Abstract
Background
Pertuzumab is widely used for the treatment of HER2 + breast cancer. But its safety in the real world should be continuously monitored. So, we evaluated the safety of pertuzumab by pharmacovigilance analyze based on related adverse events (AEs) from the FDA Adverse Event Reporting System (FAERS) and find whether potential or uncertain adverse events were present.
Methods
In disproportionality analysis, four algorithms were employed to detect the signals of pertuzumab from the FAERS between 2012 and 2022. In addition, we also used MYSQL 8.0, Navicat Premium 15, and Microsoft EXCEL 2019 to analyze the potential and high-ROR (reporting odds ratio) signals of pertuzumab. We also collected the onset times of pertuzumab-associated AEs.
Results
From January 2012 to December 2022, there are 39,190,598 AEs reported from the FAERS database, of which 14,707 AEs listed pertuzumab as the ‘primary suspected (PS)’ drug. A total of 115 (46 potential) significant disproportionality preferred terms (PTs) conforming to the four algorithms were retained. Finally, we detected that the pertuzumab-induced AEs occurred in 12 organ systems. For pertuzumab, unexpected and significant PTs of AEs were found, including but not limited to below PTs: haematotoxicity, cardiotoxicity, cardiomyopathy, mitral valve incompetence, tachycardia, intestinal perforation, hemorrhoids, erysipelas, dehydration, pneumonitis, skin toxicity, onychomadesis, cyanosis, and circulatory collapse. We found there were 9 strong signals (5 potential safety signals) and 68 medium intensity signals (21 potential safety signals) according to IC025 (information component). The potential strong signals (IC025 > 3.0) were myelosuppression, cardiotoxicity, cardiac dysfunction, ejection fraction decreased, interstitial lung disease, and onychomadesis. Excluding unreported or unreasonable onset time reports, a total of 2016 AEs reported onset time and the median onset time was 117 days (4, 96), as median (Q1, Q3). Notably, most of the all AEs (n = 1133, 56%) and cardiac-related events (n = 405, 53%) all occurred within one month after pertuzumab therapy.
Conclusion
Analysis of FAERS data identified pertuzumab-associated AEs, and our findings supported continuous clinical monitoring, pharmacovigilance, and further studies of pertuzumab. A significant association was detected between pertuzumab and some potential adverse events which should be regarded with some care. We have to pay attention to the first month after pertuzumab therapy and prepare emergency measures, especially for the elderly and patients with cardiovascular diseases.
Similar content being viewed by others
Background
As early as 2020, breast cancer (BC) has become the commonly cancer in female and 10–15% of women will be possibly diagnosed with breast cancer at some time of their lifetime [1,2,3]. Noteworthily, 15-20% of patients with breast cancer overexpress the human epidermal growth factor receptor (EGFR) 2, also known as HER2, ERBB2 or CD340 [4,5,6]. Because of expensive treatments, a poor prognosis, and high recurrence rates, its burden has been rising over the past decades [5]. HER2 is different from other identified extracellular ligands (such as HER1, HER3, and HER4), because HER2 does not directly bind to any ligands [7]. It leads to that high expression of HER2 on cell surface has been used as an ideal target by different mechanisms and anti-HER2-directed agents have been developed in succession, such as trastuzumab, pertuzumab, afatinib, dacomitinib, margetuximab and antibody-drug conjugates (ADCs) [8,9,10]. However, the combination of trastuzumab, pertuzumab and taxane remains the preferred first-line therapy for HER2-positive metastatic breast cancer (MBC) in different guidelines [2, 4].
According gene expression patterns of previous studies, breast cancer is dived into five subtypes, known as the luminal A, luminal B, basal-like, HER2 overexpression, and normal breast-like subtype [11, 12]. The HER2 gene, as an actionable actuator, has advanced the development of HER-targeting monoclonal antibodies (mAbs) such as trastuzumab and pertuzumab, which resulted in the ameliorative survival time and quality of life [12,13,14]. HER2 mediates multiple signaling pathways in breast cancer and activates downstream signaling pathways to control cell growth, proliferation, differentiation, apoptosis, and metastasis [3]. Despite many conspicuous mAbs therapies developed, 15–25% of patients will still relapse in the early stage of BC and this causes treatments very difficult [15, 16].
In adverse events (AEs) of pertuzumab from the FAERS, females were accounted for a larger proportion than males which accord with the epidemiology of breast cancer. With the passage of time, FDA-approved HER2-targeted therapies has been more and more, including monoclonal antibodies (e.g., trastuzumab and pertuzumab), antibody-drug conjugates (e.g., trastuzumab emtansine), and small-molecule HER1/2 TKIs (e.g., lapatinib, neratinib, and tucatinib) [3, 17]. Additional anti-HER2 targeted treatment clinical studies are now being conducted. This significantly lessens the strain on breast cancer sufferers.
Although trastuzumab, the first HER2-targeted medication authorized by the FDA, significantly improved PFS (progression-free survival) in patients with HER2-positive breast cancer, approximately 25% patients will still relapse within the first decade after trastuzumab treatment [18]. Another randomized trial brought hope showing the addition of trastuzumab to chemotherapy could improve the survival outcomes of patients with metastatic HER2 + BC and reduce the recurrence [19]. Subsequently, a long-term follow-up study indicated that compared with two years of trastuzumab, one year of adjuvant trastuzumab after chemotherapy for HER2-positive BC improved long-term PFS significantly [15].
