Abstract
Background
Asthma is one of the most common chronic respiratory conditions worldwide. Asthma-related economic burden has been reported in Latin America, but knowledge about its economic impact to the Colombian health care system and the influence of disease severity is lacking. This study estimated direct medical costs and health care resource utilization (HCRU) in patients with asthma according to severity in Colombia.
Methods
This study identified all-age patients who had at least one medical event linked to an asthma diagnosis (CIE-10: J45-J46) between 2004 and 2014. Patients were selected if they had a continuous enrollment and uninterrupted insurance coverage between January 1–2015 and December 31–2015 and were categorized into 4 different severity levels using a modified algorithm based on Leidy criteria. Healthcare utilization and costs were estimated in a 1-year period after the identification period. A Generalized Linear Model (GLM) with gamma distribution and log link was used to analyze costs adjusting for patient demographics.
Results
A total of 20,410 patients were included: 69.5% had mild intermittent, 18.0% mild persistent, 6.9% moderate persistent and 5.5% severe persistent asthma; with mean costs (SD) of $67 (134), $482 (1506), $1061 (1983), $2235 (3426) respectively (p < 0.001). The mean total direct cost was estimated at $331 (1278) per patient. Medication and hospitalization had the higher proportion in total costs (46% and 31% respectively). General physician visits was the most used service (57.2%) and short-acting β-2 agonists the most used medication (24%).
Conclusions
Health services utilization and direct costs of asthma were highly related to disease severity. Nationwide health policies aimed at the effective control of asthma are necessary and would play an important role in reducing the associated economic impact.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
As the most prevalent chronic respiratory disease worldwide, asthma contributes enormously to the total economic burden of non-communicable diseases [1,2,3]. This chronic and difficult-to-treat condition demands high expenditures in medical care services and impairs quality of life and productivity of patients [4, 5]. Recent estimations indicated that asthma caused 1.1% of global disability-adjusted life years (DALYs). From 1990 to 2015, its global prevalence increased by 12.6%, affecting 358.2 million all-age individuals worldwide [6,7,8].
Annual asthma-related direct costs are highly variable among countries. Estimations have been reported from less than US$150 per person-year in Abu Dhabi, United Arab Emirates to more than US$3000 per person-year in the United States (US) [9]. Disease severity is considered a major factor influencing health care resource utilication (HCRU) and related costs. Even though severe asthma is not common, its contribution to total costs is high [10,11,12,13].
Despite some pharmacological advances and the divulgation of guidelines for diagnosis, treatment and prevention, asthma is still a global difficult-to-treat condition and the implementation of strategies for achieving better outcomes remains heterogeneous, especially in developing countries [14,15,16,17,18]. In Latin America, as in other developing regions in the world, several barriers exist to achieve asthma control [19,20,21]. Disease mechanisms are poorly understood and co-existence of infectious and chronic diseases represents major challenges to health care systems [22,23,24,25]. As a result, high rates of uncontrolled and severe asthma have been reported and asthma remains neglected as a public health priority [26,27,28].
Colombia is a predominantly urban country (76%) of over 48 million inhabitants where chronic diseases are emerging as public health concerns [29]. In 1993, the Colombian Congress sanctioned the Law 100, which replaced the former National Health System (NHS) and introduced a healthcare system known as “Sistema General de Seguridad Social en Salud (SGSSS) (The General System of Social Security in Health)”, an obligatory national health insurance system based on regulated competition. Formally employed individuals, retirees or self-employed individuals earning at least the minimum wage must contribute to SGSSS through a mandatory payroll deduction (contributive regime) and individuals from the low-income population (near 23 million) are affiliated through governmental subsidies (subsidized regime). Currently, almost of 95% of the population is covered by SGSSS and both have equal access to healthcare services.
A nationwide study conducted in Colombia estimated a prevalence rate of 12% (95% CI: 10.5–13.7) for current asthma symptoms suggesting an increase compared to a 10% rate (95% CI: 9.7–11.1) reported 10 years earlier. Furthermore, 43% of subjects with reported asthma symptoms also informed requiring an emergency department (ED) visit or hospitalization in the past year [30, 31]. Nevertheless, little is known about the economic burden of asthma in Colombia and cost of illness studies assessing the influence of disease severity in direct costs and HCRU have not been conducted.
There are no studies in Latin America assessing asthma-related costs through claim-based approaches and micro-costing methodologies in spite of their usefulness as inputs for economic evaluations. Thus, current estimations are associated with uncertainty as high variability in study designs exists. Determining the costs of asthma will help to identify the main expenditure predictors, to analyze if current spending is allocated effectively and to suggest how it should be invested in the future. Assessing the direct medical costs is a valuable input in the design, monitoring and evaluation of health policies and strategies for disease management. In addition, targeting strategies to approach specific groups of the population with asthma according to cost predictors, may contribute to reduce the resulting economic burden and therefore to improve efficiency in the resource allocation process. In this study, we sought to estimate the HCRU and direct medical costs of asthma for different severity stages from the Colombian health care system perspective.
