Abstract
The deposition of aggregated proteins is a common neuropathological denominator for neurodegenerative disorders. Experimental evidence suggests that disease propagation involves prion-like mechanisms that cause the spreading of template-directed aggregation of specific disease-associated proteins. In transgenic (Tg) mouse models of superoxide dismutase-1 (SOD1)-linked amyotrophic lateral sclerosis (ALS), inoculation of minute amounts of human SOD1 (hSOD1) aggregates into the spinal cord or peripheral nerves induces premature ALS-like disease and template-directed hSOD1 aggregation that spreads along the neuroaxis. This infectious nature of spreading pathogenic aggregates might have implications for the safety of laboratory and medical staff, recipients of donated blood or tissue, or possibly close relatives and caregivers. Here we investigate whether transmission of ALS-like disease is unique to the spinal cord and peripheral nerve inoculations or if hSOD1 aggregation might spread from the periphery into the central nervous system (CNS). We inoculated hSOD1 aggregate seeds into the peritoneal cavity, hindlimb skeletal muscle or spinal cord of adult Tg mice expressing mutant hSOD1. Although we used up to 8000 times higher dose—compared to the lowest dose transmitting disease in spinal cord inoculations—the peripheral inoculations did not transmit seeded aggregation to the CNS or premature ALS-like disease in hSOD1 Tg mice. Nor was any hSOD1 aggregation detected in the liver, kidney, skeletal muscle or sciatic nerve. To explore potential reasons for the lack of disease transmission, we examined the stability of hSOD1 aggregates and found them to be highly vulnerable to both proteases and detergent. Our findings suggest that exposed individuals and personnel handling samples from ALS patients are at low risk of any potential transmission of seeded hSOD1 aggregation.
Similar content being viewed by others
Introduction
Amyotrophic lateral sclerosis (ALS) is characterized by adult-onset progressive degeneration of upper and lower motor neurons. Symptoms begin focally and then spread contiguously, resulting in progressive paralysis and death from respiratory failure [18]. Previous research suggests that age-related neurodegenerative disorders, including Alzheimer’s disease (AD), Parkinson’s disease (PD), multiple system atrophy (MSA), frontotemporal dementia, and ALS share a common pathogenic mechanism involving a prion-like spread of disease-associated misfolded protein aggregates [4, 11, 23, 43, 48]. Prion-like spread in neurodegenerative diseases may have implications for the safety of relatives, medical staff, and recipients of donated blood or tissue, especially if protein aggregates are able to spread from the periphery into the central nervous system (CNS).
Mutations in the gene encoding superoxide dismutase-1 (SOD1) can cause ALS [53] and are found in 1–9% of all patients, depending on the population [1]. Cytoplasmic neuronal inclusions containing aggregated SOD1 are a hallmark of ALS, both in patients and transgenic (Tg) animal models overexpressing mutant human SOD1 (hSOD1) [32]. A number of studies have provided compelling evidence for a prion-like propagation of hSOD1 aggregation in cell cultures [8, 19, 26, 27, 47, 49]. We previously showed that inoculation of two distinct strains (type A and B) of hSOD1 aggregate seeds, prepared from the spinal cords from terminally ill Tg ALS-model mice into the spinal cords of asymptomatic Tg mice expressing mutant hSOD1, induced spreading of template-directed hSOD1 aggregation and premature fatal ALS-like disease [10, 11]. Furthermore, inoculation of ALS patient-derived hSOD1 aggregate seeds into the spinal cord also induced spreading aggregation, and an aggressive premature motor neuron disease in hSOD1 Tg mice [23]. Moreover, Ayers et al. found that both spinal cord and sciatic nerve inoculations, using homogenates from spinal cords of terminally ill hSOD1 Tg mice, transmit ALS-like disease in mice expressing hSOD1 fused to yellow fluorescent protein [5, 6].
Similar to the infectious isoform of prion protein (PrPSc), aggregates of alpha-synuclein (αSyn), β-amyloid (Aβ), and tau are able to invade the CNS and induce seeded aggregation after peripheral injection in Tg mouse models of PD, MSA and AD [15, 17, 21, 22, 38, 54, 59]. In the case of PD, several studies have further suggested that αSyn aggregation may initially develop in the olfactory bulb, or the gut, and propagate to the CNS via neuroanatomically connected tracts [13, 14, 28, 34, 51].
Here we aimed to investigate whether efficient spread of seeded hSOD1 aggregation and ALS-like symptoms is unique to direct inoculations into the CNS and peripheral nerve, or if peripherally administered hSOD1 aggregates have the potential to spread into the CNS, e.g. via the circulation or neuromuscular junctions. We inoculated large amounts of hSOD1 aggregates into the peritoneal cavity or hindlimb skeletal muscle of adult asymptomatic hSOD1G85R Tg mice. In contrast to the highly pathogenic spinal cord inoculations, peripheral administration of hSOD1 aggregates did not induce spreading aggregation and premature ALS in the recipient mice. To explore potential reasons for the lack of transmission, we examined the stability of strain A hSOD1 aggregates and found them to be highly vulnerable to both proteases and detergent. Our findings suggest a low risk of transmission for potentially exposed individuals and medical staff handling samples from ALS patients carrying SOD1 mutations.
Materials and methods
Mouse husbandry and procedures
In this study, we used hemizygous Tg mice that express hSOD1G85R (line 148) [16] that were backcrossed for more than 30 generations and maintained on the C57BL/6J background. In our colony, the average lifespan of hSOD1G85R mice is 398 ± 42 days (n = 86). There was no significant difference in lifespan between the sexes: females 401 ± 42 days (n = 38); males 395 ± 43 days (n = 48). Sacrificed non-Tg C57BL/6J mice from the breeding colony were used to make control spinal cord homogenates. All animals were housed under environmentally controlled standard conditions with a 12 h light/dark cycle and free access to food and water. To facilitate free access after the onset of paresis symptoms, a plate with wet food on the floor was provided daily.
Reagents and chemicals
Reagents and chemicals were obtained from Sigma-Aldrich or Thermo Fisher Scientific unless stated otherwise.
Preparation of spinal cord homogenates used for inoculations
Homogenates containing strain A hSOD1 aggregates were prepared from the spinal cord and brainstem of terminally ill hSOD1G85R Tg mice (359–446 days old) and control inoculum from a 300-day-old non-Tg C57BL/6 mouse. Whole spinal cords and brainstem from the mice were homogenized in 10 weight volumes (w/v) of phosphate-buffered saline (PBS) using an Ultraturrax apparatus (IKA) for 20 s followed by sonication for 1 min and centrifugation at 1000 g for 10 min at 4 °C. The resulting supernatants were aliquoted and stored at − 80 °C until used for inoculations.
The hSOD1G85R spinal cord homogenate contained 10 µg/ml of total hSOD1 and 1.62 µg/ml detergent-resistant hSOD1 aggregates. The total protein contents of the hSOD1G85R and control homogenates were 2079 µg/ml and 2956 µg/ml, respectively, and were analyzed using the Pierce BCA Protein Assay (Thermo Fisher Scientific).