A report of drug reactions with HER2-Positive BC from the Italian pharmacovigilance database, showed serious AEs reports of anti-HER2 therapy mainly involved the following: thrombocytopenia, diarrhea, asthenia, cardiac failure, vomiting, hypersensitivity, ejection fraction decreased and stomatitis [20]. For the safety of trastuzumab emtansine (T-DM1) and trastuzumab deruxtecan (T-DXd), a pharmacovigilance study based on the FAERS database reported that T-DXd was more likely to induce ILD (interstitial lung disease)/pneumonia and myelosuppression than T-DM1, whereas T-DM1 had higher risk of hepatotoxicity, cardiotoxicity, and thrombocytopenia than T-DXd [21]. Compared anti-HER2 monotherapies and combination regimens, an analysis based on the FAERS showed that trastuzumab and pertuzumab/T-DM1 had higher odds of heart failure reporting than other anti-HER2 therapies [22].
Pertuzumab binds to the extracellular domain II (subdomain II) of HER2 receptor, different from the other domain of trastuzumab (subdomain IV) [23]. So, the combination of trastuzumab and pertuzumab can multiply inhibit Her2 signaling and interact with immune effector cell Fc receptors to cause antibody dependent cellular cytotoxicity (ADCC) [24]. The previous CLEOPATRA trial demonstrated that pertuzumab, combined with trastuzumab and docetaxel chemotherapy, significantly improved PFS and overall survival (OS) compared with trastuzumab and docetaxel alone [25]. Although the development of antibody drug conjugates (ADCs), ASCO (American Society of Clinical Oncology) guideline indicated that the dual HER2-targeted treatment including pertuzumab and trastuzumab, additional chemotherapy (taxane) remained the first-line standard therapy for patients with HER2 + BC [17].
Pertuzumab-related AEs (≥ Grade 3, severe adverse events, MedDRA) were reported as cardiotoxicity, diarrhea, neutropenia and left ventricular systolic dysfunction [26]. But in CLEOPATRA trial (NCT00567190), no heart failure, symptomatic left ventricular systolic dysfunction, or left ventricular ejection fraction decline (< 40%) were reported [26]. While, safety was similar in many clinical trials with no potential safety signals [26,27,28,29,30,31]. In addition, the FAERS, as a spontaneous report system, could display more information than clinical trials, like non-selective sampling.
Compared with trastuzumab and chemotherapy, additional pertuzumab for treatment of metastatic breast cancer can shorten the median OS and improved progression-free survival (PFS) obviously [30, 32]. Furthermore, there were also no significant differences for heart failure–related and febrile neutropenia–related adverse events in the first-line standard therapy [32, 33]. In a random phase III study of pertuzumab, trastuzumab, and docetaxel, no heart failure cases or symptomatic LVEF (Left ventricular ejection fraction) declines were reported [34]. Similarly, in the APHINITY study of cardiac safety of pertuzumab plus trastuzumab, the dual blockade did not increase the risk of cardiac events (CEs) compared with trastuzumab alone and the anthracycline-based chemotherapy increased the risk of a CE [35]. But in FDA label, pertuzumab can result in subclinical and clinical cardiac failure manifesting as decreased LVEF and congestive heart failure (CHF) [36]. So, there were not enough evidences to confirm the cardiotoxicity and if there were potential adverse events occurred. In this article, we use the disproportionality analysis to find the potential safety signals of pertuzumab, comprehensively.
Methods
Data sources
We collected the data of the drug (pertuzumab, Perjeta) from the FAERS from January 2012 to December 2022. The FAERS, as a spontaneous report system, its adverse events including update information were submitted by medical personnel, consumers, manufacturers and others. In addition, we removed duplicate individual safety reports with the same identifier number from demographic (DEMO) file and performed the interlink of reaction (REAC) file with the MedDRA by using PTs [37].
Data mining
We applied disproportionality analysis to evaluate the safety signals for patients with pertuzumab and its types in medical subject headings [MeSH]. We chose “pertuzumab” as the target drugs, and primary suspect drugs as the drug role code in the dataset [38]. Otherwise, we used MySQL (version 8.0) and Navicat (Navicat Premium 16.0) to establish the dataset from FAERS. The outcomes of the dataset were standardized vocabularies with drug names corresponding to the preferred terms (PTs) from Medical Dictionary for Regulatory Activities (MedDRA®) (version 24.0) and also used Excel software to compute drug-reaction signals statistically [39].
Statistical analysis
A disproportionality analysis is commonly used to analyze post-marketing surveillance databases to explore potential associations between drugs and adverse events [40, 41]. We completed the normal operation including disposal, cleaning, collecting, and calculating the signals of clinical characteristics from the dataset by MySQL (version 8.0), Microsoft EXCEL, and Navicat (Navicat Premium 16.0) [42]. Based on a fourfold table, the reporting odds ratio (ROR), the proportional reporting ratio (PRR), the Bayesian confidence propagation neural network (BCPNN), and the multi-item gamma Poisson shrinker (MGPS) were applied to detect an association between various pertuzumab regimens and adverse events in accordance with the disproportionality analysis [40, 43,44,45,46,47,48]. This method compares the proportion of a certain event of the target drug in the ADE spontaneous reporting system with the proportion of the target event of all other drugs (background data) [49]. The equations and criteria for the above four algorithms are shown in Supplementary Table S1. We will investigate the statistical association between this targeted drug and the event to detect potential AE signals. A positive signal was accord with each criterion of four algorithms. The time-to-onset of adverse events used the formula as follows:
, after we removed the reports with obvious errors such as illogical dates, such as missing data and the negative number of time-to-onset. The onset time of AEs induced by pertuzumab was calculated and shown as the percentage, expressed as “%” [50].