Methods
Data source
The primary data source for cost estimation was a claims database from a subsidized regime insurance company of national coverage (with almost two million affiliates) that provides health services to the poorest populations that are not affiliated to the health system through formal employment. Person-level information on demographics, HCRU and total expenditures were available for the study.
Study design
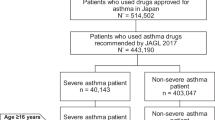
This was a retrospective analysis of a claims database to estimate the utilization of medical services and asthma-related medication within an open cohort of asthmatic patients. We used a stepwise process to identify and select patients for inclusion as well as for disease severity assessment. Patients were identified from January 1, 2004 through December 31, 2014. An “asthma patient” was defined as any occurrence of an International Classification of Diseases, Tenth Revision (ICD-10) code J45 and/or J46 linked to a medical event such as outpatient visit, ED visit or hospitalization during the identification period. Then, to select the most accurate sample among the eligible patients, an individual must have fulfilled a continuous enrollment and uninterrupted health insurance coverage for at least 12 months during the cost analysis period (from January 1, 2015 through December 31, 2015) (Fig. 1) to be included in the study. In addition, to ensure quality of information, a physician of the research staff revised image/laboratory procedures and prescription data from selected cases to filter and include only those derived from asthma management and not with other unrelated co-morbidity.
Disease severity classification
Asthma severity classification was mainly based on Leidy criteria [32, 33]. This algorithm has been used previously in other administrative claims studies [34,35,36] and is based on the number of β2-agonist inhalers and oral corticosteroid (OCS) fills used during the year of cost analysis. The number of exacerbations was also included in the algorithm of classification for minimizing the likelihood of underassessment of severity. An exacerbation was defined as an ED visit or hospitalization within the cost analysis period.
Mild intermittent asthma was defined as one (or less) SABA fill and zero oral OCS fills per year and zero exacerbations. Mild persistent asthma was defined by four to six SABA fills and zero oral OCS fills per year, or two to three SABA fills and less than two OCS fills per year, or one exacerbation. Furthermore, one (or less) SABA fill and one oral OCS fills per year can also account for mild persistent asthma. Moderate persistent asthma included more than six SABA fills and less than two OCS fills per year, or four to six SABA fills and one to two OCS fills per year or 2–3 exacerbations. Patients with severe persistent asthma required to have more than six SABA fills per year, and the number of OCS fills per year, was greater than or equal to two or 4 or more exacerbations. Moreover, zero to six SABA fills and three or more SABA fills per year also constitute severe persistent asthma [33].
Patient information
Demographic (i.e., age, sex and place of residence) and socioeconomic characteristics (the category in the information system used in Colombia to identify potential beneficiaries of public spending – SISBEN) [37] of the final sample were stratified and compared among asthma severity categories. Associated comorbidities were identified on the claims database as the additional occurrence of their respective ICD-10 codes on the sample of asthmatic subjects.
Direct costs
Costs derived from medical services: hospitalizations, ED visits, outpatient visits, specialized care and other ambulatory services (i.e., domiciliary care, laboratory/image procedures and ambulances) as well as prescriptions of controller or rescue medications (see Additional file 1) were obtained directly from the billing database of the health insurance company. The cost per patient was calculated in each type of health care resource (or medication category) as the sum of the cost of the respective events reported during 2015. Mean costs were estimated among all subjects belonging to each disease category or among only those who used the medical service or received the prescription. The total cost per patient including all expended medical services and all prescriptions (or both) was also calculated to further estimate mean total costs. To allow for cost comparability, 2015 purchasing power parity (PPP) exchange rate from the World Bank International Comparison Program Database was used to convert costs estimations to 2015 International Dollars (I$). Total expenditures were divided by the PPP exchange rate ($1203.9 COP) [38]. Purchasing Power Parity adjustment allows a comparable analysis of economic data from different countries by expressing expenditures in a common price index (i.e., based in US) due to potential differences in purchasing powers between countries despite conversion using market exchange rates. A PPP exchange rate is the number of units of a country currency required to purchase the same amounts of goods and services in the domestic market as a US dollar would buy in the US. An International Dollar is therefore a hypothetical currency that has the same purchasing power as the US Dollar has in the US for similar goods and services [39,40,41].
Sensitivity analysis
We analyzed the impact of other respiratory co-morbidities and allergic diseases on asthma-related direct costs by performing a sensitivity analysis. All patients with any of the selected co-morbidities (i.e., rhinitis, atopic eczema, acute bronchitis, pulmonary emphysema and COPD) were excluded and total costs compared with the entire database. Sub-group analyses in age-categories with more potential of misclassification with other respiratory diseases were also done.
Statistical analysis
Data analysis was performed in Stata 14 software (StataCorp LP Lakeway, TX, US) and R statistical software version 3.3.4. Descriptive information about clinical and sociodemographic data of patients involved in the study is shown in Table 1. Differences between proportions were analyzed by Pearson chi-squared test. The Cochran-Armitage test was used for trend association analysis.
