Abstract
Background
Network modeling has been proposed as an effective approach to examine complex associations among antecedents, mediators and symptoms. This study aimed to investigate whether the severity of depressive symptoms affects the multivariate relationships among symptoms and mediating factors over a 2-year longitudinal follow-up.
Methods
We recruited a school-based cohort of 1480 primary and secondary school students over four semesters from January 2020 to December 2021. The participants (n = 1145) were assessed at four time points (ages 10–13 years old at baseline). Based on a cut-off score of 5 on the 9-item Patient Health Questionnaire at each time point, the participants were categorized into the non-depressive symptom (NDS) and depressive symptom (DS) groups. We conducted network analysis to investigate the symptom-to-symptom influences in these two groups over time.
Results
The global network metrics did not differ statistically between the NDS and DS groups at four time points. However, network connection strength varied with symptom severity. The edge weights between learning anxiety and social anxiety were prominently in the NDS group over time. The central factors for NDS and DS were oversensitivity and impulsivity (3 out of 4 time points), respectively. Moreover, both node strength and closeness were stable over time in both groups.
Conclusions
Our study suggests that interrelationships among symptoms and contributing factors are generally stable in adolescents, but a higher severity of depressive symptoms may lead to increased stability in these relationships.
Similar content being viewed by others
Background
Depression in adolescents is a serious public health concern [1, 2] that is associated with various negative outcomes, such as loss of productivity, psychosocial dysfunction and suicide, contributing to a substantial burden of disability [3]. Additionally, depression in early life has long-lasting impacts, including increased risks for adulthood depression, anxiety and substance abuse, as well as worse health status [4, 5]. Increasing evidence suggests that depressive disorder is a continuum with features of emotional distress, including low mood, irritability, impulsivity, helplessness and other symptoms [6, 7]. Similar to clinically diagnosed depression, depressive symptoms (DSs) in adolescents are linked to social functioning problems, impaired educational attainment and poor outcomes in adulthood [8, 9]. Despite the frequent occurrence and significant consequences of depressive symptoms, symptoms are often overlooked by families, teachers and clinicians [10, 11]. China has initiated a national program to screen for depression in school-going children [12], highlighting the global importance of understanding the features that contribute to the persistence of DSs in adolescents and their later evolution into a depressive disorder.
Depression and anxiety symptoms are highly interconnected from early childhood through mid-adolescence [13]. In addition, childhood anxiety is associated with the childhood-persistent trajectory of DSs [5]. Moreover, several aspects of anxiety in childhood, such as physiological reactivity, worry/oversensitivity, social anxiety and alienation, can influence mental health outcomes in adolescence in the presence of a depressive burden [14, 15]. Furthermore, contextual factors, such as a lack of friendships and poor home (family) environment [16], and behavioral factors, such as impulsivity [17], loss of temper [18] and low help-seeking behaviors [19], are significant in predicting persistent depression in adolescents. Taken together, these results show that the consolidation effect of DSs to a syndrome needing intervention depends on the various contextual and behavioral factors described above, as well as the emergence of comorbidities, especially anxiety.
Current study
Symptom network studies offer a systems perspective of phenomenological features and allow us to probe how contextual and behavioral factors relate to a system [20]. While network analysis has been applied to depressive burden and anxiety symptoms in a cross-sectional manner in previous studies [13, 21,22,23], this approach has not been used to study the longitudinal trajectory of DSs among adolescents to date. Longitudinal sampling in an untreated community-based sample will allow us to examine how the relationship among depression, anxiety and contextual and behavioral factors affecting mental health operates over time in adolescents. One promising aspect of the network approach is that it can gain insight into intervention strategies by identifying the central symptoms that contribute to most of the complex interactions; these symptoms tend to carry a higher overall importance than other symptoms in a network [13, 22].
In the present study, we investigated DSs and related factors (comorbid anxiety, contextual and behavioral factors) at the network level among adolescent students over 4 time points with a 2-year longitudinal cohort design. We hypothesized that the interrelationship among anxiety symptoms, contextual factors and behavioral factors indicating symptom persistence would be stronger in adolescents with DSs than in those with non-depressive symptoms (NDSs). We also anticipated that the consolidating effect of depression on behavioral factors and anxiety would be seen across multiple time points in a school-based cohort during a time of macrosystem disruption (SARS-CoV-2 pandemic phase, 2020-21). On the other hand, adolescents without notable depressive symptoms could still experience anxiety-related symptoms but would not show a consolidation effect involving contextual and behavioral factors.
