Abstract
Background
Erythropoietin-producing hepatocellular receptor A2 (EPHA2) is overexpressed on the cell surface in many cancers and predicts poor prognosis. DS-8895a is a humanized anti-EPHA2 IgG1 monoclonal antibody afucosylated to enhance antibody-dependent cellular cytotoxicity activity. We conducted a two-step, phase I, multicenter, open-label study to determine the safety, tolerability, and pharmacokinetics of DS-8895a in patients with advanced solid tumors.
Methods
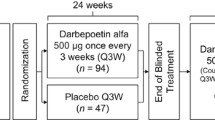
Step 1 was a dose escalation cohort in advanced solid tumor patients (six dose levels, 0.1–20 mg/kg) to determine Step 2 dosing. Step 2 was a dose expansion cohort in EPHA2-positive esophageal and gastric cancer patients. DS-8895a was intravenously administered every 2 weeks for the duration of the study, with a 28-day period to assess dose-limiting toxicity (DLT). Safety, pharmacokinetics, tumor response, and potential biomarkers were evaluated.
Results
Thirty-seven patients (Step 1: 22, Step 2: 15 [9: gastric cancer, 6: esophageal cancer]) were enrolled. Although one DLT (Grade 4 platelet count decreased) was observed in Step 1 (dose level 6, 20 mg/kg), the maximum tolerated dose was not reached; the highest dose (20 mg/kg) was used in Step 2. Of the 37 patients, 24 (64.9%) experienced drug-related adverse events (AEs) including three (8.1%) with Grade ≥ 3 AEs. Infusion-related reactions occurred in 19 patients (51.4%) but were manageable. All patients discontinued the study (evident disease progression, 33; AEs, 4). Maximum and trough serum DS-8895a concentrations increased dose-dependently. One gastric cancer patient achieved partial response and 13 patients achieved stable disease. Serum inflammatory cytokines transiently increased at completion of and 4 h after the start of DS-8895a administration. The proportion of CD16-positive natural killer (NK) cells (CD3−CD56+CD16+) decreased 4 h after the start of DS-8895a administration, and the ratio of CD3−CD56+CD137+ to CD3−CD56+CD16+ cells increased on day 3.
Conclusions
Twenty mg/kg DS-8895a infused intravenously every 2 weeks was generally safe and well tolerated in patients (n = 21) with advanced solid tumors. The exposure of DS-8895a seemed to increase dose-dependently and induce activated NK cells.
Trial registration
Phase 1 Study of DS-8895a in patients with advanced solid tumors (NCT02004717; 7 November 2013 to 2 February 2017); retrospectively registered on 9 December 2013.
Similar content being viewed by others
Background
Erythropoietin-producing hepatocellular receptor A2 (EPHA2) is a 130 kDa type-I transmembrane tyrosine kinase receptor, and EPH-related receptor tyrosine kinase ligand A1 (EPHRIN-A1) is the principle ligand for EPHA2 [1]. EPHA2/EPHRIN-A1 signaling contributes to the maintenance of epithelial cell homeostasis [1,2,3]. EPHA2 is expressed in several normal human tissues including skin, colon, bladder, kidney, lung, and stomach [4,5,6]. EPHA2 is overexpressed in many types of cancers [7,8,9,10,11,12,13], including 60% of gastric cancers [5] and nearly 50% of esophageal cancers [14]. It is widely reported that EPHA2 overexpression is correlated with poor prognosis for cancer patients [1, 4, 15,16,17]. Overexpressed EPHA2 promotes tumor cell proliferation, migration, invasion, and metastasis; and EPHA2 is activated through phosphorylation at serine-897 by AKT, p90 ribosomal S6 kinases, and protein kinase A, but not by EPHRIN-A1 [1,2,3, 18, 19]. In addition, Ras-Erk signaling, which is frequently activated in aggressive tumors, promotes expression of EPHA2 [20]. These features of EPHA2 make it an attractive target for cancer therapy.
Fragment crystallizable gamma receptor IIIa (FcγRIIIa, CD16) is highly expressed on natural killer (NK) cells. FcγRIIIa/CD16 binds to the Fc portion of IgG antibodies and induces the release of perforin and granzyme upon antibody/target cell binding, resulting in the death of target cells. This process is called antibody-dependent cellular cytotoxicity (ADCC). Afucosylation of the carbohydrate chain in IgG1 Fc substantially potentiates the binding affinity of the IgG1 portion to FcγRIIIa/CD16, which results in enhancement of ADCC [21, 22]. DS-8895a is a humanized anti-EPHA2 IgG1 monoclonal antibody (Additional file 1) that is afucosylated to enhance ADCC (POTELLIGENT®; BioWa Inc., Princeton, NJ, USA) and is expected to produce antitumor effects on EPHA2-overexpressing tumor cells through ADCC, as demonstrated in pre-clinical studies [23]. DS-8895a had neither complement-dependent cytotoxicity nor agonist activity against EPHA2 in vitro, and only weakly inhibited EPHRIN-A1-mediated phosphorylation of EPHA2 [23]. ADCC function is associated with antigen density [24], and overexpression of EPHA2 in solid tumors is considered a suitable and promising target for the ADCC-enhanced antibody DS-8895a.
The promising findings in pre-clinical studies led us to the clinical development of DS-8895a. We aimed to assess the safety, tolerability, and pharmacokinetics (PK) of DS-8895a administered in repeat doses to patients with advanced solid tumors and EPHA2-positive gastric or esophageal cancer in this first-in-human study of DS-8895a. Additionally, tumor response and potential biomarkers of tumor response were explored.