Results
Descriptive analysis
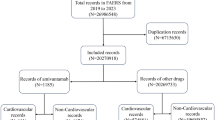
From January 2012 to December 2022, there are 39,190,598 AEs reported in the FAERS database in Fig. 1. Of which, 14,707 AEs excluded repetitive and missing data were found to be related to pertuzumab. The clinical characteristics of pertuzumab were showed in Table 1. Among all AEs, females (12,903, 87.7%) were accounted for a larger proportion than males (246, 1.7%). As the Table 1 shows, the most reported indication was breast cancer (5682, 38.6%), followed by HER-2 positive breast cancer (3238, 22.0%) and breast cancer metastatic (2159, 14.9%). In our collected data, the median age of patients was 56.4 (48, 65), as median (Q1, Q3). In outcomes of pertuzumab treatments, in addition to other serious medical events (2247, 15.3%), hospitalization-initial or prolonged (1787, 12.2%) was the most frequently reported serious outcome. Most of AEs were reported from United States (4696, 31.9%), followed by Canada (1574, 10.7%), Germany (1360, 9.2%), China (870, 5.9%), and Great Britain (839, 5.7%). Physician (7408, 50.4%) reported the most, followed by consumers (2583, 17.6%). In terms of reporting years, the most reported year was 2022 (2673, 18.2%), followed by 2021 (2615, 17.8%), 2020 (2107, 14.3%), and 2019 (1650, 11.2%), respectively.
Signal of system organ class
Based on the original data, all cases with missing doses, frequencies, or indications were excluded. The signal strength of AEs of pertuzumab at the System Organ Class (SOC) level are described in Table 2. Finally, we detected that pertuzumab- induced AEs occurred in targeting 12 organ systems. The significant SOCs of pertuzumab that at least one of the four indices accorded with the criteria were blood and lymphatic system disorders (SOC: 10005329, 848), cardiac disorders (SOC: 10007541, 645), gastrointestinal disorders (SOC: 10017947, 2104), respiratory, thoracic and mediastinal disorders (SOC: 10038738, 1088), skin and subcutaneous tissue disorders (SOC: 10040785, 1132), hepatobiliary disorders (SOC: 10019805, 171), vascular disorders (SOC: 10047065, 414), investigations (SOC: 10022891, 1067) and so on.
Signal of preferred terms
We detected suspicious signals of pertuzumab by four pharmacovigilance algorithms (ROR, PRR, BCPNN, and MGPS) and showed the results in Table 3. First, we evaluated preferred terms (PT) levels from MedDRA® to describe the toxicity spectrum of pertuzumab. In Supplementary Table S2, we further examined all PT signals and a total of 116 (46 potential PTs) PTs significant disproportionality PTs conformed to the four algorithms simultaneously. Blood system events, cardiac disorders events, gastrointestinal disorders events, and respiratory system events that are included in the label are usually reported in patients with pertuzumab.
In Table 3, we enumerated the potential and suspicious PTs signals of pertuzumab from the FAERS database. In the analysis of pertuzumab, unexpected significant AEs were found in Table 3, including but not limited to below PTs: myelosuppression (ROR 86.09; PT 10028584), haematotoxicity (ROR 3.89; PT 10061188), cardiotoxicity (ROR 35.04; PT 10048610), cardiomyopathy (ROR 6.98; PT 10007636), mitral valve incompetence (ROR 4.38; PT 10027727), tachycardia (ROR 3.33; PT 10043071), intestinal perforation (ROR 3.87; PT 10022694), hemorrhoids (ROR 3.09; PT 10019022), erysipelas (ROR 10.51; PT 10015145), carbohydrate antigen 15 − 3 increased (ROR 36.77; PT 10051415), dehydration (ROR 4.21; PT 10012174), pneumonitis (ROR 8.54; PT 10035742), onychomadesis (ROR 26.77; PT 10049274), cyanosis (ROR 4.85; PT 10011703), and circulatory collapse (ROR 3.49; PT: 10009192). If IC025 (the lower limit of 95% CI of the BCPNN) > 3.0, it indicated a strong signal and if 1.5 < IC025 ≤ 3.0, it indicated a medium intensity signal [51]. So, we found there were 9 strong signals (5 potential safety signals) and 69 medium intensity signals (22 potential safety signals). The potential strong signals (IC025 > 3.0) were myelosuppression, cardiotoxicity, cardiac dysfunction, ejection fraction decreased, interstitial lung disease, and onychomadesis.
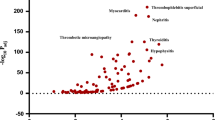
Onset time of pertuzumab-related AEs
We collected the onset times of pertuzumab-associated AEs from the FAERS database and showed the results in Fig. 2. Excluding unreported or unreasonable onset time reports such that event onset date was before therapy start date, a total of 2016 AEs reported onset time and the median onset time was 117 days (4, 96), as median (Q1, Q3). In Fig. 2, most of the AEs occurred within 1 month (n = 1133, 56%) after pertuzumab therapy. Notably, we also found that in 764 cardiac-related events, most of the AEs also occurred within 1 month (n = 405, 53%) after pertuzumab therapy.
Discussion
To the best of our knowledge, this large real-world comparison of pertuzumab used the FAERS data firstly. Our study showed that the most commonly reported and fire-potential safety signals were found at PT levels. In the SOC level, blood and lymphatic system disorders were the most commonly reported and signficant signals. In contrast, signficant disproportionality of AEs in cardiac disorders, gastrointestinal disorders, respiratory disorders, skin disorders, hepatobiliary disorders, vascular disorders, and investigations were less common.
HER2 + inhibitors such as trastuzumab and pertuzumab are not only widely used in breast cancer, but also other HER-positive diseases such as colorectal cancer, metastatic gastric cancer, biliary tract cancer, and leptomeningeal disease due to the susceptibility gene and PI3K-signaling pathway [52,53,54]. Physicians may need to exercise additional caution on blood, cardiac, and gastrointestinal system disorders while using pertuzumab. In an analysis of anti-HER2 therapy from the Italian pharmacovigilance database, cardiac failure, vascular disorder and infusion-related reactions with hypersensitivity were more frequent in the treatment of pertuzumab and trastuzumab [20]. According to the BC Cancer Agency (BCCA) drug assessment report, 13.0–40.0% of patients treated with pertuzumab have been observed infusion-related reactions, including symptoms of asthenia, chills, fatigue, and hypersensitivity [20, 55].
