Abstract
Tau is a predominantly neuronal, soluble and natively unfolded protein that can bind and stabilize microtubules in the central nervous system. Tau has been extensively studied over several decades, especially in the context of neurodegenerative diseases where it can aberrantly aggregate to form a spectrum of pathological inclusions. The presence of tau inclusions in the form of neurofibrillary tangles, neuropil threads and dystrophic neurites within senile plaques are essential and defining features of Alzheimer’s disease. The current dogma favors the notion that tau is predominantly an axonal protein, and that in Alzheimer’s disease there is a redistribution of tau towards the neuronal soma that is associated with the formation of pathological inclusions such as neurofibrillary tangles and neuropil threads. Using novel as well as previously established highly specific tau antibodies, we demonstrate that contrary to this overwhelmingly accepted fact, as asserted in numerous articles and reviews, in adult human brain, tau is more abundant in cortical gray matter that is enriched in neuronal soma and dendrites compared to white matter that is predominantly rich in neuronal axons. Additionally, in Alzheimer’s disease tau pathology is significantly more abundant in the brain cortical gray matter of affected brain regions compared to the adjacent white matter regions. These findings have important implications for the biological function of tau as well as the mechanisms involved in the progressive spread of tau associated with the insidious nature of Alzheimer’s disease.
Similar content being viewed by others
Introduction
Tau is a microtubule (MT) associated protein that is predominately expressed in neurons in the human central nervous system (CNS) [74]. The physiological functions of tau include promoting tubulin polymerization and MT stability, which are mediated through the MT binding repeat domain of tau and the upstream adjacent proline rich domains [12, 17, 40]. The expression of tau is developmentally regulated and in human adult brain tau presents as 6 isoforms through alternative splicing of exons 2, 3, and 10 which lead to tau proteins having 0, 1, or 2 N terminal inserts and 3 or 4 MT binding repeats (see Fig. 1) [21, 33]. Under non-pathological conditions, tau exists predominantly as a soluble and natively unfolded protein [6, 44] which lacks secondary structure and discontinuously associates and regulates MTs [45]. Under pathological conditions, including Alzheimer’s disease (AD), tau forms insoluble aggregates such as paired helical filaments and straight filaments which form the components of neurofibrillary tangles (NFT) [12, 20, 21, 32, 34, 41, 44, 47, 52, 56, 74, 80]. The pathological hallmarks of AD include amyloid β (Aβ) deposits known as senile plaques and pathological tau inclusions that present as NFT, neuropil threads, and dystrophic neurites within senile plaques [24, 28, 51].
Characterization of the specificity of the new tau antibodies 1B1 and 1H11. a Schematic of full-length human tau (2N4R) with the location of the antibody epitopes used in the study. Created with BioRender.com. b Amino acid sequence of human and mouse tau corresponding to residues 19 to 38 in human tau. Non-homologous amino acids between species are indicated in black lettering. Dashes indicate residues that are not present in mouse tau. c 10 µg of total brain lysate from tau KO, nTg, and PS19 mice were resolved by SDS-PAGE as indicated above each lane and used for immunoblotting as described in Materials and Methods. Blots were probed with antibodies 3026 (mouse and human tau), 1B1 (human tau), 1H11 (human tau), CP27 (human tau) and anti-GAPDH as a loading control. The mobility of protein markers with their molecular masses are indicated on the left side of each immunoblot. d IHC was performed as described in Materials and Methods. Brains of tau KO, nTg, and PS19 mice were stained with the total tau antibody Tau-5, and the two novel monoclonal total human tau antibodies, 1B1 and 1H11. Sections were counterstained with hematoxylin. Scale bar indicates 300 \(\mu \mathrm{m}\)
The presence and accumulation of insoluble tau aggregates is also found in other neurodegenerative diseases collectively termed tauopathies [12, 30, 53, 74]. The mechanism(s) through which tau aggregation is prompted and causes neurodegeneration in AD and other neurodegenerative diseases is still unknown, but a leading hypothesis is that tau pathology propagates through a prion-like mechanism and spreads transcellularly through connected brain regions [4, 30, 62].
The neuronal distribution of tau was initially described in rat and bovine brain and was found to be predominantly localized in axons [7]. The current dogma posits that under pathological conditions, where tau is aggregated and highly phosphorylated, it is aberrantly re-localized to the somatodendritic compartment of the neuron [2, 71, 74, 85]. While our understanding of tau pathology has been furthered by the availability of tau antibodies generated using synthetic peptides and AD brain lysate, a limitation of these antibodies is that many cross-react with other microtubule associated proteins (MAPs) due to the homology in the MT binding region [8, 57, 73]. Furthermore, binding of many tau antibodies depends on the phosphorylation state of the targeted epitopes and thus staining with these antibodies does not reveal the distribution of all tau species [2, 61, 64, 69]. In the current study, we generated and characterized two novel monoclonal tau antibodies raised against a phosphorylation independent epitope in the N terminal domain which do not cross react with other MAPs. Histologically and biochemically, it is demonstrated that in the brains of healthy adult controls, tau is more abundant in the cerebral cortical gray matter where neuronal soma and dendrites are located rather than the cerebral cortical white matter that is highly enriched in axons. A similar distribution was observed in the cortical subregions of AD brains where pathological tau aggregation also is predominantly observed in the gray matter compared to white matter. These findings have important implications for the normal biological function of tau in the adult human brain as well as the underlying mechanisms resulting in pathological tau aggregation including a critical reshaping of the prion-type spreading model.
Materials and methods
Mice
All animal experimental procedures were performed in accordance to University of Florida Institutional Animal Care and Use Committee regulatory policies following approval. BALB/c mice, tau knockout (KO) [22] and PS19 tau transgenic mice [84] were obtained from Jackson Laboratories (Bar Harbor, ME). For immunohistochemistry (IHC), mice were euthanized with CO2, perfused with a heparin/PBS solution, fixed in formalin and embedded in paraffin before staining.
Generation of new N-terminal Tau monoclonal antibodies
Monoclonal antibodies were generated as previously described [66]. In brief, a synthetic peptide (CGLGDRKDQGGYTMHQDQEGD) corresponding to amino acids 19–38 of human tau was synthesized and purified by GenScript USA, Inc. (Piscataway, NJ). This peptide contains an added cysteine residue at the amino-terminus that allows for conjugation to Imject maleimide-activated mariculture keyhole limpet hemocyanin (mcKLH; Termo Scientifc, Waltham, MA). The peptides conjugated to mcKLH were used to immunize female BALB/c mice (Jackson Laboratory, Bar Harbor, ME).