Inoculations
Before surgeries, the recipient mice were anesthetized with 5% isofluorane (Baxter) in an induction chamber. The mice were fixed on a small animal stereotactic frame (Kopf Instruments) and anesthesia was maintained with 1.5–2% isofluorane via a facemask. Before starting the surgery, mice were injected subcutaneously with Carprofen (Rimadyl, 5 mg/kg, Pfizer) to relieve pain. The body temperature was monitored and regulated with a TCAT-2LV temperature controller (AgnTho's). After surgeries, physiological saline was injected subcutaneously for rehydration, and mice were placed on a heating blanket for recovery before being returned to their home cage. After the procedure, mice were monitored to ensure full mobility and no signs of impairment. Surgery clips were removed two weeks after surgery.
Intramuscular inoculations (i.m.) of the spinal cord homogenates were performed in ~ 100-day-old asymptomatic hSOD1G85R Tg mice. Mice were anesthetized, and the incision site was shaved and disinfected. A small incision in the skin of the right hindlimb to expose the quadriceps femoris muscle. The needle was inserted ∼ 1 mm deep into the right quadriceps femoris muscle and 10 µl of spinal cord homogenate was injected into the muscle during 3 min. Injections were performed using a 10 µl syringe with a beveled 26-gauge needle (Hamilton). Separate syringes were used for each type of inoculum to prevent any contamination. The syringe was then slowly retracted over 3 min and the skin incision closed with stainless steel clips (Reflex Autoclip System, 10 mm, AgnTho’s).
Spinal cord inoculations were performed as previously described [11, 23]. In summary, the recipient ~ 100-day-old asymptomatic hSOD1G85R Tg mice were anesthetized, and 1 µl of the spinal cord homogenate from the hSOD1G85R, or control mice was inoculated into the ventral horn of the left lumbar spinal cord between two vertebrae at the L2–L3 level. Injections were performed using a 5 µl syringe with a 33-gauge needle (Hamilton).
Intraperitoneal inoculations (i.p.) were performed in asymptomatic hSOD1G85R Tg mice that received two injections, each containing 150 µl of the spinal cord homogenate, and administered one week apart. No anesthesia was used on these animals.
Monitoring of mice
All mice were examined and weighed weekly. No obvious disturbances in bladder control or hindlimb sensory response were observed in any of the inoculated mice. Mice were sacrificed when considered terminally ill. The criterion for the terminal ALS-like disease was defined as advanced paralysis in both hindlimbs or more than 20% loss of body weight. In mice with prominent forelimb symptoms, end-stage criteria also included severe eye infection.
Excluded mice
Seven i.m. and one spinal cord inoculated hSOD1G85R Tg mice were excluded and not reported in Results, Discussion, Figures or Tables. Four mice that received i.m. inoculation of homogenate from hSOD1G85R Tg spinal cord were euthanized 15, 62, 62, and 112 days after inoculation, respectively, due to non-surgery-related wounds. Three mice inoculated intramuscularly with homogenates from control mice were euthanized 44, 45, and 48 days after inoculation, respectively, due to non-surgery-related wounds. One mouse that received spinal cord inoculation with a 1:3 diluted homogenate from hSOD1G85R Tg spinal cord was euthanized 57 days after inoculation due to wound infection adjacent to the injection site. None of the excluded mice showed any paretic symptoms.
Tissue handling and immunohistochemistry
The i.p. inoculated mice were sacrificed following a lethal i.p. injection of pentobarbital (60 mg/mL, APL Pharma) and perfused transcardially with PBS. Peripheral tissues (liver, kidney, quadriceps femoris muscle, and sciatic nerve) were collected and snap-frozen in liquid nitrogen. The spinal cord was retrieved by flushing with saline using a syringe inserted caudally to sacral levels and was divided into two sagittal halves, and then into lumbar, thoracic, and cervical segments. One lateral half of each segment was snap-frozen in liquid nitrogen. Frozen tissues were stored at − 80 °C until analysis. The other half of the spinal cord was immersion fixed in formalin for histopathology. The brains were dissected and divided into right and left hemispheres, cerebellum, and brainstem, and processed like the spinal cords. Fixed tissue was paraffin-embedded and 5 µm thick sections were cut with a microtome (Microm HM400) and mounted on glass slides.
Sections from the lumbar spinal cord and brainstem from six i.p. hSOD1G85R homogenate inoculated and six control inoculated mice were processed for immunohistological analysis.
For immunofluorescence staining sections were deparaffinized, rehydrated, and pre-treated with Cell Conditioning 1 (CC1, pH 6, Ventana Medical Systems) solution at 95 °C for 76 min using the Ventana Benchmark Ultra (Ventana Medical Systems). After blocking with 10% (v/v) fetal bovine serum (FBS) in Tris-buffered saline (TBS) containing 0.3% (v/v) Triton X-100 for 1 h at room temperature, sections were incubated with 5% (v/v) FBS in TBS containing 0.1% (v/v) Triton X-100 overnight at 4 °C with primary antibodies. The primary antibodies used were a rabbit anti-hSOD1 antibody raised against a peptide corresponding to amino acids (aa) 131–153 (0.96 μg/ml) and a biotinylated Griffonia Simplicifolia Lectin I (GSL I) isolectin B4 (20 μg/ml, B-1205, Vector Laboratories). Sections were washed with TBS and incubated for 2 h at room temperature with Alexa-Fluor conjugated Streptavidin (1:1000, Invitrogen) and 4′,6-diamidino-2-phenylindole (DAPI; 0.3 μM, Sigma-Aldrich) for nuclear counterstaining. Following washing with TBS, sections were mounted with a Fluorescence Mounting Media (Dako). Images were obtained using an Olympus BX 61 microscope equipped with cellSens Dimension imaging software (cellSens Dimension 1.11, Olympus).
Quantitative binary epitope-mapping assay
Human SOD1 aggregate contents in the peripheral tissues of i.p. inoculated hSOD1G85R Tg mice were quantified using a binary epitope-mapping (BEM) assay previously described [10]. Tissue homogenates were prepared from the lumbar, thoracic, and cervical spinal cord, brainstem, brain, cerebellum, liver, kidney, quadriceps femoris muscle, and sciatic nerve of i.p. inoculated hSOD1G85R Tg mice. Tissues were homogenized in 25 volumes of ice-cold PBS containing 1.8 mM EDTA, 1 mM DTT, and a Complete EDTA-free protease inhibitor cocktail (Roche Diagnostics) using an Ultraturrax apparatus (IKA) for 20 s followed by sonication 1 min. The resulting crude tissue homogenates were stored at − 80 °C for the subsequent analysis of hSOD1 aggregate contents. The tissue homogenates were further diluted in 20 volumes of PBS containing 1 mM DTT, 1.8 mM EDTA, and 1% (v/v) Nonidet P-40 (NP-40), sonicated for 30 s, and centrifuged at 1000 g for 10 min at 4 °C. The resulting supernatants were serially diluted 1:1 in PBS and hSOD1 aggregates were captured on 0.2 µm cellulose acetate filters using a 96-well dot-blot apparatus (Whatman GmbH). The blots were incubated with an anti-hSOD1 primary antibody overnight at 4 °C and developed as described for western blotting. The hSOD1 aggregate content in tissue extracts was determined similar to western blot analysis. The primary antibody used for the quantitative BEM assay was a rabbit antibody raised against a peptide corresponding to aa 57–72 of hSOD1. Of the eight anti-peptide antibodies that cover the hSOD1 sequence and are used in the BEM analysis, this antibody gives the strongest reaction with strain A aggregates. As standard for quantification by BEM assay, we used a frozen aliquot of a spinal cord homogenate from an end-stage hSOD1G93A Tg mouse (set to 1).
