Abstract
Background
The study was designed to investigate effects of single intravenous injection of esketamine on the incidence of postpartum depression (PPD) after labor analgesia and explore the potential mechanisms.
Methods
A total of 120 women who underwent labor analgesia by epidural analgesia pump were enrolled and divided into two groups randomly. Esketamine at a dose of 0.2 mg/kg was intravenously injected after fetal disengagement in the test group and placebo was administered in the control group. The occurrence of PPD and side effects after delivery were recorded. Some indicators related to stress and inflammation were measured before labor analgesia and at 24 h, 1 week, and 6 weeks after delivery in this study. Data were analyzed by independent t-test, repeated measures analysis of variance and Chi-square test in SPSS software (version 25.0). It was considered statistically significant since a p value less than 0.05.
Results
The incidence of PPD was significantly decreased both for one week and six weeks after delivery by using of esketamine (3.4% vs. 15.3%, p = 0.004 and 5.2% vs. 18.6%, p = 0.006, respectively). There were also significant differences between the stress and inflammation-related indicators in different time points in this study, while the side effects for 48 h after delivery were similar between the two groups.
Conclusions
Single intravenous injection of esketamine after delivery in participants underwent labor analgesia can decrease the occurrence of postpartum depression for one week and six weeks after delivery, while the side effects were not increased. The antidepressant effects of esketamine may be related to the reduction of stress response and inflammation.
Trial registration
The trial was registered at the Chinese Clinical Trial Registry on 5/30/2022 (CTRI registration number—ChiCTR2200060387). URL of registry: https://www.chictr.org.cn/bin/home.
Similar content being viewed by others
Introduction
Due to the particularity of physiology, maternal perinatal safety has been a special concern. At present, the labor analgesia is gradually recommended on the premise of ensuring maternal and fetal safety [1]. Postpartum depression (PPD) is a mental illness occurring in the puerperium, showing a series symptoms such as depression, sadness, crying, irritability, even hallucinations or suicide, which seriously endangers the physical and mental health of pregnant women [2, 3]. PPD is related to maternal psychological and physical, family, social and obstetric factors, and occurs during six weeks after delivery in either primigravida or multipara undergoing cesarean section or vaginal delivery [4, 5], with the incidence even up to 38.5% [6]. Due to its high incidence and harmfulness, the treatment and prevention of PPD have become an important topic.
Nowadays, medication combined with psychological counseling are mainly used for the treatment of PPD. However, long-term medication may have side effects for lactating women on the infant’s motional, behavioral and neurological development [7]. Thus, prevention of PPD is even more important than treatment. As an intravenous anesthetic drug, ketamine is often used in pediatric, obstetric, and outpatient anesthesia. In addition, as a psychotropic drug, the antidepressant effect of ketamine is also gradually recognized. Studies have shown that ketamine can significantly reduce the incidence and severity of depression [8, 9]. As an isomer of ketamine, compared with racemic ketamine, esketamine has stronger analgesic and sedative effects, smaller cardiovascular and psychiatric adverse effects, and can also be used in patients with refractory, severe depression and epilepsy [10]. Our previous studies have suggested that esketamine prevent PPD in women underwent cesarean Sects. [11, 12]. However, with the widespread use of labor analgesia in obstetrics, it was also unknown whether esketamine was effective in such maternal postpartum depression. Additionally, the mechanisms of antidepressant effects of esketamine were unclear now. Therefore, we designed the study which was aimed to confirm the antidepressant effect of esketamine in women underwent labor analgesia and explore potential mechanisms.
Methods
Study design
This randomized, double-blinded, controlled trial was conducted at the Affiliated Jiangning Hospital of Nanjing Medical University, Nanjing, China, from 6/1/2022 to 2/28/2023, which performed in accordance with the declaration of Helsinki. The Consolidated Standards of Reporting Trials (CONSORT) recommendations were followed in this study [13]. The study protocol was approved by the medical ethics committee of our hospital on 1/14/2022 (Ethical approval number: 2021-03-031-K01). Then, the study was registered at the Chinese Clinical Trial Registry on 5/30/2022 (CTRI registration number—ChiCTR2200060387). All participants involved were informed of the proposal and gave their written, informed consent form voluntarily before enrollment.