Methods
Study objectives
The primary objectives of this phase I, multicenter, open-label study, were to assess the safety, tolerability, and PK of repeated dosing of DS-8895a in patients with advanced solid tumours and to determine its optimal dose for subsequent clinical studies. The secondary objectives were to explore tumor response to DS-8895a treatment and the potential biomarkers related to DS-8895a.
Patients
Inclusion criteria were as follows: advanced solid tumors in Step 1, immunohistologically confirmed EPHA2-positive gastric or esophageal cancer in Step 2, refractory to standard treatment or no standard treatment available, age ≥ 20 years old, Eastern Cooperative Oncology Group performance status ≤1, sufficient organ function within 7 days prior to registration (Additional file 2), adverse drug reaction of prior anti-cancer therapy resolved to Grade 1 or Grade 2 and assessed as clinically eligible by investigators, certain treatment-free period from the final dose/treatment of any previous therapy to the date of registration (Additional file 3), life expectancy ≥3 months, and written informed consent to the study including agreement to biomarker analysis of archival and biopsied tumor samples. A tumor was considered EPHA2-positive if ≥25% of tumor cells had weak to moderate (score 2+) or strong (3+) EPHA2 staining immunohistochemically.
Major exclusion criteria were as follows: symptomatic or treatment-required brain metastasis within 6 months of registration; positive for hepatitis B surface antigen, hepatitis C virus, or human immunodeficiency virus antibody; active gastrointestinal hemorrhage requiring blood transfusions within 2 weeks of registration; treatment with other investigational drugs within 3 weeks of registration; lactating or pregnant mothers; and unwillingness to use adequate contraception during the study and for 6 months after the final DS-8895a administration.
Study design and treatment
The study protocol, amendments, and informed consent forms were approved by the Institutional Review Boards at each study site, and the study was conducted in accordance with the ethical principles of the Declaration of Helsinki and the International Council for Harmonisation guideline for Good Clinical Practice, and followed all other applicable regulatory requirements in Japan. Research using samples for genome/gene analysis was conducted in compliance with the Ethical Guidelines for Human Genome/Gene Analysis Research [25] and the Ethical Guideline for Clinical Research [26] as well as the above guidelines. This study was registered at clincaltrials.gov (NCT02004717).
This phase I study conducted in Japan comprised two steps: Step 1 as the dose escalation cohort in patients with advanced solid tumors, and Step 2 as the dose expansion cohort in patients with EPHA2-positive esophageal and gastric cancers (Additional file 4). In Step 1, the dose of DS-8895a was sequentially increased from Level 1 (0.1 mg/kg) to Level 6 (20 mg/kg), and intravenously administered over 2 h every 2 weeks with a 28-day period for assessment of dose-limiting toxicity (DLT). Each dose level consisted of three or six patients. If no DLT was observed in the first three patients, the dose level was escalated. If a DLT occurred in 1/3 patients, three patients were added to that dose level. If 2/6 or 3/6 patients experienced a DLT, dose escalation was discontinued and the dose level was judged as maximum tolerated dose (MTD). If the first 2/3 or 3/3 patients experienced a DLT, this dose level was also judged as MTD. In this case, further evaluation of the previous dose level was conducted, adding three or more patients. If the initial dose level was MTD, the study was stopped. Intra-patient dose escalation was not allowed. DLTs are defined in Additional file 5. Infusion-related reactions (IRRs) were excluded from the DLT evaluation.
The starting dose and administration schedule of DS-8895a were determined based on data from unpublished studies of intravenous administration of DS-8895a to cynomolgus monkeys (data on file, Daiichi Sankyo Co., Ltd.). Starting dose of 0.1 mg/kg was 260 times lower than the calculated human equivalent dose of no-observed-adverse-effect level obtained in these studies. An administration schedule of 2 weeks was chosen based on PK in cynomolgus monkeys and mice after a single intravenous or intraperitoneal administration of DS-8895a, respectively.
In Step 2, safety and PK were evaluated in up to 20 patients at the dose determined in Step 1. In both Steps 1 and 2, one cycle consisted of 4 weeks, and multiple cycles were allowed unless the discontinuation criteria for an individual patient were met.
Discontinuation criteria included evident disease progression, an adverse event (AE) making treatment continuation difficult, postponement of the study treatment > 4 weeks, deviation from the inclusion criteria after registration, patient’s request of withdrawal from study treatment, and investigator’s judgement.
Administration of DS-8895a was postponed if the patients did not meet the following criteria: ≥1000/μL neutrophil count, ≥75000/μL platelet count, non-hematological toxicity ≤ Grade 2 or improvement to the baseline level. Cancer treatment other than DS-8895a was prohibited from the day of obtaining informed consent to the day of follow-up assessment (30–45 days after final administration). Treatment for concomitant symptoms of cancer was allowed.
Safety and tolerability assessments
All AEs, clinical laboratory tests (hematology, blood chemistry, and urinalysis), vital signs (systolic and diastolic blood pressure, pulse rate, body temperature), and electrocardiogram (ECG) were assessed according to the National Cancer Institute – Common Terminology Criteria for Adverse Events, version 4.0 (Japanese version).
Initially, no premedication was used to prevent IRRs. However, after IRRs were observed at dose Levels 1 and 2, the protocol was amended to allow a premedication with antihistamines and antipyretics in Level 3, and a premedication with additional corticosteroids in Level 4 and thereafter. If no IRR occurred in previous DS-8895a administration, it could be omitted from subsequent doses.