Methods
Study sample
Data were collected from primary and secondary school students through a school-level survey administered at the beginning of every spring and fall semester from January 2020 to December 2021. In this study, entire cohorts of 4th, 5th, 6th and 7th grade students aged 10–13 years were recruited for the initial assessment. The total sample included 1480 participants. We collected data across four time points, including t1 (baseline), t2, t3 and t4. The interval between the two assessments was half a year. Informed parental consent was required before adolescents could be invited to participate. This study was carried out in accordance with the Declaration of Helsinki and was approved by the local research ethics committee.
Measures
The survey was administered by the study team and trained teachers during school hours in a computer room. Demographic information, including age, sex and grade, was recorded. The 9-item Patient Health Questionnaire (PHQ-9) was used to measure the presence and severity of depressive symptomatology [24]. A score of more than or equal to 5 indicated that a participant had DSs [25]. In this study, participants with a PHQ-9 score below 5 at baseline and each follow-up were included in the NDS group, and those with a score equal to or above 5 were included in the DS group.
The Mental Health Test (MHT) was used to assess general anxiety on 8 dimensions, including learning anxiety, social anxiety, loneliness, self-blaming tendencies, oversensitivity, somatic anxiety, phobia anxiety and impulsive tendencies [26]. A score of greater than 8 on any subscale or a total score of more than 56 is considered to indicate high risk of psychological problems. In addition, it was included six additional questions regarding the following to capture factors that affect depressive burden in this age group: family environment, friendship, help-seeking behaviors, loss of temper, hopelessness, and lying. The questions were rated on a five-point scale, and the two items for hopelessness and lying were reverse scored (see online Supplementary Information for details). Participants (n = 1145) who completed the self-report scales at all four time points were included in the analysis. The data screening flowchart is shown in Supplementary Fig. S1.
Statistical analysis
The chi-square test was used to compare sex and DS frequency over time, and the Wilcoxon rank sum t test was used to compare scale scores between the NDS and DS groups. The Kruskal‒Wallis test was applied to compare scale scores between time points in each group. A probability level of p <.05 was considered statistically significant. Effect size was calculated using Cohen’s d. The Jaccard similarity coefficient, a measure of the similarities between sample sets [27], was calculated for each group across the four time points.
Network construction
All analyses were conducted using R (Version 4.1.3) [28]. A Gaussian graphical model (GGM) [29] was used to fit the data to understand conditional dependency relationships between variables. Based on different feature dimensions, including depressive symptom levels (PHQ-9 as a single score, given its one-factor fit in Chinese adolescents [30]), mediating factors and anxiety features, networks were constructed using 14 nodes [PHQ-9 score, Learning anxiety (Learn), Social anxiety (Soc), Loneliness (Lon), Self-blaming (Blame), Worry and Oversensitivity (Sen), Somatic anxiety (Som), Phobia (Pho), Impulsivity (Imp), Family environment (FE), Friendship (FS), Loss of temper (LT), Hopelessness (HL), and Help-seeking behavior (HS)] for the two groups at each time point. The edge weights of the GGM were computed by partial correlations. Gaussian Markov random fields were applied to learn the graphical structure, and graphical LASSO [31] and the extended Bayesian information criterion (EBIC) model [32] were used to select the optimal regularization parameter. For the EBIC model, the tuning hyperparameter (γ) was set to 0.5, which yields accurate network estimations [33]. The network layouts were computed and derived from the Fruchterman–Reingold algorithm [34].
Network analysis
Global network metrics
Global network metrics consisting of the network density, global strength, average clustering coefficient and characteristic path length were calculated using the ‘qgraph’ [35] and ‘igraph’ [36]. The network density was the ratio of the number of edges to the number of all possible edges, and global strength was defined as the weighted absolute sum of all edges in a given network [37]. The clustering coefficient was defined as the probability that the adjacent nodes of a node were connected in a graph, and characteristic path length was the average shortest path length between all pairs of nodes in the network. In network comparisons, the R package ‘NetworkToolbox’ [38] was used to investigate the differences in the network density, average clustering coefficient and characteristic path length between networks. The ‘Network Comparison Test (NCT)’ [39] was applied to compare the invariance of global strength between networks using a resampling-based permutation test and randomly repeated 1000 times.