Hybridoma clones were screened by enzyme-linked immunosorbent assay (ELISA) with 96-well ELISA plates (Thermo Fisher Scientifc, Waltham, MA) coated with 1 µg/ml of peptide in PBS using the unconjugated peptide used from immunization. Wells were washed with PBS and blocked with PBS/5% fetal bovine serum (FBS). Media from hybridomas were added to plates and incubated at room temperature. Plates were washed with PBS and were then incubated with horseradish peroxidase-conjugated anti-mouse antibody (Jackson Immuno Research Labs, West Grove, PA) in 5% FBS/PBS for an hour. Following washes with PBS, 3,3′,5,5′-tetramethylbenzidine (TMB substrate, Thermo Fisher Scientifc, Waltham, MA) was added to each well until a color change was observed. The reactions were stopped by adding 0.5 M HCl and the optical density was measured at 450 nm with a plate reader. Positive clones were further tested by ELISA using recombinant tau protein as well as synthetic peptide (AGTYGLGDRKDQGG) corresponding to amino acid residues 15–28 in human tau. The isotypes of antibodies 1B1 and 1H11 were determined to be IgG1 using a mouse monoclonal isotyping kit (Millipore Sigma, Burlington, MA).
Preparation of total protein lysate from mouse brain tissue
Mice were euthanized with CO2 and the brains from PS19 tau transgenic mice, tau KO mice, and non-transgenic (nTg) mice were harvested. Mouse brain were disrupted by sonication in 2% SDS/50 mM Tris, pH 7.5 and the lysates were heated to 95 \(^\circ\)C for 10 min. Protein concentrations were determined using BCA assay using bovine serum albumin as the standard (Thermo Fisher Scientific, Waltham, MA). SDS sample buffer was added to the lysates and heated to 95 \(^\circ\)C for 10 min and stored at − 80 °C.
Immunohistochemistry
Tissue sections from paraffin-embedded blocks were rehydrated in xylene and a series of descending alcohols (100–70%) and washed in water. Heat-induced epitope retrieval (HIER) was performed in a steam bath for 60 min for human tissue or 30 min for mouse tissue in a citrate solution (Target Retrieval Solution Citrate pH 6; Agilent, Santa Clara, CA). Next, slides were washed in water and endogenous peroxidases were quenched by incubating sections in 1.5% hydrogen peroxide in PBS (Invitrogen, Waltham, MA). Sections were then rinsed in water and incubated in 0.1 M Tris and blocked in 2% FBS/0.1 M Tris. Primary antibodies were diluted in blocking solution or applied undiluted and were added onto tissue sections at 4 °C overnight. Slides were washed in 0.1 M Tris and incubated with biotinylated anti-mouse secondary antibody (1:3000) and immPRESS HRP horse anti-mouse polymer detection (1:5) (Vector Laboratories; Burlingame, CA) diluted in blocking solution for 1 h at room temperature. Slides were subsequently washed with 0.1 M Tris and incubated with an avidin–biotin complex (Vectastain ABC Elite kit; Vector Laboratories, Burlingame, CA) for 1 h at room temperature. Immunocomplexes were detected with the chromogen 3,3′-diaminobenzidine (DAB kit; KPL, Gaithersburg, MD). Sections were counterstained with Mayer’s hematoxylin (Sigma Aldrich, St. Louis, MO), washed in water, dehydrated in a series of ascending alcohols (70–100%) and xylenes, and coverslipped using Cytoseal (Thermo Scientific, Waltham, MA).
Sequential brain fractionation for isolation of soluble and insoluble Tau
Frozen human brain was obtained from the University of Florida Neuromedicine Human Brain and Tissue Bank (Table 1). Gray and white matter from the temporal and occipital brain cortices were carefully dissected, weighed and disrupted by sonication in 6 mL of high-salt (HS) buffer (50 mM Tris–HCl, pH 7.5, 0.75 M NaCl, 2 mM EDTA) containing a protease inhibitor cocktail (1 mM phenylmethylsulfonyl fluoride and 1 \(\upmu\)g/ml each of pepstatin, leupeptin, N-tosyl-l-phenylalanyl chloromethyl ketone, N-tosyl-lysine chloromethyl ketone, and soybean trypsin inhibitor) per gram of tissue. The lysate was centrifuged at 100,000 × g at 4 \(^\circ\)C for 30 min. The supernatants were kept as the HS soluble fractions and the pellets were homogenized in 4 mL of HS buffer with 1% Triton buffer per gram of tissue, and centrifuged at 100,000× g at 4 \(^\circ\)C for 30 min. These fractions were kept as the HS/1% Triton-soluble fractions and the pellet was homogenized in 6 mL HS buffer with 1% Triton and 1 M sucrose, and centrifuged at 100,000 × g at 4 \(^\circ\)C for 30 min to float the myelin. This fraction was discarded, and the pellet was homogenized in 2 mL of HS buffer with 1% Sarkosyl per gram of tissue, incubated at 37 \(^\circ\)C for 30 min and centrifuged at 100,000 × g at 4 \(^\circ\)C for 30 min. This fraction was kept as the HS/Sarkosyl soluble fractions and the pellets were sonicated in 1 mL SDS/urea (2% SDS, 4 M urea, 25 mM Tris–HCl pH 7.6) per gram of tissue, centrifuged at 100,000 × g at 25 \(^\circ\)C for 30 min. This fraction was collected as the SDS/urea soluble fraction. SDS was added to the HS, Triton/HS, and Sarkosyl/HS fractions, for a final concentration of 2% SDS. These were heated at 95 °C for 10 min and all fractions were kept frozen in -80 °C till further use. Protein concentrations were determined using bicinchoninic acid (BCA) assay using bovine serum albumin as the standard (ThermoFisher Scientific, Waltham, MA). SDS sample buffer was added to the HS soluble/2% SDS, Triton/HS/2% SDS, and Sarkosyl/HS/2%SDS fractions that were incubated for 10 min at 95 \(^\circ\)C. SDS sample buffer was added to the SDS/urea soluble samples that were incubated for 10 min at 45 \(^\circ\)C.
Immunoblotting
5 µg of protein extracts from human tissue and 10 µg of protein extracts from mouse tissue were loaded on 8% SDS–polyacrylamide gels, separated by PAGE, and electrophoretically transferred onto 0.45 µm nitrocellulose membranes. The membranes were blocked in 5% non-fat milk in Tris-buffered saline (TBS) for 1 h at room temperature and incubated in primary antibody diluted in milk overnight at 4 \(^\circ\)C. Membranes were washed in TBS and incubated in anti-mouse or anti-rabbit secondary antibodies conjugated to horseradish peroxidase (Jackson ImmunoResearch, West Grove, PA). Following washing in TBS, the membranes were imaged by chemiluminescence using Western Lighting Plus ECL reagents (PerkinElmer Life Sciences, Waltham, MA) and a GeneGnome XRQ imaged system (Syngene, Frederick, MD).
Additional antibodies
Mouse monoclonal antibodies, CP27 and PHF-1 were generous gifts from the late Dr. Peter Davies [26, 60]. Total Tau 3026 rabbit polyclonal antibody was previously described [68, 81]. Mouse monoclonal antibody Tau-5 was purchased from Invitrogen (Waltham, MA). Mouse monoclonal anti-NFL antibody NR4 and mouse monoclonal anti-NFM antibody NN18 were obtained from Sigma (St. Louis, MO). A mouse monoclonal antibody specific for glyceraldehyde-3-phosphate dehydrogenase (GAPDH, clone GA1R) was from Fisher Scientific.