Pharmacokinetic assessments
In Cycles 1 and 2, blood samples for PK analysis were collected immediately before and after DS-8895a administration; 4, 7, 24, and 72 h after starting administration on day 1; any time point on day 8; immediately before and after the next DS-8895a administration on day 15; and immediately before subsequent DS-8895a administration on day 29. From Cycle 3, blood samples were taken immediately before and after DS-8895a administration on day 1. Blood was also collected on the day of study discontinuation and on the 30th day after the final dose.
The serum concentrations of DS-8895a in Cycles 1 and 2 were used to calculate PK parameters (maximum serum concentration [Cmax], time to reach maximum serum concentration [Tmax], area under the concentration-time curve [AUClast] up to the last quantifiable time, AUC during dosing interval, AUC up to infinity [AUCinf], and terminal elimination half-life [T1/2]) using non-compartment models and the WinNonlin® software program (Certara, Princeton, USA). The lower limit of detection was set at 1000 ng/mL.
Pharmacodynamics assessments
Archival tumor samples were assessed for EPHA2, E-cadherin, human epidermal growth factor receptor 2 (HER2), and epidermal growth factor receptor (EGFR) expression (Steps 1 and 2). In Step 2, tumor biopsy samples were obtained before Cycle 1 and 2, and EPHA2, CD16, NKp46/NCRI, CD3, CD68, programmed death ligand-1 (PD-L1), E-cadherin, EGFR, and HER2 expression were assessed by immunohistochemistry. EPHA2 was detected using anti-human EPHA2 mouse monoclonal antibodies (clones 018 and 058, Daiichi Sankyo Co., Ltd.).
Blood and serum samples were collected to test circulating CD16-positive NK cells, NK activity, human leukocyte antigen (HLA)/killer cell immunoglobin-like receptor (KIR) mismatch, cytokines, and soluble EPHA2; a detailed blood sampling schedule is given in Additional file 6. HLA/KIR mismatch was assessed by typing these genes using previously described methods [27]. Circulating CD16-positive NK cells (CD3−CD56+CD16+, in Steps 1 and 2) and the ratio of CD3−CD56+ CD137+ cells to CD3−CD56+CD16+ cells (only in Step 2) in blood samples were analyzed using flow cytometry. Circulating soluble EPHA2 (only in Step 2) in serum was analyzed by sandwich ELISA. Cytokines (granulocyte-macrophage colony-stimulating factor, interferon [IFN]γ, interleukin [IL]-2, IL-3, IL-4, IL-5, IL-6, IL-7, IL-8, IL-10, IL-18, macrophage inflammatory protein [MIP]-1α, MIP-1β, monocyte chemotactic protein [MCP]-1, tumor necrosis factor [TNF]α, and TNFβ) in serum samples were analyzed by multiplex assays (in Steps 1 and 2). Natural cytotoxicity (NK cell activity) of NK cells was assessed by measuring the ability of the patient’s peripheral blood mononuclear cells to lyse K562 cells in vitro before Cycle 1 in Step 2.
Efficacy assessments
Tumor response to DS-8895a (best overall response, duration of best overall response, response rate, and disease control rate) was evaluated using the Response Evaluation Criteria in Solid Tumors, Version 1.1., using transverse section images of computerized tomography or magnetic resonance imaging scans. All baseline evaluations were performed using images taken within 21 days of registration. Tumor evaluation was performed every 6 weeks (± 1 week), or whenever investigators considered necessary.
Statistical analysis
The Guidelines for the Clinical Evaluation of Anti-cancer Drugs [28] were used to determine the sample size for Step 1. For Step 2, the sample size of up to 20 patients was estimated to be sufficient to evaluate safety and efficacy of DS-8895a.
Summary statistics were calculated for all categorical and quantitative data. The Kaplan–Meier method was used to estimate the survival distribution function for time-to-event analyses. Progression-free survival (PFS) was defined as the time from the first dose of DS-8895a to progression, relapse, or death from any cause, whichever occurred first. Pre-planned analytical populations consisted of an efficacy analysis set (patients who received at least one dose of the study drug and had at least one tumor assessment), an MTD evaluable set (patients who received at least one dose of the study drug in Step 1), a PK and pharmacodynamics analysis set (patients who received at least one dose of the study drug and from whom appropriate samples were obtained), and a safety analysis set (patients who received at least one dose of the study drug). SAS® System Release 9.2 software (SAS Institute Inc., Cary, NC) was used to perform statistical analysis.
Results
Patients
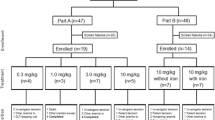
In total, 37 patients (22 in Step 1 and 15 in Step 2) were enrolled from 7 November 2013 to 2 February 2017. The number of patients (total [Step 1, Step 2]) in each pre-planned analysis set was as follows: safety analysis set (37 [22, 15]), efficacy analysis set (36 [21, 15]), MTD evaluable analysis set (21, [21, 0]), PK analysis set (36 [21, 15]), and pharmacodynamics analysis set (37 [21, 15]). One patient in Step 1 (Level 6) was excluded from the efficacy, PK, and MTD analysis sets because of unavailable efficacy/PK data or unevaluable DLT due to an IRR, which prevented the patient from completing the initial DS-8895a administration/finishing the trial.