Human SOD1 antibodies
The hSOD1 antibodies used in this study were raised against peptides corresponding to aa 24–39, 57–72, and 131–153 in rabbits as previously described [25, 29], and purified using Protein A-Sepharose (GE Healthcare) followed by Sulfolink gel coupled to the respective target peptides (Thermo Fisher Scientific).
Strain A aggregate preparations for stability tests
Whole spinal cords from end-stage hSOD1G85R Tg mice were homogenized in 5 volumes of ice-cold PBS containing 1.8 mM EDTA, 0.25 M guanidinium chloride, 2% (v/v) NP-40, and a Complete EDTA-free protease inhibitor cocktail (Roche Diagnostics) using an Ultraturrax apparatus (IKA) for 20 s followed by sonication for 2 min. The homogenate was then diluted with 0.66 volumes of water containing 1% (v/v) NP-40 to achieve physiological ionic strength (0.15 M salt), sonicated for 1 min, and centrifuged at 1000 g for 20 min at 4 °C. The supernatant was collected, supplemented with 3% iohexol and transferred to 4 ml UltraClear flexible ultracentrifugation tubes (Thermo Fisher Scientific) containing 0.25 ml (2 mm height) of 75.5% iohexol, followed by a layering of 1.5 ml (10 mm) of 13% iohexol, 1.5 ml (10 mm) of the homogenate containing 3% iohexol, and finally ≈ 0.75 ml PBS to fill up the tubes. The homogenate was then centrifuged through the iohexol density cushion for 2 h at 360,000 g at 4 °C and the suspension containing aggregated hSOD1 and other heavy components that sedimented to the 13%/75.5% iohexol interphase was collected. The iohexol was removed by dialysis against PBS (pH 7.0). The resulting preparation, which contained 1.39 µg/ml detergent-resistant hSOD1G85R aggregates and 526 µg/ml total protein, was aliquoted and stored at -80 °C until used for stability analysis of the strain A hSOD1 aggregates.
Quantification of detergent-resistant hSOD1 aggregates
To determine the content of detergent-resistant hSOD1 aggregates in the homogenate and strain A-aggregate preparation, an aliquot of each was sonicated for 1 min in ice-cold buffer, containing PBS, Complete EDTA-free protease inhibitor cocktail (Roche Diagnostics) and 1% (v/v) NP-40 (for homogenate) or 2% (v/v) NP-40 (for strain A preparation). After sonication, the samples were centrifuged at 337,000 g for 3 h at 4 °C and the hSOD1 content in the resulting pellet was analyzed by western blotting. A human hemolysate, calibrated against pure hSOD1, was used as standard for estimations of hSOD1 content.
Western blotting
Western blots were performed on Any kD Criterion TGX precast gels (BioRad) as previously described [29]. The immunoreactivity was detected using ECL Select reagent (GE Healthcare), recorded on a ChemiDoc Touch Imaging System (BioRad), and analyzed using Image Lab software (BioRad). The primary antibody used for western blot experiments was a rabbit anti-hSOD1 antibody raised against a peptide corresponding to aa 24–39 (1.7 μg/ml). This antibody is human-specific and does not detect murine SOD1.
Stability tests of strain A aggregates
The hSOD1 aggregate preparation was vortexed for 2 min and then 10 µl aliquots were incubated with or without different concentrations of trypsin (10, 100 and 1000 µg/ml; Sigma-Aldrich); proteinase K (10, 50 and 250 µg/ml; Thermo Fisher Scientific); sodium dodecyl sulfate (SDS; 0.3, 1, 3 and 10 g/L; Sigma-Aldrich); or glycochenodeoxycholic acid (GCDCA; 8 mM; Sigma-Aldrich) in a total volume of 50 µl of PBS for different time intervals (0, 0.5, 1, 2, 4 and 6 h) at 37 °C using a shaker (IKA). GCDCA incubation was performed in the presence of the Complete EDTA-free protease inhibitor cocktail (Roche Diagnostics). Proteolysis with proteinase K was terminated by the addition of phenylmethylsulphonylflouride (PMSF; 20 and 100 mM; Sigma-Aldrich). After completed incubation, each sample reaction was immediately attenuated by the addition of 500 µl of water as a diluent, snap-frozen in liquid nitrogen and stored at − 80 °C. Frozen samples were thawed in a water bath at 25 °C for 2 min and then centrifuged at 25,000 g for 30 min at 4 °C and the supernatants were transferred to new tubes. The pellets were washed by suspension in 1 ml PBS and centrifuged again at 25,000 g for 30 min at 4 °C. The amount of hSOD1 in both supernatant and pellet was determined by western blotting.
Statistical analyses
Statistical analyses were performed using Prism version 6.00 (GraphPad). To test for statistical significance between two groups, Mann–Whitney U test was used. Alpha ≤ 0.05 was used as the cut-off for significance. All values are given as mean ± SD.
Results
Peripheral inoculations of transgenic homogenates do not induce premature ALS
We performed seed inoculations into the peritoneal cavity (i.p.) and quadriceps femoris muscle (i.m.) and compared with the effect of inoculations into the lumbar spinal cord (Fig. 1, Additional file 1: Table S1). The recipients were asymptomatic 100-day-old hSOD1G85R Tg mice, a well-characterized ALS mouse model, which has the advantage of a long symptom-free period followed by a late middle-age onset of aggregation and paresis [11, 23].
