Abstract
Background
This study was performed to evaluate the clinicopathologic characteristics of Lymph Node metastasis between investing layer of Cervical fascia and deep fascia of infrahyoid strap Muscles (LNCM) in papillary thyroid carcinoma (PTC).
Methods
Retrospective review of patients with PTC who underwent thyroidectomy and central compartment neck dissection (CND) from January 2016 to January 2018 was performed in two tertiary referral academic medical centers. A total of 2104 consecutive patients with PTC who underwent thyroidectomy and CND were included in the retrospective review. The LNCM was resected as a separate specimen by the surgeon and the clinicopathologic characteristics of the patients were recorded. Multivariate logistic regression analysis was performed to identify risk factors for LNCM metastasis.
Results
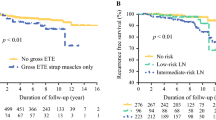
Of 2104 PTC patients, 451 patients (21.4%) had lymph nodes in the LNCM. Among them, 68 (15.1%) cases were confirmed to be positive in the LNCM. In total, the metastasis rate of LNCM in PTC patients was 3.2% (68/2104). Univariate analysis revealed that the metastasis of LNCM were more likely to have a primary site in the inferior pole, extrathyroidal extension (ETE), central cervical metastasis, level III and level IV metastasis. Multivariate analysis further showed tumor location in the inferior pole, ETE, level III and level IV metastasis conferred a significantly increased odds ratio for LNCM metastasis.
Conclusion
Attention should be paid to the lymph tissue in the LNCM for PTC patients, especially in presence of a primary site in the inferior pole, ETE, level III and level IV metastasis.
Similar content being viewed by others
Introduction
Patients with papillary thyroid carcinoma (PTC) have a favorable prognosis with central neck locoregional recurrence varying from 0 to 20% [1]. The goal of a prophylactic or therapeutic central compartment neck dissection (pCND or tCND) is to decrease the incidence of local recurrence by removing all lymphatic tissue within the levels VI and VII compartments, which are generally the first and the most commonly involved with metastasis [2]. For patients without evidence of lymph node metastasis on preoperative evaluation, the additive value of a pCND at the time of thyroidectomy is controversial. Some authors advocate pCND, considering high rate (24–88%) of occult metastatic nodal disease in cN0 PTC [1], while other authors consider that there is no high-level evidence in favor of pCND [3]. The performance of pCND is dependent on the weight given to the risks and benefits of pCND [4]. Considering the oncologic benefits of CND and the risks of a repeat neck operation, performing pCND is recommended to every patient in China [5, 6].
Although American Thyroid Association (ATA) guideline has defined the boundary of central neck compartment, there is also significant variability in terms of the extent of CND. In routine clinical practice, CND can range from sampling a few nodes in the paratracheal region to a complete clearance from left carotid artery to right carotid artery and down to and including the upper mediastinum [7]. Owing to the variant extent of CND, some central compartments are easily to be neglected. For thyroid carcinoma patients with specific clinicopathologic characteristics, incomplete lymph node dissection may result in increased recurrence, reoperation, and reoperation-associated complications [8]. Lymph Node between investing layer of Cervical fascia and deep fascia of infrahyoid strap Muscles (LNCM) has not been reported. The LNCM compartment is defined as follows: superiorly by the hyoid bone, laterally by the carotid arteries, anteriorly by the investing layer of cervical fascia, and posteriorly by the deep fascia of infrahyoid strap muscles. LNCM space includes suprasternal space and intra-infrahyoid strap muscle space.
Anatomically, LNCM is located anterior to the strap muscles. We consider that what is special about the concept of the LNCM is that it is belong to level VI but is an easily overlooked anatomical area by a strap musculature involving the sternohyoid and sternothyroid muscles during selective or modified neck dissection. Although the metastasis in LNCM was seldom, it did occur in some PTC patients with regional recurrence. As part of LCNM, suprasternal space metastasis for thyroid cancer were investigated in three studies [9,10,11]. Thus, we routinely detected the suprasternal space and intra-infrahyoid strap muscle space (Fig. 1). This study was performed to identify the clinicopathologic characteristics and indication for lymph node metastasis dissection in the LNCM.
