Abstract
Background
The burden of gastric cancer (GC) should be further clarified worldwide, and helped us to understand the current situation of GC.
Methods
In the present study, we estimated disability-adjusted life-years (DALYs) and mortality rates attributable to several major GC risk factors, including smoking, dietary risk, and behavioral risk. In addition, we evaluated the incidence rate and trends of incidence-based mortality (IBM) due to GC in the United States (US) during 1992–2018.
Results
Globally, GC incidences increased from 883,395 in 1990 to 1,269,805 in 2019 while GC-associated mortality increased from 788,316 in 1990 to 957,185 in 2019. In 2019, the age-standardized rate (ASR) of GC exhibited variations around the world, with Mongolia having the highest observed ASR (43.7 per 100,000), followed by Bolivia (34 per 100,000) and China (30.6 per 100,000). A negative association was found among estimated annual percentage change (EAPC) and ASR (age-standardized incidence rate (ASIR): r = − 0.28, p < 0.001; age-standardized death rate (ASDR): r = − 0.19, p = 0.005). There were 74,966 incidences of GC and 69,374 GC-related deaths recorded between 1992 and 2018. The significant decrease in GC incidences as well as decreasing trends in IBM of GC were first detected in 1994. The GC IBM significantly increased at a rate of 35%/y from 1992 to 1994 (95% CI 21.2% to 50.4%/y), and then begun to decrease at a rate of − 1.4%/y from 1994 to 2018 (95% CI − 1.6% to − 1.2%/y).
Conclusion
These findings mirror the global disease burden of GC and are important for development of targeted prevention strategies.
Similar content being viewed by others
Introduction
Gastric cancer (GC) ranks as the fifth most common malignant tumor in the world [1]. More than 70% of GC cases are reported in developing countries, of which, about 50% occur in East Asian countries, especially China, Japan, and Korea [1]. It is estimated that 26,380 cases of gastric cancer will be diagnosed in 2022 in the United States, and approximately 11,090 cancer-related deaths are expected [2]. Late diagnosis and lack of effective treatments have contributed to high GC incidence, high mortality and poor prognosis [3]. The GC incidence is 5–tenfold higher in high-risk compared with low-risk countries [4]. While smoking, dietary factors, and genetic susceptibility can contribute to GC risk, most cases (90%) are due to H. pylori infection [5]. In addition, the contribution of behavioral factors to the development of GC has been established [6]. At the same time, a high salt diet, frequent consumption of moldy substances, genetic factors, and older age are also associated with the emergency of gastric cancer [6]. With advancements in technology and endoscopic techniques, endoscopy has become the core in diagnosis and management of GC [7]. Surgical intervention is primarily used for early GC, whereas chemotherapy is recommended for patients who cannot be resected or with advanced metastasis but the prognosis is always unsatisfactory as GC is highly heterogeneous in gene and biology [8].
Different regions of the world have specific situations when it comes to gastric cancer. The area with the highest age-standardized rate (ASR) of incidence is Eastern Asia, with 22.4 cases per 100,000 inhabitants and Eastern Asia also experiences the greatest mortality from gastric cancer, with an ASR of 14.6 deaths per 100,000 [9]. Meanwhile, GC is one of the most common causes of tumor-related deaths and disability-adjusted life-years (DALYs) in males (12.2 million DALYs and 542,000 deaths) [10]. GC mortality rates differ by region depending on human development index (HDI) and incidence rates [2]. In addition, the temporal trends and incidence of GC vary by gender and age [11]. Studies have reported a declining trend in GC burden in the elderly population (> 50 years old), but not in the younger population [12]. Based on the analysis of mortality-to-incidence ratios (MIRs) data for 57 countries from the GLOBOCAN 2012 database, Tsai et al. [13] found that the more developed regions had high GC mortality and crude incidence rates, but lower MIR values than the less developed regions. Nevertheless, other factors, such as tumor stage and treatment strategy can also have a significant effect on patients’ prognosis. About two thirds of GC patients who undergo surgical resection with curative intent can benefit from adjuvant chemoradiation therapy [14]. Although overall survival (OS) for GC patients correlates well with stage, only 61–65% of patients with local–regional disease undergoes surgery [15]. Nowadays, the Surveillance, Epidemiology, and End Results (SEER) cancer registries record the incidence, incidence-based mortality (IBM), stage and treatment data of GC. However, this database is mainly focused on the US population. Nevertheless, the data can be used to develop targeted strategies for other populations. From 1975 to 2014, the incidence rate of GC in the US decreased at a steady rate of − 1.5% per year and the overall annual US death rate per 100,000 per year decreased from 5.1 to 3.1 based on the SEER database [16]. Based on the analysis of the SEER data, Pourmousavi et al. [17] found that GC patients who experienced endoscopic therapy vs. surgery had a comparable long-term cancer-specific mortality.
A Global Burden of Disease (GBD) study evaluated the burden of GC in 204 countries and regions worldwide, revealing the current situation of GC [10]. In the present study, we used GC data from the GBD study 2019 to analyze the incidence and mortality cases of GC from 1990 to 2019, as well as estimate age-standardized morbidity, mortality and DALY rate. Moreover, we estimated DALYs and mortality rates attributable to several major GC risk factors, including smoking, dietary risk, and behavioral risk. In addition, we evaluated the incidence rate and trends of IBM due to GC in the US during 1992–2018.