Expression and purification of recombinant human tau isoforms
Human tau isoforms were cloned into the pRK172 bacterial expression vector using NdeI and EcoRI restriction sites as previously described [27, 31, 75]. Recombinant tau isoforms were expressed in Escherichia coli BL21 (New England Biolabs, Ipswich, MA) and purified. In brief, expression was induced by isopropyl-β-D-1-thiogalactopyranoside (IPTG) and high-salt 100 °C heat stable bacterial protein lysates were purified by MonoS cation exchange chromatography.
Analysis of tissue staining and immunoblots
All slides were digitally scanned using an Aperio ScanScope CS instrument (40× magnification; Aperio Technologies Inc., Vista, CA), and images of antibody staining were captured using the ImageScope software (40× magnification; Aperio Technologies Inc). Immunoblots and IHC images were individually white leveled. Brightness and contrast corrections were applied to each IHC figure using Adobe Photoshop (Adobe Systems, San Jose,CA,USA). Raw files are available upon request.
Results
Generation and characterization of novel tau monoclonal antibodies with epitopes in the amino-terminal region
The amino-terminal region of tau is the least studied region of this molecule [12, 55] and there are relatively few available antibodies that target this region. Mice were immunized with a peptide corresponding to residues 19–38 in human tau, numbered according to the 2N/4R human tau isoform, that is upstream of the N1 and N2 alternatively spliced protein segments (Fig. 1a). Two monoclonal antibodies 1B1 and 1H11 were identified by ELISA screen with the original peptide used for immunization as well as recombinant tau proteins. These antibodies recognize all 6 major tau isoforms expressed in the human CNS (Additional file 1: Fig. S1). ELISAs using a peptide spanning residues 15–28 in human tau reveal that these antibodies did not recognize this region of tau (data not shown) indicating that their epitopes include residues 29–38, that has 2 amino acid difference between human and mouse tau (Fig. 1b). To further characterize the specificity of the new antibodies, immunoblotting and IHC were performed using brain tissue from tau KO [22], non-transgenic (nTg), and PS19 tau transgenic mice [84] (Fig. 1c, d). PS19 mice express 1N/4R human tau with the P301S mutation. By immunoblotting, tau that is predominantly expressed as the 0N/4R isoform in adult mouse brain [58] and human 1N/4R transgenic tau in PS19 mice were detected with total tau antibody 3026 (Fig. 1c). Antibodies 1B1 and 1H1 only reacted with human tau and similar to antibody CP27 that is also human tau specific but with an epitope at residues 130–150 in the middle region of tau [26]. IHC analyses also demonstrated that antibodies 1B1 and 1H11 only specifically stained human tau as compared to antibody Tau-5 that reacts with both mouse and human tau [65] (Fig. 1d).
Immunohistochemical analysis with novel antibodies reveal that tau is more abundant in cortical gray matter relative to white matter in human brain
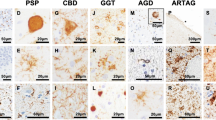
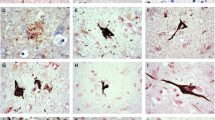
Staining of control cases with new tau antibodies 1B1 and 1H11 revealed predominant staining of cortical gray matter regions (Figs. 2, 3, Additional file 1: S2 and S3). In fact, the cortical gray and white matter were easily distinguished in control tissue from all four regions by staining with these new tau antibodies, which was surprising given the current dogma that tau is predominately an axonal protein (Figs. 2, 3, Additional file 1: S2 and S3). Staining of advanced stages (Braak V/VI) AD brain tissue (Table 1) with new tau antibodies 1B1 and 1H11 labelled NFT, neuropil threads, and dystrophic neurites within senile plaques (Figs. 2, 3, Additional file 1: S2 and S3). While staining in the white matter region revealed sparse tau immunoreactive glial inclusions and processes, in AD brain tissue these antibodies revealed much more intense staining of the gray matter neuropil regions relative to the white matter regions in the frontal cortex (Fig. 2), temporal cortex (Fig. 3), parietal cortex (Additional file 1: Fig. S2), and occipital cortex (Additional file 1: Fig. S3). A similar staining pattern was observed with another human tau antibody, CP27, and this clear difference in tau staining pattern was also observed among brain regions of control and AD individuals (Figs. 2, 3, Additional file 1: S2 and S3). In the cortical gray matter of control cases, neuronal cell bodies, dendrites, and unmyelinated axons were stained in all four regions with the new N-terminal tau antibodies and CP27.
Immunohistochemistry of the frontal cortex of a control individual and an AD individual with phospho-independent tau antibodies. IHC was performed as described in Materials and Methods. A representative control case (a) and a representative AD case (b) were stained with total human tau antibodies 1B1, 1H11, and CP27. Low magnification and high magnification images of gray matter and white matter were taken as indicated. “G” indicates gray matter region. “W” indicates white matter region. Scale bar for low magnification images is 2 mm. Scale bar for high magnification images is 60 µm; and insets 30 µm. Sections were counterstained with hematoxylin
Immunohistochemistry of the temporal cortex of a control individual and an AD individual with phospho-independent tau antibodies. IHC was performed as described in Materials and Methods. A representative control case (a) and a representative AD case (b) were stained with total human tau antibodies 1B1, 1H11, and CP27. Low magnification and high magnification images of gray matter and white matter were taken as indicated. “G” indicates gray matter region. “W” indicates white matter region. Scale bar for low magnification images is 2 mm. Scale bar for high magnification images is 60 µm; and insets 30 µm. Sections were counterstained with hematoxylin
Most antibodies typically used to detect tau pathological inclusions in human brain rely on conformation dependent epitopes or tau phospho-epitopes, as tau can be phosphorylated at many sites that become hyperphosphorylated in disease conditions [77, 83]. Therefore, many antibodies specific for phosphorylated tau have been used to detect pathological inclusions, but these cannot be used to inform us on the normal distribution of tau. Staining of AD brain tissue with one of these antibodies PHF-1, specific for tau phosphorylated at Ser396 and Ser404, revealed NFT, neuropil threads and dystrophic neurites with more robust labeling of the gray matter compared to white matter areas (Additional file 1: Fig. S4). But this difference in staining in AD tissue is confounded by the pathological accumulation of tau in the gray matter as well as tau’s phosphorylation state. In brain tissue from control individuals, a difference in PHF-1 staining intensity between gray and white matter could be observed but it was less obvious than with the phosphorylation independent tau antibodies. In addition, to ensure that this distinct staining pattern was not due to the IHC methodology, human brain tissue was also stained for another neuronal cytoskeletal protein, the neurofilament medium molecular mass subunit (NFM) showing equivalent reactivity in all gray and white brain cortical regions (Additional file 1: Fig. S5).