Patient characteristics are shown in Table 1 and were similar between patients in Steps 1 and 2. Overall, 76% of patients were male with an average age of 67 years. EPHA2 expression was positive (2+ and 3+) in approximately one-third of patients tested in Step 1. In Step 2, 72 patients were screened and 27 were positive for EPHA2 expression; 15 of these 27 patients met the eligibility criteria and were included in Step 2. All 37 enrolled patients received the study treatment and eventually discontinued the study. Most patients discontinued because of evident disease progression (20 in Step 1 and 13 in Step 2), and all others discontinued because of adverse events (Additional file 7).
Safety
In Step 1, only one DLT was observed in one patient at Level 6 (20 mg/kg) as Grade 4 platelet count decreased. This was the only drug-related serious AE (SAE) and the only AE that required a dose delay in this study. MTD was not reached within the pre-planned doses. The dose for Step 2 was determined to be the highest dose from Step 1: 20 mg/kg.
AEs of any grade were observed in 21 (95.5%) and 15 (100%) patients in Steps 1 and 2, respectively (Table 2). The most common AEs were chills, decreased appetite, pyrexia, hypotension, nausea, anemia, hypoxia, constipation, dry skin, cancer pain, and vomiting. Drug-related AEs were observed in 14 patients (63.6%) in Step 1 and 10 patients (66.7%) in Step 2. The frequency of Grade 3 or 4 AEs was less than 10% in both Steps. IRRs related to DS-8895a occurred in 13 patients (59.1%) in Step 1 and 6 (40.0%) in Step 2. Among these patients, transient interruption of DS-8895a infusion was required in 10 patients. One patient in Level 3 (1.0 mg/kg) discontinued treatment because of a Grade 3 IRR, syncope. All other IRRs were Grade 1 or 2.
In Steps 1 and 2, there were nine AEs in four patients that led to discontinuation of study treatment. Of these, AEs of hypoesthesia, hypotension, peripheral coldness, nausea, and vomiting occurred in a single patient on the day of the first dose and immediately resolved after cessation of DS-8895a infusion. These five events were determined as being related to DS-8895a while the remaining four AEs were symptoms associated with disease progression. Therefore, a single patient of the 37 patients enrolled in the study (2.7%) discontinued treatment due to DS-8895a-related toxicity. Eleven SAEs occurred in seven patients including three deaths due to disease progression, and all were unrelated to DS-8895a except for the Grade 4 platelet decreased previously mentioned.
No clinically relevant differences from baseline or consistent trends were observed for other laboratory parameters (blood chemistry, hematology, and urology), vital signs, and ECG.
Pharmacokinetics
The mean maximum and trough serum concentrations of DS-8895a increased as the dose increased. PK parameters (Cmax and AUC) increased with increasing dose of DS-8895a (Table 3) for both Cycles 1 and 2. No apparent trends were observed for Tmax. The mean T1/2 of DS-8895a was 10–14 days in patients treated with 1.0 mg/kg or higher.
Efficacy
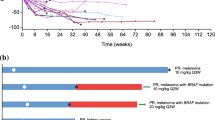
One gastric cancer patient in Step 2 achieved partial response (PR) (6.7%). Stable disease (SD) was observed in seven patients (33.3%; 95% confidence interval [CI]: 14.6, 57.0) of Step 1 and six patients (40.0%; 95% CI: 16.3, 67.7) of Step 2 (Table 4). Tumor shrinkage demonstrated no clear correlation with DS-8895a dose (Fig. 1) or EPHA2 expression (Table 4).
The median (range) duration of study treatment was 4.1 (0.14–31) weeks for 22 patients in Step 1 and 5.1 (2.1–22) weeks for 15 patients in Step 2. Time to response of the PR patient was 5.1 weeks, and duration of response was 18.4 weeks. In the patients with PR and SD, the median (range) duration of disease control was 11.7 (5.0–34) weeks. The median (range) PFS for Steps 1 and 2 were 5.9 (4.0–34.3) and 6.0 (3.3–23.4) weeks, respectively.
Pharmacodynamics
Serum levels of IFN-γ, IL-6, IL-7, IL-8, IL-10, MIP-1α, MIP-1β, MCP 1, and TNFα increased transiently at completion of DS-8895a administration and 4 h after the start of administration in Cycle 1. Elevated serum levels returned to baseline at 24 h. Soluble EPHA2 protein levels increased over time from baseline levels to day 8 of Cycle 2 in Step 2. Various levels of NK cell activity were observed in all patients before the first dose of DS-8895a in Step 2. Levels of circulating CD16-positive NK cells in the blood decreased 4 h after start of DS-8895a administration and remained low at 24 h in Cycle 1 of Step 1 (Fig. 2a) and Step 2 (Fig. 2b). The ratio of CD3−CD56+CD137+ cells to CD3−CD56+CD16+ cells increased on day 3 of Cycle 1 in Step 2, compared with baseline (Fig. 2c). There were no apparent relationships between the levels or changes of these biomarkers and tumor responses.
Mismatch of HLA/KIR polymorphism was detected in 20 patients (2 matched) in Step 1 and 14 patients (1 matched) in Step 2. All three patients with matched HLA/KIR had progressive disease. No association with tumor response could be determined because of the high incidence of HLA/KIR mismatch.