Materials and methods
Patients
A retrospective review from the clinical and histopathology database of two tertiary referral academic medical centers, Tongji Hospital of Huazhong University of Science and Technology and Zhongnan Hospital of Wuhan University from January 2016 to January 2018 were conducted. In the institutions, preoperative examinations consisted of a thorough physical examination, neck ultrasound, a clinical evaluation of thyroid nodules and neck lymph nodes. Fine needle aspiration cytology (FNAC) were performed in patients who were suspected thyroid nodules or lymph node. With a pathological confirmation of PTC, all the patients received a thyroidectomy with CND. Accordingly, a pCND was performed for cN0 patients, and a therapeutic CND was performed for cN1 patients. The inclusion criteria for the patients were as follows: (1) the clinical history completely recorded; (2) the LNCM was resected as a separate specimen by the surgeon; (3) PTC patients who underwent thyroidectomy plus CND with or without lateral neck dissection. A total of 2104 consecutive PTC patients were enrolled. The medical ethic committee of Zhongnan Hospital of Wuhan University approved the procedure and informed written consent was obtained from all patients.
Surgical approach
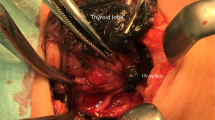
All the operations were performed by the same senior surgeon (Gaosong Wu), with the patients under general anesthesia. Thyroidectomy was performed with a standard technique of fine capsular en bloc dissection and resection, from inferior pole to superior pole [12,13,14,15,16]. Intraoperative neuromonitoring was employed for all of the thyroidectomies [17]. Superior parathyroid glands were identified and preserved in situ, inferior parathyroid glands were protected in situ or autotransplanted in the sternocleidomastoid muscle according to three certain types based on their blood supply and location [14, 18].
After the incision of the investing layer of cervical fascia, the interval between sternohyoid and sternothyroid muscles and the space anterior to the sternohyoid muscle above the clavicle and the sternum were detected. If there was fibrofatty tissue Instead of the en bloc removal of the entire central lymph nodes, the LNCM was resected as a separate specimen if occurred. The presence or absence of lymph node metastasis was defined according to postoperative pathological reports. While dissecting paratracheal lymph nodes, intraoperative neuromonitoring was employed to detect RLN from distally to proximally, minimizing morbidity from injury to RLN during compartment nodal dissection. LNCM and other compartment lymphatic tissue were processed for routine hematoxylin and eosine (H&E) separately. The pathologic results were independently determined by two qualified pathologists, without any prior knowledge of the patients’ clinical data.
Data collection and statistics analysis
To determine the relation between LNCM metastasis and clinicopathologic factors, such as age, sex, primary tumor site, lateral cervical lymph node metastasis, level VI metastasis, the chi-square test and Fisher’s exact test were used as appropriate. Multivariate logistic regression analysis was performed to identify risk factors for LNCM metastasis of PTC. P < 0.05 was considered statistically significant. All calculations were performed using SPSS 20.0 for windows. Post-thyroidectomy hypocalcemia lasting for more than 6 months was considered as permanent VCP. All patients were followed up every 3–6 months postoperatively.
Results
Patients detected with LNCM
After reviewing 2104 patients who underwent thyroidectomy plus CND with or without lateral neck dissection from January 2016 to January 2018, 451 patients (21.4%) were detected with LNCM and 1653 patients were absent of LNCM. The average tumor size of LNCM was 2.35 cm and the mean number of lymph nodes sampled from LNCM was 3.5, ranging from 0 to 9. Table 1 shows the comparison of clinicopathologic characteristics between the present LNCM group and the absent group. In univariate analysis, Hashimoto’s disease (p = 0.001), multifocality leisions (p < 0.001), the tumor located in inferior portion (p < 0.001), extrathyroidal extension (ETE) (p < 0.001), central cervical metastasis (p = 0.017), level III and level IV metastasis (p < 0.001) were significantly associated with high prevalence of LNCM.