Biochemical fractionation and immunoblotting analyses reveal that tau is more abundantly present in the gray cortical cerebral tissue than the adjacent white matter tissue
To further investigate the distribution of tau in adult human brain that was revealed by the IHC studies, gray and white matter form the temporal cortex of control and AD brains was carefully dissected and biochemically fractionated (Additional file 1: Fig. S6) followed by immunoblotting analyses. Cortical gray matter is enriched in neuronal cell bodies and dendrites, while the subcortical white matter is enriched in myelinated axons. Immunoblotting with the new tau antibodies 1B1 (Fig. 4) and 1H11 (Additional file 1: Fig. S7) reveal that tau, which migrates as multiple bands around 55 kDa, was predominately found in the HS and Triton/HS fractions and was more abundant within the gray matter cerebral brain cortical tissue compared to the white matter cerebral brain cortical tissue in control brain tissue in the temporal brain region. Several low molecular weight bands between 25 and 37 kDa were observed in the gray and white matter, but these bands were more pronounced in the gray matter. These low molecular weight bands are predicted to be proteolytically cleaved tau products. A similar relative abundance in the gray versus white matter tissue was also observed in AD temporal cortical brain tissue. In AD temporal cortical brain tissue tau was also found in the Sarkosyl/HS-soluble and SDS/urea fractions, predominantly in the gray matter. An additional band at ~ 150 kDa was observed in the Sarkosyl/HS soluble and SDS/urea fractions from AD cases.
Comparative biochemical fraction analyses of gray and white matter from the temporal cortex of AD and control cases with anti-tau antibody 1B1. Biochemical fractionation of AD and CTL cerebral temporal cortex was performed as described in Materials and Methods. Equal amount of protein (5 \(\upmu\)g) from the high salt (HS) soluble, Triton/HS soluble, Sarkosyl/HS soluble, and Sarkosyl-insoluble SDS/urea soluble fractions were separated by SDS-PAGE and analyzed by immunoblotting with tau antibody, 1B1. The HS fractions were also probed for GAPDH and the SDS/urea fractions were probed for NFL. The mobility of protein markers with their molecular masses are indicated on the left side of each immunoblot
These studies were expanded to assess if these tau distribution patterns were also observed in the occipital cortex (Additional file 1: Fig. S8 and S9). Consistent results were obtained where tau was more abundant in the gray matter than the white matter and accumulated as biochemically Triton X-100 insoluble aggregates in AD tissue. To further investigate this distribution of tau in the temporal cortex, the biochemical fractions were also analyzed with another phospho-independent antibody, CP27, where similar results were obtained analyzing biochemical fractions from the temporal (Fig. 5) and occipital cortex (Additional file 1: Fig. S10). As tau in AD brain is hyperphosphorylated, the biochemical fractions were also probed with phosphorylation specific antibody, PHF-1. Hyperphosphorylated tau was predominantly observed in the gray matter of AD individuals within both regions, as indicated by a smear in the gray matter lanes with one case also showing some pathological tau in the white matter in the occipital cortex (Fig. 5, Additional file 1: Fig. S10).
Comparative biochemical fraction analyses of gray and white matter from the temporal cortex of AD and control cases with tau antibodies CP27 and PHF-1. Biochemical fractionation of AD and CTL cerebral temporal cortex was performed as described in Materials and Methods. Equal amount of protein (5 \(\upmu\)g) from the high salt (HS) soluble, Triton/HS soluble, Sarkosyl/HS soluble, and Sarkosyl-insoluble SDS/urea soluble fractions were separated by SDS-PAGE and analyzed by immunoblotting with antibodies CP27 or PHF-1. The mobility of protein markers with their molecular masses are indicated on the left side of each immunoblot
Discussion
Tau was first identified in 1975 as a MAP which colocalizes with MTs and promotes tubulin polymerization reaction [76]. Tau was subsequently further purified and confirmed to have a pivotal role in MT formation [18, 79]. Following the advent of tau monoclonal antibodies raised from immunization with human brain homogenate, it was initially observed by IHC that tau is localized in axons [7, 50, 63]. Many others groups have conducted studies to try to elucidate the distribution of tau using both IHC and biochemical methodology. Consistent with our findings, one group performed IHC staining which found “normal” tau to localize in the neuropil in several brain regions of adult individuals, with limited staining in axons [72]. Other groups performed biochemistry on gray and white matter from adult human frontal cortex from AD and control individuals [46] and bovine brain [1] and found tau to be highly localized in the gray matter. While these studies cast doubt on the current dogma of tau’s axonal localization, they were limited by their use of antibodies which are now known to either cross-reacts with other MAPs, are dependent on tau’s phosphorylation state, or do not react with all tau isoforms. Despite these contradictory results on the neurobiology of tau protein, it still widely accepted as a protein highly enriched in axons with limited involvement in the soma of neurons [7, 25, 35, 39, 42, 50, 63]; and thus tau’s distribution is thought to change under pathological conditions in which tau is re-localized to accumulate towards the soma of neurons [2, 3, 23, 36, 37, 48, 49, 54, 70, 71, 74, 85, 86]. However, the interpretations of many earlier studies were limited due to the fact that many available tau antibodies are dependent on the phosphorylation state of tau or can cross-react to other non-tau proteins such as other MAPs that share sequence homology to tau.
In our study, we evaluated the distribution of tau protein under normal and pathological conditions in the adult human brain using monoclonal antibodies that are not phosphorylation dependent and with epitopes outside of the MT binding region. We used two novel total tau antibodies raised against a phosphorylation independent epitope shared by all 6 tau isoforms in the N-terminus and another phosphorylation independent antibody CP27 with the epitope in the middle region of tau. We demonstrated that these antibodies are highly specific for tau.
IHC was used to assess the distribution of tau in control and AD brain cortical tissue from four distinct cortical regions (temporal, frontal, parietal, and occipital regions) that are differentially affected during the progression of AD as described by Braak staging [10]. We observed strong IHC staining for tau in the neuropil within the gray matter region of control brains in all four regions studied. The staining in the gray matter region was significantly more intense than in the adjacent white matter. In AD tissue, staining for tau in the gray matter was also more intense than in the white matter. Additional immunoreactivity for NFT, neuropil threads, and dystrophic neurites were observed in the cortical gray matter.
The enrichment of tau in the cortical gray matter tissue compared to white matter was confirmed by biochemical fractionation followed by immunoblotting. Sequentially fractionated tau was found to be more abundant in the gray matter which was observed using our new phosphorylation-independent tau antibodies. Soluble tau bands were located at molecular weights of ~ 55 kD as well as 25–37 kD. Tau is known to be cleaved by proteases such as caspases and cathepsins present in neurons which could potentially accounts for these lower molecular weight species [82]. As expected, these studies revealed that Sarkosyl-insoluble tau is present in AD brain tissue but not in controls. However, in AD brains, HS and HS/Triton soluble tau was also present in a more highly phosphorylated state compared to controls as shown with antibody PHF-1. It is not clear if this finding reflects smaller tau aggregates that did not sediment during fractionation or hyperphosphorylated monomeric tau. Collectively, our findings have significant implication for the current dogma about normal tau biology and its pathobiology. Our findings demonstrate that under normal conditions in the human adult brain tau is more abundant in the cortical gray matter region, enriched in neuronal soma and dendrites than the region (white matter) that is predominantly comprised of axons.