Materials and methods
GBD source
Age-standardized and annual incidence of gastric cancer from 1990 to 2019 by region, sex, country, and risks were downloaded from the Global Health Data Exchange query tool [18]. The Socio-Demographic Index (SDI) is a composite measure of economic, social, and demographic factors that can be used to describe the characteristics of a population and its distribution across a country or region. As a good composite measure of social development, including education, income, and fertility, SDI is closely correlated with health outcomes [10]. Based on the SDI, 204 countries and territories were categorized into five regions: high, high-middle, middle, low-middle, and low. In addition, the world was geographically divided into 21 regions. The HDI is a composite measure of human development across countries, created by the United Nations Development Program (UNDP) to provide a single measure of a country's progress and the standard of living of its citizens and the HDI is calculated using three main components: health, education, and income [2]. DALYs were calculated by summing years lived with disability and years of life lost. Rates were standardized to the GBD world population and reported as age-standardized DALY rates, age-standardized incidence rates, and age-standardized death rates per 100,000 people. Age-standardized rate (ASR) and estimated annual percentage change (EAPC) were used to quantify the trends of gastric cancer incidence, deaths, and DALYs rate [19]. ASR trend was used to better reflect the change in disease patterns in the population and establish targeted preventive strategies for gastric cancer [20]. EAPC summary was used to quantify the trends of ASR among different populations in a period [21]. The Global Burden of Disease study typically uses the World Health Organization's World Standard Population (WHO 2000–2025) for standardizing rates across different populations.
SEER source
The SEER Program gets data on all deceases happening in the US based on the National Center for Health Statistics (NCHS) on an annual basis and denominator data for both incidence and death rates were got from the Bureau of the Census [22]. We also collected GC patients from the SEER-13 registry database (1992–2018) using National Cancer Institute (NCI)’s SEER*Stat software (version 8.4.0). Histologic codes from the International Classification of Diseases for Oncology, Third Edition (ICD-O-3), and site codes to determine GC patients. GC were diagnosed as the merely primary malignancy based on histology and diagnostic information can only be obtained from patients with autopsy reports or death certificates. Cases were removed for unknown detailed data. Variables used in both GBD study and SEER data involved calendar year, sex, and age groups. SEER historic stage A (1973–2015) used for GC staging: localized, regional, unstaged, and distant. For treatment data, SEER offers therapy classification such as chemotherapy, radiotherapy, and surgery based on SEER-specific documents. We choose surgery applying the SEER code “Reason no cancer-direct surgery”, while radiotherapy and chemotherapy were determined applying items “radiation recode” and “chemotherapy recode”. The IBM reveals the population-level mortality caused by certain tumor sets. This method can classify the mortality of the general population based on the characteristics related to cancer diagnosis and recorded in the SEER register [23].
Joinpoint regression analysis
The determination of changes in recent disease trends is useful in the analysis of cancer mortality and incidence data. To describe such continuous changes, Joinpoint regression analysis was performed on the age-adjusted rates to estimate piecewise log-linear time calendar trends by country using NCI Joinpoint Regression software (version 4.9.0.0). Using Joinpoint regression model analysis, a long-term trend line was cut into significant trend sections characterized by continuous linearity through the model fitting [24]. The temporal trends were fitted with up to five joinpoints for gastric cancer incidence and death rates during 1990–2019 in the GBD study. To characterize the trend of the incidence rate of cancer over time, the best fitting logarithmic linear regression model was used to estimate the annual percentage change (APC), average APC (AAPC), and the corresponding 95% confidence interval (CI) for each trend and to determine the significant connection point.
Age-period-cohort analyses
Age period cohort analysis is used to analyze disease trends by age, population-level demographic changes (period), and initial life or generational exposures (cohort) effects [25]. Investigating age, period, and cohort effects at the same time is significant as characteristics of patients change with age. In the present study, we used the NCI’s age period cohort analysis online tool (http://analysistools.nci.nih.gov/apc/) to explore the relationship of the observed incidence rates with age, period, and cohort effects. Briefly, the number of incidents or deaths by age set was entered in a calendar phase as the number and the relevant person-year at-risk cases as the population. Mortality was assessed based on the age groups and corresponding calendar periods. The mortality of GBD data was estimated using 6 corresponding calendar periods and 13 five-year age groups. The rate ratio (RR) of mortality rates in each calendar period and a reference period was also calculated, adjusting for age and nonlinear cohort effects.
Statistical analysis
ASR and EAPC were calculated according to the procedure by Liu et al. [21]. Both EAPC value and the upper 95% CI boundary were < 0, suggesting a downward trend in ASR. In contrast, the EAPC value and the lower boundary of the 95% CI were > 0, suggesting a rising trend of ASR. A 95% CI of 0 indicates that ASR has a constant trend. Incidence rates were calculated per 100,000 person-years, and age‐adjusted to the 2000 US standard population. Moreover, to determine the affect factors for EAPC, Pearson correlation analysis was used to explore the relationship among EAPC and ASR (1990), and HDI (2019) at the national level was evaluated respectively. Hierarchical cluster analysis was performed using the “factoextra” R package combining EAPC data on morbidity and mortality to group the countries and territories into 4 categories (significant increase, significant decrease, minor decrease and minor increase). All statistical analyses were conducted using R software (R 4.1.2 software). Values with p < 0.05 were considered statistically significant.