Patients with metastatic LNCM
Among a total of 451 patients with LNCM, metastatic LNCM was found in 68 (15.1%) patients. Table 2 compares the clinicopathologic characteristics between the metastatic LNCM group and the nonmetastatic LNCM group. Three hundred eighty-three patients were confirmed free of LNCM metastasis, 249 (65.0%) of them with clinically negative node performed pCND and 134 of them with clinically positive performed tCND. All the patients in the metastatic LNCM group performed tCND. Lateral neck dissection was performed in 31 (81.6%) cases in the metastatic LNCM group and 185 (48.3%) cases in the nonmetastatic group, all lateral neck dissection was therapeutically performed. Univariate analysis was performed for the 68 patients with and 383 patients without metastatic LNCM. Age at diagnosis, gender and tumor size, coexistent thyroid disease, tumor focality, and level II metastasis were not correlated with LNCM metastasis. Univariate analysis identified tumor located in the inferior pole, central cervical metastasis, ETE, level III and level IV metastasis as significant predictors of LNCM metastasis in our study population. Multivariate analysis further showed that tumor location, ETE, level III and level IV metastasis conferred a significantly increased odds ratio for LNCM metastasis (Table 3).
Complications
The median follow-up time was 21.7 months (range 15–41). 67 (3.2%) of 2104 patients had voice changes, all of whom recovered within 1–6 months. Temporary vocal cord paralysis was confirmed in 46 patients (2.2%) by laryngoscope, and thirteen permanent hypocalcemia (0.4%) was observed after surgery.
Discussion
In order to achieve the best chance of cure and effective disease control, thoroughness of dissection has to be taken into account. We prospectively performed comprehensive CND for PTC patients who underwent thyroidectomy and CND. In addition, data were analyzed for 2104 PTC patients to investigate the clinicopathologic characteristics for LNCM metastasis. The occurrence rate of LNCM was 21.4% (451/2104), and 68 (15.1%) of the 451 patients harbored metastatic LNCM. In total, the positive rate of the LNCM was 3.2% (68/2104). In this study, multivariate analysis revealed that a primary site in the inferior pole, ETE, level III and level IV metastasis were of higher LNCM metastasis rate, which was consistent with the findings by the previous report of lymph node metastasis between sternocleidomastoid and sternohyoid muscle [9].
Several studies have emphasized the importance of similar compartment in neck dissection for thyroid carcinoma. Sun et al. pioneered the confirmation of the significant involvement of lymph node metastasis between sternocleidomastoid and sternohyoid muscle (LNSS) in lateral neck dissection [9], which anatomically classified as part of the space of Burns. They concluded that the positive rate of LNSS was 22.6% in clinically node-positive (cN+) PTC, which was correlated with a primary site in the inferior pole, the lateral nodal metastasis, level III and level IV nodal metastasis [9]. Then, Homma et al. [10] reported two cases of PTC patients with level III and IV lymph node metastases as well as metastasis in the suprasternal space. Yu et al. [11] investigated the clinical significance of the suprasternal space lymph node (SSLN) in pathological node-positive (pN+) PTC patients. They concluded that metastasis rate of SSLN was 20.7% and the high SSLN metastasis of PTC was correlated with primary cancer site in the inferior thyroid pole, strap muscle invasion, level IV metastasis and LNSS metastasis. In our experience, LNCM was rarely occurred in the central neck compartment (21.4%), and the positive LNCM in PTC patients was infrequent as well (3.2%). Notably, among the 2348 patients with pN+ PTC, the metastasis rate of LNCM was 4.1%, which was much lower than the metastasis incidence of SSLN (20.7%) described by Yu et al. [11] According to their results, one fifth patients with pN+ PTC were performed incomplete CND and remained metastatic lymph nodes.