Pertuzumab has been often used in conjunction with other HER2-targeted drugs and chemotherapy such as trastuzumab, trastuzumab emtansine (T-DM1), atezolizumab, docetaxel, and taxane, significantly improving PFS or delaying brain metastases in patients with BC [56]. But, some therapies express some more serious AEs, studies have shown that major severe AEs of T-DM1 + pertuzumab ± taxane included thrombocytopenia, neutropenia, fatigue, increased ALT, anemia and peripheral neuropathy [57]. However, the addition of pertuzumab to T-DM1 ± taxane only led to higher risks of diarrhea (especially grade ≥ 3 diarrhea), rash and vomiting, and decreased risks of thrombocytopenia [58]. In the real-world, we found that whether it was in combination or not, pertuzumab as the primary suspect drug was detected a total of 115 (46 in potential) significant PTs signals, such as haematotoxicity, cardiotoxicity, cardiomyopathy, mitral valve incompetence, tachycardia, intestinal perforation, hemorrhoids, erysipelas, carbohydrate antigen 15 − 3 increased, dehydration, pneumonitis, skin toxicity, onychomadesis, cyanosis, and circulatory collapse. We also found there were 9 strong signals (5 potential safety signals) and 68 medium intensity signals (21 potential safety signals) in the PTs level. The potential strong signals (IC025 > 3.0) were myelosuppression, cardiotoxicity, cardiac dysfunction, ejection fraction decreased, interstitial lung disease, and onychomadesis. Noteworthily, pertuzumab currently have not a ‘boxed warning’ for an obvious risk of myelosuppression in its FDA label.
For cardiovascular events, both HER2 receptors and their ligands are expressed in cardiac cells; inhibition of these pathways may affect the ability of the heart to withstand stress and thus impact cell survival [59]. In a pharmacovigilance analysis of anti-HER2 monotherapies, trastuzumab and pertuzumab/T-DM1 (12.04%) had a higher risk of heart failure than other anti-HER2 therapies (1–2%) [22]. So, pertuzumab may had a synergistic effect with trastuzumab on cardiac disorders in older patients. In a phase IIIb single‑arm safety study (NCT02402712), safety and efficacy with subcutaneous trastuzumab plus intravenous pertuzumab and docetaxel in BC are consistent with this intravenous combination, and the most common severe events were neutropenia, febrile neutropenia, and hypertension, with no cardiac deaths and stable LVEF [31].
Gastrointestinal events also were common in our analysis. We found some unexpected signals of pertuzumab including enterocolitis, intestinal perforation, colitis, and hemorrhoids, excepting other common events such as abdominal pain, nausea, and vomiting. The substantive enteropathy may be caused by the development of cancer diseases. Some studies have suggested that blocking EGFR can cause excess chloride secretion, resulting in impaired gut absorption and secretory diarrhea [60, 61]. Additionally, compared to trastuzumab plus chemotherapy, dual anti-HER2 blockade regimens revealed an increased probability of gastrointestinal reactions [62].
It’s worth noting that we found disproportionality reporting for skin and subcutaneous tissue disorders. In addition to breast and cardiac cells, HER2 is also expressed in keratinocytes [59]. Aside from reported skin- related AEs such as palmar-plantar erythrodysaesthesia syndrome, nail disorder, and skin reaction, we found potential strong signals of pertuzumab including nail discolouration (ROR = 10.1), ermatitis acneiform (ROR = 14.9) and onychomadesis (ROR = 26.8). Interestingly, onychomadesis was not found in any study of pertuzumab. Based on our disproportionality analysis, multiple organ systems were involved and the strongest signal was blood and lymphatic system (IC025 = 1.71, it indicated a medium intensity signal), follow by cardiac disorders, gastrointestinal disorders, respiratory, thoracic disorders, skin disorders, and hepatobiliary disorders.
In Supplementary Table S2, Metastases to central nervous system (ROR = 30.93) also showed a strong signal. According to statistics, approximately one-third of patients with HER2 + breast cancer will finally transfer to CNS (central nervous system) [63]. Despite this high incidence of CNS metastases, compared to other subtypes, patients with HER2-positive MBC achieve a better survival rate because of better systemic and cranial disease control provided by anti-HER2 agents [64,65,66]. Additionally, the phase I/II study showed that the outcomes of HER-positive leptomeningeal disease patients treated with intrathecal trastuzumab remained safe and well-tolerated [64]. To symptomatic brain metastases, the treatments including neurosurgery and/or radiotherapy are more depending on the number of metastases, performance status, and systemic disease control [4].
Results of this study indicated that the median onset time was 117 days (4, 96), as median (Q1, Q3) and most of the cases occurred within the first month (n = 1133, 56%) after pertuzumab. So, we have to pay attention to the first month after pertuzumab and take emergency measures, especially the elderly and patients with cardiovascular diseases.
In our study, we also have some limitations in the FAERS. Unfortunately, because the causal relationship for submitted reports and some information are lacking, such as underreporting, incomplete reporting, and false reporting, it is difficult to control confounding factors [67]. Second, because of the lack of total number of patients with pertuzumab treatment and the same event reported by two sources (physician and consumer) resulting in two IDs potentially, it is impossible to calculate relevant statistics such as the adverse reaction ratio. Third, because of a lack of information, the important risk factors of pertuzumab have become challenging to deal with. So, while data mining cannot compensate for the inherent limitations of self-reporting systems or replace expert review, it does have a place when large amounts of data are involved [68].