Peripheral inoculations of spinal cord homogenate from paralytic end-stage hSOD1G85R mice do not induce premature ALS in Tg mice. a–c Experimental overview: ~ 100-day-old pre-symptomatic hSOD1G85R Tg ALS-model mice were inoculated with spinal cord tissue homogenates from either end-stage paralytic hSOD1G85R Tg mice or control non-Tg C57BL/6 mice. We administrated the homogenates a into the spinal cord (spc) (single inoculation into the left ventral horn of the lumbar spinal cord, 1 µl), b i.p. (two inoculations into the peritoneal cavity, 150 µl each, 1 week apart), and c i.m. (single inoculation into the right quadriceps femoris muscle, 10 µl). d–f Kaplan–Meier plots show the survival of the spinal cord homogenate inoculated hSOD1G85R Tg mice. As a reference, the plots contain survival data for non-inoculated hSOD1G85R Tg mice. d Concentration-dependent induction of premature fatal motor neuron disease after intraspinal inoculation of the Tg homogenate. Survival of hSOD1G85R Tg mice after spinal cord inoculation of an undiluted 10% homogenate from end-stage hSOD1G85R Tg spinal cord and 1:3, 1:9 and 1:27 dilutions, compared to inoculation with control extract
As seeds, we used whole spinal cord homogenate preparations from end-stage hSOD1G85R Tg mice and non-Tg C57BL/6 control mice. The hSOD1G85R spinal cord homogenate, which contained ~ 1.7 ng/µl of strain A hSOD1 aggregates, was found to be highly active. Inoculations into the spinal cord using 1 µl of undiluted homogenate, as well as three- and ninefold dilutions, resulted in close to identical shortened survivals. Even a 27-fold diluted homogenate induced seeded pathogenic aggregation and premature motor neuron disease that resulted in a significant shortening of the lifespan of inoculated mice (Fig. 1d, Additional file 1: Table S1).
In contrast, i.p. inoculation of 300 µl of the homogenates, which is more than 8000 times the smallest effective dose used in spinal cord inoculations, did not induce premature paralysis in the hSOD1G85R Tg mice (Fig. 1e). Likewise, inoculations of 10 µl of the homogenate into the quadriceps femoris muscle failed to transmit seeding of premature ALS-like disease (Fig. 1f). There were no differences in survival between the mice that received i.p. or i.m. inoculations of hSOD1G85R Tg homogenates compared to recipients of non-Tg control spinal cord homogenates (Fig. 1e, f and Additional file 1: Table S1).
Intraperitoneal administration of transgenic homogenate does not induce hSOD1 aggregation in the CNS or peripheral tissues
Although SOD1 is ubiquitously expressed, end-stage paralytic hSOD1G85R Tg mice that accumulate a substantial hSOD1 aggregation in the spinal cord do not develop detectable hSOD1 aggregations in peripheral organs [10]. To determine whether the copious i.p. homogenate inoculations induced aggregation of the ubiquitously expressed hSOD1G85R in organs non-secluded by the blood–brain barrier, we analyzed hSOD1 aggregation in the liver and kidney, which both express higher levels of hSOD1G85R protein than spinal cord tissue [16]. Skeletal muscle and sciatic nerve were also analyzed (Fig. 2a, Additional file 1: Table S2). We found no evidence for transmission of hSOD1 aggregation in peripheral tissues. The reactivity of the antibody in liver homogenates was comparable to the background reactivity with non-Tg control, or SOD1-knockout spinal cord homogenates (Fig. 2a), and about 1000 times lower than end-stage hSOD1G85R Tg spinal cord homogenates [11, 23]. The reactivity was even lower in skeletal muscle, kidney and peripheral nerve. There were no significant differences between mice inoculated with homogenates from hSOD1G85R Tg and the non-Tg control mice (Fig. 2a, Additional file 1: Table S2).
Intraperitoneal administration of hSOD1 aggregate seeds does not induce hSOD1 aggregation in the CNS or peripheral tissues. a and b Plots depict hSOD1 aggregates detected in the CNS (lumbar, thoracic, and cervical spinal cord, brainstem, brain and cerebellum) and peripheral organs (liver, kidney, sciatic nerve and quadriceps femoris muscle) of hSOD1G85R Tg mice that were inoculated with hSOD1G85R Tg or control spinal cord homogenates into the peritoneal cavity. Amounts of hSOD1 aggregates in tissue homogenates were analyzed with a binary epitope mapping assay using the hSOD1 57–72 Ra-Ab with an end-stage hSOD1G93A spinal cord homogenate used as standard (set to 1). a Black line indicates the median value. The shaded area indicates the range of background reactivity to spinal cord homogenates from non-Tg and SOD1-knockout mouse controls (mean ± 2 SD) (n = 8) [10]. Note that the antibody likely would show different background reactivities to dot-blotted homogenates of other tissues from controls. b Distribution of hSOD1 aggregates along the neuraxis in individual end-stage Tg mice. The amount of filtertrapped aggregates from different segments was normalized against the levels from the lumbar spinal cord. Note the altered scale used to visualize reactivity to brain and cerebellum homogenates. The results for individual mice are presented in different colors to improve distinction. c Immunohistopathological analysis of tissue sections from the lumbar spinal cord and brainstem of end-stage i.p. inoculated hSOD1G85R Tg mice. Tissue sections from the lumbar spinal cord and brainstem were stained using the hSOD1 131–153 Ra-Ab (green), isolectin B4 (red) as a marker for endothelial cells and DAPI (blue). Aggregated hSOD1 was similarly distributed around blood vessels in the lumbar spinal cord and brainstem in the end-stage mice inoculated with either hSOD1G85R Tg spinal cord homogenate or control homogenate. Scale bar represents 50 μm
Even though there was no effect on the survival of the i.p. inoculated mice, we determined the distribution of hSOD1 aggregation along the neuraxis (Fig. 2b). We found no significant differences in distribution of hSOD1 aggregation in the neuraxis between mice inoculated with homogenates from hSOD1G85R Tg and non-Tg control mice. The highest levels of hSOD1 aggregates were detected in the cervical spinal cord in both i.p. inoculated groups (Fig. 2a, b, Additional file 1: Table S2).
It has previously been shown that peripheral administration of Aβ results in distribution of Aβ aggregation close to blood vessels in the brain which is different from Aβ aggregation induced by intracerebral inoculations [22]. To further explore the distribution of hSOD1 aggregation, we performed an immunohistopathological analysis of tissue sections from the lumbar spinal cord and brainstem of end-stage i.p. inoculated mice. Human SOD1 aggregates around the blood vessels in the ventral horn of the lumbar spinal cord and brainstem were similarly distributed in end-stage hSOD1G85R Tg mice i.p. inoculated with extracts from the hSOD1G85R Tg and control mice (Fig. 2c).
Stability of spinal cord-derived hSOD1G85R aggregates
We found that large amounts of peripherally administrated hSOD1 aggregates did not induce premature ALS in hSOD1G85R Tg mice or aggregation in the peripheral organs (Figs. 1, 2a and Additional file 1: Tables S1, S2). To explore the physical stability of the aggregates as a contributing factor to the lack of disease transmission, we examined the resistance of hSOD1 aggregates to proteases and detergents. This evaluation is also of importance for the risk assessment of handling potentially hazardous materials from patients or models of pathogenic aggregation.
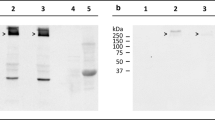
Natively folded wild-type SOD1 is an extremely stable protein that is resistant to high concentrations of guanidinium chloride, urea, proteases, and detergents, whereas mutant SOD1 variants with a structural loosening of the native fold and misfolded SOD1 exhibit variable sensitivities [3, 7, 9, 24, 26, 33, 37, 40, 41, 50, 55]. To assess the resistance of strain A hSOD1 aggregates, we exposed a spinal cord-derived hSOD1G85R aggregate preparation to different concentrations of proteases and detergents and incubated the samples for different time intervals at 37 °C. Samples were centrifuged at 25,000 g before hSOD1 content in both supernatant and insoluble pellet fractions were analyzed by western blotting (Fig. 3, Additional file 1: Figure S1).