Tau has been most vastly studied for its functions as a neuronal MAP where is can regulate MT dynamics and MT interactions with other proteins. Within the somatodendritic compartment of neurons tau can facilitate cellular trafficking as a MAP [5, 13], but it can have many other functions as it known to interact with other neuronal proteins such as actin, other MAPs, scaffolding proteins, protein kinases and phosphatases that are present throughout neurons consistent with tau’s physiological distribution observed herein [39].
Our findings challenge the prevailing notion that tau is mostly an axonal protein under physiological conditions which it is redistributed towards the soma and dendrites in AD brains. Furthermore, many studies have indicated that tau aggregation can exhibit prion-like behavior in which tau competent seeds are able to induce a conformational change in endogenous tau that propels its neuroanatomical pathological spread [4, 11, 14,15,16, 19, 29, 30, 38, 43, 59, 67, 78] reflecting the stage-wise progression of tau pathology described by Braak staging [9, 10]. Using phospho-specific tau antibodies such as PHF-1 or AT8, as well as silver staining, Braak and others demonstrated that tau pathology progressively spreads in the gray matter, typically starting in the entorhinal cortex region of the hippocampal formation [9, 10]. Using highly specific phospho-independent tau antibodies by IHC as well as biochemical fractionation/immunoblotting analysis, we further confirm that pathological tau is predominantly present in the cortical gray matter. The higher abundance of tau in the gray matter likely contributes to its preferential aggregation and spread in these brain regions compared to white matter. However, if prion-like progression plays a major role in the progression of tau pathology it is still puzzling that tau pathology is sparse in the axons of the white matter. In primary neuronal cell culture studies it has been shown that tau aggregates can travel down axons and even seed the formation of tau inclusions in post-synaptic neurons [30, 38]. Perhaps in human adult brain, tau within the white matter axonal compartment is not available for recruitment by tau prion-type seeds as it is mainly sequestered onto MTs or the mechanisms involved in intercellular transmission of seeds occurs preferentially between cell bodies and dendrites. In AD, A\(\upbeta\) brain deposition also occurs predominantly in the gray matter region compared to the white matter so perhaps A\(\upbeta\) plays a critical role in dictating the directionality of pathological tau spread. Maybe the accumulation of A\(\upbeta\) deposits enhance the neuronal activities involved in the secretion/uptake of tau seeds or promote the cellular apparatus that can directly result in intercellular exchange such as nanotubes [30, 38]. These hypotheses will have to be investigated in future studies, but the current findings presented here have important implication for basic tau biology and AD pathogenesis as well as therapeutic targeting.
Conclusions
The data presented here underscore that the current dominant notions on the normal neuronal distribution and function of tau in the adult human brain need significant adjustments. Our data indicate that in adult human brain cortical neurons tau has a more prevailing abundance within the somatodendritic compartments compared to axons. This physiological distribution of tau that mirrors the neuroanatomical deposition of tau inclusion pathology in AD brains also has important implications for the current models on the progressive spread of tau pathology in neurodegenerative diseases.
Abbreviations
- Aβ:
-
Amyloid β
- ABC:
-
Avidin–biotin complex
- AD:
-
Alzheimer’s disease
- CTL:
-
Control
- CNS:
-
Central nervous system
- DAB:
-
3,3′-Diaminobenzidine
- FBS:
-
Fetal bovine serum
- IHC:
-
Immunohistochemistry
- KO:
-
Knockout
- MAP:
-
Microtubule associated protein
- MT:
-
Microtubule
- NFT:
-
Neurofibrillary tangles
- nTg:
-
Non-transgenic
- TBS:
-
Tris-buffered saline
References
De Ancos JG, Avila J (1993) Differential distribution in white and grey matter of tau phosphoisoforms containing four tubulin-binding motifs. Biochem J 296:351–354
Aragão Gomes L, Uytterhoeven V, Lopez-Sanmartin D, Tomé SO, Tousseyn T, Vandenberghe R, Vandenbulcke M, von Arnim CAF, Verstreken P, Thal DR (2021) Maturation of neuronal AD-tau pathology involves site-specific phosphorylation of cytoplasmic and synaptic tau preceding conformational change and fibril formation. Acta Neuropathol 141:173–192. https://doi.org/10.1007/S00401-020-02251-6
Arendt T, Stieler JT, Holzer M (2016) Tau and tauopathies. Brain Res Bull 126:238–292. https://doi.org/10.1016/J.BRAINRESBULL.2016.08.018
Ayers JI, Giasson BI, Borchelt DR (2018) Prion-like Spreading in Tauopathies. Biol Psychiatry 83:337–346. https://doi.org/10.1016/J.BIOPSYCH.2017.04.003
Baas PW, Rao AN, Matamoros AJ, Leo L (2016) Stability properties of neuronal microtubules. Cytoskeleton (Hoboken) 73:442. https://doi.org/10.1002/CM.21286
von Bergen M, Barghorn S, Jeganathan S, Mandelkow EM, Mandelkow E (2006) Spectroscopic approaches to the conformation of tau protein in solution and in paired helical filaments. Neurodegener Dis 3:197–206. https://doi.org/10.1159/000095257
Binder LI, Frankfurter A, Rebhun L (1985) The distribution of tau in the mammalian central nervous system. J Cell Biol 101:1371–1378. https://doi.org/10.1083/JCB.101.4.1371
Binder LI, Frankfurter A, Rebhun LI (1986) Differential localization of MAP-2 and Tau in mammalian neurons in situ. Ann N Y Acad Sci 466:145–166. https://doi.org/10.1111/J.1749-6632.1986.TB38392.X
Braak H, Alafuzoff I, Arzberger T, Kretzschmar H, Tredici K (2006) Staging of Alzheimer disease-associated neurofibrillary pathology using paraffin sections and immunocytochemistry. Acta Neuropathol 112:389–404. https://doi.org/10.1007/s00401-006-0127-z
Braak H, Braak E (1991) Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol 82:239–259. https://doi.org/10.1007/BF00308809