Local network metrics
Given that previous research suggested that betweenness and closeness centrality seem unsuitable as measures of node importance for psychological networks [40, 41], in this study, node strength was calculated for the centrality index. In the ‘qgraph’ procedure [35], the node strength was defined as the sum of z scores of absolute weights connected to the central node. Additionally, the NCT [39] was used to compare the invariance of the network structure and node strength among the networks. If the network structure exhibited significant differences, the specific edges were calculated and identified.
Network accuracy and stability
The accuracy and stability of the network were estimated using the ‘bootnet’ [42]. For the nonparametric bootstrapped networks, 1000 iterations were run to estimate 95% confidence intervals (CIs) for the accuracy of edge weights, and the case-dropping subset bootstrapping networks were calculated to investigate the order stability of node centrality indices. In addition, the correlation stability coefficient (CS-coefficient) was calculated to measure the stability of node centrality indices [42]. The correlation between the original centrality indices based on the full data was compared to the correlation obtained from the subset of data representing different percentages of the overall sample. The CS-coefficient should be above 0.25 and, preferably, above 0.5. Finally, bootstrapped difference tests were performed on edge weights and centrality indices to test whether they differed significantly from each other.
Results
Sample characteristics
Among the 1480 eligible students, 1145 participants (585 [51.1%] girls) had valid data at the four time points, including 277 4th grade students (24.2%; average age 10 years), 242 5th grade students (21.1%; average age 11 years), 258 6th grade students (22.5%; average age 12 years) and 368 7th grade students (32.1%; average age 13 years). At the four time points, the percentages of PHQ-9 scores equal to or above 5 were 27.9%, 27.9%, 32.2% and 31.2%, respectively. There were no significant changes in DS frequency over time (p =.05). The total and subscale scores of the MHT were significantly lower in the NDS group than in the DS group over time (Table 1). No significant differences were found in the PHQ-9 scores between t1 and every follow-up in any group (Supplementary Table S1). Supplementary Fig. S2 illustrates the heatmap of the Pearson correlation matrix among all fourteen variables across the entire sample. The Jaccard similarity coefficient was 0.20 and 0.53 in the DS and NDS groups, respectively, at all four time points.
Global network metrics
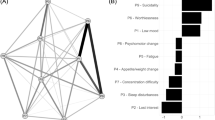
The resulting network was well connected, with no isolated nodes (Fig. 1). There were no significant differences in the global network metrics between the NDS and DS groups at the four time points (Table 2), except for a trend of higher global strength in the DS group than the NDS group at t2 and t3 (p =.05). This indicates that the presence of a higher DS burden does not alter the overall risk-symptom relationship per se.
Estimated network structures. (A) The non-depressive symptom (NDS) group at t1 (baseline). (B) The depressive symptom (DS) group at t1 (baseline). (C) The NDS group at t2. (D) The DS group at t2. (E) The NDS group at t3. (F) The DS group at t3. (G) The NDS group at t4. (H) The DS group at t4. The names of the nodes (‘Learn’, ‘Soc’, ‘Lon’, ‘Blame’, ‘Sen’, ‘Som’, ‘Pho’, ‘Imp’, ‘FE’, ‘FS’, ‘LT’, ‘HL’, ‘HS’ and ‘PHQ-9’) were ‘Learning anxiety’, ‘Social anxiety’, ‘Loneliness’, ‘Self-blaming’, ‘Oversensitivity’, ‘Somatic anxiety’, ‘Phobia’, ‘Impulsivity’, ‘Family environment’, ‘Friendship’, ‘Loss of temper’, ‘Hopelessness’, ‘Help-seeking’ and ‘PHQ-9 score’. MHT, mental health testing. PHQ-9, the 9-item Patient Health Questionnaire. Red dashed edges indicate negative weights, and blue edges indicate positive weights
Local network metrics
The top three positive edge weights for the NDS group were almost the same over time and comprised edges between learning anxiety and social anxiety, between somatic anxiety and phobia, and between self-blaming and oversensitivity (at t1, t2 and t3). The link between social anxiety and self-blaming was also prominent at t4 in the NDS group. The top three positive edge weights for the DS group differed over time and included edges between impulsivity and loss of temper, between the PHQ-9 score and hopelessness, among items related to impulsivity, somatic anxiety, learning anxiety, self-blaming and social anxiety in the MHT (Fig. 1). This indicates that DSs influence the covariance among anxiety and externalizing behaviors, and may introduce a degree of instability within the symptom network. The weights of all edges in both groups at the four time points are listed in Tables S2–S9.