Stability of spinal cord-derived hSOD1G85R aggregates. Human SOD1G85R aggregates were incubated either with or without a trypsin (10, 100 and 1000 µg/ml), b proteinase K (PK; 10, 50 and 250 µg/ml), c sodium dodecyl sulfate (SDS; 10 g/L) or d glycochenodeoxycholic acid (GCDCA; 8 mM) for different time intervals (0, 0.5, 1, 2, 4 and 6 h) at 37 °C. a–d Amounts of hSOD1, in both supernatant and insoluble fraction, were determined by western blotting. A human-specific SOD1 24–39 peptide antibody was used, and the reactivities was compared to a wild-type hSOD1 standard. Note that the hSOD1 standard has a lower electrophoretic mobility than the hSOD1G85R mutant
Both trypsin and proteinase K efficiently degraded the aggregates and no hSOD1 was detected in the insoluble fraction after 30 min of incubation (Fig. 3a, b). We did not detect hSOD1 in the soluble fraction at any time point. Thus, hSOD1 aggregates are highly sensitive to protease digestion.
Next, we determined the solubility of hSOD1G85R aggregates following incubation with different concentrations of sodium dodecyl sulfate (SDS) (Fig. 3c, Additional file 1: Figure S1). We found that the mutant SOD1 aggregates were completely dissolved by 10 g/L of SDS for 1 h at 37 °C and appeared in the supernatant fraction (Fig. 3c). Thus, strain A SOD1 aggregates were highly susceptible to SDS. However, SOD1 aggregates were resistant to treatment with a high concentration of another anionic detergent, glycochenodeoxycholic acid, which is the principal bile acid in the gut (Fig. 3d).
Discussion
Multiple studies have demonstrated that peripherally administrated disease-associated proteins linked to other neurodegenerative diseases have a high potency to transmit aggregation to the CNS. PD- and MSA-associated αSyn aggregates, and AD-associated Aβ- and Tau aggregates, can transmit and spread disease-associated aggregation into the CNS via several different routes [15, 17, 20,21,22, 31, 38, 39, 44, 46, 54, 59]. Nonetheless, both higher concentrations and longer incubation periods were required for peripherally delivered seeds compared to intracerebral inoculations [21, 22, 54]. In contrast, our results suggest that i.p. or i.m injections of large amounts of hSOD1 aggregates with prion-like properties do not transmit spreading pathogenic aggregation or premature fatal ALS-like disease in the hSOD1G85R Tg model, which is highly susceptible to seeding of template-directed aggregation. The hSOD1G85R spinal cord homogenate used as seeds was highly potent and even a 27-fold dilution readily induced ALS-like symptoms following spinal cord inoculations (Fig. 1d, Additional file 1: Table S1). Still, administration of 270 times more spinal cord homogenate via the i.m route or an 8000 times larger amount via the i.p. route did not induce premature fatal ALS-like disease (Fig. 1e, f, Additional file 1: Table S1). Moreover, there were no differences in distribution of aggregation pathology along the neuraxis in the hSOD1 aggregate inoculated, versus control inoculated mice. Thus, our current data suggest that the potential for transmission of SOD1-prion activity from the periphery to the CNS is very low.
SOD1 is ubiquitously expressed, and the levels of SOD1 in the liver and kidney are six and three times higher, respectively, than in the CNS [29, 30, 42]. We, therefore, investigated whether high amounts of peripherally administrated hSOD1 aggregates would accumulate and possibly induce aggregation in tissues outside the CNS. Our highly sensitive BEM assay showed that there were no significant differences in aggregate load when comparing liver, kidney, skeletal muscle, or sciatic nerves from end-stage Tg mice, inoculated i.p. with control or hSOD1 aggregate containing homogenates (Fig. 2a, Additional file 1: Table S2). This finding is in line with previous studies in AD where no Aβ deposition was found in peripheral organs of end-stage transgenic mice following i.p. inoculations [22]. However, the amyloid precursor protein, as well as Aβ-peptides, are generally only sparsely expressed outside of the CNS [2, 52].
We showed that strain A SOD1 aggregates in preparations from hSOD1G85R Tg mouse spinal cords are highly sensitive to degradation by proteases. These results corroborate with in cell-, and in vitro studies by Grad et al. which demonstrated that mutant SOD1 species, capable of transmitting misfolding to natively folded wild-type SOD1, are sensitive to protease treatment [26]. We further show that strain A SOD1 aggregates are efficiently degraded by exposure to SDS, which is a constituent of commonly used household and laboratory detergents (Fig. 3a–c). However, exposure to another anionic detergent, glycochenodeoxycholic acid, did not dissolve hSOD1 aggregates (Fig. 3d). Possibly the long flexible non-polar alkane chain in SDS interacts with and disrupts the hSOD1 fibril core more efficiently than the bulky partly polar steroid nucleus in the bile acid. Future studies of potential spreading via the gastro-intestinal route may shed light on possible uptake and spread via the enteric nervous system. However, although the aggregates were resistant to bile acid, the high sensitivity to proteases suggests that SOD1 aggregates should be efficiently degraded by the abundant proteases in the gastrointestinal tract, if ingested.
In contrast, like the highly infectious PrPSc, aggregated αSyn and Aβ are remarkably stable and resistant to inactivation. Moreover, both Aβ and αSyn aggregates extracted from the brain tissue of AD, PD, or MSA patients and Tg mice are highly robust and retain their seeding activity after exposure to both detergents and proteinase K [12, 35, 36, 45, 56,57,58,59]. Hence, inferior physical stability and low resistance to proteases may be contributing factors to why peripherally administrated hSOD1 aggregates did not transmit seeded aggregation to the CNS.
Conclusions
While inoculation of minute amounts of SOD1 aggregates with prion-like properties into the CNS readily induces spreading aggregation and premature fatal motor neuron disease, peripheral administration of large amounts did not induce disease in the hSOD1 Tg mice. Moreover, although SOD1 is ubiquitously expressed, no SOD1 aggregation was detected in peripheral tissues. These findings indicate that any potential risk for transmission of pathogenic SOD1 aggregation in exposed personnel handling samples from ALS patients or transgenic disease models should be considered low. However, precautionary safety measures should still be taken, especially while handling samples containing elevated concentrations of hSOD1 aggregates.
To this end, there is a need for guidelines for handling procedures and decontamination of laboratory material and surfaces, medical devices, and surgical instruments. Our results indicate that solutions of common commercially available detergents, containing > 1% SDS, efficiently degrade mutant hSOD1 aggregates.