Braak H, Del Tredici K (2016) Potential pathways of abnormal Tau and α-synuclein dissemination in sporadic Alzheimer’s and Parkinson’s siseases. Cold Spring Harb Perspect Biol. https://doi.org/10.1101/CSHPERSPECT.A023630
Buée L, Bussière T, Buée-Scherrer V, Delacourte A, Hof PR (2000) Tau protein isoforms, phosphorylation and role in neurodegenerative disorders. Brain Res Rev 33:95–130. https://doi.org/10.1016/S0165-0173(00)00019-9
Cáceres A, Banker GA, Binder L (1986) lmmunocytochemical localization of tubulin and microtubule-associated protein 2 during the development of hippocampal neurons in culture. J Neurosci 6:714–722
Clavaguera F, Akatsu H, Fraser G, Crowther RA, Frank S, Hench J, Probst A, Winkler DT, Reichwald J, Staufenbiel M, Ghetti B, Goedert M, Tolnay M (2013) Brain homogenates from human tauopathies induce tau inclusions in mouse brain. Proc Natl Acad Sci USA 110:9535–9540. https://doi.org/10.1073/PNAS.1301175110
Clavaguera F, Hench J, Goedert M, Tolnay M (2015) Invited review: Prion-like transmission and spreading of tau pathology. Neuropathol Appl Neurobiol 41:47–58
Clavaguera F, Tolnay M, Goedert M (2017) The prion-like behavior of assembled tau in transgenic mice. Cold Spring Harb Perspect Med 7:a024372. https://doi.org/10.1101/CSHPERSPECT.A024372
Cleveland DW, Hwo SY, Kirschner MW (1977) Purification of tau, a microtubule-associated protein that induces assembly of microtubules from purified tubulin. J Mol Biol 116:207–225. https://doi.org/10.1016/0022-2836(77)90213-3
Cleveland DW, Hwo SY, Kirschner MW (1977) Physical and chemical properties of purified tau factor and the role of tau in microtubule assembly. J Mol Biol 116:227–247. https://doi.org/10.1016/0022-2836(77)90214-5
Cope TE, Rittman T, Borchert RJ, Jones PS, Vatansever D, Allinson K, Passamonti L, Vazquez Rodriguez P, Bevan-Jones WR, O’Brien JT, Rowe JB (2018) Tau burden and the functional connectome in Alzheimer’s disease and progressive supranuclear palsy. Brain 141:550. https://doi.org/10.1093/BRAIN/AWX347
Crowther RA, Olesen OF, Smith MJ, Jakes R, Goedert M (1994) Assembly of Alzheimer-like filaments from full-length tau protein. FEBS Lett 337:135–138. https://doi.org/10.1016/0014-5793(94)80260-2
Crowther T, Goedert M, Wischik CM (1989) The repeat region of microtubule-associated protein tau forms part of the core of the paired helical filament of Alzheimer’s disease. Ann Med 21:127–132. https://doi.org/10.3109/07853898909149199
Dawson HN, Ferreira A, Eyster MV, Ghoshal N, Binder LI, Vitek MP (2001) Inhibition of neuronal maturation in primary hippocampal neurons from tau deficient mice. J Cell Sci 114:1179–1187. https://doi.org/10.1242/JCS.114.6.1179
Delacourte A, Flament S, Dibe EM, Hublau P, Sablnnière P, Hémon B, Shérrer V, Défossez A (1990) Pathological proteins Tau 64 and 69 are specifically expressed in the somatodendritic domain of the degenerating cortical neurons during Alzheimer’s disease. Demonstration with a panel of antibodies against Tau proteins. Acta Neuropathol 80:111–117. https://doi.org/10.1007/BF00308912
Deture MA, Dickson DW (2019) The neuropathological diagnosis of Alzheimer’s disease. Mol Neurodegener 14(1):32. https://doi.org/10.1186/s13024-019-0333-5
Dotti CG, Banker GA, Binder LI (1987) The expression and distribution of the microtubule-associated proteins tau and microtubule-associated protein 2 in hippocampal neurons in the rat in situ and in cell culture. Neuroscience 23:121–130. https://doi.org/10.1016/0306-4522(87)90276-4
Duff K, Knight H, Refolo LM, Sanders S, Yu X, Picciano M, Malester B, Hutton M, Adamson J, Goedert M, Burki K, Davies P (2000) Characterization of pathology in transgenic mice over-expressing human genomic and cDNA tau transgenes. Neurobiol Dis 7:87–98. https://doi.org/10.1006/NBDI.1999.0279
Giasson BI, Forman MS, Higuchi M, Golbe LI, Graves CL, Kotzbauer PT, Trojanowski JQ, Lee VMY (2003) Initiation and synergistic fibrillization of tau and alpha-synuctein. Science 300:636–640. https://doi.org/10.1126/SCIENCE.1082324/SUPPL_FILE/GIASSONSOM.PDF
Goedert M (1997) The neurofibrillary pathology of Alzheimer’s disease. Neuroscientist 3:131–141. https://doi.org/10.1177/107385849700300212
Goedert M (2015) Alzheimer’s and Parkinson’s diseases: the prion concept in relation to assembled Aβ, tau, and α-synuclein. Science 349:1255555. https://doi.org/10.1126/SCIENCE.1255555
Goedert M, Eisenberg DS, Crowther RA (2017) Propagation of Tau aggregates and neurodegeneration. Annu Rev Neurosci 40:189–210. https://doi.org/10.1146/ANNUREV-NEURO-072116-031153
Goedert M, Jakes R (1990) Expression of separate isoforms of human tau protein: Correlation with the tau pattern in brain and effects on tubulin polymerization. EMBO J 9:4225–4230
Goedert M, Spillantini MG, Jakes R, Crowtherp RA, Vanmechelen E, Probst A, Götz J, Bürki K, Cohen P (1995) Molecular dissection of the paired helical filament. Neurobiol Aging 16:325–334. https://doi.org/10.1016/0197-4580(95)00017-9
Goedert M, Spillantini MG, Jakes R, Rutherford D, Crowther RA (1989) Multiple isoforms of human microtubule-associated protein tau: sequences and localization in neurofibrillary tangles of Alzheimer’s disease. Neuron 3:519–526. https://doi.org/10.1016/0896-6273(89)90210-9
Goedert M, Wischik CM, Crowther RA, Walker JE, Klug A (1988) Cloning and sequencing of the cDNA encoding a core protein of the paired helical filament of Alzheimer disease: identification as the microtubule-associated protein tau. Proc Natl Acad Sci USA 85:4051–4055. https://doi.org/10.1073/PNAS.85.11.4051
Gotz J, Probst A, Spillantini MG, Schafer T, Jakes R, Burki K, Goedert M (1995) Somatodendritic localization and hyperphosphorylation of tau protein in transgenic mice expressing the longest human brain tau isoform. EMBO J 14:1304–1313
Grundke-Iqbal I, Iqbal K, Quinlan M, Tung YC, Zaidi MS, Wisniewski HM (1986) Microtubule-associated protein tau. A component of Alzheimer paired helical filaments. J Biol Chem 261:6084–6089. https://doi.org/10.1016/S0021-9258(17)38495-8
Grundke-Iqbal I, Iqbal K, Tung YC, Quinlan M, Wisniewski HM, Binder LI (1986) Abnormal phosphorylation of the microtubule-associated protein tau (tau) in Alzheimer cytoskeletal pathology. Proc Natl Acad Sci USA 83:4913–4917. https://doi.org/10.1073/PNAS.83.13.4913