In NCT analysis, the network structure invariance test revealed a significant difference in edge weights (p =.03) between the NDS and DS groups only at t1. The particular edges that differed across the two networks were investigated and identified with Bonferroni‒Holm correction. The edge weights between impulsivity and loss of temper were statistically significant, and at t1, the DS group manifested higher strength between impulsivity and loss of temper than the NDS group (0.33 versus 0.12).
In terms of the centrality index, oversensitivity had the highest node strength for the networks of the NDS group over time. The items with the highest node strength for the networks of the DS group were impulsivity at t1, t2 and t4 and somatic anxiety at t3 (Fig. 2). In the NDS group, the average node strength between follow-up and baseline was greatest for oversensitivity. In the DS group, the average node strength was greatest for impulsivity (see Table 3). Oversensitivity and impulsivity had the largest effect-size differences between the NDS and DS groups among the four time points. This was consistent with the results of network comparison tests for node strength between the two groups from t1 to t4 (Table S10).
Centrality index of nodal strength. (A) The depressive symptom and non-depressive symptom groups at baseline (DS-t1 and NDS-t1). (B) The depressive symptom and non-depressive symptom groups at t2 (DS-t2 and NDS-t2). (C) The depressive symptom and non-depressive symptom groups at t3 (DS-t3 and NDS-t3). (D) The depressive symptom and non-depressive symptom groups at t4 (DS-t4 and NDS-t4). The centrality index is shown as standardized z scores. The names of the nodes (‘Blame’, ‘FE’, ‘FS’, ‘HL’, ‘HS’, ‘Imp’, ‘Learn’, ‘Lon’, ‘LT’, ‘Pho’, ‘PHQ-9’, ‘Sen’, ‘Soc’, ‘Som’) were ‘Self-blaming’, ‘Family environment’, ‘Friendship’, ‘Hopelessness’, ‘Help-seeking’, ‘Impulsivity’, ‘Learning anxiety’, ‘Loneliness’, ‘Loss of temper’, ‘Phobia’, ‘PHQ-9 score’, ‘Oversensitivity’, ‘Social anxiety’, and ‘Somatic anxiety’. PHQ-9, the 9-item Patient Health Questionnaire
Network accuracy and stability
The results of the edge weight bootstrap analysis (Fig. S3) presented an overlap among the 95% CIs of the edge weights, especially in the strongest edges. Fig. S4 indicates a high stability of the centrality estimates. The results of the bootstrapped difference tests between edge weights and node centralities are listed in Fig. S5–S6. For the robustness analysis, the CS-coefficients for node strength were above 0.50, and those for closeness were above 0.40 in the two groups from t1 to t4 (Table S11), suggesting that the network was sufficiently stable and that a greater number of cases could be dropped from the original sample without significant changes in the magnitude of the centrality estimates. However, the CS-coefficient for betweenness ranged from 0.13 to 0.28 in the NDS group and ranged from 0.05 to 0.36 in the DS group, which partly reduced the strong support of stability reached by the two other indices and should be interpreted cautiously.
Discussion
In this longitudinal study, we used a nondiagnostic framework to explore complex associations between DSs and associated factors at the network level in the NDS and DS groups across four time points. Our main findings suggest that the network connection strength varied with symptom severity over time, and unique central nodes were identified for the NDS and DS groups as oversensitivity and impulsivity (3 out of 4 time points), respectively. Additionally, the NDS group exhibited relatively stable connection strengths. These findings are consistent with our hypothesis that adolescents in the NDS group may have experienced some degree of anxiety.
In the global network metrics, the NDS and DS groups showed no significant differences over time. However, the network structure invariance between the two groups differed significantly at t1, and the DS group exhibited larger edge weights between impulsivity and loss of temper than the NDS group. In addition, the central factor with the highest average node strength in the DS group was impulsivity. Prior research suggests that impulsivity moderates the relationship between DSs and risk behaviors during adolescence [43, 44]. In addition, loss of temper and irritable mood are associated with subsequent DSs assessed in follow-ups [18], and in adolescents with depression, irritable mood is identified as a core diagnostic symptom [3]. Moreover, a recent study indicated that irritable mood is a prominent central node in the network analysis of depressive and anxiety symptoms among adolescents [22]. Furthermore, adolescents with impulsivity or irritable mood are prone to use poor emotion regulation strategies in response to negative events, which may contribute to the generation of depressed mood [44, 45].