Results
Global gastric cancer burden
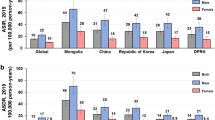
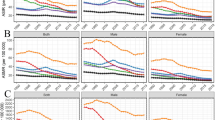
Globally, GC incidences increased from 883,395 in 1990 to 1,269,805 in 2019 while GC-associated mortality increased from 788,316 in 1990 to 957,185 in 2019. In 2019, the ASR of GC exhibited variations around the world, with Mongolia having the highest observed ASR (43.7 per 100,000), followed by Bolivia (34 per 100,000) and China (30.6 per 100,000) (Fig. 1A). The ASR decreased by an average of − 1.22% (95% CI − 1.35% to − 1.09%) per year in the same period (from 22.4 per 100,000 in 1990 to 15.6 per 100,000 in 2019) (Table 1). The most pronounced increase was in the United Arab Emirates, where it increased by 475.8% (95% CI 48.2% to 277.5%) (Fig. 1B). The largest increase in ASR was in the Dominican Republic (EAPC = 1.07; 95% CI 0.91 to 1.23) while the largest decrease in ASR was in the Maldives (EAPC = − 3.72; 95% CI − 4.02 to − 3.41) (Fig. 1C). Hierarchical cluster analysis found that four countries (or territories such as Lesotho, Dominican Republic, Zimbabwe, and Honduras) were included in the “significant increase” group. Forty-nine countries (or territories such as Egypt, Irag and Yemen) were included in the “significant decrease” group. One hundred and eleven countries (or territories such as the Australia, Brazil, USA, and China) were included in the “minor decrease” group. Forty countries (or territories such as the UK, Switzerland, and Japan) were included in the “minor increase” group (Additional file 1: Fig. S1). The observed regional in connection to SDI, versus the expected level for individual location on the basis of SDI was demonstrated in Additional file 2: Fig. S2. These results indicate that central and Eastern Europe as well as southern Latin America exhibited the expected trends over the study period, while in the Asian regions, there were wide variations in observed patterns. Comparable trends were also observed at the national level. Then, we assessed the relationship between EAPC and ASR (in 1990) and HDI (in 2019), respectively. A negative association was found among EAPCs and ASR (ASIR: r = − 0.28, p < 0.001; ASDR: r = − 0.19, p = 0.005). In addition, a significant negative association was determined among EAPCs and HDI (ASIR: r = − 0.50, p < 0.001; ASDR: r = − 0.66, p < 0.001), implying that countries with higher HDI exhibited a rapid decrease in ASR of GC from 1990 to 2019 (Fig. 2).
The global disease burden of gastric cancer (GC) in countries and territories in 2019. A The age-standardized rate (ASR) of gastric cancer, B the relative change in incident cases of gastric cancer among 1990 to 2019; C the estimated annual percentage change (EAPC) of gastric cancer ASR from 1990 to 2019
The relationship between estimated annual percentage change (EAPC) and age-standardized rate (ASR) in 1990, and human development index (HDI) in 2019 of gastric cancer, respectively. A The relationship between EAPC and ASR; B the relationship between EAPC and HCI. ASIR: age-standardized incident rate; ASDR: age-standardized death rate
Global gastric cancer burden by subgroup
Incidences of GC and associated mortalities among different age groups at the global level in 1990 and 2019 are shown in Fig. 3. In 1990, the incidences and mortalities were highest among males and females aged 60 to 69 years, and there were more new cases among males aged 35 to 84 years and in females aged 85 years and older. In contrast, in 2019, the incidences and mortalities were highest in both males and females aged 65 to 74 years, and there were more new cases in males aged 30 to 89 years as well as in females aged 90 years and older in 2019, which means that the incidences and mortalities of GC are gradually younger. At the regional level, incidences of GC were higher in high or high-middle SDI, relative to low or low-middle SDI, while, the mortality rate was comparable. Meanwhile, in all region groups, the incidence, prevalence and death cases were higher in males than in females, especially in high-income Asia Pacific, East Asia, and Middle SDI (Additional file 3: Fig. S3). Globally, in 2019, a considerable percentage of DALYs were attributable to the three risk factors for which GBD estimates were accessible; 17.2% (95% UI 13.8 to 20.4) attributable to smoking, 7.8% (0.2 to 30.9) to dietary risks, and 23.6% (14.9 to 42.7) to behavioral risks. Moreover, in 2019, the deaths attributable to these three risk factors were; 18.0% (95% UI 14.7 to 21.1) attributable to smoking, 7.7% (0.2 to 30.9) to dietary risks, and 24.2% (15.7 to 43.1) to behavioral risks. Some region exhibited high percentage of smoking, such as Central Europe, East Asia, and Western Europe; Southeast Asia and East Asia exhibited high percentage of dietary risks, while most of region revealed high percentage of behavioral risks, such as High-middle SDI, Middle SDI, and East Asia (Additional file 4: Fig. S4).
