Abstract
Background
The outbreak of the Corona Virus Disease 2019 (COVID-2019) has resulted in a significant number of diagnosed patients requiring treatment in designated hospitals. However, limited evidence exists regarding the prevalence of mental health problems and associated psychological factors in COVID-19 patients.
Objectives
This study investigated the prevalence rates of anxiety, depression, and insomnia among COVID-19 patients, as well as explored the associations between these mental health problems and psychological factors.
Methods
A cross-sectional study was conducted among 387 COVID-19 patients in a designated shelter hospital. Online measures were used to assess anxiety, depression, insomnia, social support, coping styles, and emotional regulation. Data were analyzed to determine the prevalence rates of mental health problems and examine the associations between these problems and the psychological factors.
Results
The results revealed high prevalence rates of anxiety (21.80%), depression (49.0%), and insomnia (63.70%) among COVID-19 patients. Objective social support scores and positive coping style scores were significantly associated with lower levels of anxiety, depression, and insomnia, respectively. Conversely, high negative coping style scores, higher education level, and self-perceived illness severity, were significantly related to higher levels of anxiety, depression, or insomnia symptoms. Emotional regulation scores did not show a significant association with any of the examined mental health problems.
Conclusions
These findings have implications for guiding psychological interventions tailored to COVID-19 patients in future outbreaks. By targeting social support and promoting adaptive coping strategies, psychological interventions can address the psychological distress experienced by COVID-19 patients.
Similar content being viewed by others
Background
The outbreak of coronavirus disease 2019 ( COVID-19) originated in China and rapidly spread to numerous countries, leading to a global pandemic [1]. The escalating global morbidity and mortality rates associated with COVID-19 have raised significant public health concerns [2], affecting more than 281 million individuals worldwide [3]. The immediate psychological impact of the COVID-19 outbreak has been extensively studied in China. A survey assessed the initial psychological response of the general public after two weeks into the COVID-19 outbreak in China [4]. The findings indicated that 16.5% of patients reported moderate to severe depressive symptoms, 28.8% reported moderate to severe anxiety symptoms, and 8.1% reported moderate to severe stress levels. The prevalence of psychological problems was higher among individuals affected by the disease compared to the general population [5]. Similar findings have been observed in other countries as well [6].
Previous studies have primarily focused on the mental health implicates of COVID-19 among the general population, healthcare workers, and individuals in quarantine [7, 8]. However, the psychological impacts on individuals infected with the virus should also be considered. Currently, there is limited and unclear evidence regarding the prevalence of mental disorders in patients with COVID-19. A recent cross-sectional study examined the psychological problems of patients with COVID-19 who were treated in designated hospitals in Wuhan, China [9]. The study revealed a higher prevalence of anxiety, depression, and sleep disturbance among these patients. Similarly, Yadav and colleagues investigated the psychological distress experienced by patients with COVID-19 at a tertiary care center in North India [10]. Their findings indicated that 27% of patients experienced depression, 67% reported anxiety, and 62% had sleep disorders. Moreover, observational studies [11] and meta-analysis studies [12] have consistently demonstrated that patients with COVID-19 are more susceptible to anxiety, depression, and sleep problems due to the highly infectious nature of the disease. These findings suggested that individuals with COVID-19 are at a heightened risk of developing mental health issues.
Several factors have been identified to impact individual mental health, including social support, coping styles, and emotion regulation strategies. Social support plays a crucial role in reducing psychological distress [13]. Adequate social support has been shown to alleviate depression, and anxiety symptoms [14] and positively influence on sleep quality [15]. Conversely, individuals lacking access to social support tend to experience higher levels of anxiety and depression symptoms [16]. Coping styles are also associated with mental health outcomes during the COVID-19 pandemic [17]. Positive or problem-focused coping styles have been found to alleviate symptoms of depression, insomnia, and post-traumatic stress symptoms [18], while negative or emotion-focused coping styles may exacerbate mental health symptoms [19]. Additionally, emotion regulation is strongly linked to overall well-being [20]. Adaptive emotion regulation strategies enable individuals to cope with environmental stressors [21] and have been shown to reduce COVID-19-related anxiety [22], depression [23], and sleep disturbance [24].