Although pertuzumab has some AEs, double anti-HER2 blockade associated with a taxane currently remains the best option in the first line. The standard of care was dual blockade with trastuzumab and pertuzumab as first-line, followed by TDM-1 as second-line [23]. With the development of related clinic trials, more effective and more safe therapeutic regimens will be brought to the patient with HER2+/- breast cancer.
Conclusion
In conclusion, this is the first study to analyze pertuzumab from FAERS data comprehensively and systematically. It is very important for continuous monitoring of drug safety profiles in the real-world. For pertuzumab, unexpected and 46 potential significant PTs of AEs were found, such as cardiotoxicity, cardiomyopathy, mitral valve incompetence, cyanosis, lymphoedema, circulatory collapse, intestinal perforation, polyneuropathy, onychomadesis, interstitial lung diseases, tachycardia, and so on. In the onset times of all AEs and cardiovascular events, we must pay attention to the first month after pertuzumab.
Availability of data and materials
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADCC:
-
Antibody dependent cellular cytotoxicity
- ADCs:
-
Antibody-drug conjugates
- AEs:
-
Adverse events
- ASCO:
-
American Society of Clinical Oncology
- BC:
-
Breast cancer
- BCPNN:
-
Bayesian confidence propagation neural network
- CEs:
-
Cardiac events
- CHF:
-
Congestive heart failure
- CNS:
-
central nervous system
- DEMO:
-
Demographic
- DFS:
-
Disease-free survival
- EGFR:
-
Epidermal growth factor receptor
- FDA:
-
U.S. Food and Drug Administration
- FAERS:
-
FDA Adverse Event Reporting System
- HER2:
-
human epidermal growth factor receptor 2
- IC:
-
Information component
- IC025:
-
The lower limit of 95% confidence interval of the IC
- ILD:
-
Interstitial Lung Disease
- LVEF:
-
Left ventricular ejection fraction
- mAbs:
-
Monoclonal antibodies
- MBC:
-
Metastatic breast cancer
- MedDRA:
-
Medical Dictionary for Regulatory Activities
- MGPS:
-
Multi-item gamma Poisson shrinker
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- PRR:
-
Proportional reporting ratio
- PS:
-
Primary suspected
- PTs:
-
Preferred terms
- REAC:
-
Reaction
- ROR:
-
Reporting odds ratio
- T-DM1:
-
Trastuzumab emtansine
- T-DXd:
-
Trastuzumab deruxtecan
References
Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS, Bilous M, Ellis IO, Fitzgibbons P, Hanna W, et al. Human epidermal growth factor receptor 2 testing in breast cancer: american society of clinical oncology/college of american pathologists clinical practice guideline focused update. J Clin Oncol. 2018;36(20):2105–22.
Vega Cano KS, Marmolejo Castañeda DH, Escrivá-de-Romaní S, Saura C. Systemic therapy for HER2-positive metastatic breast cancer: current and future trends. Cancers. 2022;15(1):51.
Arnold M, Morgan E, Rumgay H, Mafra A, Singh D, Laversanne M, Vignat J, Gralow JR, Cardoso F, Siesling S, et al. Current and future burden of breast cancer: global statistics for 2020 and 2040. Breast (Edinburgh Scotland). 2022;66:15–23.
Nader-Marta G, Martins-Branco D, de Azambuja E. How we treat patients with metastatic HER2-positive breast cancer. ESMO open. 2022;7(1):100343.
Yamamoto Y, Iwata H, Taira N, Masuda N, Takahashi M, Yoshinami T, Ueno T, Toyama T, Yamanaka T, Takano T, et al. Pertuzumab retreatment for HER2-positive advanced breast cancer: a randomized, open-label phase III study (PRECIOUS). Cancer Sci. 2022;113(9):3169–79.
Rizzo A, Cusmai A, Acquafredda S, Giovannelli F, Rinaldi L, Misino A, Palmiotti G. KEYNOTE-522, IMpassion031 and GeparNUEVO: changing the paradigm of neoadjuvant immune checkpoint inhibitors in early triple-negative breast cancer. Future Oncol (London England). 2022;18(18):2301–9.
Yarden Y, Sliwkowski MX. Untangling the ErbB signalling network. Nat Rev Mol Cell Biol. 2001;2(2):127–37.
Rassy E, Rached L, Pistilli B. Antibody drug conjugates targeting HER2: clinical development in metastatic breast cancer. Breast (Edinburgh Scotland). 2022;66:217–26.
Ferrando-Díez A, Felip E, Pous A, Bergamino Sirven M, Margelí M. Targeted therapeutic options and future perspectives for HER2-Positive Breast Cancer. Cancers. 2022;14(14):3305.
Rugo HS, Im SA, Cardoso F, Cortés J, Curigliano G, Musolino A, Pegram MD, Wright GS, Saura C, Escrivá-de-Romaní S, et al. Efficacy of margetuximab vs trastuzumab in patients with pretreated erbb2-positive advanced breast cancer: a phase 3 randomized clinical trial. JAMA Oncol. 2021;7(4):573–84.
Perou CM, Sørlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, Pollack JR, Ross DT, Johnsen H, Akslen LA, et al. Molecular portraits of human breast tumours. Nature. 2000;406(6797):747–52.
Sørlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, Hastie T, Eisen MB, van de Rijn M, Jeffrey SS, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA. 2001;98(19):10869–74.
Bartsch R, Berghoff AS, Furtner J, Marhold M, Bergen ES, Roider-Schur S, Starzer AM, Forstner H, Rottenmanner B, Dieckmann K, et al. Trastuzumab deruxtecan in HER2-positive Breast cancer with brain metastases: a single-arm, phase 2 trial. Nat Med. 2022;28(9):1840–7.
Sorlie T, Tibshirani R, Parker J, Hastie T, Marron JS, Nobel A, Deng S, Johnsen H, Pesich R, Geisler S, et al. Repeated observation of breast tumor subtypes in Independent gene expression data sets. Proc Natl Acad Sci USA. 2003;100(14):8418–23.