Joinpoint regression analysis
Globally, in 1993–1998, GC incidences significantly decreased APC at − 1.93% per year (/y) (95% CI − 2.4% to − 1.5%/y); from 1998 to 2004, they significantly increased at a rate of 0.58%/y (95% CI 0.23% to 0.93%/y), while from 2004 to 2017, they significantly decreased at a rate of − 2.05%/y (95% CI − 2.17% to − 1.93%/y) (Fig. 4). From 1990 to 2019, the high-income Asia Pacific had the most significant decrease in AAPC at a rate of − 2.71%/y (95% CI − 3.12% to − 2.31%/y), with Singapore showing the most significant decrease at − 3.23%/y (95% CI − 3.65% to − 2.80%/y) (Additional file 12: Table S1–4). Meanwhile, the global had a decrease in AAPC at a rate of − 1.24%/y (95% CI − 1.48% to − 0.99%/y), China shown a decrease in AAPC at a rate of − 0.70%/y (95% CI − 0.88% to − 0.51%/y).
Age-period-cohort analyses
At the global level, DALYs were attributable to the smoking, dietary risks, and behavioral risks. We next performed age-period-cohort analyses to explore the mortality attributed to these three risk factors. Net Drift represents the overall temporal trend in mortality/morbidity, but also takes into account trends attributable to period and cohort factors. For smoking, the overall Net Drift was − 2.51%/y (95% CI − 2.60% to − 2.41%/y) and the mortality rate under the age of 87.5 is decreasing per year based on the local drift values. The age effect analyses of mortality shown that in the same birth cohort, mortality rate increased gradually until age 72.5 at 20.97%/y (95% CI 20.58% to 21.36%/y) and then began to decline based on the longitudinal age curves values. For period effect based on the period RR values, the RR revealed that the effect in decreasing the death of GC occurred and the relative risk of mortality/morbidity was higher before 2002 than in the reference period. The cohort effect analyses based on the cohort RR values indicating that the mortality risk of GC decreasing among all birth cohorts and the relative risk of mortality/morbidity was higher before 1945 than in the reference birth cohorts Additional file 5: Fig. S5. Similar trends were also observed for dietary risks Additional file 6: Fig. S6 and behavioral risks Additional file 7: Fig. S7 as well.
SEER data analysis
In this study, a decrease in ASR was found in the US (AAPC = − 1.26; 95% CI − 1.44 to − 1.07), based on GBD study, therefore, we assessed the incidence, IBM, stage and treatment data for GC using the SEER database as a likely validation set. There were 74,966 incidences of GC and 69,374 GC-related deaths recorded between 1992 and 2018 (Tables 2, 3). The overall incidence decreased (AAPC = − 1.4; 95% CI − 1.5 to − 1.2) between 1992 and 2018. The significant decrease in GC incidences as well as decreasing trends in IBM of GC were first detected in 1994. The GC IBM significantly increased at a rate of 35%/y from 1992 to 1994 (95% CI 21.2% to 50.4%/y), and then begun to decrease at a rate of − 1.4%/y from 1994 to 2018 (95% CI − 1.6% to − 1.2%/y). Comparable trends in IBM were also found among males, relative to females (Additional file 8: Figure S8, Additional file 9: Figure S9). Meanwhile, there were variations in GC incidences and mortality patterns among the age subgroups. Across the study periods, incidences of GC increased until patients aged 45–49 (AAPC = 0.5; 95% CI 0.1 to 0.9) then declined (patients aged 50–54). Moreover, there were variations in IBM rates of GC among the age subgroups. The IBM rates decreased among individuals aged 45–59 (AAPC = − 0.5; 95% CI − 1.2 to 0.2) and 50–54 (AAPC = − 1.1; 95% CI − 1.9 to − 0.4). Among individuals aged 60–64, IBM rates of GC were increased (1992–1994: APC = 43.4; 95% CI 14.5 to 79.8), then declined (1992–2015: APC = − 2.5; 95% CI − 2.9 to − 2.0), and finally increased (2015–2018: APC = 5.9; 95% CI − 2.3 to 14.9). Mortality rates for older patients aged > 75 years showed increasing trends. In contrast, incidences and mortality rates for younger GC people were more inclined to enter the plateau period. Finally, we assessed the trends in tumor stages and therapeutic options for GC in the US from 1992 to 2015. There was an increasing trend in the use of chemotherapy in overall disease stage (from 9.5% to 22.2%, p < 0.001) and metastatic disease (from 20.0% to 38.8%, p < 0.001). However, a decreasing trend in the choice of surgery was observed for regional disease (from 39.4% to 8.3%, p < 0.001) and localized disease (from 51.8% to 11.3%, p < 0.001) (Additional file 10: Fig. S10). Chemotherapy + radiotherapy was the most frequently used option for distant stage GC patients. Surprisingly, over the past three decades, the overall survival outcomes for GC patients have been at a plateau, with no significant improvements [26]. The flow chart of the study can find in Additional file 11: Fig. S11.
Discussion
In this study, we investigated the temporal trends in GC incidences and specific mortality at global, regional, and national levels based on the GBD study and the SEER database. In general, there was a steady global decrease in GC incidences and mortality from 1990 to 2019, and from 1992–2018 in the US. Changes in population growth and age structure imply that GC incidences and associated deaths will continue to increase [9]. Our research helps to understand the epidemiological characteristics of gastric cancer and its impact on global health. Revealing the main risk factors leading to gastric cancer, such as smoking and dietary habits, can help develop prevention strategies for gastric cancer and understand the differences between different regions to optimize patient management and treatment.