The current findings revealed that the central factor with the highest node strength in the NDS group over four time points was worry and oversensitivity. Intriguingly, the NDS group presented similar top positive edge weights over time, including those between learning anxiety and social anxiety and those between somatic anxiety and phobia. Previous research indicated that oversensitivity appears to reflect an individual feeling of being overwhelmed by a general sense of worry, which is strongly linked to developmental changes with age and cognitive ability [14, 46]. In addition, worry and oversensitivity may longitudinally predict depression and anxiety disorders, especially in subpopulations of adolescents with high and increasing anxiety levels [14, 47]. Notably, learning anxiety is the most prevalent anxiety subtype in Chinese adolescents [48, 49]. From an early age, Chinese youth need to handle great academic pressure and a substantial amount of homework and face high expectations and strict supervision from their parents [46, 50]. Additionally, prior studies have revealed that high academic stress has been linked to depressive and anxiety symptoms in adolescents [48, 49, 51]. Moreover, social anxiety states appear to be stable in adolescents, and higher social anxiety is associated with poorer psychosocial adjustment [52].
Considering values of node strength from baseline to follow-up, different network patterns emerged in the NDS and DS groups. Additionally, with the NCT, significant differences in node strength were noted in oversensitivity and impulsivity between the NDS and DS groups over time. At the network level, there were no significant findings in the comparisons of node strength between networks in the DS group over time, but the edge weights in the DS group differed. Given the relatively low Jaccard similarity coefficient in the DS group among the four time points, adolescents who reported DSs partly overlapped and varied somewhat over time. Prior research has reported that adolescents experience greater mood instability than adults [53]. Additionally, adolescence is a period with low emotion differentiation [54], and emotion differentiation also fluctuates within individuals over time [55]. Moreover, neuroendocrine changes during puberty affect alterations of brain regions implicated in emotion processing that may relate to the changes in adolescents’ self-reported emotional experiences [56]. Furthermore, contributing factors associated with DSs at the population level may be different and complex over time, which may be linked to the heterogeneity of depression, especially in adolescents [3, 57].
This study has some limitations. First, self-report questionnaires were used, and the screening results may not be sufficient to confirm a clinical diagnosis of depression. Therefore, professional assistance should be sought, and comprehensive evaluations should be performed for those whose PHQ-9 scores indicate possible depressive disorders [58]. Second, while the sample size of this longitudinal study was adequate to perform the analysis, future studies with a larger and more diverse population, may help confirm and extend the present findings. Third, other factors, such as genetic liability, adverse childhood experiences, screen use and family socioeconomic status, may be associated with DSs in adolescents. Future longitudinal research examining DSs in adolescents could benefit from focusing on these research areas to enhance our understanding of the complex and multifactorial nature of depressive symptoms in this population.
Conclusion
This study found that the network connection strength varied with symptom severity over time, and a higher severity of DSs may have introduced a degree of stability in the network. Depressive severity may have altered the structure of the symptom network and potential risk predictors. These findings have important implications for clinical practice and school educators, particularly when assisting adolescents suffering from depression. Future research and preventive strategies and intervention efforts should consider targeting a reduction if nonclinical DSs to prevent the consolidation of antecedent or risk-symptom relationships.
Data availability
The authors declare that all data supporting the findings of this study are available within the paper and its supporting information. The data are available from the corresponding author upon reasonable request.
References
Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, Rohde LA, Srinath S, Ulkuer N, Rahman A. Child and adolescent mental health worldwide: evidence for action. Lancet. 2011;378(9801):1515–25.
Gore FM, Bloem PJ, Patton GC, Ferguson J, Joseph V, Coffey C, Sawyer SM, Mathers CD. Global burden of disease in young people aged 10–24 years: a systematic analysis. Lancet. 2011;377(9783):2093–102.
Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. Lancet. 2012;379(9820):1056–67.
Copeland WE, Alaie I, Jonsson U, Shanahan L. Associations of Childhood and Adolescent Depression with Adult Psychiatric and Functional outcomes. J Am Acad Child Adolesc Psychiatry. 2021;60(5):604–11.