Study participants
One hundred and twenty primiparous women who underwent labor analgesia, aged 22 to 38, with American society of Aneshesiologists (ASA) physical status II, with 1 fetal 0 labor, pregnancy time greater than 38 weeks and less than 42 weeks, and single term pregnancy, were enrolled. The exclusion criteria were as follows: not suitable for transvaginal delivery; combined with coagulation disorders; having mental disorder; organic or pharmacogenic depression before delivery; the Self-rating Anxiety Scale (SAS) ≥ 50 or the Self-rating Depression Scale (SDS) ≥ 0.5 [14]; perineal tears or a lateral cut required during delivery; Apgar score of fetus at delivery < 8; postpartum hemorrhage > 500 ml; failure of epidural puncture; changed to cesarean section.
Sample size estimation
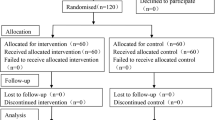
Based on the results of our pre-experiment (10 participants in each group), the incidence of PPD at 6 weeks after delivery can be reduced by 12% in the tested group. Power analysis showed that a reduction rate of 15% with α = 0.05 and a 10% dropout rate within a power value of 90%, a sample size of at least 54 per group were needed. A total of 120 samples were designed in this study, for 60 in each group respectively. Figure 1 showed the consolidated standards of reporting trials (CONSORT) flow diagram of the study participant’s recruitment.
CONSORT flow diagram. In the study, a total of 120 participants were enrolled initially and three participants were excluded during the trial. Finally, There were 117 participants included in the statistical analysis (58 in Group E and 59 in Group C, respectively). CONSORT: the Consolidated Standards of Reporting Trials
Randomization and allocation concealment
Participants were randomly assigned to one of two groups. Random tables were generated by SPSS 20.0. One hundred and twenty sealed envelopes were prepared by a statistician who did not participate in the study. The study was performed with neither patients’ nor observers’ awareness of the group to which each patient belonged. To assure concealment of allocation, numbers were kept in sealed and opaque envelopes, which were opened by an anaesthesiologist who was not involved in the study.
Study interventions
After entering the delivery room, peripheral venous access was opened in all participants, maternal heart rate, noninvasive blood pressure measurement, electrocardiography and pulse oximetry were monitored. All women were received oxygen for 3 L/min by transnasal catheter. Epidural anaesthesia were operated between L2 and L3 after cervical dilation up to 2 ~ 3 cm. After successful puncture, the epidural catheter was placed for 3.5 cm toward the head position and 1% lidocaine was injected for 3 ml. The epidural analgesia pump was connected, in which was 0.75% ropivacaine hydrochloride (20 ml) were diluted by normal saline up to 100 ml. All pumps were set with a bolus of 10 ml, continuous infusion amount of 8 ml/h, single dose of 4 ml, locking time of 15 min and stopped after fetal disengagement. Esketamine (0.2 mg/kg) was intravenously injected after fetal disengagement in the test group (Group E), while the placebo (normal saline) was administered in the control group (Group C). Labor analgesia was performed by the same anesthesiologist and esketamine or placebo were administrated by the same nurse anesthetist. Perinatal management was completed by the same obstetric team. Neither the subjects and the investigators were aware of the enrollment.
Outcome measurements
The primary outcomes of the study were the incidence of PPD at one week and six weeks after delivery. The diagnosis of postpartum depression was based on the reference [15] and [16], in which the depression score (Edinburgh Postpartum Depression Scale, EPDS) and the diagnostic criteria for mental disorders are included.