Costs were reported both as their arithmetic mean with standard deviation (SD) and median with interquartile range (IQR). The Shapiro-Wilk test was used to test for normal distribution of the cost data and the Levene test to evaluate homogeneity of variances. The International Society of Pharmacoeconomics and Outcomes Research – ISPOR good research practice guidelines were used for cost data analysis [42]. As the sample/arithmetic mean cost is considered to be the most appropriate and informative measure for health care policy-makers, the Welch analysis of variance- ANOVA test and the Games-Howell test for post hoc analyses were used for analyzing mean costs among disease severity categories despite unequal variances and a non-normal distribution were found in the cost data [43,44,45]. In addition, as recommended by Mihaylova et al. [46] and highlighted by Gray et al. [47], “simple methods” (assuming normal distributions for costs) should be preferred when sample sizes are sufficiently large for the central limit theorem to exert itself.
To identify factors influencing asthma-related costs in the study population, expenditures were also analyzed in a one-part generalized linear model (GLM) with gamma distribution, log-link function and robust standard errors. GLM models with gamma distribution are considered to be the most suitable option for cost data analysis due to the advantage of analyzing both the mean and variance functions on the original dollar scale and addressing the frequently right-skewed distribution of cost data [46,47,48,49]. The association of the different sociodemographic covariates (i.e., place of residency, co-morbidities, etc.) and disease severity with asthma-related costs (as dependent variable) was explored by univariate analysis. Potential confounders (age, gender and SES) and those predictors with a p-value < 0.1 were included in the multivariate model. Estimated coefficients were reported as cost ratios (exponentiated form) which can be interpreted as a ratio of adjusted costs between the category of interest versus the category of reference for binary predictors or as the percentage of increase in the mean cost per unit increase in a continuous covariate [50,51,52]. A p-value less than 0.05 was considered statistically significant. Predicted adjusted costs were also used for comparisons in regard to clinical and sociodemographic features.
Results
Sample characteristics
The identification and selection process of the study sample is shown in Fig. 1. A final sample of 20,410 patients was analyzed. Frequencies of disease severity categories were: 69.5%, 18.0%, 6.9% and 5.5% for mild intermittent, mild persistent, moderate persistent and severe persistent asthma, respectively. As shown in Table 1, distribution of socio-demographic features and co-morbidities was significantly different among asthma severity categories. Living in an urban setting and having a low socioeconomic status (patients in the first category of SISBEN index) were predominant characteristics among all severity stages. With regard to comorbidities, atopic eczema and COPD cases were concentrated in the 0-4 yr. (45.2%) and > 60 yr. (50.7%) age groups, respectively (see Additional file 2). The estimated prevalence for atopic eczema and COPD for these age groups was 4.1% and 43.4%, respectively.
Health care resource utilization
General physician visit (57.2%) was the most commonly used medical service and emergency department (ED) visit, the least (3.5%). Frequency distribution of asthma-related services in regard to disease severity is shown in Table 2. The overall frequency of HCRU increased significantly with disease severity (p for a trend = 0.026), but it was only evident among persistent asthma categories. When analyzed individually, the use of most services also increased significantly with disease severity in contrast to ED visits that showed a negative trend.
Unadjusted direct costs according to disease severity
Mean costs of asthma-related medical services and medications increased in regard to disease severity (Table 3) except for ED visits that showed no differences (p = 0.187). The estimated mean annual (SD) direct cost per patient was I$331 (1278). Costs for mild intermittent, mild persistent, moderate and severe persistent asthma were I$67 (134), I$482 (1506), I$1061 (SD 1983) and I$2235 (SD 3426) respectively (p < 0.001). Among medical services and medications, hospitalizations and SABA treatment had the highest mean costs, respectively. Mean and median direct costs among only those who used asthma-related resources are presented in Additional files 3 and 4, respectively. Significant differences were found among costs distributed by age groups (p < 0.001) and the highest costs were observed for patients older than 60 yr. (I$533) (1942), those between 45 and 59 yr. (I$391) (1160) and children ≤4 years old (I$352) (1233).
With respect to the distribution of costs according to the type of service and severity (Fig. 2), medication expenditures accounted for almost half of the total direct costs (46.1%) with the highest proportions in moderate and severe persistent groups (53% and 61.3%, respectively). Hospitalizations expenditures accounted for 31.8% of total costs and were more concentrated among patients in the mild persistent category (49.6%) compared to moderate and severe persistent (34.7% and 29.6%, respectively). The overall proportion of costs related to general physician visits was 11.4% and was higher among mild intermittent patients (44.7%), but decreased across the other three categories. Total annual direct costs were estimated to be I$6.7 million.