Kwong ASF, López-López JA, Hammerton G, Manley D, Timpson NJ, Leckie G, Pearson RM. Genetic and environmental risk factors Associated with trajectories of Depression symptoms from adolescence to Young Adulthood. JAMA Netw Open. 2019;2(6):e196587.
Angst J, Sellar R, Merikangas KR. Depressive spectrum diagnoses. Compr Psychiatry. 2000;41(2, Supplement 1):39–47.
Hankin BL, Fraley RC, Lahey BB, Waldman ID. Is depression best viewed as a continuum or discrete category? A taxometric analysis of childhood and adolescent depression in a population-based sample. J Abnorm Psychol. 2005;114(1):96–110.
Dekker MC, Ferdinand RF, van Lang ND, Bongers IL, van der Ende J, Verhulst FC. Developmental trajectories of depressive symptoms from early childhood to late adolescence: gender differences and adult outcome. J Child Psychol Psychiatry. 2007;48(7):657–66.
Yaroslavsky I, Pettit JW, Lewinsohn PM, Seeley JR, Roberts RE. Heterogeneous trajectories of depressive symptoms: adolescent predictors and adult outcomes. J Affect Disord. 2013;148(2–3):391–9.
Tang X, Tang S, Ren Z, Wong DFK. Prevalence of depressive symptoms among adolescents in secondary school in mainland China: a systematic review and meta-analysis. J Affect Disord. 2019;245:498–507.
Li F, Cui Y, Li Y, Guo L, Ke X, Liu J, Luo X, Zheng Y, Leckman JF. Prevalence of mental disorders in school children and adolescents in China: diagnostic data from detailed clinical assessments of 17,524 individuals. J Child Psychol Psychiatry. 2022;63(1):34–46.
Kong LZ, Lai JB, Hu SH. China initiates depression screening in children and adolescents. Lancet Psychiatry. 2022;9(2):107–8.
McElroy E, Fearon P, Belsky J, Fonagy P, Patalay P. Networks of depression and anxiety symptoms Across Development. J Am Acad Child Adolesc Psychiatry. 2018;57(12):964–73.
Olatunji BO, Cole DA. The longitudinal structure of general and specific anxiety dimensions in children: testing a latent trait-state-occasion model. Psychol Assess. 2009;21(3):412–24.
Gullone E, King NJ, Ollendick TH. Self-reported anxiety in children and adolescents: a three-year follow-up study. J Genet Psychol. 2001;162(1):5–19.
van Harmelen AL, Gibson JL, St Clair MC, Owens M, Brodbeck J, Dunn V, Lewis G, Croudace T, Jones PB, Kievit RA, et al. Friendships and family support reduce subsequent depressive symptoms in At-Risk adolescents. PLoS ONE. 2016;11(5):e0153715.
Cataldo MG, Nobile M, Lorusso ML, Battaglia M, Molteni M. Impulsivity in depressed children and adolescents: a comparison between behavioral and neuropsychological data. Psychiatry Res. 2005;136(2):123–33.
Stringaris A, Zavos H, Leibenluft E, Maughan B, Eley TC. Adolescent irritability: phenotypic associations and genetic links with depressed mood. Am J Psychiatry. 2012;169(1):47–54.
Sawyer MG, Borojevic N, Ettridge KA, Spence SH, Sheffield J, Lynch J. Do help-seeking intentions during early adolescence vary for adolescents experiencing different levels of depressive symptoms? J Adolesc Health. 2012;50(3):236–42.
Wichers M, Riese H, Hodges TM, Snippe E, Bos FM. A narrative review of Network studies in Depression: what different methodological approaches tell us about Depression. Front Psychiatry. 2021;12:719490.
Platania GA, Savia Guerrera C, Sarti P, Varrasi S, Pirrone C, Popovic D, Ventimiglia A, De Vivo S, Cantarella RA, Tascedda F, et al. Predictors of functional outcome in patients with major depression and bipolar disorder: a dynamic network approach to identify distinct patterns of interacting symptoms. PLoS ONE. 2023;18(2):e0276822.
Cai H, Bai W, Liu H, Chen X, Qi H, Liu R, Cheung T, Su Z, Lin J, Tang YL, et al. Network analysis of depressive and anxiety symptoms in adolescents during the later stage of the COVID-19 pandemic. Transl Psychiatry. 2022;12(1):98.