Guo JL, Lee VMY (2014) Cell-to-cell transmission of pathogenic proteins in neurodegenerative diseases. Nat Med 20:130–138. https://doi.org/10.1038/NM.3457
Guo T, Noble W, Hanger DP (2017) Roles of tau protein in health and disease. Acta Neuropathol 133:665–704. https://doi.org/10.1007/S00401-017-1707-9
Gustke N, Trinczek B, Biernat J, Mandelkow EM, Mandelkow E (1994) Domains of tau protein and interactions with microtubules. Biochemistry 33:9511–9522. https://doi.org/10.1021/BI00198A017
Hasegawa M, Morishima-Kawashima M, Takio K, Suzuki M, Titani K, Ihara Y (1992) Protein sequence and mass spectrometric analyses of tau in the Alzheimer’s disease brain. J Biol Chem 267:17047–17054. https://doi.org/10.1016/S0021-9258(18)41890-X
Higuchi M, Lee VMY, Trojanowski JQ (2002) Tau and axonopathy in neurodegenerative disorders. NeuroMolecular Med 2:131–150. https://doi.org/10.1385/NMM:2:2:131
Holmes BB, Diamond MI (2014) Prion-like properties of Tau protein: the importance of extracellular Tau as a therapeutic target. J Biol Chem 289:19855–19861. https://doi.org/10.1074/JBC.R114.549295
Jeganathan S, Von Bergen M, Mandelkow EEM, Mandelkow EEM (2008) The natively unfolded character of tau and its aggregation to Alzheimer-like paired helical filaments. Biochemistry 47:10526–10539. https://doi.org/10.1021/BI800783D
Kellogg EH, Hejab NMA, Poepsel S, Downing KH, DiMaio F, Nogales E (2018) Near-atomic model of microtubule-tau interactions. Science 360:1242–1246. https://doi.org/10.1126/SCIENCE.AAT1780
Khatoon S, Grundke-Iqbal I, Iqbal K (1994) Levels of normal and abnormally phosphorylated tau in different cellular and regional compartments of Alzheimer disease and control brains. FEBS Lett 351:80–84. https://doi.org/10.1016/0014-5793(94)00829-9
Kidd M (1963) (1963) Paired helical filaments in electron microscopy of Alzheimer’s disease. Nat 1974863(197):192–193. https://doi.org/10.1038/197192b0
Konzack S, Thies E, Marx A, Mandelkow EM, Mandelkow E (2007) Swimming against the tide: Mobility of the microtubule-associated protein tau in neurons. J Neurosci 27:9916–9927. https://doi.org/10.1523/JNEUROSCI.0927-07.2007
Kosik KS, Crandall JE, Mufson EJ, Neve RL (1989) Tau in situ hybridization in normal and Alzheimer brain: Localization in the somatodendritic compartment. Ann Neurol 26:352–361. https://doi.org/10.1002/ANA.410260308
Kosik KS, Finch EA (1987) MAP2 and tau segregate into dendritic and axonal domains after the elaboration of morphologically distinct neurites: an immunocytochemical study of cultured rat cerebrum. J Neurosci 7:3142–3153. https://doi.org/10.1523/JNEUROSCI.07-10-03142.1987
Kosik KS, Joachim CL, Selkoe DJ (1986) Microtubule-associated protein tau (τ) is a major antigenic component of paired helical filaments in Alzheimer disease. Proc Natl Acad Sci USA 83:4044–4048
Lee VMY, Balin BJ, Otvos L, Trojanowski JQ (1991) A68: a major subunit of paired helical filaments and derivatized forms of normal Tau. Science 251:675–678. https://doi.org/10.1126/SCIENCE.1899488
Lee VMY, Goedert M, Trojanowski JQ (2001) Neurodegenerative tauopathies. Annu Rev Neurosci 24:1121–1159. https://doi.org/10.1146/ANNUREV.NEURO.24.1.1121
Li X, Kumar Y, Zempel H, Mandelkow EEM, Biernat J, Mandelkow EEM (2011) Novel diffusion barrier for axonal retention of Tau in neurons and its failure in neurodegeneration. EMBO J 30:4825–4837. https://doi.org/10.1038/EMBOJ.2011.376
Mandelkow E-M, Mandelkow E (2012) Biochemistry and cell biology of Tau protein in neurofibrillary degeneration. Cold Spring Harb Perspect Med 2:1–25. https://doi.org/10.1101/CSHPERSPECT.A006247
Mandelkow EM, Schweers O, Drewes G, Biernat J, Gustke N, Trinczek B, Mandelkow E (1996) Structure, microtubule interactions, and phosphorylation of tau protein. Ann N Y Acad Sci 777:96–106. https://doi.org/10.1111/J.1749-6632.1996.TB34407.X
Matsuo ES, Shin RW, Billingsley ML, Van deVoorde A, O’Connor M, Trojanowski JQ, Lee VMY (1994) Biopsy-derived adult human brain tau is phosphorylated at many of the same sites as Alzheimer’s disease paired helical filament tau. Neuron 13:989–1002. https://doi.org/10.1016/0896-6273(94)90264-X
McMillan P, Korvatska E, Poorkaj P, Evstafjeva Z, Robinson L, Greenup L, Leverenz J, Schellenberg GD, D’Souza I (2008) Tau isoform regulation is region and cell-specific in mouse brain. J Comp Neurol 511:788. https://doi.org/10.1002/CNE.21867
Mudher A, Colin M, Dujardin S, Medina M, Dewachter I, Naini MA, Mandelkow E-M, Mandelkow E, Buée L, Goedert M, Brion J-P (2017) What is the evidence that tau pathology spreads through prion-like propagation? Acta Neuropathol Commun 5:99. https://doi.org/10.1186/s40478-017-0488-7
Otvos L, Feiner L, Lang E, Szendrei GI, Goedert M, Lee VM (1994) Monoclonal antibody PHF-1 recognizes Tau protein phosphorylated at serine residue 396 and 404. J Neurosci Res 39:669–673. https://doi.org/10.1002/JNR.490390607
Papasozomenos SC, Binder LI (1987) Phosphorylation determines two distinct species of Tau in the central nervous system. Cell Motil Cytoskeleton 8:210–226. https://doi.org/10.1002/CM.970080303
Peng C, Trojanowski JQ, Lee VM-Y (2020) Protein transmission in neurodegenerative disease. Nat Rev Neurol 16:199–212. https://doi.org/10.1038/s41582-020-0333-7
Peng I, Binder LI, Black MM (1986) Biochemical and immunological analyses of cytoskeletal domains of neurons. J Cell Biol 102:252–262. https://doi.org/10.1083/JCB.102.1.252
Petry FR, Pelletier J, Bretteville A, Morin F, Calon F, H́ebert SS, Whittington RA, Planel E, (2014) Specificity of anti-Tau antibodies when analyzing mice models of Alzheimer’s disease: problems and solutions. PLoS ONE 9:e94251. https://doi.org/10.1371/JOURNAL.PONE.0094251
Porzig R, Singer D, Hoffmann R (2007) Epitope mapping of mAbs AT8 and Tau5 directed against hyperphosphorylated regions of the human tau protein. Biochem Biophys Res Commun 358:644–649. https://doi.org/10.1016/J.BBRC.2007.04.187
Rutherford NJ, Brooks M, Giasson BI (2016) Novel antibodies to phosphorylated α-synuclein serine 129 and NFL serine 473 demonstrate the close molecular homology of these epitopes. Acta Neuropathol Commun 4:80