Direct cost predictors
Having a comorbid condition (i.e., COPD, rhinitis, acute bronchitis), more severe asthma, belonging to highest-socioeconomic status (SISBEN 2–3 versus 1 as reference) and living in an urban setting were significant predictive factors for greater direct costs. No associations of costs with sex and age were found. Neither atopic eczema nor emphysema as co-morbidities were significantly related to direct costs (p = 0.066 and p = 0.064, respectively). The cost ratios (exponentiated form of estimated coefficients) of covariates are shown in Table 4. Adjusted mean (SD) cost of any patient with asthma was I$336 (615). Direct costs were higher in patients with severe persistent asthma compared to the other categories (p < 0.001). Adjusted mean costs stratified by different characteristics (age, gender, asthma severity, etc.) are shown in Table S5 (see Additional file 5).
Sensitivity analysis
Three different sensitivity analyses were conducted. First, exclusion of asthmatic patients with any of the five selected comorbidities decreased total costs by 39.7% (from I$6.7 million to I$4 million). Asthmatic patients with COPD added I$1.9 million (or 29%) to direct costs of the total sample of patients with asthma. Analysis in the sub-groups indicated that the mean annual cost per patient decreased from I$391 to I$236 (39.6%) and I$533 to I$308 (42.2%) in the age groups of 45-59 yr. and > 60 yr., respectively. In addition, asthmatic patients with acute bronchitis added I$361,000 to total costs estimations and the exclusion of children with this co-morbidity decreased the mean cost by less than 2% (from I$352 to I$347) among those in the 0-4 yr. of age group.
Discussion
This is the first claim-based study in Colombia that estimated the economic burden of asthma in terms of direct costs and its differences between disease severity categories. As expected, most severe cases of asthma incurred greater direct costs. Mean costs had a positive trend in relation with disease severity. Medication and hospitalizations accounted for approximately 78% of the total costs in the general cohort. In spite that patients with severe persistent asthma accounted for about 5% of the total sample, these cases contributed to more than a third of total costs (37%). Unadjusted as well as adjusted mean costs showed a positive trend with disease severity. Also, patients between 0 to 4 yrs. and > 60 yr. of age were significantly more likely to have had history of comorbidities and its effect in costs was considerable.
The influence of asthma severity and control levels in direct costs have been previously documented in some countries of Latin America [28, 53], but no information about Colombia has been published yet. The availability of large scale statistics of HCRU is mainly restricted to high-income countries [12, 54] and data are lacking for most low-and middle-income countries [2]. Gold et al. [55] used the Latin America Asthma Insights and Management Survey (LA AIM) to assess different levels of asthma control based on Global Initiative for Asthma (GINA) guidelines in five countries, and found that a poor control was a significant factor influencing health care resources use and greater medical costs, ranging from $70 for a well-controlled patient in Brazil, for an $5400 uncontrolled patient in Argentina (2013 US dollars). However, Colombia was not included in this study and therefore it is difficult to make a comparison of our results with previous estimations.
In addition, the Asthma Insights and Reality in Latin America (AIRLA) survey, conducted in 11 countries of the region, including Colombia, demonstrated the considerable lag in asthma care and control existing in these countries [28]. Based on the AIRLA survey, Neffen et al. [53], found that approximately 73.2% of annual costs of asthma-related health care for 10 countries in Latin America were due to unscheduled health care and overall related expenditure was higher among adults and children with severe persistent asthma symptoms (2010 US$558 and $769, respectively). Nevertheless, researchers were unable to include medication costs in this study; thus, estimations may underestimate the total economic impact in terms of direct costs. Even though these studies have contributed to the knowledge of asthma costs in the region, there is a potential limitation linked to their design (survey-based); frequencies may be underestimated, mainly because outcomes are reported by patients (recall bias) [56].
In Colombia, Hinestrosa et al. [57] conducted a retrospective analysis of clinical data (n = 2007) obtained from a hospital in a municipality of Colombia and found that between 2007 and 2009, medication was the main source of asthma-related direct cost (74%) derived mainly by inhaled corticosteroids. Similar results have been observed in previous studies in different countries, medication and hospitalization being the largest contributors. In 1985, hospital inpatient costs were estimated as the largest component cost of direct medical expenditures in the United States (44.6%) but, in 1994, medications had the higher proportions (40.1%) [58, 59]. Our study suggests a similar cost distribution with medications as the most important cost-deriver and SABA treatment accounting for the highest proportion of total cost among mild and moderate persistent asthma patients.
Living in an urban setting and higher SES were predictive factors for greater asthma expenditures in our study. Although there are many possible explanations (differences in the availability/proximity of health care services, level of education, environmental factors and even reverse causality) we were unable to identify causal relationships by means of this retrospective and cross-sectional study design [60]. With regard to comorbidities, the asthma and COPD overlap considerably increased costs compared to patients who had only an asthma diagnosis, indicating that COPD is also an important source of economic burden and this group of patients should be a target for policies aimed at reducing the burden associated with chronic respiratory diseases [61, 62].