EPHA2, E-cadherin, HER2, and EGFR expression in retained tumor tissues; and EPHA2, CD16, NKp46/NCRI, CD3, CD68, PD-L1, E-cadherin, EGFR, and HER2 expression in paired biopsies obtained before Cycle 1 and 2 also demonstrated no apparent relationship between these expression levels or changes in expression levels and tumor responses. Pre- and post-treatment tumor tissues from the patient who achieved PR showed high expression of PD-L1 and E-cadherin at baseline, which decreased after DS-8895a administration. Also, in this patient, the number of infiltrated CD3-positive cells increased after DS-8895a treatment.
Discussion
Here we report the results of the first-in-human study of DS-8895a, an afucosylated, humanized anti-EPHA2 antibody. DS-8895a was safe and well tolerated up to 20 mg/kg in patients with advanced solid tumors (Step 1) and EPHA2-positive gastric or esophageal cancer (Step 2). Although one DLT event was observed at 20 mg/kg in Step 1, the MTD was not reached. The safety of a 20 mg/kg dose level was further confirmed in Step 2. IRRs were reported in about half of the patients but were generally manageable. One patient with EPHA2-positive gastric cancer achieved PR and 13 patients showed SD as best response. Serum DS-8895a concentrations and exposure increased in a dose-dependent manner, as expected. The mean T1/2 of DS-8895a was 10–14 days in patients treated with 1.0 mg/kg or higher and a stable concentration level was reached after long-term treatment, suggesting that administration every 2 weeks is a reasonable treatment schedule.
In this study, a decrease in CD16-positive NK cells and a transient increase in serum inflammatory cytokines were observed after DS-8895a administration, both of which indicate DS-8895a ADCC activity. Reduction of CD16-positive NK cells was maintained for 24 h, which was consistent with reports of other ADCC-enhanced antibodies [29, 30], suggesting a decrease in CD16-positive NK cells by ADCC. The increase in cytokines might also contribute to the occurrence of IRRs, which has been reported for other types of afucosylated monoclonal antibodies [31, 32].
We also observed that the ratio of CD3−CD56+CD137+ cells to CD3−CD56+CD16+ cells increased from baseline to Day 3 of Cycle 1. It has been reported that induction of ADCC activity upregulates CD137 expression on NK cells [33, 34], and increased CD137 expression on circulating NK cells has also been identified in patients treated with cetuximab, an anti-EGFR antibody with ADCC activity [35]. However, no apparent relationship was noted between this ratio and the best overall response in this study, given that we had only one patient who achieved PR. This suggests that enhanced ADCC activity by our afucosylated antibody was not sufficient to induce strong tumor shrinkage in solid tumors. The addition of an agonistic anti-CD137 monoclonal antibody with other antibodies, such as cetuximab or anti-CD20 antibody, has shown that activation of CD137 on NK cells enhanced their antitumor activity [34, 35]. A previous study suggested that the combination of HLA and KIR gene polymorphisms may affect ADCC activity [36]. However, as HLA/KIR mismatch was present in most patients in both Step 1 and Step 2, we were unable to assess a relationship between HLA/KIR mismatch and ADCC activity in our study.
Additional investigations of pharmacodynamic biomarkers conducted in Step 2 — including NK cell activity before the first study treatment and tumor expression levels of EPHA2, CD16, NKp46/NCRI, CD3, CD68, PD-L1, E-cadherin, EGFR, and HER2 — yielded no apparent trends of correlation between baseline level or on-treatment changes of these biomarkers and best overall response or disease control ratio. In Step 2, patients with EPHA2-positive gastric or esophageal cancer were enrolled. However, only one patient achieved a response, indicating that patient enrichment or drug activity may not have been sufficient. The patient who achieved PR had higher PD-L1 expression at baseline compared with the other patients and showed an increase in CD3-positive cells in Cycle 2 and decreased PD-L1 expression compared with baseline levels. Activated NK cells can stimulate the activity of other immune processes through their release of cytokines (such as IFNγ), providing a link to initiate subsequent immune responses to attack target tumors, which may have resulted in a tumor response in this patient. Preclinical studies using combination treatment of DS-8895a with other agents such as immune check point inhibitors are warranted.
As the first-in-human study of DS-8895a, this study has provided initial insights into the safety and potential activity of DS-8895a in patients and their response to the drug, providing a valuable knowledge base for future studies of afucosylated, humanized antibodies for the treatment of solid tumors. While clinical recommendations cannot be made based on this early-stage study, our phase I clinical study results warrant further studies involving a greater number of patients to determine the significance of our reported observations in relation to the treatment of EPHA2-positive solid tumors. Exploratory pharmacodynamic analysis suggested that immunological change was induced by our afucosylated monoclonal antibody with enhanced ADCC activity, which warrants further investigations to assess the efficacy of DS-8895a with different combinations of immune checkpoint inhibitors.
Limitations
One limitation of this study was that only Japanese patients were involved; therefore, the generalizability of the findings to other ethnic populations may be limited. Additionally, the PFS results from this single-arm study (without comparators) are considered exploratory.
Conclusions
This study showed that 20 mg/kg DS-8895a administered by infusion every 2 weeks was generally safe and well tolerated in patients with advanced solid tumors and that serum concentrations of DS-8895a increased in a dose-dependent manner. While no associations between biomarker changes and best overall response were observed, it will be of particular interest to further investigate changes in the ratio of CD137+ NK cells to NK cells after DS-8895a treatment to understand if an increased ratio may correlate with a positive treatment response or if the addition of agonistic anti-CD137 monoclonal antibodies may enhance the treatment response in patients with increased CD137 expression on NK cells.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article and its additional files.