Ramsay sedation score before analgesia (T0), 5 (T1), 10 (T2), 20 (T3), 30 (T4) and 60 (T5) minutes after administration of esketamine were measured. The scoring criteria [17] were as follows: 1 point, patients were awake, feeling anxiety or irritability; 2 points, patients were awake, being cooperative, directional or quiet; 3 points, patients were awake, only being responsive to commands; 4 points, patients were asleep, being responsive quickly to tapping eyebrow or soft tone stimulation; 5 points, patients were asleep, being responsive slowly to tapping eyebrow or strong acoustic stimulation; 6 points, patients were asleep, being no responsive to tapping eyebrow or strong acoustic stimulation.
All women were tested levels of norepinephrine (NE), epinephrine (E) ,C-reactive protein (CRP), interleukin-6 (IL-6) and interleukin-10 (IL-10) in peripheral venous blood before labor analgesia (when the woman was quiet in the ward), at 24 h, 1 week, and 6 weeks after delivery. Serum concentrations of IL-6 and IL-10 were determined by enzyme linked immunosorbent assay (ELISA).
The duration of the first and second stage of labor, the Apgar score of fetus at delivery, and the volume of postpartum hemorrhage was calculated for 24 h after delivery. Side effects such as nightmares, drowsiness, nausea and vomiting were measured for 48 h after delivery as well.
Statistical analysis
The statistical analysis were performed using SPSS software package (version 25.0; IBM, Inc., Chicago, IL, USA). The continuous data were presented as mean (M) ± standard deviation (SD) and examined by independent t-test. The categorical data were shown as n(%) and examined with a Chi-square test. It was considered statistically significant since a p value < 0.05.
Results
Patient recruitment
In the study, a total of 120 participants were enrolled initially and three participants were excluded during the trial. One case was excluded for failure of epidural puncture, and another one was for changed to cesarean section in Group E, while one participant was excluded for failure of epidural puncture in Group C. Finally, There were 117 participants included in the statistical analysis (58 in Group E and 59 in Group C, respectively. Figure 1, CONSORT flow diagram).
Patient characteristics
There were no significant difference of the patient characteristics (age, height, weight, BMI, gestational week, the duration of the first and second stage of labor, the Apgar score of fetus at delivery, volume of postpartum hemorrhage) between the two groups (Table 1).
Ramsay sedation score
There were no significant difference of the Ramsay sedation score at T0 and T5 between the two groups. Compared with Group C, the Ramsay sedation score at T1, T2, T3 and T4 were significantly higher in Group E (Table 2).
Incidence of PPD and side effects
The incidence of PPD was significantly decreased both for one week and six weeks after delivery in Group E (3.4% vs. 15.3%, p = 0.004 and 5.2% vs. 18.6%, p = 0.006, respectively).The incidence of side effects after delivery were similar between the two groups (Table 3).
Levels of NE, E, CRP, IL-6 and IL-10
There were no significant difference of the levels of NE, E, CRP, IL-6 and IL-10.
between the two groups before labor analgesia and 6 weeks after delivery. Compared with Group C, the levels of NE, E, CRP and IL-6 were significantly lower for 24 h and 1 week after delivery in Group E, while IL-10 were higher at the same time (Table 4).
Discussion
Pain in the perinatal period is one of the factors leading to the development of PPD. The symptoms of PPD are more prominent in women who experience frequent pain during childbirth [18]. Although maternal pain can be relieved by labor analgesia, psychological degeneration, emotional vulnerability, stress response and inflammation may also lead to a high occurrence of PPD [19]. The study of Bruno et al. [20] also showed that anger experience and expression can be considered as vulnerability factors for postpartum mood disorders onset. In the study of Rizzo et al. [21], the role of subthreshold mental disorders were examined as predictors of PPD. The results suggested that agoraphobia/panic, depressed mood, social anxiety and eating problems relate positively to PPD at 3/6 months. In our study, participants combined with coagulation disorders, mental disorder; organic or pharmacogenic depression, SAS ≥ 50 and SAS ≥ 0.5 before delivery were all excluded. The results of this study showed that single intravenous injection of esketamine decreased the occurrence of PPD for one week and six weeks after delivery in women underwent labor analgesia without increasing related side effects.