Availability of data and material
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- ALS:
-
amyotrophic lateral sclerosis
- hSOD1:
-
human SOD1
- SOD1:
-
superoxide dismutase-1
References
Andersen PM, Al-Chalabi A (2011) Clinical genetics of amyotrophic lateral sclerosis: what do we really know? Nat Rev Neurol 7:603–615. https://doi.org/10.1038/nrneurol.2011.150
Arai H, Lee VM, Messinger ML, Greenberg BD, Lowery DE, Trojanowski JQ (1991) Expression patterns of beta-amyloid precursor protein (beta-APP) in neural and nonneural human tissues from Alzheimer’s disease and control subjects. Ann Neurol 30:686–693. https://doi.org/10.1002/ana.410300509
Ayers J, Lelie H, Workman A, Prudencio M, Brown H, Fromholt S, Valentine J, Whitelegge J, Borchelt D (2014) Distinctive features of the D101N and D101G variants of superoxide dismutase 1; two mutations that produce rapidly progressing motor neuron disease. J Neurochem 128:305–314. https://doi.org/10.1111/jnc.12451
Ayers JI, Borchelt DR (2020) Phenotypic diversity in ALS and the role of poly-conformational protein misfolding. Acta Neuropathol. https://doi.org/10.1007/s00401-020-02222-x
Ayers JI, Fromholt S, Koch M, DeBosier A, McMahon B, Xu G, Borchelt DR (2014) Experimental transmissibility of mutant SOD1 motor neuron disease. Acta Neuropathol 128:791–803. https://doi.org/10.1007/s00401-014-1342-7
Ayers JI, Fromholt SE, O’Neal VM, Diamond JH, Borchelt DR (2016) Prion-like propagation of mutant SOD1 misfolding and motor neuron disease spread along neuroanatomical pathways. Acta Neuropathol 131:103–114. https://doi.org/10.1007/s00401-015-1514-0
Ayers JI, McMahon B, Gill S, Lelie HL, Fromholt S, Brown H, Valentine JS, Whitelegge JP, Borchelt DR (2017) Relationship between mutant Cu/Zn superoxide dismutase 1 maturation and inclusion formation in cell models. J Neurochem 140:140–150. https://doi.org/10.1111/jnc.13864
Benkler C, O’Neil AL, Slepian S, Qian F, Weinreb PH, Rubin LL (2018) Aggregated SOD1 causes selective death of cultured human motor neurons. Sci Rep 8:16393. https://doi.org/10.1038/s41598-018-34759-z
Bergemalm D, Forsberg K, Srivastava V, Graffmo KS, Andersen PM, Brannstrom T, Wingsle G, Marklund SL (2010) Superoxide dismutase-1 and other proteins in inclusions from transgenic amyotrophic lateral sclerosis model mice. J Neurochem 114:408–418. https://doi.org/10.1111/j.1471-4159.2010.06753.x
Bergh J, Zetterström P, Andersen PM, Brännström T, Graffmo KS, Jonsson PA, Lang L, Danielsson J, Oliveberg M, Marklund SL (2015) Structural and kinetic analysis of protein-aggregate strains in vivo using binary epitope mapping. Proc Natl Acad Sci U S A 112:4489–4494. https://doi.org/10.1073/pnas.1419228112
Bidhendi EE, Bergh J, Zetterstrom P, Andersen PM, Marklund SL, Brannstrom T (2016) Two superoxide dismutase prion strains transmit amyotrophic lateral sclerosis-like disease. J Clin Invest 126:2249–2253. https://doi.org/10.1172/JCI84360
Bourdenx M, Nioche A, Dovero S, Arotcarena ML, Camus S, Porras G, Thiolat ML, Rougier NP, Prigent A, Aubert P et al (2020) Identification of distinct pathological signatures induced by patient-derived alpha-synuclein structures in nonhuman primates. Sci Adv 6:eaaz9165. https://doi.org/10.1126/sciadv.aaz9165
Braak H, Del Tredici K, Rub U, de Vos RA, Jansen Steur EN, Braak E (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24:197–211. https://doi.org/10.1016/s0197-4580(02)00065-9
Braak H, Rub U, Gai WP, Del Tredici K (2003) Idiopathic Parkinson’s disease: possible routes by which vulnerable neuronal types may be subject to neuroinvasion by an unknown pathogen. J Neural Transm (Vienna) 110:517–536. https://doi.org/10.1007/s00702-002-0808-2
Breid S, Bernis ME, Babila JT, Garza MC, Wille H, Tamgüney G (2016) Neuroinvasion of α-synuclein prionoids after intraperitoneal and intraglossal inoculation. J Virol 90:9182–9193. https://doi.org/10.1128/jvi.01399-16
Bruijn LI, Becher MW, Lee MK, Anderson KL, Jenkins NA, Copeland NG, Sisodia SS, Rothstein JD, Borchelt DR, Price DL et al (1997) ALS-linked SOD1 mutant G85R mediates damage to astrocytes and promotes rapidly progressive disease with SOD1-containing inclusions. Neuron 18:327–338. https://doi.org/10.1016/s0896-6273(00)80272-x
Burwinkel M, Lutzenberger M, Heppner FL, Schulz-Schaeffer W, Baier M (2018) Intravenous injection of beta-amyloid seeds promotes cerebral amyloid angiopathy (CAA). Acta Neuropathol Commun 6:23. https://doi.org/10.1186/s40478-018-0511-7
Charcot JM (1873) Lecons sur les maladies du système nervaux. 2nd series, collected by Bourneville. In: Charcot JM (1881) Lectures on the diseases of the nervous system, vol 2, series 2, Sigersen G (trans and ed). New Sydenham Society, London, pp 163–204
Chia R, Tattum MH, Jones S, Collinge J, Fisher EM, Jackson GS (2010) Superoxide dismutase 1 and tgSOD1 mouse spinal cord seed fibrils, suggesting a propagative cell death mechanism in amyotrophic lateral sclerosis. PLoS ONE 5:e10627. https://doi.org/10.1371/journal.pone.0010627
Clavaguera F, Bolmont T, Crowther RA, Abramowski D, Frank S, Probst A, Fraser G, Stalder AK, Beibel M, Staufenbiel M et al (2009) Transmission and spreading of tauopathy in transgenic mouse brain. Nat Cell Biol 11:909–913. https://doi.org/10.1038/ncb1901
Clavaguera F, Hench J, Lavenir I, Schweighauser G, Frank S, Goedert M, Tolnay M (2014) Peripheral administration of tau aggregates triggers intracerebral tauopathy in transgenic mice. Acta Neuropathol 127:299–301. https://doi.org/10.1007/s00401-013-1231-5
Eisele YS, Obermüller U, Heilbronner G, Baumann F, Kaeser SA, Wolburg H, Walker LC, Staufenbiel M, Heikenwalder M, Jucker M (2010) Peripherally applied Aβ-containing inoculates induce cerebral β-amyloidosis. Science 330:980–982. https://doi.org/10.1126/science.1194516