Abbreviations
- ADCC:
-
Antibody-dependent cellular cytotoxicity
- AE:
-
Adverse event
- AUC:
-
Area under the concentration-time curve
- CI:
-
Confidence interval
- Cmax :
-
Maximum serum concentration
- DLT:
-
Dose-limiting toxicity
- ECG:
-
Electrocardiogram
- EGFR:
-
Epidermal growth factor receptor
- EPHA2:
-
Erythropoietin-producing hepatocellular receptor A2
- EPHRIN-A1:
-
EPH-related receptor tyrosine kinase ligand A1
- FcγRIIIa:
-
Fragment crystallizable gamma receptor IIIa
- HER2:
-
Human epidermal growth factor receptor 2
- HLA:
-
Human leukocyte antigen
- IFN:
-
Interferon
- IL:
-
Interleukin
- IRR:
-
Infusion-related reaction
- KIR:
-
Killer cell immunoglobin-like receptor
- MCP:
-
Monocyte chemotactic protein
- MIP:
-
Macrophage inflammatory protein
- MTD:
-
Maximum tolerated dose
- NK:
-
Natural killer
- PD-L1:
-
Programmed death ligand-1
- PFS:
-
Progression-free survival
- PK:
-
Pharmacokinetics
- PR:
-
Partial response
- SAE:
-
Serious adverse event
- SD:
-
Stable disease
- T1/2 :
-
Terminal elimination half-life
- Tmax :
-
Time to reach maximum serum concentration
- TNF:
-
Tumor necrosis factor
References
Tandon M, Vemula SV, Mittal SK. Emerging strategies for EphA2 receptor targeting for cancer therapeutics. Expert Opin Ther Targets. 2011;15:31–51.
Miao H, Wang B. EphA receptor signaling-complexity and emerging themes. Semin Cell Dev Biol. 2012;23:16–25.
Pasquale EB. Eph-ephrin bidirectional signaling in physiology and disease. Cell. 2008;133:38–52.
Hafner C, Becker B, Landthaler M, Vogt T. Expression profile of Eph receptors and ephrin ligands in human skin and downregulation of EphA1 in nonmelanoma skin cancer. Mod Pathol. 2006;19:1369–77.
Hou F, Yuan W, Huang J, et al. Overexpression of EphA2 correlates with epithelial–mesenchymal transition-related proteins in gastric cancer and their prognostic importance for postoperative patients. Med Oncol. 2012;29:2691–700.
Hafner C, Schmitz G, Meyer S, et al. Differential gene expression of Eph receptors and ephrins in benign human tissues and cancers. Clin Chem. 2004;50:490–9.
Saito T, Masuda N, Miyazaki T, et al. Expression of EphA2 and E-cadherin in colorectal cancer: correlation with cancer metastasis. Oncol Rep. 2004;11:605–11.
Abraham S, Knapp DW, Cheng L, et al. Expression of EphA2 and Ephrin A-1 in carcinoma of the urinary bladder. Clin Cancer Res. 2006;12:353–60.
Dunne PD, Dasgupta S, Blayney JK, et al. EphA2 expression is a key driver of migration and invasion and a poor prognostic marker in colorectal cancer. Clin Cancer Res. 2016;22:230–42.
Zelinski DP, Zantek ND, Stewart JC, Irizarry AR, Kinch MS. EphA2 overexpression causes tumorigenesis of mammary epithelial cells. Cancer Res. 2001;61:2301–6.
Easty DJ, Guthrie BA, Maung K, et al. Protein B61 as a new growth factor: expression of B61 and up-regulation of its receptor epithelial cell kinase during melanoma progression. Cancer Res. 1995;55:2528–32.
Wykosky J, Gibo DM, Stanton C, Debinski W. EphA2 as a novel molecular marker and target in glioblastoma multiforme. Mol Cancer Res. 2005;3:541–51.
Brannan JM, Dong W, Prudkin L, et al. Expression of the receptor tyrosine kinase EphA2 is increased in smokers and predicts poor survival in non-small cell lung cancer. Clin Cancer Res. 2009;15:4423–30.
Miyazaki T, Kato H, Fukuchi M, Nakajima M, Kuwano H. EphA2 overexpression correlates with poor prognosis in esophageal squamous cell carcinoma. Int J Cancer. 2003;103:657–63.
Biao-xue R, Xi-guang C, Shuan-ying Y, Wei L, Zong-juan M. EphA2-dependent molecular targeting therapy for malignant tumors. Curr Cancer Drug Targets. 2011;11:1082–97.
Merritt WM, Kamat AA, Hwang JY, et al. Clinical and biological impact of EphA2 overexpression and angiogenesis in endometrial cancer. Cancer Biol Ther. 2010;10:1306–14.
Yang P, Yuan W, He J, et al. Overexpression of EphA2, MMP-9, and MVD-CD34 in hepatocellular carcinoma: implications for tumor progression and prognosis. Hepatol Res. 2009;39:1169–77.
Neill T, Buraschi S, Goyal A, et al. EphA2 is a functional receptor for the growth factor progranulin. J Cell Biol. 2016;215:687–703.
Zhou Y, Sakurai H. Emerging and diverse functions of the EphA2 noncanonical pathway in cancer progression. Biol Pharm Bull. 2017;40:1616–24.
Macrae M, Neve RM, Rodriguez-Viciana P, et al. A conditional feedback loop regulates Ras activity through EphA2. Cancer Cell. 2005;8:111–8.
Kubota T, Niwa R, Satoh M, Akinaga S, Shitara K, Hanai N. Engineered therapeutic antibodies with improved effector functions. Cancer Sci. 2009;100:1566–72.