The traditional treatment for depression is to increase the amount of serotonin in the synaptic space to achieve the effect of alleviating depression, but these antidepressants are slow to act, generally taking three to six weeks to achieve therapeutic effects [22]. In 2019, the U. S. Food and Drug Administration (FDA) granted esketamine for the treatment of major depressive disorder and drug-resistant depression with urgent suicide risk. The results of a meta-analysis indicated that esketamine can significantly improve the patients’ low mood, low self-evaluation, and even weaken the suicidal ideation, especially improve the therapeutic effect for treatment resistant depression (TRD) [23].
Another retrospective analysis have showed that both esketamine’s approval for use in TRD and longer-term safety data may position it preferentially above racemic ketamine, though the efficacy of esketamine compared to racemic ketamine remained unclear [24]. However, there are few studies on esketamine used in postpartum depression. Our previous studies indicated that the incidence of PPD was reduced by prophylactic intravenous use of esketamine or combined with patient control intravenous analgesia for women underwent cesarean Sects. [11, 12]. The study of Wang et al. [25] also have showed that the application of esketamine after cesarean section can effectively reduce depression-related scores and the risk of postpartum depression without increasing adverse reactions and had high safety. However, a lower dose of esketamine was used in our study. Based on previous studies, we applied esketamine to the prevention of postpartum depression in labor analgesia and achieved certain results in this study.
As endocrine hormones, NE and E can affect the bodies’ mood by modulating the sensitivity of neuronal synapses and neurotransmitters [26]. NE can return to the synaptic space under the action of NE transporter protein, and also form E by acting on phenylmethylamine-N-methyltransferase, which easily lead to fear and tension [27]. It had been reported that the blue spot located in the brain stem was activated due to the changes in stress and hormone levels during pregnancy, thus releasing a large number of NE to participate in the regulation of the nervous system, which was easy to cause tension and depression [28]. In this study, the levels of NE and E were significantly lower at 24 h and 1 week after delivery in Group E than in Group C, which also suggested that the maternal stress response was decreased in the tested group. The antidepressant mechanism may be the target of esketamine for monoaminergic nervous system, can affect the brain stem blue spot, and further affect the noradrenergic system, promote the transcription and expression of the gene, increase the synthesis of transporter, resulting in NE migration from plasma membrane to cytoplasm, decrease the concentration of serum NE and E [29]. Additionally, due to the sedative and analgesic effects of esketamine, the Ramsay sedation score was decreased at 5, 10, 20 and 30 min after administration of esketamine in this study, which might be one of the reasons for the reduced stress response in the tested group.
As a non-specific inflammatory marker, CRP reflects the stress and inflammation response of the human body. When infection and injury take place, CRP rises sharply in the plasma [30]. Besides, among the inflammatory mediators released by the human body under pain and traumatic stress, IL-6 is the earliest and highly sensitive proinflammatory factor expressed, which is closely related to the size of trauma, body immune status and prognosis [31]. IL-10 is an inflammatory suppressor, which can exert an anti-inflammatory effect by inhibiting nuclear factors activity and promoting neutrophil apoptosis to reduce pro-inflammatory factors [32]. Therefore, the levels of CRP, IL-6 and IL-10 were observed in the present study to measure the effects of esketamine on inflammatory response. In this study, the levels of CRP and IL-6 were significantly lower at 24 h and 1 week after delivery in the tested group, while IL-10 were higher at the same time. This results indicated that the antidepressant effect of esketamine might be related to the reduced inflammatory response in puerperants underwent labor analgesia.