Cameron D, Piccart-Gebhart MJ, Gelber RD, Procter M, Goldhirsch A, de Azambuja E, Castro G Jr, Untch M, Smith I, Gianni L, et al. 11 years’ follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive early Breast cancer: final analysis of the HERceptin adjuvant (HERA) trial. Lancet (London England). 2017;389(10075):1195–205.
Garcia-Murillas I, Schiavon G, Weigelt B, Ng C, Hrebien S, Cutts RJ, Cheang M, Osin P, Nerurkar A, Kozarewa I, et al. Mutation tracking in circulating Tumor DNA predicts relapse in early Breast cancer. Sci Transl Med. 2015;7(302):302ra133.
Korde LA, Somerfield MR, Carey LA, Crews JR, Denduluri N, Hwang ES, Khan SA, Loibl S, Morris EA, Perez A, et al. Neoadjuvant chemotherapy, endocrine therapy, and targeted therapy for breast cancer: ASCO guideline. J Clin Oncol. 2021;39(13):1485–505.
Slamon D, Eiermann W, Robert N, Pienkowski T, Martin M, Press M, Mackey J, Glaspy J, Chan A, Pawlicki M, et al. Adjuvant trastuzumab in HER2-positive breast cancer. N Engl J Med. 2011;365(14):1273–83.
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, Fleming T, Eiermann W, Wolter J, Pegram M, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344(11):783–92.
Barbieri MA, Sorbara EE, Cicala G, Santoro V, Cutroneo PM, Franchina T, Spina E. Adverse drug reactions with HER2-positive breast cancer treatment: an analysis from the italian pharmacovigilance database. Drugs - real World Outcomes. 2022;9(1):91–107.
Ma P, Tian H, Shi Q, Liu R, Zhang Y, Qi X, Chen Y. High risks adverse events associated with trastuzumab emtansine and trastuzumab deruxtecan for the treatment of HER2-positive/mutated malignancies: a pharmacovigilance study based on the FAERS database. Exp Opin Drug Saf. 2023;22(8):685–96.
Waliany S, Caswell-Jin J, Riaz F, Myall N, Zhu H, Witteles RM, Neal JW. Pharmacovigilance analysis of heart failure associated with Anti-HER2 monotherapies and combination regimens for cancer. JACC CardioOncology. 2023;5(1):85–98.
Swain SM, Baselga J, Kim SB, Ro J, Semiglazov V, Campone M, Ciruelos E, Ferrero JM, Schneeweiss A, Heeson S, et al. Pertuzumab, trastuzumab, and docetaxel in HER2-positive metastatic breast cancer. N Engl J Med. 2015;372(8):724–34.
Deng W, Liu J, Pan H, Li L, Zhou C, Wang X, Shu R, Dong B, Cao D, Li Q, et al. A bispecific antibody based on pertuzumab fab has potent antitumor activity. J Immunotherapy (Hagerstown Md: 1997). 2018;41(1):1–8.
Baselga J, Cortés J, Kim SB, Im SA, Hegg R, Im YH, Roman L, Pedrini JL, Pienkowski T, Knott A, et al. Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. N Engl J Med. 2012;366(2):109–19.
Xu B, Li W, Zhang Q, Li Q, Wang X, Li H, Sun T, Yin Y, Zheng H, Feng J, et al. Pertuzumab, trastuzumab, and docetaxel for Chinese patients with previously untreated HER2-positive locally recurrent or metastatic breast cancer (PUFFIN): final analysis of a phase III, randomized, double-blind, placebo-controlled study. Breast Cancer Res Treat. 2023;197(3):503–13.
Xie XF, Zhang QY, Huang JY, Chen LP, Lan XF, Bai X, Song L, Xiong SL, Guo SJ, Du CW. Pyrotinib combined with trastuzumab and chemotherapy for the treatment of human epidermal growth factor receptor 2-positive metastatic Breast cancer: a single-arm exploratory phase II trial. Breast Cancer Res Treat. 2023;197(1):93–101.
Lavasani SM, Somlo G, Yost SE, Frankel PH, Ruel C, Cui Y, Murga M, Tang A, Martinez N, Kruper L, et al. Phase 2 prospective open label study of neoadjuvant nab-paclitaxel, trastuzumab, and pertuzumab in patients with HER2-positive primary Breast cancer. Cancer. 2023;129(5):740–9.
Mazieres J, Lafitte C, Ricordel C, Greillier L, Negre E, Zalcman G, Domblides C, Madelaine J, Bennouna J, Mascaux C, et al. Combination of Trastuzumab, Pertuzumab, and Docetaxel in patients with Advanced Non-small-cell Lung Cancer harboring HER2 mutations: results from the IFCT-1703 R2D2 trial. J Clin Oncology: Official J Am Soc Clin Oncol. 2022;40(7):719–28.
Ahn HK, Sim SH, Suh KJ, Kim MH, Jeong JH, Kim JY, Lee DW, Ahn JH, Chae H, Lee KH, et al. Response rate and safety of a neoadjuvant Pertuzumab, Atezolizumab, Docetaxel, and Trastuzumab Regimen for patients with ERBB2-Positive stage II/III Breast Cancer: the Neo-PATH phase 2 Nonrandomized Clinical Trial. JAMA Oncol. 2022;8(9):1271–7.
Kuemmel S, Tondini CA, Abraham J, Nowecki Z, Itrych B, Hitre E, Karaszewska B, Juárez-Ramiro A, Morales-Vásquez F, Pérez-García JM, et al. Subcutaneous trastuzumab with pertuzumab and docetaxel in HER2-positive metastatic Breast cancer: final analysis of MetaPHER, a phase IIIb single-arm safety study. Breast Cancer Res Treat. 2021;187(2):467–76.
