, Parthsarathy V, Faivre E, Holscher C. The diabetes drug liraglutide prevents degenerative processes in a mouse model of Alzheimer’s disease. J Neurosci. 2011;31(17):6587–94.
Meng X, Xu H, Zhang Z, Fawcett JP, Li J, Yang Y, et al. Differential mobility spectrometry tandem mass spectrometry with multiple ion monitoring for the bioanalysis of liraglutide. Anal Bioanal Chem. 2017;409(20):4885–91.
Neeland IJ, Marso SP, Ayers CR, Lewis B, Oslica R, Francis W, et al. Effects of liraglutide on visceral and ectopic fat in adults with overweight and obesity at high cardiovascular risk: a randomised, double-blind, placebo-controlled, clinical trial. Lancet Diabetes Endocrinol. 2021;9(9):595–605.
Nuffer WA, Trujillo JM. Liraglutide: a new option for the treatment of obesity. Pharmacotherapy. 2015;35(10):926–34.
Pinho AR, Fortuna A, Falcao A, Santos AC, Seica R, Estevens C, et al. Comparison of ELISA and HPLC-MS methods for the determination of exenatide in biological and biotechnology-based formulation matrices. J Pharm Anal. 2019;9(3):143–55.
Rabiei M, Kashanian S, Bahrami G, Derakhshankhah H, Barzegari E, Samavati SS, et al. Dissolving microneedle-assisted long-acting Liraglutide delivery to control type 2 diabetes and obesity. Eur J Pharm Sci. 2021;167:106040.
Sauter M, Uhl P, Majewsky M, Fresnais M, Haefeli WE, Burhenne J. An ultrasensitive UPLC-MS/MS assay for the quantification of the therapeutic peptide liraglutide in plasma to assess the oral and nasal bioavailability in beagle dogs. Bioanalysis. 2019;11(9):887–98.
Secher A, Jelsing J, Baquero AF, Hecksher-Sorensen J, Cowley MA, Dalboge LS, et al. The arcuate nucleus mediates GLP-1 receptor agonist liraglutide-dependent weight loss. J Clin Invest. 2014;124(10):4473–88.
Seo YG. Side effects associated with liraglutide treatment for obesity as well as diabetes. J Obes Metab Syndr. 2021;30(1):12–9.
Shah M, Vella A. Effects of GLP-1 on appetite and weight. Rev Endocr Metab Disord. 2014;15(3):181–7.
Shah M, Reddy P, Reddy Y, Bhawanishankar M, Raja M, Pillai M. UHPLC-MS/MS determination of GLP-1 analogue, liraglutide a bioactive peptide in human plasma. 2017;4:304–11.
Song CH, Kim K, Kang E, Jeong B, Lee MS, Jung J, et al. Determination of pharmacokinetics and tissue distribution of a novel lutetium-labeled PSMA-targeted ligand, (177)Lu-DOTA-PSMA-GUL, in rats by using LC-MS/MS. Sci Rep. 2022;12(1):15452.
Tahrani AA, Piya MK, Kennedy A, Barnett AH. Glycaemic control in type 2 diabetes: targets and new therapies. Pharmacol Ther. 2010;125(2):328–61.
Turton MD, O’Shea D, Gunn I, Beak SA, Edwards CM, Meeran K, et al. A role for glucagon-like peptide-1 in the central regulation of feeding. Nature. 1996;379(6560):69–72.
US FDA. Bioanalytical method validation: guidance for industry. Silver Spring, MD2018.
Vargas-Soria M, Carranza-Naval MJ, Del Marco A, Garcia-Alloza M. Role of liraglutide in Alzheimer’s disease pathology. Alzheimers Res Ther. 2021;13(1):112.
Verbeke F, Bracke N, Debunne N, Wynendaele E, De Spiegeleer B. LC-MS compatible antiadsorption diluent for peptide analysis. Anal Chem. 2020;92(2):1712–9.
Zhai J, Li L, Dong L, Dong K, Xiang S, Gui L, et al. Simultaneous quantitative determination of liraglutide and insulin degludec in rat plasma by liquid chromatography-tandem mass spectrometry method and its application. Biomed Chromatogr. 2020;34(10):e4921.
Acknowledgements
Not applicable.
Funding
This work was supported by the Ministry of Trade, Industry and Energy of Korea Grant no. 20012631.
Author information
Authors and Affiliations
Contributions
EJP, THK, SS and BSS were involved in conceptualization; HSO, MC, THK, SS and BSS helped in methodology; HSO, MC, TSL, YA, EJP and BSS contributed to investigation; HSO, MC and BSS helped in writing—original draft preparation; SS and BSS helped in writing—review and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Eun Ji Park is an employee of D&D Pharmatech. No other potential conflicts of interest relevant to this article exist.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oh, H.S., Choi, M., Lee, T.S. et al. Pharmacokinetics and brain distribution of the therapeutic peptide liraglutide by a novel LC–MS/MS analysis. J Anal Sci Technol 14, 19 (2023). https://doi.org/10.1186/s40543-023-00382-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40543-023-00382-5