Guerrera CS, Platania GA, Boccaccio FM, Sarti P, Varrasi S, Colliva C, Grasso M, De Vivo S, Cavallaro D, Tascedda F, et al. The dynamic interaction between symptoms and pharmacological treatment in patients with major depressive disorder: the role of network intervention analysis. BMC Psychiatry. 2023;23(1):885.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Kroenke K. Enhancing the clinical utility of depression screening. CMAJ. 2012;184(3):281–2.
Zhou B. Mental health test. Shanghai: East China Normal University Press; 1991.
Jaccard P. Nouvelles recherches sur la distribution florale. Bull Soc Vaud Sci Nat. 1908;44:223–70.
R Core Team: R: A language and environment for statistical computing. 2013. https://www.r-project.org/.
Lauritzen SL, Wermuth N. Graphical models for associations between variables, some of which are qualitative and some quantitative. Ann Stat. 1989;17(1):31–57.
Leung DYP, Mak YW, Leung SF, Chiang VCL, Loke AY. Measurement invariances of the PHQ-9 across gender and age groups in Chinese adolescents. Asia Pac Psychiatry. 2020;12(3):e12381.
Friedman J, Hastie T, Tibshirani R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics. 2008;9(3):432–41.
Foygel R, Drton M. Extended Bayesian Information Criteria for Gaussian Graphical Models. In: NIPS: 2010; 2010. https://doi.org/10.48550/arXiv.1011.6640.
Boccaletti S, Latora V, Moreno Y, Chavez M, Hwang DU. Complex networks: structure and dynamics. Phys Rep. 2006;424(4):175–308.
Fruchterman TM, Reingold EM. Graph drawing by force-directed placement. Softw Pract Exp. 1991;21(11):1129–64.
Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D. Qgraph: network visualizations of relationships in Psychometric Data. J Stat Softw. 2012;48(4):1–18.
Csárdi G, Nepusz T. The igraph software package for complex network research. Int J Complex Syst. 2006;1695(5):1–9.
Opsahl T, Agneessens F, Skvoretz J. Node centrality in weighted networks: generalizing degree and shortest paths. Soc Netw. 2010;32(3):245–51.
Christensen AP. NetworkToolbox: methods and measures for Brain, Cognitive, and Psychometric Network Analysis in R. R J. 2018;10:422.
Borkulo CDv, Boschloo L, Kossakowski JJ, Tio P, Schoevers RA, Borsboom D, Waldorp LJ. Comparing network structures on three aspects: a permutation test. Psychol Methods. 2022. https://doi.org/10.1037/met0000476.
Bringmann LF, Elmer T, Epskamp S, Krause RW, Schoch D, Wichers M, Wigman JTW, Snippe E. What do centrality measures measure in psychological networks? J Abnorm Psychol. 2019;128(8):892–903.
Piao YH, Yun JY, Nguyen TB, Kim WS, Sui J, Kang NI, Lee KH, Ryu S, Kim SW, Lee BJ et al. Longitudinal symptom network structure in first-episode psychosis: a possible marker for remission. Psychol Med. 2021:1–9.
Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. 2018;50:195–212.
Felton JW, Shadur JM, Havewala M, Gonçalves S, Lejuez CW. Impulsivity moderates the relation between depressive symptoms and substance use across adolescence. J Clin Child Adolesc Psychol. 2020;49(3):365–77.
d’Acremont M, Van der Linden M. How is impulsivity related to depression in adolescence? Evidence from a French validation of the cognitive emotion regulation questionnaire. J Adolesc. 2007;30(2):271–82.
Malhi GS, Byrow Y, Outhred T, Das P, Fritz K. Irritability and internalizing symptoms: modeling the mediating role of emotion regulation. J Affect Disord. 2017;211:144–9.
Li H, Ang RP, Lee J. Anxieties in Mainland Chinese and Singapore Chinese adolescents in comparison with the American norm. J Adolesc. 2008;31(5):583–94.
Allan NP, Capron DW, Lejuez CW, Reynolds EK, MacPherson L, Schmidt NB. Developmental trajectories of anxiety symptoms in early adolescence: the influence of anxiety sensitivity. J Abnorm Child Psychol. 2014;42(4):589–600.
Liu H, Shi Y, Auden E, Rozelle S. Anxiety in rural Chinese children and adolescents: comparisons across provinces and among subgroups. Int J Environ Res Public Health. 2018, 15(10).