The high prevalence of SABA treatment use in our findings may indicate poor adherence to controller medications or potential lack of knowledge about the efficacy of novel therapies in asthma treatment as well as established guidelines for asthma management by physicians in a clinical setting [63, 64]. The use frequency of SABA was similar to that of IC, but considerably high compared to IC + LABA combination. Together with a high rate of rescue medication, it was observed that IC prescriptions – the gold standard controller medication for persistent asthma [15] – were lower than expected. This improper management could also be explained by a low frequency of specialized physician visits even in those categorized as severe asthma (52%). In this regard, this scenario of poor asthma control and insufficient medical attention associated with elevated costs due to exacerbations and medication could imply the need for changes in Colombian policies for asthma treatment, including the creation of care management programs as observed in other Latin American countries [65].
This study has limitations in its methodology. Due to its focus on the third payer perspective, this work has restrictions to estimate epidemiologically important variables that may reflect asthma control. Frequency of exacerbations in asthmatic patients may be underestimated since many cases may have been treated at home. This could also explain why frequency of exacerbations are lower than those reported in the literature [30]. A negative trend in ED visits as disease severity increased may be explained by the positive direction in hospitalization frequencies. Our sample was not representative of the total population with asthma in Colombia; since our data was provided by an insurance company that offers health care services to less affluent inhabitants, estimations may be biased to reflect expenditures of this part of the population. Since indirect and direct non-medical asthma-related costs were not included, the total economic burden of asthma in Colombia is underestimated. Due to the nature of administrative databases, it is not possible in this type of study to assess disease control, nor to classify asthma severity according to the clinical criteria defined by internationally well-accepted guidelines or methods (i.e. GINA/ NAEPP guidelines or ERS/ATS) since claims information does not include direct clinical data inputs which usually are derived from medical charts, such as measures of daily symptoms, lung function, forced expiratory volume or peak expiratory flow [15, 18, 33]. However, the use of administrative claims data provides valuable information to estimate the magnitude in which asthma imposes an economic burden and it is, therefore, an important input for conducting economic evaluations [66, 67].
Although there is not a best-practice established algorithm for assessing disease severity in patients with asthma using administrative data, we considered that from those available in the literature, Leidy criteria is a reliable method for disease classification and the most suitable for analyzing information obtained from Colombian health system records. However, we aimed to optimize this classification adding exacerbation data, which are highly representative of disease severity. The implementation of an algorithm based in Leidy criteria in the Colombian context was possible due to the improvement of health care information systems and the availability of codified and documented data of health care utilization by patients. Limitations of prescription data for disease severity definition have been discussed by others [33]; for example, it does not ensure medication use by patients. In addition, prescriptions may be subjectively determined by the physician opinion and not accurately reflect asthma severity.
In the absence of empirical and clinical studies, this methodology can be further applied to other disease groups in the context of the developing world as a useful mechanism for generating evidence to health policy creation and evaluation. However, considerable improvements are required as there has been relatively little progress in data analysis and application despite a rapid rise of data production in this particular setting [68].
Conclusions
Asthma severity is an important factor for increasing disease-related HCRU and direct costs. Our results demonstrate the considerable economic burden of asthma to health systems in the context of the developing world. Reinforcement of asthma control programs, with a focus on disease severity and the integral management of co-morbidities, may optimize the efficacy of intervention strategies and reduce costs to the health system.
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- ED:
-
Emergency department visit
- GLM:
-
Generalized Linear Model
- HCRU:
-
Health Care Resource Utilization
- ICS + LABA:
-
Inhaled corticosteroids-long acting B2 agonist combination
- ICS:
-
Inhaled corticosteroids
- LABA:
-
Long acting B2 agonist
- OCS:
-
Oral corticosteroid
- PPA:
-
Purchasing Power Parities
- SABA:
-
Short-acting β2-agonist
- SISBEN:
-
System for Selecting Beneficiaries of Social Spending
References
Masoli M, Fabian D, Holt S, et al. The global burden of asthma: executive summary of the GINA dissemination committee report. Allergy. 2004;59:469–78. https://doi.org/10.1111/j.1398-9995.2004.00526.x.
The Global Asthma Report 2014. Auckland, New Zealand: 2014.
Hay S, Abajobir AA, Abate KH, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390:1260–344. https://doi.org/10.1016/S0140-6736(17)32130-X.
Soriano JB, Abajobir AA, Abate KH, et al. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet Respir Med. 2017;5:691–706. https://doi.org/10.1016/S2213-2600(17)30293-X.
To T, Stanojevic S, Moores G, et al. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health. 2012;12:204. https://doi.org/10.1186/1471-2458-12-204.
Bahadori K, Doyle-Waters MM, Marra C, et al. Economic burden of asthma: a systematic review. BMC Pulm Med. 2009;9:24. https://doi.org/10.1186/1471-2466-9-24.
Gergen PJ. Understanding the economic burden of asthma. J Allergy Clin Immunol. 2001;107:445–8. https://doi.org/10.1067/mai.2001.114992.
Bousquet J, Bousquet PJ, Godard P, et al. The public health implications of asthma. Bull World Health Organ. 2005;83:548–54 doi:S0042-96862005000700016 [pii].