Studies have shown the brain causes negative emotions by the clustering of the lateral halterate nucleus, where the excitatory transmitter is the N-methyl-D-aspartate (NMDA) receptor of the glutamate-gated ion channel [33, 34]. As a blocker of the glutamate-gated ion channel NMDA receptor, the main antidepressant mechanism of esketamine is to sustainable block the NMDA receptor, block the elongation factor 2 (eEF 2) kinase, increase the release of brain-derived neurotrophic factor (BDNF) and the expression of tropomyosin receptor kinase B (TrkB), induce rapamycin target complex 1 (mTORC1) signaling pathway and extracellular regulatory protein kinase (ERK) activation, improve neuroplasticity and synapse formation [35, 36]. In short, the traditional treatment of antidepression drugs is to stimulate the “reward center” of the brain, while esketamine is to remove the inhibitory effect of the “reward center”.
Esketamine has been used clinically for many years as an anesthetic drug, which is now also widely concerned as a new antidepressant. Considering the possible side effects such as nightmare, hallucination and abusement [37], esketamine was used only once in the study and was lower than the subanesthetic dose. In addition, through the follow-up after delivery, we found that the adverse reactions did not increase in the test group.
There were some limitations in this study, such as the strong subjectivity of the PPD evaluation by EPDS. To minimize the subjective differences, the PPD valuator in this study was the same physician who did not participate in the specific study. Furthermore, the objective indicators such as levels of, NE, E, CRP, IL−6 and IL−10 were also combined in the study, which could better reflect maternal depression. Furthermore, the severity of PPD was not measured in this study, which would be content of next studies.
Conclusions
In conclusion, single intravenous injection of esketamine (0.2 mg/kg) after delivery in participants underwent labor analgesia can decrease the occurrence of postpartum depression for one week and six weeks after delivery, while the side effects were not increased. The antidepressant effects of esketamine may be related to the reduction of stress response and inflammation.
Data Availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request. Wei Wang, e-mail: wangwei2024@163.com.
Abbreviations
- PPD:
-
postpartum depression
- ASA:
-
American society of Anesthesiologists
- CONSORT:
-
consolidated standards of reporting trials
- SAS:
-
the Self-rating Anxiety Scale
- SDS:
-
the Self-rating Depression Scale
- EPDS:
-
Edinburgh Postpartum Depression Scale
- NE:
-
norepinephrine
- E:
-
epinephrine
- CRP:
-
C-reactive protein
- IL-6:
-
interleukin-6
- IL-10:
-
interleukin-10
- NMDA:
-
N-methyl-D-aspartate
References
Zhao P, Cai Z, Huang A, Liu C, Li H, Yang S, et al. Why is the labor epidural rate low and cesarean delivery rate high? A survey of Chinese perinatal care providers. PLoS ONE. 2021;16(5):e0251345.
Wedajo LF, Alemu SS, Jarso MH, Golge AM, Dirirsa DE. Late postpartum depression and associated factors: community-based cross-sectional study. BMC Womens Health. 2023;23(1):280.
Pingeton BC, Cochran A, Goodman SH, Laurent H, Sbrilli MD, Knight B, et al. Positive affect improves a transdiagnostic model of perinatal depression symptoms. J Affect Disord. 2023;336:112–9.
Serra R, Giacchetti N, Bersani FS, Cappannini G, Martucci M, Panfili M, et al. The relationship between personality traits and individual factors with perinatal depressive symptoms: a cross-sectional study. BMC Pregnancy Childbirth. 2023;23(1):382.
Bales M, Pambrun E, Maguet C, van der Waerden J, Glangeaud-Freudenthal N, Charles MA, et al. Pathways between Risk/Protective factors and maternal postnatal depressive symptoms: the ELFE Cohort. J Clin Med. 2023;12(9):3204.
Almutairi HA, Alyousef SM, Alhamidi SA, Almoammar DN. Exploring the Healthcare Services’ contribution to reducing Postpartum Depression. SAGE Open Nurs. 2023;9:23779608231171780.
Horwitz AB, Rubin RT. Barbiturates and pyrazolopyridines for the treatment of postpartum depression-repurposing of two drug classes. Front Pharmacol. 2023;14:1139889.
Chen-Li D, Lui LMW, Rosenblat JD, Lipsitz O, Teopiz KM, Ho R, et al. Ketamine as potential treatment for postpartum depression: a narrative review. Ann Clin Psychiatry. 2022;34(4):264–74.