The total number of lymph nodes in the central neck can range from 3 to 42 [19]. There is no consensus on the number of nodes removed or examined that would constitute an adequate dissection. Aimed to allow surgeons to more accurately report the extent of lymphadenectomy, we divide the central neck compartment into four subdivisions by deep fascia of infrahyoid strap muscles, pretracheal (visceral) fascial, and right RLN (Fig. 1). The proposed LNCM compartment is bounded superiorly by the hyoid bone, laterally by the carotid arteries, anteriorly by the investing layer of the cervical fascia, and posteriorly by the deep fascia of infrahyoid strap muscles, which is defined as Level VI 1st. In the current study, suprasternal space composed part of the LNCM (Fig. 1). Compared to SSLN reported by Yu et al. [11], LNCM encompasses lymph nodes in the suprasternal space and lymph nodes between sternohyoid and sternothyroid muscles (Figs. 1 and 2). LNCM can fall under the normal subdivisions of the central compartment. Subdivisions can actually record the extent of the CND, which is able to provide detailed information for the possible second operation.
Including LNCM as an anatomical part of the central neck allows for removal of previously unrecognized micrometastatic disease in 3.2% of PTC patients with the inferior portion lesions, ETE, level III and level IV metastasis. Dissection of the LNCM space is less invasive and easy to achieve and is not time-consuming. It is at the entrance of central neck compartment, which is easy to expose and has low risk of damaging RLN or parathyroid. With the application of intraoperative neuromonitoring and in situ preservation or auto-transplantation of parathyroid, the occurrence of vocal cord paralysis (2.2%) and permanent hypoparathyroidism (0.4%) in the current study were lower in this study [18, 20]. Therefore, in cases where LNCM space metastasis is suspected or preoperative ultrasound and CT suggests LNCM metastasis, greater attention should be paid to the nodal tissue in the LNCM space in thyroid carcinoma patients. These patients might benefit from a reduced risk of regional recurrence, central neck reoperative morbidity, and improved decision making in relation to the use of radioiodine ablation.
There are several limitations in the present study. The retrospective design is a limitation of the study. And this was two tertiary referral centers retrospective review and routine prophylactic nodal surgery was offered in China, however it is not standard elsewhere in the world, which is a major limitation. A prospective randomized trial with a long time follow-up period may help to further evaluate the clinical significance of LNCM in PTC patients.
Conclusions
In summary, additional dissection of nodes in the LNCM were accessible and might not increase morbidity. Therefore, attention should be paid to the lymph tissue between investing layer of cervical fascia and deep fascia of infrahyoid strap muscles for PTC patients, especially in presence of inferior portion lesions, ETE, level III and level IV metastasis.
Availability of data and materials
Not applicable.
References
Lang BH, Ng SH, Lau LL, Cowling BJ, Wong KP, Wan KY. A systematic review and meta-analysis of prophylactic central neck dissection on short-term locoregional recurrence in papillary thyroid carcinoma after total thyroidectomy. Thyroid. 2013;23(9):1087–98.
So YK, Seo MY, Son Y. Prophylactic central lymph node dissection for clinically node-negative papillary thyroid microcarcinoma: influence on serum thyroglobulin level, recurrence rate, and postoperative complications. Surgery. 2012;151(2):192–8.
Hughes DT, Rosen JE, Evans DB, Grubbs E, Wang TS, Solórzano CC. Prophylactic central compartment neck dissection in papillary thyroid Cancer and effect on Locoregional recurrence. Ann Surg Oncol. 2018;25(9):2526–34.
McHenry CR. Is prophylactic central compartment neck dissection indicated for clinically node-negative papillary thyroid Cancer: the answer is dependent on how the data are interpreted and the weight given to the risks and benefits. Ann Surg Oncol. 2018;25(11):3123–4.
Selberherr A, Riss P, Scheuba C, Niederle B. Prophylactic “first-step” central neck dissection (level 6) does not increase morbidity after (Total) thyroidectomy. Ann Surg Oncol. 2016;23(12):4016–22.
Hartl DM, Leboulleux S, Al Ghuzlan A, Baudin E, Chami L, Schlumberger M, et al. Optimization of staging of the neck with prophylactic central and lateral neck dissection for papillary thyroid carcinoma. Ann Surg. 2012;255(4):777–83.
McAlister ED, Goldstein DP, Rotstein LE. Redefining classification of central neck dissection in differentiated thyroid cancer. Head Neck. 2014;36(2):286–90.