Ehteshami-Afshar S, Fitzgerald JM, Doyle-Waters MM, et al. The global economic burden of asthma and chronic obstructive pulmonary disease. Int J Tuberc Lung Dis. 2016;20:11–23. https://doi.org/10.5588/ijtld.15.0472.
Dilokthornsakul P, Lee TA, Dhippayom T, et al. Comparison of health care utilization and costs for patients with asthma by severity and health Insurance in Thailand. Value Heal Reg Issues. 2016;9:105–11. https://doi.org/10.1016/j.vhri.2016.03.001.
Lee YJ, Kwon S-H, Hong S-H, et al. Health care utilization and direct costs in mild, moderate, and severe adult asthma: a descriptive study using the 2014 south Korean health insurance database. Clin Ther. 2017;39:1–10. https://doi.org/10.1016/j.clinthera.2017.01.025.
Chastek B, Korrer S, Nagar SP, et al. Economic burden of illness among patients with severe asthma in a managed care setting. J Manag Care Spec Pharm. 2016;22:848–61. https://doi.org/10.18553/jmcp.2016.22.7.848.
Antonicelli L, Bucca C, Neri M, et al. Asthma severity and medical resource utilisation. Eur Respir J. 2004;23:723–9. https://doi.org/10.1183/09031936.04.00004904.
Bush A, Kleinert S, Pavord ID. The asthmas in 2015 and beyond: a lancet commission. Lancet. 2015;385:1273–5. https://doi.org/10.1016/S0140-6736(15)60654-7.
Global Initiative for Asthma. Global Strategy For Asthma Management and Prevention. 2017.
Lalloo UG, Walters RD, Adachi M, et al. Asthma programmes in diverse regions of the world: challenges, successes and lessons learnt. Int J Tuberc Lung Dis. 2011;15:1574–86. https://doi.org/10.5588/ijtld.11.0289.
Reddel HK, Taylor DR, Bateman ED, et al. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations - standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med. 2009;180:59–99. https://doi.org/10.1164/rccm.200801-060ST.
Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma task force report ers/ats guidelines on severe asthma Executive Summary. Eur Respir J. 2014;43:343–73. https://doi.org/10.1183/09031936.00202013.
Rabe KF, Adachi M, Lai CKW, et al. Worldwide severity and control of asthma in children and adults: the global asthma insights and reality surveys. J Allergy Clin Immunol. 2004;114:40–7. https://doi.org/10.1016/j.jaci.2004.04.042.
Rabe KF, Vermeire PA, Soriano JB, et al. Clinical management of asthma in 1999 : the Asthma Insights and Reality in Europe ( AIRE ) study. Eur Respir J. 2000:802–7.
Gold LS, Thompson P, Salvi S, et al. Level of asthma control and health care utilization in Asia-Pacific countries. Respir Med. 2014;108:271–7. https://doi.org/10.1016/j.rmed.2013.12.004.
Beran D, Zar HJ, Perrin C, et al. Burden of asthma and chronic obstructive pulmonary disease and access to essential medicines in low-income and middle-income countries. Lancet Respir Med. 2015;3:159–70. https://doi.org/10.1016/S2213-2600(15)00004-1.
Caraballo L, Zakzuk J, Lee BW, et al. Particularities of allergy in the tropics. World Allergy Organ J. 2016;9:20. https://doi.org/10.1186/s40413-016-0110-7.
Mallol J. Asthma in Latin America: where the asthma causative/protective hypotheses fail. Allergol Immunopathol (Madr). 2008;36:150–3. https://doi.org/10.1157/13124721.
Sánchez-Borges M, Capriles-Hulett A, Caballero-Fonseca F. Asthma care in resource-poor settings. World Allergy Organ J. 2011;4:68–72. https://doi.org/10.1097/WOX.0b013e318213598d.
Lopez AD, Williams TN, Levin A, et al. Remembering the forgotten non-communicable diseases. BMC Med. 2014;12:200. https://doi.org/10.1186/s12916-014-0200-8.
Maspero JF, Jardim JR, Aranda A, et al. Insights, attitudes, and perceptions about asthma and its treatment: findings from a multinational survey of patients from Latin America. World Allergy Organ J. 2013;6:1–7. https://doi.org/10.1186/1939-4551-6-19.
Neffen H, Fritscher C, Schacht FC, et al. Asthma control in Latin America: the asthma insights and reality in Latin America (AIRLA) survey. Rev Panam Salud Publica/Pan Am J Public Heal. 2005;17:191–7.
WHO and UN partners. Colombia: WHO statistical profile. Ctry. Stat. Glob. Heal. Estim. 2015.http://www.who.int/gho/countries/col.pdf?ua=1 (accessed 12 Dec 2017).
Dennis RJ, Caraballo L, García E, et al. Prevalence of asthma and other allergic conditions in Colombia 2009–2010: a cross-sectional study. BMC Pulm Med. 2012;12:17. https://doi.org/10.1186/1471-2466-12-17.