Ekhtiari Bidhendi E, Bergh J, Zetterström P, Forsberg K, Pakkenberg B, Andersen PM, Marklund SL, Brännström T (2018) Mutant superoxide dismutase aggregates from human spinal cord transmit amyotrophic lateral sclerosis. Acta Neuropathol. https://doi.org/10.1007/s00401-018-1915-y
Forman HJ, Fridovich I (1973) On the stability of bovine superoxide dismutase. The effects of metals. J Biol Chem 248:2645–2649. https://doi.org/10.1016/S0021-9258(19)44055-6
Forsberg K, Jonsson PA, Andersen PM, Bergemalm D, Graffmo KS, Hultdin M, Jacobsson J, Rosquist R, Marklund SL, Brännström T (2010) Novel antibodies reveal inclusions containing non-native SOD1 in sporadic ALS patients. PLoS ONE 5:e11552. https://doi.org/10.1371/journal.pone.0011552
Grad LI, Guest WC, Yanai A, Pokrishevsky E, O’Neill MA, Gibbs E, Semenchenko V, Yousefi M, Wishart DS, Plotkin SS et al (2011) Intermolecular transmission of superoxide dismutase 1 misfolding in living cells. Proc Natl Acad Sci U S A 108:16398–16403. https://doi.org/10.1073/pnas.1102645108
Grad LI, Yerbury JJ, Turner BJ, Guest WC, Pokrishevsky E, O’Neill MA, Yanai A, Silverman JM, Zeineddine R, Corcoran L et al (2014) Intercellular propagated misfolding of wild-type Cu/Zn superoxide dismutase occurs via exosome-dependent and -independent mechanisms. Proc Natl Acad Sci U S A 111:3620–3625. https://doi.org/10.1073/pnas.1312245111
Holmqvist S, Chutna O, Bousset L, Aldrin-Kirk P, Li W, Bjorklund T, Wang ZY, Roybon L, Melki R, Li JY (2014) Direct evidence of Parkinson pathology spread from the gastrointestinal tract to the brain in rats. Acta Neuropathol 128:805–820. https://doi.org/10.1007/s00401-014-1343-6
Jonsson PA, Ernhill K, Andersen PM, Bergemalm D, Brännström T, Gredal O, Nilsson P, Marklund SL (2004) Minute quantities of misfolded mutant superoxide dismutase-1 cause amyotrophic lateral sclerosis. Brain 127:73–88. https://doi.org/10.1093/brain/awh005
Jonsson PA, Graffmo KS, Andersen PM, Marklund SL, Brannstrom T (2009) Superoxide dismutase in amyotrophic lateral sclerosis patients homozygous for the D90A mutation. Neurobiol Dis 36:421–424. https://doi.org/10.1016/j.nbd.2009.08.006
Kane MD, Lipinski WJ, Callahan MJ, Bian F, Durham RA, Schwarz RD, Roher AE, Walker LC (2000) Evidence for seeding of β-amyloid by intracerebral infusion of alzheimer brain extracts in β-amyloid precursor protein-transgenic mice. J Neurosci 20:3606–3611. https://doi.org/10.1523/jneurosci.20-10-03606.2000
Kato S, Takikawa M, Nakashima K, Hirano A, Cleveland DW, Kusaka H, Shibata N, Kato M, Nakano I, Ohama E (2000) New consensus research on neuropathological aspects of familial amyotrophic lateral sclerosis with superoxide dismutase 1 (SOD1) gene mutations: inclusions containing SOD1 in neurons and astrocytes. Amyotroph Lateral Scler Other Motor Neuron Disord 1:163–184. https://doi.org/10.1080/14660820050515160
Kikuchi H, Almer G, Yamashita S, Guégan C, Nagai M, Xu Z, Sosunov AA, McKhann GM, Przedborski S (2006) Spinal cord endoplasmic reticulum stress associated with a microsomal accumulation of mutant superoxide dismutase-1 in an ALS model. Proc Natl Acad Sci U S A 103:6025–6030. https://doi.org/10.1073/pnas.0509227103
Kim S, Kwon SH, Kam TI, Panicker N, Karuppagounder SS, Lee S, Lee JH, Kim WR, Kook M, Foss CA et al (2019) Transneuronal propagation of pathologic alpha-synuclein from the gut to the brain models Parkinson’s disease. Neuron 103(627–641):e627. https://doi.org/10.1016/j.neuron.2019.05.035
Langer F, Eisele YS, Fritschi SK, Staufenbiel M, Walker LC, Jucker M (2011) Soluble Abeta seeds are potent inducers of cerebral beta-amyloid deposition. J Neurosci 31:14488–14495. https://doi.org/10.1523/JNEUROSCI.3088-11.2011
Lau A, So RWL, Lau HHC, Sang JC, Ruiz-Riquelme A, Fleck SC, Stuart E, Menon S, Visanji NP, Meisl G et al (2020) α-Synuclein strains target distinct brain regions and cell types. Nat Neurosci 23:21–31. https://doi.org/10.1038/s41593-019-0541-x
Lindberg MJ, Tibell L, Oliveberg M (2002) Common denominator of Cu/Zn superoxide dismutase mutants associated with amyotrophic lateral sclerosis: decreased stability of the apo state. Proc Natl Acad Sci U S A 99:16607–16612. https://doi.org/10.1073/pnas.262527099
Lohmann S, Bernis ME, Tachu BJ, Ziemski A, Grigoletto J, Tamguney G (2019) Oral and intravenous transmission of alpha-synuclein fibrils to mice. Acta Neuropathol 138:515–533. https://doi.org/10.1007/s00401-019-02037-5
Luk KC, Kehm VM, Zhang B, O’Brien P, Trojanowski JQ, Lee VMY (2012) Intracerebral inoculation of pathological α-synuclein initiates a rapidly progressive neurodegenerative α-synucleinopathy in mice. J Exp Med 209:975–986. https://doi.org/10.1084/jem.20112457
Lyons TJ, Gralla EB, Valentine JS (1999) Biological chemistry of copper-zinc superoxide dismutase and its link to amyotrophic lateral sclerosis. Met Ions Biol Syst 36:125–177. https://doi.org/10.1201/9780203747605-5
Malinowski DP, Fridovich I (1979) Subunit association and side-chain reactivities of bovine erythrocyte superoxide dismutase in denaturing solvents. Biochemistry 18:5055–5060. https://doi.org/10.1021/bi00590a005
Marklund SL (1984) Extracellular superoxide dismutase in human tissues and human cell lines. J Clin Invest 74:1398–1403. https://doi.org/10.1172/JCI111550
McAlary L, Plotkin SS, Yerbury JJ, Cashman NR (2019) Prion-like propagation of protein misfolding and aggregation in amyotrophic lateral sclerosis. Front Mol Neurosci 12:262. https://doi.org/10.3389/fnmol.2019.00262
Meyer-Luehmann M, Coomaraswamy J, Bolmont T, Kaeser S, Schaefer C, Kilger E, Neuenschwander A, Abramowski D, Frey P, Jaton AL et al (2006) Exogenous induction of cerebral ß-amyloidogenesis is governed by agent and host. Science 313:1781–1784. https://doi.org/10.1126/science.1131864
Miake H, Mizusawa H, Iwatsubo T, Hasegawa M (2002) Biochemical characterization of the core structure of alpha-synuclein filaments. J Biol Chem 277:19213–19219. https://doi.org/10.1074/jbc.M110551200