Lieberman J. The ABCs of granule-mediated cytotoxicity: new weapons in the arsenal. Nat Rev Immunol. 2003;3:361–70.
Hasegawa J, Sue M, Yamato M, et al. Novel anti-EPHA2 antibody, DS-8895a for cancer treatment. Cancer Biol Ther. 2016;17:1158–67.
Velders MP, van Rhijn CM, Oskam E, Fleuren GJ, Warnaar SO, Litvinov SV. The impact of antigen density and antibody affinity on antibody-dependent cellular cytotoxicity: relevance for immunotherapy of carcinomas. Br J Cancer. 1998;78:478–83.
Ministry of Education, Culture, Sports, Science and Technology, Ministry of Health, Labour and Welfare, and Ministry of Economy, Trade and Industry. Ethical Guidelines for Human Genome/Gene Analysis Research (issued on March 29, 2001, fully revised on December 28, 2004, partially revised on June 29, 2005, partially revised on December 1, 2008, and fully revised on February 8, 2013). http://www.lifescience.mext.go.jp/files/pdf/n796_00.pdf. Accessed 11 Dec 2018.
Ministry of Health, Labour and Welfare. Ethical Guideline for Clinical Research (issued on July 30, 2003, fully revised on December 28, 2004, and fully revised on July 31, 2008).
Delgado DC, Hank JA, Kolesar J, et al. Genotypes of NK cell KIR receptors, their ligands, and Fcγ receptors in the response of neuroblastoma patients to Hu14.18-IL2 immunotherapy. Cancer Res. 2010;70(23):9554–61.
Guidelines for the clinical evaluation of anti-cancer drugs, notification no. 1101001 of the evaluation and licensing division, pharmaceutical and food safety bureau (November 1, 2005).
Paz-Ares LG, Gomez-Roca C, Delord JP, et al. Phase I pharmacokinetic and pharmacodynamic dose-escalation study of RG7160 (GA201), the first glycoengineered monoclonal antibody against the epidermal growth factor receptor, in patients with advanced solid tumors. J Clin Oncol. 2011;29:3783–90.
Delord JP, Tabernero J, García-Carbonero R, et al. Open-label, multicenter expansion cohort to evaluate imgatuzumab in pre-treated patients with KRAS-mutant advanced colorectal carcinoma. Eur J Cancer. 2014;50:496–505.
Duvic M, Pinter-Brown LC, Foss FM, et al. Phase 1/2 study of mogamulizumab, a defucosylated anti-CCR4 antibody, in previously treated patients with cutaneous T-cell lymphoma. Blood. 2015;125:1883–9.
Shitara K, Ueha S, Shichino S, et al. First-in-human phase 1 study of IT1208, a defucosylated humanized anti-CD4 depleting antibody, in patients with advanced solid tumors. Society for Immunotherapy of Cancer 2018. Poster #P300 presented at SITC 2018. Washington, D.C; 2018.
Kohrt HE, Houot R, Weiskopf K, et al. Simulation of natural killer cells with a CD137-specific antibody enhances trastuzumab efficacy in xenotransplant models of breast cancer. J Clin Invest. 2012;122:1066–75.
Kohrt HE, Houot R, Goldstein MJ, et al. CD137 stimulation enhances the antilymphoma activity of anti-CD20 antibodies. Blood. 2011;117:2423–32.
Wang L, Wei Y, Fang W, et al. Cetuximab enhanced the cytotoxic activity of immune cells during treatment of colorectal cancer. Cell Physiol Biochem. 2017;44:1038–50.
Tarek N, Le Luduec JB, Gallagher MM, et al. Unlicensed NK cells target neuroblastoma following anti-GD2 antibody treatment. J Clin Invest. 2012;122:3260–70.
Acknowledgments
We thank Sarah Bubeck, PhD, of Edanz Medical Writing, for providing medical writing support, which was funded by Daiichi Sankyo Co., Ltd.
Funding
This study was funded by Daiichi Sankyo Co., Ltd. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Author information
Authors and Affiliations
Contributions
KS, IH and KN conceived the study design and supervised the study. KS, TS, SI, KY, KM, YK, TN (T Nishina) and TE collected and processed the data and conducted safety assessments. EK, KN, JH and TN (T Nakata) performed pharmacodynamic and pharmacokinetic assessments and interpreted the data. YK carried out statistical analyses. IH supervised the experiments and interpreted the findings. KS and HS drafted the initial manuscript. All authors contributed to the writing of the manuscript, design and implementation of the research and provided critical feedback on the manuscript. All authors approved the final manuscript before submission. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole and have given their approval for this version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol, amendments, informed consent forms, and information sheets were approved by the Institutional Review Boards at each study site. All patients provided written informed consent.
Consent for publication
Not applicable.
Competing interests
Kohei Shitara has received consultation fees from Astellas Pharma, Lilly, Bristol-Myers Squibb, Takeda Pharmaceutical, Pfizer, and Ono Pharmaceutical; honoraria from Novartis, Abbvie, and Yakult Honsha; and research funding from Dainippon Sumitomo Pharma, Eli Lilly, MSD, Daiichi Sankyo, Taiho Pharmaceutical, Chugai Pharmaceutical, and Ono Pharmaceutical.