Włodarczyk A, Dywel A, Cubała WJ. Safety and Tolerability of the Acute ketamine treatment in treatment-resistant depression: focus on Comorbidities interplay with dissociation and psychomimetic symptoms. Pharmaceuticals (Basel). 2023;16(2):173.
Vasiliu O. Esketamine for treatmentresistant depression: a review of clinical evidence (review). Exp Ther Med. 2023;25(3):111.
Wang W, Xu H, Ling B, Chen Q, Lv J, Yu W. Effects of esketamine on analgesia and postpartum depression after cesarean section: a randomized, double-blinded controlled trial. Med (Baltim). 2022;101(47):e32010.
Wang W, Ling B, Chen Q, Xu H, Lv J, Yu W. Effect of pre-administration of esketamine intraoperatively on postpartum depression after cesarean section: a randomized, double-blinded controlled trial. Med (Baltim). 2023;102(9):e33086.
Calvert M, Blazeby J, Altman DG, Revicki DA, Moher D, Brundage MD, CONSORT PRO Group. Reporting of patient-reported outcomes in randomized trials: the CONSORT PRO extension. JAMA. 2013;309(8):814–22.
Chen W, Peng W, Zhang Y, Zhou H, Zhang M. Anxiety and depression among perinatal women during the long-term normal prevention of COVID-19 pandemic period in China: a cross-sectional study. BMC Psychiatry. 2023;23(1):451.
Srisurapanont M, Oon-Arom A, Suradom C, Luewan S, Kawilapat S. Convergent validity of the Edinburgh Postnatal Depression Scale and the Patient Health Questionnaire (PHQ-9) in pregnant and Postpartum women: their construct correlations with functional disability. Healthc (Basel). 2023;11(5):699.
Kammerer M, Marks MN, Pinard C, Taylor A, von Castelberg B, Künzli H, et al. Symptoms associated with the DSM IV diagnosis of depression in pregnancy and post partum. Arch Womens Ment Health. 2009;12(3):135–41.
Zaki HA, Ibrahim T, Osman A, Elnabawy WA, Gebril A, Hamdi AH, et al. Comparing the safety and effectiveness of ketamine Versus Benzodiazepine/Opioid combination for Procedural Sedation in Emergency Medicine: a Comprehensive Review and Meta-Analysis. Cureus. 2023;15(3):e36742.
Levin G, Ein-Dor T. A unified model of the biology of peripartum depression. Transl Psychiatry. 2023;13(1):138.
Du W, Bo L, Xu Z, Liu Z, Childbirth Pain. Labor Epidural Analgesia, and Postpartum Depression: recent evidence and future directions. J Pain Res. 2022;15:3007–15.
Bruno A, Laganà AS, Leonardi V, Greco D, Merlino M, Vitale SG, et al. Inside-out: the role of anger experience and expression in the development of postpartum mood disorders. J Matern Fetal Neonatal Med. 2018;31(22):3033–8.
Rizzo A, Bruno A, Torre G, Mento C, Pandolfo G, Cedro C, et al. Subthreshold psychiatric symptoms as potential predictors of postpartum depression. Health Care Women Int. 2022;43(1–3):129–41.
Witkin JM, Golani LK, Smith JL. Clinical pharmacological innovation in the treatment of depression. Expert Rev Clin Pharmacol. 2023;16(4):349–62.
Floriano I, Silvinato A, Bernardo WM. The use of esketamine in the treatment of patients with severe depression and suicidal ideation: systematic review and meta-analysis. Rev Assoc Med Bras (1992). 2023;69(4):e2023D694.
Swainson J, Thomas RK, Archer S, Chrenek C, MacKay MA, Baker G, et al. Esketamine for treatment resistant depression. Expert Rev Neurother. 2019;19(10):899–911.