Mougenot A-L, Nicot S, Bencsik A, Morignat E, Verchère J, Lakhdar L, Legastelois S, Baron T (2012) Prion-like acceleration of a synucleinopathy in a transgenic mouse model. Neurobiol Aging 33:2225–2228. https://doi.org/10.1016/j.neurobiolaging.2011.06.022
Munch C, O’Brien J, Bertolotti A (2011) Prion-like propagation of mutant superoxide dismutase-1 misfolding in neuronal cells. Proc Natl Acad Sci U S A 108:3548–3553. https://doi.org/10.1073/pnas.1017275108
Peng C, Trojanowski JQ, Lee VM (2020) Protein transmission in neurodegenerative disease. Nat Rev Neurol 16:199–212. https://doi.org/10.1038/s41582-020-0333-7
Pokrishevsky E, Hong RH, Mackenzie IR, Cashman NR (2017) Spinal cord homogenates from SOD1 familial amyotrophic lateral sclerosis induce SOD1 aggregation in living cells. PLoS ONE 12:e0184384. https://doi.org/10.1371/journal.pone.0184384
Ratovitski T, Corson LB, Strain J, Wong P, Cleveland DW, Culotta VC, Borchelt DR (1999) Variation in the biochemical/biophysical properties of mutant superoxide dismutase 1 enzymes and the rate of disease progression in familial amyotrophic lateral sclerosis kindreds. Hum Mol Genet 8:1451–1460. https://doi.org/10.1093/hmg/8.8.1451
Rey NL, Petit GH, Bousset L, Melki R, Brundin P (2013) Transfer of human alpha-synuclein from the olfactory bulb to interconnected brain regions in mice. Acta Neuropathol 126:555–573. https://doi.org/10.1007/s00401-013-1160-3
Roher AE, Esh CL, Kokjohn TA, Castano EM, Van Vickle GD, Kalback WM, Patton RL, Luehrs DC, Daugs ID, Kuo YM et al (2009) Amyloid beta peptides in human plasma and tissues and their significance for Alzheimer’s disease. Alzheimers Dement 5:18–29. https://doi.org/10.1016/j.jalz.2008.10.004
Rosen DR, Siddique T, Patterson D, Figlewicz DA, Sapp P, Hentati A, Donaldson D, Goto J, O’Regan JP, Deng HX (1993) Mutations in Cu/Zn superoxide dismutase gene are associated with familial amyotrophic lateral sclerosis. Nature 362:59–62. https://doi.org/10.1038/362059a0
Sacino AN, Brooks M, Thomas MA, McKinney AB, Lee S, Regenhardt RW, McGarvey NH, Ayers JI, Notterpek L, Borchelt DR et al (2014) Intramuscular injection of α-synuclein induces CNS α-synuclein pathology and a rapid-onset motor phenotype in transgenic mice. Proc Natl Acad Sci 111:10732–10737. https://doi.org/10.1073/pnas.1321785111
Senoo Y, Katoh K, Nakai Y, Hashimoto Y, Bando K, Teramoto S (1988) Activity and stability of recombinant human superoxide dismutase in buffer solutions and hypothermic perfusates. Acta Med Okayama 42:169–174. https://doi.org/10.18926/AMO/31026
Stöhr J, Watts JC, Mensinger ZL, Oehler A, Grillo SK, DeArmond SJ, Prusiner SB, Giles K (2012) Purified and synthetic Alzheimer’s amyloid beta (Aβ) prions. Proc Natl Acad Sci 109:11025–11030. https://doi.org/10.1073/pnas.1206555109
Tarutani A, Arai T, Murayama S, Hisanaga SI, Hasegawa M (2018) Potent prion-like behaviors of pathogenic alpha-synuclein and evaluation of inactivation methods. Acta Neuropathol Commun 6:29. https://doi.org/10.1186/s40478-018-0532-2
Watts JC, Condello C, Stohr J, Oehler A, Lee J, DeArmond SJ, Lannfelt L, Ingelsson M, Giles K, Prusiner SB (2014) Serial propagation of distinct strains of Abeta prions from Alzheimer’s disease patients. Proc Natl Acad Sci U S A 111:10323–10328. https://doi.org/10.1073/pnas.1408900111
Woerman AL, Kazmi SA, Patel S, Freyman Y, Oehler A, Aoyagi A, Mordes DA, Halliday GM, Middleton LT, Gentleman SM et al (2018) MSA prions exhibit remarkable stability and resistance to inactivation. Acta Neuropathol 135:49–63. https://doi.org/10.1007/s00401-017-1762-2
Acknowledgements
We are grateful for skillful technical assistance provided by Ann-Charloth Nilsson, Agneta Öberg, Samaneh Shabani Åhrling, Berna Keskin, Helena Alstermark, Isabelle Sigfridsson, Eva Jonsson, Ulla-Stina Spetz and Karin Hjertkvist for skillful technical assistance.
Funding
Open access funding provided by Umea University. Funding for this project was provided by P.A., T.B., S.M., and I.K., through support by the Swedish Research Council (VR-MH 2012-3167; 2015-02804; 2017-03100; 2019-01707), the Knut and Alice Wallenberg Foundation (2012.0091; 2014.0305; 2020.0232), the Swedish Brain Foundation (Hjärnfonden 2015-0234; 2016-0303; 2018-0310; 2019-0320; 2020-0353), the Ulla-Carin Lindquist Foundation, the Bertil Hållsten Foundation, the Torsten and Ragnar Söderberg Foundation, Neuroförbundet, Västerbotten County Council, King Gustaf V and Queen Victoria’s Freemason’s Foundation; Kempe Foundations, the Research Foundation at the Medical Faculty of Umeå University, and the Research Foundation for Neurosciences at Umeå University, Sweden.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Animal surgery was performed by I.K., E.E.B., and U.N. Animal handling, tissue and material preparation, data collection was performed by I.K., M.M., E.E.B., and U.N. Data analysis were performed by I.K., E.E.B., M.M., S.M., T.B., P.A., and U.N. The first draft of the manuscript was written by I.K, S.M. and U.N. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Animal maintenance and handling protocols were approved by the Regional Ethics Committee for Animal Research (Umeå, Sweden).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Disease and survival data, SOD1 aggregate levels in tissue samples, and detergent resistance of hSOD1 aggregates.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Keskin, I., Ekhtiari Bidhendi, E., Marklund, M. et al. Peripheral administration of SOD1 aggregates does not transmit pathogenic aggregation to the CNS of SOD1 transgenic mice. acta neuropathol commun 9, 111 (2021). https://doi.org/10.1186/s40478-021-01211-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40478-021-01211-9