Consistent with previous studies, we found that the prevalence and death cases were higher among males than in females in all region groups. In 2019, the incidence and mortality rate of GC in both males and females peaked at age 65 to 74 years, and there were more new cases in males aged 30 to 89 years, and in females aged between 90 years and older in 2019. Most of the GC patients outside the US were younger (< 60 years old) and had the poorly differentiated (diffuse) subtype, presented high intratumor heterogeneity and poor cellular differentiation, while within US, GC was highly prevalent among older patients, which was commonly well differentiated (intestinal) [27]. In a previous meta-analysis, longer exposure to estrogen from either ovarian or exogenous origin was shown to reduce risk of GC among females [28]. In females, a lack of lactation history, nulliparity, old age at first delivery (> 35 years), and poor nutritional status throughout pregnancy were associated with increased risk of GC while family history was more closely correlated with GC among males [29]. Although early estrogen exposure may have some protective effects, female reproduction may not have a significance influence on GC development. Age distribution for female patients is not closely correlated with estrogen levels, thus, the protective effects of estrogen should be evaluated further [30]. Epstein-Barr virus (EBV) has been causally associated with GC. Prevalence estimates of EBV positivity with a twofold difference by sex were found to be 11.1% in males vs 5.2% in females [31]. Atrophy and intestinal metaplasia scores in patients with H. pylori infections have been shown to be severe in males than in females, particularly in elderly patients [32]. This difference in risk factors between males and females may contribute to differences in incidences and death.
The incidence rate and mortality of gastric cancer in different countries and regions are also different. Eastern Asia, the Pacific region of South America, and Central/Eastern Europe exhibit a higher GC incidence of ASR, while North America and Africa have the lowest rates. Before 1940, GC was the leading cause of cancer death in American males and the third cause in American females [33]. Moreover, between 1957 and 1981, 31,716 cases of gastric cancer were registered in the West Midlands, UK and the age-standardized incidence has shown a decrease from 17.42 per 100,000 population during the first quinquennium to 15.30 per 100,000 in the last [34]. Nowadays, the incidence rate of gastric cancer in the US and UK is at a lower level compared with other countries. The variability of GC incidence is associated with the geographical distribution of risk factors [35]. Developing countries exposures more increased GC risk include tobacco use and industrial and chemical pollutants [36]. Different ethnic groups have a widely varying prevalence of the GC anatomic subsite. The cardias is more commonly affected in Afro-Americans, Hispanics, and Amerindians, while Caucasians primarily experience the non-cardia type of GC [37]. The extent of the decrease differs in various countries, we observed some countries are actually facing an increase in their burden, such as Dominican Republic, El Salvador and Honduras. Consequently, it is essential to enhance measures aimed at reducing the disease burden in countries like China and Egypt, which currently bear a larger burden and have experienced a lower decline. In 2020, gastric cancer resulted in over 1 million new cases and approximately 770,000 deaths. China accounted for about half of the global new cases, which is roughly 478,000 [38]. By enhancing public awareness and education regarding health and fostering the adoption of disease prevention measures, it is possible to decrease disease occurrence and transmission, ultimately relieving the burden caused by diseases. The incidence rate of gastric cancer in the United States is at a lower level compared with other countries, which is more valuable for research. In fact, for regions with low incidence rate, research can help reveal the specific pathogenic factors and environmental factors in the region, so as to provide more reference information for the prevention and treatment of gastric cancer worldwide.
H. pylori infection is among the most significant risk factors for GC development, thus, various prevention strategies against GC focus on H. pylori infection [39]. Virulence factors of H. pylori, such as CagA or VacA, have been determined to increase GC risk [40]. Treatment of H. pylori reduces the risk of GC development; however, the extent of risk reduction relies on the extent of pre-existing injury at the time of eradication. In addition, salty food intake increases the risk of H. pylori infection, and may synergistically contribute to GC development [1]. In this study, 7.7% deaths were attributable to dietary risks, therefore, dietary adjustment to reduce salt and salt intake is a possible strategy for preventing GC. Importantly, H. pylori infection was strong related to dietary risks. In the United States, the decline was most reflected in the non-Hispanic White population, but prevalence is still high (30–40%) among Hispanic and African American populations and significantly increased rates (approximately 75%) are seen in the Alaskan Native populations [41]. A low and stable prevalence of H. pylori infection has been reported in the USA. Currently, the high GC-associated mortality rate in Japan has also been correlated with increased rates of smoking, as the prevalence of smoking has been high among males, especially among those born before the late 1950s in Japan [42]. In a study involving 371,813 veterans with H. pylori infection, it was established that there was a significantly high risk of GC among smokers [37]. In this study, globally, 17.2% DALYs and 18.0% deaths were attributable smoking. Thus, to reduce GC incidences, there is a need for lifestyle interventions involving smoking and diet, as well as screening and treatment of H. pylori, especially in high GC mortality countries.