Qin J, Ding Y, Gao J, Wu Y, Lv H, Wu J. Effects of COVID-19 on Mental Health and anxiety of adolescents aged 13–16 years: a comparative analysis of Longitudinal Data from China. Front Psychiatry. 2021;12:695556.
Xu DD, Rao WW, Cao XL, Wen SY, An FR, Che WI, Bressington DT, Cheung T, Ungvari GS, Xiang YT. Prevalence of depressive symptoms in primary school students in China: a systematic review and meta-analysis. J Affect Disord. 2020;268:20–7.
Feng T, Jia X, Pappas L, Zheng X, Shao T, Sun L, Weisberg C, Li ML, Rozelle S, Ma Y. Academic performance and the link with depressive symptoms among rural Han and Minority Chinese adolescents. Int J Environ Res Public Health. 2022, 19(10).
Camacho A, Ortega-Ruiz R, Romera EM. Adolescents’ social anxiety dynamics in a latent transition analysis and its psychosocial effects. Int J Clin Health Psychol. 2022;22(3):100311.
Larson R, Csikszentmihalyi M, Graef R. Mood variability and the psychosocial adjustment of adolescents. J Youth Adolesc. 1980;9(6):469–90.
Nook EC, Sasse SF, Lambert HK, McLaughlin KA, Somerville LH. The Nonlinear development of emotion differentiation: Granular Emotional experience is low in adolescence. Psychol Sci. 2018;29(8):1346–57.
Erbas Y, Kalokerinos EK, Kuppens P, van Halem S, Ceulemans E. Momentary emotion differentiation: the derivation and validation of an index to Study within-person fluctuations in emotion differentiation. Assessment. 2022;29(4):700–16.
Bailen NH, Green LM, Thompson RJ. Understanding emotion in adolescents: a review of emotional frequency, intensity, instability, and clarity. Emot Rev. 2019;11(1):63–73.
Goldberg D. The heterogeneity of major depression. World Psychiatry. 2011;10(3):226–8.
Tsai FJ, Huang YH, Liu HC, Huang KY, Huang YH, Liu SI. Patient health questionnaire for school-based depression screening among Chinese adolescents. Pediatrics. 2014;133(2):e402–409.
Acknowledgements
We would like to express our gratitude to all the participants who took part in the study. We would also like to thank the school teachers and educators who contributed to the research by providing their support and assistance.
Funding
This work was supported by the National Natural Science Foundation of China Key Project (81920108018 and 82230046 to TL); the China Brain Project (grant number 2021ZD0200404 to TL), the Key R & D Program of Zhejiang (grant number 2022C03096 to TL); the Project for Hangzhou Medical Disciplines of Excellence & Key Project for Hangzhou Medical Disciplines; the Science & Technology Development Project of Hangzhou (202004A11 to TL, A20210013 to SGL); and the Leading Healthcare Talents of Zhejiang Province; the Monique H. Bourgeois Chair in Developmental Disorders and Graham Boeckh Foundation (Douglas Research Centre, McGill University) (to LP).
Author information
Authors and Affiliations
Contributions
ZJH and TL designed the study and wrote the protocol. SGL, LP and YW managed the literature searches and analyses. YQW and ZQZ had interview with participants and gathered data. SGL undertook the statistical analysis with some help from LP, WJG and YMZ. SGL and LP wrote the first draft of the manuscript. TL, LP, SDF and ZYC were involved in the revision and completion of the work. All authors contributed to and have approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the research ethics committee of Affiliated Mental Health Centre, Zhejiang University School of Medicine. The research was performed in accordance with the ethical standards as laid down in the Declaration of Helsinki. The parents of all participants gave informed consent and all participants gave informed assent prior to participation.
Consent for publication
Not Applicable.
Competing interests
LP reports personal fees from Janssen Canada, Otsuka Canada, SPMM Course Limited, UK, Canadian Psychiatric Association; book royalties from Oxford University Press; investigator-initiated educational grants from Janssen Canada, Sunovion and Otsuka Canada outside the submitted work. All other authors report no relevant conflicts.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liang, S., Huang, Z., Wang, Y. et al. Using a longitudinal network structure to subgroup depressive symptoms among adolescents. BMC Psychol 12, 46 (2024). https://doi.org/10.1186/s40359-024-01537-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40359-024-01537-8