Strang KH, Golde TE, Giasson BI (2019) MAPT mutations, tauopathy, and mechanisms of neurodegeneration. Lab Invest 99:912. https://doi.org/10.1038/S41374-019-0197-X
Strang KH, Goodwin MS, Riffe C, Moore BD, Chakrabarty P, Levites Y, Golde TE, Giasson BI (2017) Generation and characterization of new monoclonal antibodies targeting the PHF1 and AT8 epitopes on human tau. Acta Neuropathol Commun 5:58. https://doi.org/10.1186/s40478-017-0458-0
Szendrei GI, Lee VM, Otvos L (1993) Recognition of the minimal epitope of monoclonal antibody Tau-1 depends upon the presence of a phosphate group but not its location. J Neurosci Res 34:243–249. https://doi.org/10.1002/JNR.490340212
Tashiro K, Hasegawa M, Ihara Y, Iwatsubo T (1997) Somatodendritic localization of phosphorylated tau in neonatal and adult rat cerebral cortex. NeuroReport 8(12):2797–2801
Thies E, Mandelkow EM (2007) Missorting of tau in neurons causes degeneration of synapses that can be rescued by the kinase MARK2/Par-1. J Neurosci 27:2896–2907. https://doi.org/10.1523/JNEUROSCI.4674-06.2007
Trojanowski JQ, Schuck T, Schmidt ML, Lee VMY (1989) Distribution of tau proteins in the normal human central and peripheral nervous system. J Histochem Cytochem 37:209–215. https://doi.org/10.1177/37.2.2492045
Viereck C, Tucker RP, Binder LI, Matus A (1988) Phylogenetic conservation of brain microtubule-associated proteins MAP2 and tau. Neuroscience 26:893–904. https://doi.org/10.1016/0306-4522(88)90107-8
Wang Y (2015) Mandelkow E (2015) Tau in physiology and pathology. Nat Rev Neurosci 171(17):22–35. https://doi.org/10.1038/nrn.2015.1
Waxman EA, Giasson BI (2011) Induction of intracellular tau aggregation is promoted by α-synuclein seeds and provides novel insights into the hyperphosphorylation of tau. J Neurosci 31:7604–7618. https://doi.org/10.1523/JNEUROSCI.0297-11.2011
Weingarten M, Lockwood A, Hwo S, Kirschner M (1975) A protein factor essential for microtubule assembly. Proc Natl Acad Sci USA 72:1858–1862. https://doi.org/10.1073/PNAS.72.5.1858
Wesseling H, Mair W, Kumar M, Schlaffner CN, Tang S, Beerepoot P, Fatou B, Guise AJ, Cheng L, Takeda S, Muntel J, Rotunno MS, Dujardin S, Davies P, Kosik KS, Miller BL, Berretta S, Hedreen JC, Grinberg LT, Seeley WW, Hyman BT, Steen H, Steen JA (2020) Tau PTM profiles identify patient heterogeneity and stages of Alzheimer’s disease. Cell 183:1699–1713.e13. https://doi.org/10.1016/J.CELL.2020.10.029
Wischik CM, Schelter BO, Wischik DJ, Storey JMD, Harrington CR (2018) Modeling prion-like processing of Tau protein in Alzheimer’s disease for pharmaceutical development. J Alzheimers Dis 62:1287–1303. https://doi.org/10.3233/JAD-170727
Witman GB, Cleveland DW, Weingarten MD, Kirschner MW (1976) Tubulin requires tau for growth onto microtubule initiating sites. Proc Natl Acad Sci USA 73:4070–4074. https://doi.org/10.1073/PNAS.73.11.4070
Wolozin BL, Pruchnicki A, Dickson DW, Davies P (1986) A neuronal antigen in the brains of Alzheimer patients. Science 232:648–650. https://doi.org/10.1126/SCIENCE.3083509
Xia Y, Bell BM, Giasson BI (2021) Tau K321/K353 pseudoacetylation within KXGS motifs regulates tau–microtubule interactions and inhibits aggregation. Sci Rep 11:17069. https://doi.org/10.1038/S41598-021-96627-7
Xia Y, Lloyd GM, Giasson BI (2021) Targeted proteolytic products of τ and α-synuclein in neurodegeneration. Essays Biochem 65:905–912. https://doi.org/10.1042/EBC20210028
Xia Y, Prokop S, Giasson BI (2021) “Don’t Phos Over Tau”: recent developments in clinical biomarkers and therapies targeting tau phosphorylation in Alzheimer’s disease and other tauopathies. Mol Neurodegener 16:37. https://doi.org/10.1186/S13024-021-00460-5
Yoshiyama Y, Higuchi M, Zhang B, Huang SM, Iwata N, Saido TCC, Maeda J, Suhara T, Trojanowski JQ, Lee VMY (2007) Synapse loss and microglial activation precede tangles in a P301S tauopathy mouse model. Neuron 53:337–351. https://doi.org/10.1016/J.NEURON.2007.01.010
Zempel H, Dennissen FJA, Kumar Y, Luedtke J, Biernat J, Mandelkow E-M, Mandelkow E (2017) Axodendritic sorting and pathological missorting of Tau are isoform-specific and determined by axon initial segment architecture. J Biol Chem 292:12192–12207. https://doi.org/10.1074/JBC.M117.784702
Zempel H, Mandelkow E (2014) Lost after translation: missorting of Tau protein and consequences for Alzheimer disease. Trends Neurosci 37:721–732. https://doi.org/10.1016/J.TINS.2014.08.004
Acknowledgements
We would like to thank Jennifer Phillips, Gabriela Hery, and Qing-Shan Xue for their excellent technical assistance. We would also like to thank the patients and their caregivers for their generous contributions to our study.
Funding
This work was supported by grants from the National Institute on Aging (P30AG066506, P50AG047266).
Author information
Authors and Affiliations
Contributions
G.P., S.P., B.I.G. conceived and designed the experiments; G.P., B.M.B., K.G., B.I.G. performed the experiments; G.P., S.P., B.I.G. analyzed the data; G.P., B.I.G. wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures were performed according to the National Institute of Health Guide for the Care and Use of Experimental Animals and were approved by the University of Florida Institutional Animal Care and Use Committee. Post mortem human tissue studies were performed with approval of the University of Florida institutional review board.
Consent for publication
Informed consent was obtained according to guidelines of the University of Florida institutional review board.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
We declare no conflict of interest in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Additional data on the characterization of novel tau antibodies and the distribution of tau in human brains by immunohistochemistry and biochemical analyses.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Paterno, G., Bell, B.M., Gorion, KM.M. et al. Reassessment of Neuronal Tau Distribution in Adult Human Brain and Implications for Tau Pathobiology. acta neuropathol commun 10, 94 (2022). https://doi.org/10.1186/s40478-022-01394-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40478-022-01394-9