For GC without distant metastasis, the main treatment option is surgical resection with sufficient lymphadenectomy and chemotherapy before and after. In a previous study, the 15-year GC survival rate was 21% for the standardized limited (D1) lymphadenectomy group and 29% for the standardized extended (D2) lymphadenectomy group [43]. With regards to adjuvant therapy after curative-intent surgery, only 25% of qualified patients accepted adjuvant chemoradiation while only 3% accepted perioperative chemotherapy from 2002 to 2009 [44]. A randomized phase III trial (INT-0116) revealed powerful persistent advantages of adjuvant radiochemotherapy in GC cases at moderate risk of locoregional failure following surgery [45]. Importantly, preoperative chemoradiotherapy enhanced survival outcomes for patients with potentially curable esophageal or esophagogastric-junction cancer [46]. However, compared to postoperative chemotherapy, postoperative chemoradiotherapy did not improve the OS of patients with resectable GC who received adequate preoperative chemotherapy and surgical treatment [47]. For locally advanced GC, perioperative chemotherapy is the first choice in Europe while in the USA, adjuvant chemoradiotherapy is standard, and in Japan, adjuvant chemotherapy is recommended [48]. Thus, selection of GC patients that are likely to benefit from adjuvant therapy may help optimize the benefit for those at a high risk of mortality. The SEER database contains detailed treatment data for GC in the US; our study found that from 1992 to 2015, there was an increasing trend in the use of chemotherapy (from 9.5% to 22.2%) and a decreasing trend in the choice of surgery (from 28.5% to 5.4%). This reflects the continuous exploration of new therapeutic strategies in GC. In recent years, there has been a growing utilization of clinical prediction models in clinical practice. One such model that has gained popularity is the nomogram, which presents data in a visually comprehensive graphical format derived from multiple regression analysis results. This study has several limitations. First, we did not estimate the burden of H. pylori infection as well as cardia and non-cardia forms of GC as the data was absent, thus, we ignored the different epidemiological risk factors and clinicopathological characteristics between the two topographic categories. Second, specific factors influencing the GC burden in different regions were difficult to study. Finally, GBD data were produced by a combination of estimation corrections made by various models, therefore, they should fully account for the offset caused by the source of the original data.
Conclusion
In summary, even though we found a decrease in overall GC incidences and mortality rates, GC remains a major public health concern. Advances in screening, diagnosis (especially in endoscopy) as well as improvements in socio-economic status and targeted treatment strategies accounted for the decreased burden of GC. Prevention of GC due to smoking and dietary behavioral risks through government policy interventions should be highlighted and these factors should be adjusted to individual country's risk factor profile. These findings mirror the global disease burden of GC and are important for development of targeted prevention strategies.
Availability of data and materials
The datasets generated for this study are available on https://vizhub.healthdata.org/gbd-results/.
References
Smyth EC, Nilsson M, Grabsch HI, van Grieken NC, Lordick F. Gastric cancer. Lancet. 2020;396(10251):635–48.
Arnold M, Abnet CC, Neale RE, et al. Global burden of 5 major types of gastrointestinal cancer. Gastroenterology. 2020;159(1):335-349.e15.
Padmanabhan N, Ushijima T, Tan P. How to stomach an epigenetic insult: the gastric cancer epigenome. Nat Rev Gastroenterol Hepatol. 2017;14(8):467–78.
Bray F, Ferlay J, Laversanne M. Cancer incidence in five continents: inclusion criteria, highlights from Volume X and the global status of cancer registration. Int J Cancer. 2015;137:2060–71.
Thrift AP, Wenker TN, El-Serag HB. Global burden of gastric cancer: epidemiological trends, risk factors, screening and prevention. Nat Rev Clin Oncol. 2023;20(5):338–49.
Poorolajal J, Moradi L, Mohammadi Y, Cheraghi Z, Gohari-Ensaf F. Risk factors for stomach cancer: a systematic review and meta-analysis. Epidemiol Health. 2020;42: e2020004.
Wadhwa V, Patel N, Grover D, Ali FS, Thosani N. Interventional gastroenterology in oncology. CA Cancer J Clin. 2023;73(3):286–319.
Ishigami S, Natsugoe S, Hokita S, Che X, Tokuda K, Nakajo A, et al. Clinical importance of preoperative carcinoembryonic antigen and carbohydrate antigen 19–9 levels in gastric cancer. J Clin Gastroenterol. 2001;32(1):41–4.
López MJ, Carbajal J, Alfaro AL, Saravia LG, Zanabria D, Araujo JM, Quispe L, Zevallos A, Buleje JL, Cho CE, Sarmiento M, Pinto JA, Fajardo W. Characteristics of gastric cancer around the world. Crit Rev Oncol Hematol. 2023;181: 103841.
Global Burden of Disease Cancer Collaboration. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the global burden of disease study. JAMA Oncol. 2019;5(12):1749–68.
Luo G, Zhang Y, Guo P, Wang L, Huang Y, Li K. Global patterns and trends in stomach cancer incidence: age, period and birth cohort analysis. Int J Cancer. 2017;141:1333–44.
Anderson WF, Camargo MC, Fraumeni JF Jr, Correa P, Rosenberg PS, Rabkin CS. Age-specific trends in incidence of noncardia gastric cancer in US adults. JAMA. 2010;303:1723–8.
Tsai MC, Wang CC, Lee HL, Peng CM, Yang TW, Chen HY, et al. Health disparities are associated with gastric cancer mortality-to-incidence ratios in 57 countries. World J Gastroenterol. 2017;23(44):7881–7.