Dai WF, Beca JM, Nagamuthu C, Liu N, de Oliveira C, Earle CC, Trudeau M, Mercer RE, Chan KKW. Comparative effectiveness and safety of pertuzumab and trastuzumab plus chemotherapy vs trastuzumab plus chemotherapy for treatment of metastatic breast cancer. JAMA Netw open. 2022;5(2):e2145460.
Bachelot T, Ciruelos E, Schneeweiss A, Puglisi F, Peretz-Yablonski T, Bondarenko I, Paluch-Shimon S, Wardley A, Merot JL, du Toit Y, et al. Preliminary safety and efficacy of first-line pertuzumab combined with trastuzumab and taxane therapy for HER2-positive locally recurrent or metastatic Breast cancer (PERUSE). Anna Oncol. 2019;30(5):766–73.
Xu B, Li W, Zhang Q, Shao Z, Li Q, Wang X, Li H, Sun T, Yin Y, Zheng H, et al. Pertuzumab, trastuzumab, and docetaxel for Chinese patients with previously untreated HER2-positive locally recurrent or metastatic Breast cancer (PUFFIN): a phase III, randomized, double-blind, placebo-controlled study. Breast Cancer Res Treat. 2020;182(3):689–97.
de Azambuja E, Agostinetto E, Procter M, Eiger D, Pondé N, Guillaume S, Parlier D, Lambertini M, Desmet A, Caballero C, et al. Cardiac safety of dual anti-HER2 blockade with pertuzumab plus trastuzumab in early HER2-positive Breast cancer in the APHINITY trial. ESMO open. 2023;8(1):100772.
Swain SM, Ewer MS, Viale G, Delaloge S, Ferrero JM, Verrill M, Colomer R, Vieira C, Werner TL, Douthwaite H, et al. Pertuzumab, trastuzumab, and standard anthracycline- and taxane-based chemotherapy for the neoadjuvant treatment of patients with HER2-positive localized Breast cancer (BERENICE): a phase II, open-label, multicenter, multinational cardiac safety study. Ann Oncol. 2018;29(3):646–53.
FDA adverse event reporting system (FAERS). Available at: https://fis.fda.gov/extensions/FPD-QDE-FAERS/FPD-QDE-FAERS.html.
Peng J, Wang H, Liu Z, Xu ZL, Wang MX, Chen QM, Wu ML, Ren XL, Liang QH, Liu FP, et al. Real-world study of antiresorptive-related osteonecrosis of jaw based on the US food and drug administration adverse event reporting system database. Front Pharmacol. 2022;13:1017391.
Chen J, Wen Y, Chu X, Liu Y, Su C. Pulmonary adverse events associated with Hypertension in non-small cell Lung cancer patients receiving PD-1/PD-L1 inhibitors. Front Pharmacol. 2022;13:944342.
Jiang JJ, Zhao B, Li J. Does eltrombopag lead to thrombotic events? A pharmacovigilance study of the FDA adverse event reporting system. J Clin Pharm Ther. 2022;47(10):1556–62.
Zhang M, Li H, Huang L, Liu Y, Jiao XF, Zeng L, Jia ZJ, Cheng G, Zhang L, Zhang W. Drug-associated kidney injury in children: a disproportionality analysis of the FDA adverse event reporting system. Eur J Pediatrics. 2023;182(10):4655–61.
Shu Y, He X, Wu P, Liu Y, Ding Y, Zhang Q. Gastrointestinal adverse events associated with semaglutide: a pharmacovigilance study based on FDA adverse event reporting system. Front Public Health. 2022;10:996179.
Guo M, Shu Y, Chen G, Li J, Li F. A real-world pharmacovigilance study of FDA adverse event reporting system (FAERS) events for niraparib. Sci Rep. 2022;12(1):20601.
Hauben M. A brief primer on automated signal detection. Ann Pharmacother. 2003;37(7–8):1117–23.
Hauben M, Madigan D, Gerrits CM, Walsh L, Van Puijenbroek EP. The role of data mining in pharmacovigilance. Exp Opin Drug Saf. 2005;4(5):929–48.
Norén GN, Bate A, Orre R, Edwards IR. Extending the methods used to screen the WHO drug safety database towards analysis of complex associations and improved accuracy for rare events. Stat Med. 2006;25(21):3740–57.
Sundström A, Hallberg P. Data mining in pharmacovigilance–detecting the unexpected: the role of index of suspicion of the reporter. Drug Saf. 2009;32(5):419–27.
Szarfman A, Machado SG, O’Neill RT. Use of screening algorithms and computer systems to efficiently signal higher-than-expected combinations of Drugs and events in the US FDA’s spontaneous reports database. Drug Saf. 2002;25(6):381–92.
Wang S, Guo M, Zhang X, Fan P, Jin Z. PARP inhibitor-related haemorrhages: what does the real-world study say? Front Oncol. 2023;13:1070343.
Cazzola M, Ora J, Cavalli F, Rogliani P, Matera MG. An overview of the Safety and Efficacy of Monoclonal antibodies for the Chronic Obstructive Pulmonary Disease. Biologics. 2021;15:363–74.
Li Sun SS, Wang T, Li J. aJL: parallel ADR detection based on spark and BCPNN. Tsinghua Sci Technol. 2019;24(2):195–206.
Gupta R, Meric-Bernstam F, Rothe M, Garrett-Mayer E, Mangat PK, D’Andre S, Ahn ER, O’Lone R, Halabi S, Grantham GN, et al. Pertuzumab Plus Trastuzumab in patients with Colorectal Cancer with ERBB2 amplification or ERBB2/3 mutations: results from the TAPUR Study. JCO Precis Oncol. 2022;6:e2200306.