Taroh Satoh has received consultation fees from Bayer Yakuhin, Ltd., Eli Lilly, Ono Pharmaceutical, Takara Bio, and Merck Serono; honoraria from Chugai Pharmaceutical, Merck Serono, Bristol-Myers Squibb, Takeda Pharmaceutical, Yakult Honsha, Eli Lilly, Bayer Yakuhin, Ono Pharmaceutical, Merck, and Astellas Pharma; and research funding from Yakult Honsha, Chugai Pharmaceutical, Ono Pharmaceutical, Sanofi, Eli Lilly, Daiichi Sankyo, Merck, Merck Serono, Gilead Sciences, and Dainippon Sumitomo Pharma.
Satoru Iwasa has received honoraria from Taiho Pharmaceutical, Lilly Japan and Chugai Pharma; and research funding from Daiichi Sankyo, Chugai Pharma, Bristol-Myers Squibb, Lilly Japan, Eisai, Novartis, Merck Serono, Otsuka and Bayer.
Kensei Yamaguchi has received consultation fees from Bristol-Myers Squibb Japan and Daiichi Sankyo; speaker’s bureau funds from Chugai Pharma, Merck Serono, Bristol-Myers Squibb Japan, Takeda, Taiho Pharmaceutical, Lilly, Yakult Honsha, Ono Pharmaceutical and Sanofi; and research funding from MSD Oncology, Ono Pharmaceutical, Dainippon Sumitomo Pharma, Taiho Pharmaceutical, Daiichi Sankyo, Lilly, Gilead Sciences and Yakult Honsha.
Kei Muro has received honoraria from Chugai Pharma, Merck Serono, Takeda, Taiho Pharmaceutical, Lilly, Yakult Honsha, Ono Pharmaceutical and Bayer; and research funding from Ono Pharmaceutical, MSD, Daiichi Sankyo, Shionogi, Kyowa Hakko Kirin, Gilead Sciences, Merck Serono, Pfizer and Sanofi.
Yoshito Komatsu has received speaker’s bureau funds from Taiho Pharmaceutical, Lilly, Chugai Pharma, Merck Serono, Novartis, Pfizer, Bayer, Ono Pharmaceutical, Yakult Honsha, Takeda, Sanofi, Bristol-Myers Squibb Japan, Daiichi Sankyo, TOWA and Nipro Corporation; honoraria from Novartis, Pfizer and Bayer; and research funding from Taiho Pharmaceutical, Lilly, MSD, Ono Pharmaceutical, Novartis, Bayer, Chugai Pharma, Yakult, Takeda, Dainippon Sumitomo Pharma, Boehringer Ingelheim, Sysmex, Sanofi, Astellas Pharma and Eisai.
Tomohiro Nishina has received honoraria from Taiho Pharmaceutical, Chugai Pharma, Lilly, Merck Serono and Takeda; and research funding from Taiho Pharmaceutical, Chugai Pharma, Dainippon Sumitomo Pharma, Lilly Japan, Merck Serono, MSD, Daiichi Sankyo, and Ono Pharmaceutical.
Taito Esaki has received consultation fees from Chugai Pharma; speakers’ bureau funds from Taiho Pharmaceutical, Bristol-Myers Squibb Japan, Lilly, Eisai, Daiichi Sankyo, Merck Serono, Chugai Pharma, Ono Pharmaceutical and Takeda; honoraria from Lilly and Kyowa Hakko Kirin; and research funding from Daiichi Sankyo, Merck Serono, Taiho Pharmaceutical, MSD, Novartis, Dainippon Sumitomo Pharma and Ono Pharmaceutical.
Jun Hasegawa, Yasuyuki Kakurai, Emi Kamiyama, Tomoko Nakata, Kota Nakamura and Hayato Sakaki are employees of Daiichi Sankyo.
Ichinosuke Hyodo has received honoraria from Chugai Pharma, Taiho Pharmaceutical, Daiichi Sankyo, Lilly, Ono Pharmaceutical and Bristol-Myers Squibb; and research funding from Bristol-Myers Squibb Japan, Chugai Pharma, Kyowa Hakko Kirin, Takeda, Merck Serono, Yakult Honsha, Taiho Pharmaceutical, Sanofi, Daiichi Sankyo and Ono Pharmaceutical.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Schematic of the cytotoxic effect of DS-8895a. Abbreviations: EPHA2, erythropoietin-producing hepatocellular receptor A2; FcγRIIIa, Fragment crystallizable gamma receptor IIIa; NK, natural killer. (TIF 785 kb)
Additional file 2:
Selection criteria: sufficient organ function (DOCX 13 kb)
Additional file 3:
Description of treatment-free period (DOCX 14 kb)
Additional file 4:
Overall study design. Abbreviations: PK, pharmacokinetics; Q2W, every 2 weeks. (TIF 542 kb)
Additional file 5:
Definition of dose-limiting toxicities (DOCX 15 kb)
Additional file 6:
Schedule of blood/serum collection (DOCX 16 kb)
Additional file 7:
Disposition of patients. †One patient was excluded from the efficacy analysis set because no efficacy data were available. ‡One patient was excluded from the PK analysis set because no PK data were available. Abbreviation: PK, pharmacokinetics. (TIF 224 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Shitara, K., Satoh, T., Iwasa, S. et al. Safety, tolerability, pharmacokinetics, and pharmacodynamics of the afucosylated, humanized anti-EPHA2 antibody DS-8895a: a first-in-human phase I dose escalation and dose expansion study in patients with advanced solid tumors. j. immunotherapy cancer 7, 219 (2019). https://doi.org/10.1186/s40425-019-0679-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40425-019-0679-9