Xiong HQ, Gunderson LL, Yao J, Ajani JA. Chemoradiation for resectable gastric cancer. Lancet Oncol. 2003;4(8):498–505. https://doi.org/10.1016/s1470-2045(03)01170-7.
Lawrence W Jr, Menck HR, Steele GD Jr, Winchester DP. The National Cancer Data Base report on gastric cancer. Cancer. 1995;75(7):1734–44.
Milano AF. 20-Year comparative survival and mortality of cancer of the stomach by age, sex, race, stage, grade, cohort entry time-period, disease duration & selected ICD-O-3 oncologic phenotypes: a systematic review of 157,258 cases for diagnosis years 1973-2014: (SEER*Stat 8.3.4). J Insur Med. 2019;48(1):5–23.
Pourmousavi MK, Wang R, Kerdsirichairat T, Kamal A, Akshintala VS, Hajiyeva G, et al. Comparable cancer-specific mortality of patients with early gastric cancer treated with endoscopic therapy vs surgical resection. Clin Gastroenterol Hepatol. 2020;18(12):2824-2832.e1.
Global Burden of Disease Collaborative Network Global Burden of Disease Study 2019 (GBD 2019) Results Institute for Health Metrics and Evaluation (IHME), Seattle, United States (2019). http://ghdx.healthdata.org/gbd-results-tool
Ding Q, Liu S, Yao Y, Liu H, Cai T, Han L. Global, regional, and national burden of ischemic stroke, 1990–2019. Neurology. 2022;98(3):e279–90.
Liu Q, He H, Yang J, Feng X, Zhao F, Lyu J. Changes in the global burden of depression from 1990 to 2017: findings from the Global Burden of Disease study. J Psychiatr Res. 2020;126:134–40.
Liu Z, Jiang Y, Yuan H, Fang Q, Cai N, Suo C, et al. The trends in incidence of primary liver cancer caused by specific etiologies: results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J Hepatol. 2019;70(4):674–83.
Gloeckler Ries LA, Reichman ME, Lewis DR, Hankey BF, Edwards BK. Cancer survival and incidence from the Surveillance, Epidemiology, and End Results (SEER) program. Oncologist. 2003;8(6):541–52.
Yan KL, Li S, Tseng CH, Kim J, Nguyen DT, Dawood NB, et al. Rising incidence and incidence-based mortality of thyroid cancer in California, 2000–2017. J Clin Endocrinol Metab. 2020;105(6): dgaa121.
Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–51.
Okui T. An age-period-cohort analysis for prevalence of common psychiatric disorders in Japan, 1999–2017. Soc Psychiatry Psychiatr Epidemiol. 2021;56(4):639–48.
Yang X, Zhang T, Zhang H, Sang S, Chen H, Zuo X. Temporal trend of gastric cancer burden along with its risk factors in China from 1990 to 2019, and projections until 2030: comparison with Japan, South Korea, and Mongolia. Biomark Res. 2021;9(1):84.
Cisło M, Filip AA, Arnold Offerhaus GJ, Ciseł B, Rawicz-Pruszyński K, Skierucha M, et al. Distinct molecular subtypes of gastric cancer: from Laurén to molecular pathology. Oncotarget. 2018;9(27):19427–42.
Camargo MC, Goto Y, Zabaleta J, Morgan DR, Correa P, Rabkin CS. Sex hormones, hormonal interventions, and gastric cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2012;21(1):20–38.
Persson C, Inoue M, Sasazuki S, Kurahashi N, Iwasaki M, Ye W, et al. Female reproductive factors and the risk of gastric cancer in a large-scale population-based cohort study in Japan (JPHC study). Eur J Cancer Prev. 2008;17(4):345–53.
Chung HW, Noh SH, Lim JB. Analysis of demographic characteristics in 3242 young age gastric cancer patients in Korea. World J Gastroenterol. 2010;16(2):256–63.
Murphy G, Pfeiffer R, Camargo MC, Rabkin CS. Meta-analysis shows that prevalence of Epstein-Barr virus-positive gastric cancer differs based on sex and anatomic location. Gastroenterology. 2009;137(3):824–33.
Kato S, Matsukura N, Togashi A, Masuda G, Matsuda N, Yamada N, et al. Sex differences in mucosal response to Helicobacter pylori infection in the stomach and variations in interleukin-8, COX-2 and trefoil factor family 1 gene expression. Aliment Pharmacol Ther. 2004;20(Suppl 1):17–24.
Howson CP, Hiyama T, Wynder EL. The decline in gastric cancer: epidemiology of an unplanned triumph. Epidemiol Rev. 1986;8:1–27.
Allum WH, Powell DJ, McConkey CC, Fielding JW. Gastric cancer: a 25-year review. Br J Surg. 1989;76(6):535–40.
Bouras E, Tsilidis KK, Triggi M, Siargkas A, Chourdakis M, Haidich AB. Diet and risk of gastric cancer: an umbrella review. Nutrients. 2022;14(9):1764.
Santibañez M, Alguacil J, de la Hera MG, Navarrete-Muñoz EM, Llorca J, Aragonés N, Kauppinen T, Vioque J. Occupational exposures and risk of stomach cancer by histological type. Occup Environ Med. 2012;69:268–75.
Kumar S, Metz DC, Ellenberg S, Kaplan DE, Goldberg DS. Risk factors and incidence of gastric cancer after detection of Helicobacter pylori infection: a large cohort study. Gastroenterology. 2020;158(3):527-536.e7.
Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Machlowska J, Baj J, Sitarz M, Maciejewski R, Sitarz R. Gastric cancer: epidemiology, risk factors, classification, genomic characteristics and treatment strategies. Int J Mol Sci. 2020;21(11):4012.
Chang WL, Yeh YC, Sheu BS. The impacts of H. pylori virulence factors on the development of gastroduodenal diseases. J Biomed Sci. 2018;25:1–9.
Shakir SM, Shakir FA, Couturier MR. Updates to the diagnosis and clinical management of Helicobacter pylori infections. Clin Chem. 2023;69(8):869–80.
Funatogawa I, Funatogawa T, Yano E. Trends in smoking and lung cancer mortality in Japan, by birth cohort, 1949–2010. Bull World Health Organ. 2013;91(5):332–40.
Songun I, Putter H, Kranenbarg EM, Sasako M, van de Velde CJ. Surgical treatment of gastric cancer: 15-year follow-up results of the randomised nationwide Dutch D1D2 trial. Lancet Oncol. 2010;11(5):439–49.
Snyder RA, Penson DF, Ni S, Koyama T, Merchant NB. Trends in the use of evidence-based therapy for resectable gastric cancer. J Surg Oncol. 2014;110:285–90.
Smalley SR, Benedetti JK, Haller DG, Hundahl SA, Estes NC, Ajani JA, et al. Updated analysis of SWOG-directed intergroup study 0116: a phase III trial of adjuvant radiochemotherapy versus observation after curative gastric cancer resection. J Clin Oncol. 2012;30(19):2327–33.
van Hagen P, Hulshof MC, van Lanschot JJ, Steyerberg EW, van Berge Henegouwen MI, Wijnhoven BP, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012;366(22):2074–84.
Cats A, Jansen EPM, van Grieken NCT, Sikorska K, Lind P, Nordsmark M, et al. Chemotherapy versus chemoradiotherapy after surgery and preoperative chemotherapy for resectable gastric cancer (CRITICS): an international, open-label, randomised phase 3 trial. Lancet Oncol. 2018;19(5):616–28.
Ott K, Lordick F, Blank S, Büchler M. Gastric cancer: surgery in 2011. Langenbecks Arch Surg. 2011;396(6):743–58.
Acknowledgements
Not applicable.
Funding
This study was supported by the National Key R&D Program of China (Grant Number 2023YFC2307000), National Natural Science Foundation of China [Grant Numbers 82170571 and 81974068], China Postdoctoral Science Foundation (Grant Number 2023M741283).
Author information
Authors and Affiliations
Contributions
W.Z.H. designed and analyzed the research study; Z.K. F.M.K and W.W.J. collected the data; WZH and LR wrote and revised the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study not need institutional review board or ethics committee approval as the data all download from public free database.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1
. Hierarchical cluster analysis was performed applying the “factoextra” R package combining estimated annual percentage change data on morbidity and mortality of gastric cancer to group the countries and territories into 4 categories.
Additional file 2: Figure S2
. The observed regional in connection to socio-demographic index (SDI), versus the expected level for individual location on the basis of SDI of gastric cancer. A. The territories; B. The countries.
Additional file 3: Figure S3
. The incident, prevalence and death cases were between males than in females in all region groups of gastric cancer.
Additional file 4: Figure S4
. The disability-adjusted life-years (DALYs) and death were attributable to the smoking, dietary risks, and behavioral risks of gastric cancer.
Additional file 5: Figure S5
. Age-period-cohort analyses to explore the mortality attributed to smoking risk factor in gastric cancer from 1990 to 2019.
Additional file 6: Figure S6
. Age-period-cohort analyses to explore the mortality attributed to dietary risk factor in gastric cancer from 1990 to 2019.
Additional file 7: Figure S7
. Age-period-cohort analyses to explore the mortality attributed to behavioral risk factor in gastric cancer from 1990 to 2019.
Additional file 8: Figure S8
. Joinpoint regression analysis of gastric cancer incidence in US during 1992–2018.
Additional file 9: Figure S9
. Joinpoint regression analysis of gastric cancer incidence-based mortality (IBM) in US during 1992–2018.
Additional file 10: Figure S10
. The trends in tumor stages and therapy options of gastric cancer in the US from 1992 to 2015. A. Distant; B. Localized; C. Regional; D. Unstaged; E. Overall; F. The overall survival of GC in different tumor stages.
Additional file 11: Figure S11
. The flow chart of the study.
Additional file 12: Table S1
. The incident cases, age-standardized incidence and temporal trends of gastric cancer in countries from 1990 to 2019. Table S2. Joinpoint regression analysis of gastric cancer incidence in countries from 1990 to 2019. Table S3. Joinpoint regression analysis of gastric cancer incidence of annual percentage change (APC) in territories from 1990 to 2019. Table S4. Joinpoint regression analysis of gastric cancer incidence of average annual percentage change (AAPC) in territories from 1990 to 2019.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, Z., Zhang, K., Wang, W. et al. The differences in gastric cancer epidemiological data between SEER and GBD: a joinpoint and age-period-cohort analysis. J Big Data 11, 51 (2024). https://doi.org/10.1186/s40537-024-00907-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40537-024-00907-8