Javle M, Borad MJ, Azad NS, Kurzrock R, Abou-Alfa GK, George B, Hainsworth J, Meric-Bernstam F, Swanton C, Sweeney CJ, et al. Pertuzumab and trastuzumab for HER2-positive, metastatic biliary tract cancer (MyPathway): a multicentre, open-label, phase 2a, multiple basket study. Lancet Oncol. 2021;22(9):1290–300.
Sartore-Bianchi A, Lonardi S, Martino C, Fenocchio E, Tosi F, Ghezzi S, Leone F, Bergamo F, Zagonel V, Ciardiello F, et al. Pertuzumab and trastuzumab emtansine in patients with HER2-amplified metastatic Colorectal cancer: the phase II HERACLES-B trial. ESMO open. 2020;5(5): e000911.
Alhussein MM, Mokbel A, Cosman T, Aghel N, Yang EH, Mukherjee SD, Dent S, Ellis PM, Dhesy-Thind S, Leong DP. Pertuzumab cardiotoxicity in patients with HER2-positive cancer: a systematic review and meta-analysis. CJC open. 2021;3(11):1372–82.
Garcia-Alvarez A, Papakonstantinou A, Oliveira M. Brain metastases in HER2-positive breast cancer: current and novel treatment strategies. Cancers. 2021;13(12):2927.
Banys-Paluchowski M, Krawczyk N, Stickeler E, Muller V, Fehm T. New treatment strategies for human epidermal growth factor receptor 2-positive Breast cancer in 2023. Curr Opin Obstet Gynecol. 2023;35(1):54–61.
Zhang J, Li J, Zhu C, Song Y, Xia F, Ma X. Safety and efficacy of the addition of pertuzumab to T-DM1 ± taxane in patients with HER2-positive, locally advanced or metastatic Breast cancer: a pooled analysis. Drug Des Devel Ther. 2017;11:3235–44.
Gao J, Swain SM. Pertuzumab for the treatment of breast cancer: a safety review. Exp Opin Drug Saf. 2016;15(6):853–63.
Dang C, Iyengar N, Datko F, D’Andrea G, Theodoulou M, Dickler M, Goldfarb S, Lake D, Fasano J, Fornier M, et al. Phase II study of paclitaxel given once per week along with trastuzumab and pertuzumab in patients with human epidermal growth factor receptor 2-positive metastatic Breast cancer. J Clin Oncol. 2015;33(5):442–7.
Robert NJ, Goertz HP, Chopra P, Jiao X, Yoo B, Patt D, Antao V. HER2-Positive metastatic Breast Cancer patients receiving Pertuzumab in a community oncology practice setting: treatment patterns and outcomes. Drugs - real World Outcomes. 2017;4(1):1–7.
Li X, Yao L, Wang M, Wang M, Li X, Yu X, Guo J, Dong H, Sun X, Xu Y. Updated bayesian network Meta-analysis of adjuvant targeted treatment regimens for early human epidermal growth factor Receptor-2 positive Breast Cancer. J Breast Cancer. 2020;23(4):410–29.
Le Rhun E, Guckenberger M, Smits M, Dummer R, Bachelot T, Sahm F, Galldiks N, de Azambuja E, Berghoff AS, Metellus P, et al. EANO-ESMO clinical practice guidelines for diagnosis, treatment and follow-up of patients with brain Metastasis from solid tumours. Ann Oncol. 2021;32(11):1332–47.
Kumthekar PU, Avram MJ, Lassman AB, Lin NU, Lee E, Grimm SA, Schwartz M, Bell Burdett KL, Lukas RV, Dixit K, et al. A phase I/II study of intrathecal trastuzumab in human epidermal growth factor receptor 2-positive (HER2-positive) cancer with leptomeningeal metastases: safety, efficacy, and cerebrospinal fluid pharmacokinetics. Neurooncology. 2023;25(3):557–65.
Lin NU, Murthy RK, Abramson V, Anders C, Bachelot T, Bedard PL, Borges V, Cameron D, Carey LA, Chien AJ, et al. Tucatinib vs Placebo, both in Combination with Trastuzumab and Capecitabine, for previously treated ERBB2 (HER2)-Positive metastatic Breast Cancer in patients with brain metastases: updated exploratory analysis of the HER2CLIMB Randomized Clinical Trial. JAMA Oncol. 2023;9(2):197–205.
Cavalieri S, Nuzzolese I, Ottini A, Bergamini C, Resteghini C, Colombo E, Alfieri S, Quattrone P, Calareso G, Iacovelli NA, et al. HER2 status in recurrent/metastatic androgen receptor overexpressing salivary gland carcinoma patients. Front Oncol. 2022;12:1096068.
Tezuka T, Okuzumi S, Nakashima C, Ide T, Imai S, Mitsuboshi S, Kuwahara Y, Takizawa T, Seki M, Minematsu N, et al. Dysautonomia associated with immune checkpoint inhibitors. J Neurol. 2023;270(7):3413–23.
Shi X, Cheng Q, Zhao YZ, Zou SP, Sun MH. A real-world pharmacovigilance study of abaloparatide based on the FDA adverse event reporting System (FAERS). Osteoporos Int. 2023. https://doi.org/10.1007/s00198-023-06877-6.
Acknowledgements
None.
Funding
No funding was used for this submission.
Author information
Authors and Affiliations
Contributions
MS designed the manuscript. SZ and HY extracted the data and conducted the analysis. The data re-checking, statistical analysis, and revising were performed by MO, XS, and QC. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. This study was deemed non-human subject related research.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zou, Sp., Yang, Hy., Ouyang, Ml. et al. A disproportionality analysis of adverse events associated to pertuzumab in the FDA Adverse Event Reporting System (FAERS). BMC Pharmacol Toxicol 24, 62 (2023). https://doi.org/10.1186/s40360-023-00702-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40360-023-00702-w