Dennis R, Caraballo L, García E, et al. Asthma and other allergic conditions in Colombia: a study in 6 cities. Ann Allergy Asthma Immunol. 2004;93:568–74. https://doi.org/10.1016/S1081-1206(10)61265-3.
Leidy N, Paramore L, Watrous M, et al. Development of an algorithm for estimating asthma severity from an administrative cost database. Value Heal. 1999;2:394–5. https://doi.org/10.1016/S1098-3015(10)75867-8.
Jacob C, Haas JS, Bechtel B, et al. Assessing asthma severity based on claims data: a systematic review. Eur J Health Econ. 2017;18:227–41. https://doi.org/10.1007/s10198-016-0769-2.
Ivanova JI, Bergman R, Birnbaum HG, et al. Effect of asthma exacerbations on health care costs among asthmatic patients with moderate and severe persistent asthma. J Allergy Clin Immunol. 2012;129:1229–35. https://doi.org/10.1016/j.jaci.2012.01.039.
Wells KE, Peterson EL, Ahmedani BK, et al. The relationship between combination inhaled corticosteroid and long-acting β-agonist use and severe asthma exacerbations in a diverse population. J Allergy Clin Immunol. 2012;129:1274–9. https://doi.org/10.1016/j.jaci.2011.12.974.
Allen-ramey FC, Bukstein D, Luskin A, et al. Administrative claims analysis of asthma-related health care utilization for patients who received inhaled corticosteroids with either Montelukast or Salmeterol as combination therapy. J Manag Care Pharm. 2006;12:310–21.
Castañeda T. Targeting social spending to the poor with proxy–means testing: Colombia’s SISBEN system. Washington DC; 2005.
The World Bank. Purchasing power parity conversion factor. Int Comp Progr database. 2015; https://dataworldbankorg/indicator/PANUSPPP (accessed 12 Dec 2017.
World Health Organization. Choosing Interventions that are Cost Effective (WHO-CHOICE)-Costs and Prices. http://www.who.int/choice/costs/ppp/en/
Drummond M, Barbieri M, Cook J, et al. Transferability of economic evaluations across jurisdictions: ISPOR good research practices task force report. Value Heal. 2009;12:409–18. https://doi.org/10.1111/j.1524-4733.2008.00489.x.
Banke-Thomas A, Wilson-Jones M, Madaj B, et al. Economic evaluation of emergency obstetric care training: a systematic review. BMC Pregnancy Childbirth. 2017;17:403. https://doi.org/10.1186/s12884-017-1586-z.
Ramsey SD, Willke RJ, Glick H, et al. Cost-effectiveness analysis alongside clinical trials II—an ISPOR good research practices task force report. Value Heal. 2015;18:161–72. https://doi.org/10.1016/j.jval.2015.02.001.
Barber JA, Thompson SG, Drummond M, et al. Analysis and interpretation of cost data in randomised controlled trials: review of published studies. BMJ. 1998;317:1195–200. https://doi.org/10.1136/bmj.317.7167.1195.
Briggs A, Gray A. The distribution of health care costs and their statistical analysis for economic evaluation. J Health Serv Res Policy. 1998;3:233–45.
Thompson SG, J a B. How should cost data in pragmatic randomised trials be analysed? BMJ. 2000;320:1197–200. https://doi.org/10.1136/bmj.320.7243.1197.
Mihaylova B, Briggs A, O’Hagan A, et al. Review of statistical methods for analysing healthcare resources and costs. Health Econ. 2011;20:897–916. https://doi.org/10.1002/hec.1653.
Gray A, Clarke PM, Wolstenholme J, et al. Applied methods for cost-effectiveness analysis in health care. In: Oxford University press; 2010.
Dodd S, Bassi A, Bodger K, et al. A comparison of multivariable regression models to analyse cost data. J Eval Clin Pract. 2006;12:76–86. https://doi.org/10.1111/j.1365-2753.2006.00610.x.
Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20:461–94. https://doi.org/10.1016/S0167-6296(01)00086-8.
Blough DK, Madden CW, Hornbrook MC. Modeling risk using generalized linear models. J Health Econ. 1999;18:153–71. https://doi.org/10.1016/S0167-6296(98)00032-0.
Barber J, Thompson S. Multiple regression of cost data: use of generalised linear models. J Health Serv Res Policy. 2004;9:197–204. https://doi.org/10.1258/1355819042250249.
Brilleman SL, Gravelle H, Hollinghurst S, et al. Keep it simple? Predicting primary health care costs with clinical morbidity measures. J Health Econ. 2014;35:109–22.c.
Neffen H, Gonzalez SN, Fritscher CC, et al. The burden of unscheduled health care for asthma in Latin America. J Investig Allergol Clin Immunol. 2010;20:596–601.