Wang Q, Xiao M, Sun H, Zhang P. A Study on the Preventive Effect of Esketamine on Postpartum Depression (PPD) after Cesarean Section. Comput Math Methods Med. 2022; 2022:1524198.
Peacock BN, Scheiderer DJ, Kellermann GH. Biomolecular aspects of depression: a retrospective analysis. Compr Psychiatry. 2017;73:168–80.
Wang P, Yan F, Dong J, Wang S, Shi Y, Zhu M, et al. A multiple-step screening protocol to identify norepinephrine and dopamine reuptake inhibitors for depression. Phys Chem Chem Phys. 2023;25(12):8341–54.
Meng Q, Garcia-Garcia AL, Dranovsky A, Leonardo ED. Inhibition of norepinephrine signaling during a sensitive period disrupts locus coeruleus circuitry and emotional behaviors in adulthood. Sci Rep. 2023;13(1):3077.
Liu H, Lan X, Wang C, Zhang F, Fu L, Li W, et al. The efficacy and safety of esketamine in the treatment of major depressive disorder with suicidal ideation: study protocol for a randomized controlled trial. BMC Psychiatry. 2022;22(1):744.
Filep JG. Targeting conformational changes in C-reactive protein to inhibit pro-inflammatory actions. EMBO Mol Med. 2023;15(1):e17003.
Yeh MSL, Poyares D, D’Elia ATD, Coimbra BM, Mello AF, Tufik S, et al. Sleep characteristics and inflammatory markers in women with post-traumatic stress disorder. BMC Psychiatry. 2023;23(1):273.
Nagata K, Nishiyama C. IL-10in mast cell-mediated Immune Responses: anti-inflammatory and proinflammatory roles. Int J Mol Sci. 2021;22(9):4972.
Zanos P, Brown KA, Georgiou P, Yuan P, Zarate CA Jr, Thompson SM, et al. NMDA receptor activation-dependent antidepressant-relevant behavioral and synaptic actions of ketamine. J Neurosci. 2023;43(6):1038–50.
Chen R, Capitão LP, Cowen PJ, Harmer CJ. Effect of the NMDA receptor partial agonist, d-cycloserine, on emotional processing and autobiographical memory. Psychol Med. 2021;51(15):2657–65.
d’Andrea G, Pettorruso M, Lorenzo GD, Mancusi G, McIntyre RS, Martinotti G. Rethinking ketamine and esketamine action: are they antidepressants with mood-stabilizing properties? Eur Neuropsychopharmacol. 2023;70:49–55.
Liu B, Du Y, Xu C, Liu Q, Zhang L. Antidepressant effects of repeated s-ketamine administration as NMDAR antagonist: involvement of CaMKIIα and mTOR signaling in the hippocampus of CUMS mice. Brain Res. 2023;1811:148375.
Taillefer de Laportalière T, Jullien A, Yrondi A, Cestac P, Montastruc F. Reporting of harms in clinical trials of esketamine in depression: a systematic review. Psychol Med. 2023;53(10):4305–15.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
BL, YZ, HX, HC and WW designed the study. QWsupervised the practical carrying out of the clinical trial. WY participated in the study’s conceptualization and sampling. ZY and HX analyzed the data. BL, YZ and WW wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was performed in accordance with the declaration of Helsinki. Ethical approval for this study (2021-03-031-K01) was provided by the Institutional Ethics Committee of the Affiliated Jiangning Hospital of Nanjing Medical University. The registration of this study was approved in the Chinese Clinical Trial Registry on 5/30/2022 (CTRI registration number—ChiCTR2200060387). All volunteers involved were informed of the proposal and gave their written, informed consent.
Consent for publication
Not Applicable.
Competing interests
The authors declare no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ling, B., Zhu, Y., Yan, Z. et al. Effect of single intravenous injection of esketamine on postpartum depression after labor analgesia and potential mechanisms: a randomized, double-blinded controlled trial. BMC Pharmacol Toxicol 24, 66 (2023). https://doi.org/10.1186/s40360-023-00705-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40360-023-00705-7