Miller JE, Al-Attar NC, Brown OH, Shaughness GG, Rosculet NP, Avram AM, et al. Location and causation of residual lymph node metastasis after surgical treatment of regionally advanced differentiated thyroid Cancer. Thyroid. 2018;28(5):593–600.
Sun G, Wang Y, Zhu Y, Wang Y, Xu K, Wei W, et al. Lymph node metastasis between sternocleidomastoid and sternohyoid muscle in clinically node-positive papillary thyroid carcinoma. Head Neck. 2013;35(8):1168–70.
Homma A, Hatakeyama H, Mizumachi T, Furusawa J, Kano S, Sakashita T, et al. Lymph node metastasis in the suprasternal space from thyroid papillary cancer. Int Cancer Conf J. 2015;4(1):57–60.
Yu S, Ge J, Sun B, Wei Z, Lei S. Lymph node metastasis in suprasternal space in pathological node–positive papillary thyroid carcinoma. Eur J Surg Oncol. 2019;45:2086–9.
Wu G, Kong D. Thyroidectomy with Wu Gaosong's Procedure. VideoEndocrinologr. 2015. https://doi.org/10.1089/ve.2015.0050.
Wu G, Wang K. Intraoperative Neuromonitoring and Protection of the Superior Laryngeal Nerve with Wu Gaosong's Procedure. VideoEndocrinology. 2016. https://doi.org/10.1089/ve.2016.0070.
Wu G, Cui Q, Wang K. Carbon Nanoparticles for Identifying Lymph Nodes and Protecting Parathyroid Glands in Thyroid Lobectomy with Ipsilateral Central Compartment Lymph Nodes Dissection. VideoEndocrinology. 2016. https://doi.org/10.1089/ve.2016.0064.
Kong D, Cui Q, Gaosong W. A Novel Classification of Parathyroid Glands and Their Preservation in Thyroidectomy. VideoEndocrinology. 2017. https://doi.org/10.1089/ve.2017.0093.
Wang K, Wu G. Intraoperative Neuromonitoring in Selective Neck Dissection for Thyroid Cancer: SND (IIa Vb) with Wu Gaosong's Procedure. VideoEndocrinology. 2016. https://doi.org/10.1089/ve.2016.0082.
Yuan Q, Wu G, Hou J, Liao X, Liao Y, Chiang F. Correlation between electrophysiological changes and outcomes of vocal cord function in 1764 recurrent laryngeal nerves with visual integrity during thyroidectomy. Thyroid. 2020;30(5):739–45.
Cui Q, Li Z, Kong D, Wang K, Wu G. A prospective cohort study of novel functional types of parathyroid glands in thyroidectomy. Medicine. 2016;95(52):e5810.
Tavares MR, Cruz JA, Waisberg DR, Toledo SP, Takeda FR, Cernea CR, et al. Lymph node distribution in the central compartment of the neck: an anatomic study. Head Neck. 2014;36(10):1425–30.
Wang K, Cai H, Kong D, Cui Q, Zhang D, Wu G. The identification, preservation and classification of the external branch of the superior laryngeal nerve in thyroidectomy. World J Surg. 2017;41(10):2521–9.
Acknowledgements
The authors thank the studied patients for their willingness to cooperate with our study.
Funding
The authors have no support or funding to report.
Author information
Authors and Affiliations
Contributions
Gaosong Wu: Study concepts and design. Qianqian Yuan: Study design, manuscript preparation and editing. Jinxuan Hou: Data analysis and manuscript editing. Yiqin Liao: Data acquisition. Lewei Zheng: Manuscript preparation. Fang Lu: Data acquisition. Kun Wang: Quality control of data and algorithms. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was comprised of human participants and was approved by Medical Ethics Committee of Wuhan University Zhongnan Hospital. Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yuan, Q., Hou, J., Liao, Y. et al. Lymph node metastasis in suprasternal space and intra-infrahyoid strap muscle space from papillary thyroid carcinoma. J of Otolaryngol - Head & Neck Surg 49, 64 (2020). https://doi.org/10.1186/s40463-020-00461-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40463-020-00461-2