Janson C, Lisspers K, Ställberg B, Johansson G, Telg G, Thuresson M, Nordahl Christensen H, Larsson K. Health care resource utilization and cost for asthma patients regularly treated with oral corticosteroids - a Swedish observational cohort study (PACEHR). Respir Res. 2018;19(1):168. https://doi.org/10.1186/s12931-018-0855-3. PubMed PMID: 30176850; PubMed Central PMCID: PMC6122138.
Gold LS, Montealegre F, Allen-Ramey FC, et al. Asthma control and cost in Latin America. Value Heal Reg Issues. 2014;5:25–8. https://doi.org/10.1016/j.vhri.2014.06.007.
Short ME, Goetzel RZ, Pei X, et al. How accurate are self-reports? Analysis of self-reported health care utilization and absence when compared with administrative data. J Occup Environ Med. 2009;51:786–96. https://doi.org/10.1097/JOM.0b013e3181a86671.
Hinestrosa Hurtado F. Cost of illness of asthma in a hospital of the Colombian region of Caldas 2007–2009. 2010.http://www.bdigital.unal.edu.co/2996/1/192251.2010.pdf
Weiss KB, Gergen PJ, Hodgson TA. An economic evaluation of asthma in the United States. N Engl J Med. 1992;326:862–6. https://doi.org/10.1056/NEJM199203263261304.
Weiss KB, Sullivan SD, Lyttle CS. Trends in the cost of illness for asthma in the United States, 1985-1994. J Allergy Clin Immunol. 2000;106:493–9. https://doi.org/10.1067/mai.2000.109426.
Rona RJ. Asthma and poverty. Thorax. 2000;55:239–44. https://doi.org/10.1136/thorax.55.3.239.
Bujarski S, Parulekar AD, Sharafkhaneh A, et al. The asthma COPD overlap syndrome (ACOS). Curr Allergy Asthma Rep. 2015;15. https://doi.org/10.1007/s11882-014-0509-6.
Blanchette CM, Gutierrez B, Ory C, et al. Economic burden in direct costs of concomitant chronic obstructive pulmonary disease and asthma in a Medicare advantage population. J Manag Care Pharm. 2008;14:176–85. https://doi.org/10.18553/jmcp.2008.14.2.176.
Silveira CD, Araújo FDB, Ferreira Pereira LF, et al. Evaluation of the treatment provided to patients with asthma by the Brazilian unified care system. J Bras Pneumol. 2009;35:628–34. https://doi.org/10.1093/annonc/mdp346.
Aït-Khaled N. Enarson D a., Bencharif N, et al. implementation of asthma guidelines in health centres of several developing countries. Int J Tuberc Lung Dis. 2006;10:104–9.
Cruz AA, Souza-Machado A, Franco R, et al. The impact of a program for control of asthma in a low-income setting. World Allergy Organ J. 2010;3:167–74. https://doi.org/10.1097/WOX.0b013e3181dc3383.
Birnbaum HG, Ivanova JI, Yu AP, et al. Asthma severity categorization using a claims-based algorithm or pulmonary function testing. J Asthma. 2009;46:67–72. https://doi.org/10.1080/02770900802503099.
Thomas M, Cleland J, Price D. Database studies in asthma pharmacoeconomics: uses, limitations and quality markers. Expert Opin Pharmacother. 2003;4:351–8. https://doi.org/10.1517/14656566.4.3.351.
Wyber R, Vaillancourt S, Perry W, et al. Big data in global health: improving health in low- and middle-income countries. Bull World Health Organ. 2015;93:203–8. https://doi.org/10.2471/BLT.14.139022.
Acknowledgements
We are grateful with COOSALUD for providing the database of medical claims for this study. Special thanks to Alexandra O’Rourke for her assistance in the language revision of the manuscript.
Funding
This research was supported by the Colombian government (Departamento Administrativo de Ciencia y Tecnología e Innovación, Colciencias) through the grant #406–2011 and the scholarship Jovenes Investigadores, University of Cartagena and The Foundation for the Development of Medical and Biological Sciences (Fundemeb).
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
Data analysis (DP and AF), data interpretation (DP, AF, JZ and NA), writing (DP, AF, JZ and LC), study design (NA) or critical revision (LC). All authors read approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Ethical Committee of the University of Cartagena (Minute 36, October 11th 2011).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Table S1. Asthma medication (DOCX 18 kb)
Additional file 2:
Table S2. Distribution of comorbidities according to age (DOCX 13 kb)
Additional file 3:
Table S3. Unadjusted direct mean annual asthma-related costs among health care resource users (DOCX 20 kb)
Additional file 4:
Table S4. Unadjusted direct median annual asthma-related costs among health care resource users (DOCX 20 kb)
Additional file 5:
Table S5. Adjusted direct mean annual asthma-related costs by patient characteristics (DOCX 15 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Flórez-Tanus, Á., Parra, D., Zakzuk, J. et al. Health care costs and resource utilization for different asthma severity stages in Colombia: a claims data analysis. World Allergy Organ J 11, 26 (2018). https://doi.org/10.1186/s40413-018-0205-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40413-018-0205-4