While previous studies have extensively examined the relationship between elements such as social support, coping style, and emotion regulation, and their potential influence on the severity of anxiety, depression, and insomnia in the general public [25,26,27] and frontline healthcare workers [28,29,30] during the COVID-19 pandemic, limited attention has been given to these associations in patients with COVID-19. Understanding the psychological and social factors that can help protect against psychological distress in patients with COVID-19 is crucial. Therefore, the aim of this cross-sectional study was to investigate the mental health status of patients with COVID-19 and explore the potential factors, including social support, coping styles, and emotion regulation, that are associated with mental health status.
Methods
Participants
This cross-section investigation was conducted using an anonymous online questionnaire from April 9, 2022, to May 10, 2022. The participants of the study were recruited from inpatients with COVID-19 in a designated shelter hospital in Shanghai, China. Participants completed online questionnaire prior to their discharge. The inclusion criteria for the patients were as follows: (1) a stable state of consciousness, (2) ability to understand and complete the questionnaire, and (3) being easily approachable during the investigation. Patients were diagnosed based on the guideline for COVID-19 (eighth edition) issued by the National Health Commission of China [31]. Confirmation of the diagnosis was done through chest CT scanning or nasopharyngeal swab testing with real-time reverse transcription-polymerase chain reaction (RT-PCR). Exclusion criteria were included: (1) previously diagnosed serious mental disorders such as schizophrenia and bipolar disorder, (2) current oral medication for a chronic condition that causes side effects related to mental health issues such as anxiety and depression, and (3) refusal to provide consent to participation. A total of 407 inpatients met the specified criteria and were included in the study.
Procedure
This study was conducted by doctors working at the hospital and was approved by the Medical Ethics Committees of the Second Affiliated Hospital of Army Medical University (No.2022-332-01). Participants were provided information about the purpose of the study and assured that their data would remain confidential. They were also asked to review and sign an informed consent form indicating their voluntary participation in the study. Participants were then asked to complete a series of questionnaires that included socio-demographic information, clinical characteristics, and mental health status measurements.
Measures
Demographic and clinical characteristics
The patients in this study completed the online questionnaires by scanning the quick response code with their mobile phones. The self-designed questionnaires to collect data on demographic and clinical characteristics. The detailed information collected included gender, age, marital status, education level, employment status, oral medication, hospitalization period, and self-perceived illness severity.
Mental health status
Symptoms of anxiety were evaluated using the Generalized Anxiety Disorder-7 (GAD-7) scale, a self-administered screening tool devised for the detection of potential anxiety. The GAD-7 scoring system ranges from 0 to 21, categorizing anxiety severity into four levels: no anxiety (0–5), mild anxiety (6–10), moderate anxiety (10–15), and severe anxiety (16–21) [32]. Symptoms of depression were ascertained by the Patient Health Questionnaire-9 (PHQ-9) scale, a self-reporting diagnostic tool for depression. The PHQ-9 scoring framework spans from 0 to 27, designating depression severity classified into five categories: no depression (0–4), mild depression (5–9), moderate depression (10–14), moderately severe depression (15–19), and severe depression (20–27) [33]. Sleep problems were evaluated by Athens Insomnia Scale (AIS), a self-reported instrument specifically designed to determine the insomnia severity. Comprising 8 items rated from 0 to 3, the AIS considers a cumulative score exceeding 8 as indicative of insomnia [34]. These three scales have demonstrated strong reliability and validity in previous studies [35, 36], and in this study, their Cronbach’s alpha values were 0.949, 0.925, and 0.9, respectively.
In addition, this study evaluated social support using the Social Support Rating Scale (SSRS). This ten-item scale gauges three facets of social support: objective support, subjective support, and support utilization [37]. It has exhibited robust reliability and reliability [38], with Cronbach’s alpha values in this study being 0.893, 0.825, and 0.896, respectively, for the three scales. Coping styles were scrutinized via the Simplified Coping Style Questionnaire (SCSQ) [39]. This 20-item questionnaire assesses two coping styles: positive coping style and negative coping style, and has previously demonstrated strong reliability and validity [40]. In this study, the Cronbach’s alpah values were 0.925 and 0.810, respectively. Emotion regulation strategies were assessed using the Emotion Regulation Questionnaire (ERQ) which comprises 10 items to measure two particular strategies: cognitive reappraisal and expressive suppression [41]. This tool has shown good psychometric properties [42], and in this study, the two subscales’ Cronbach’s alpah values were 0.919 and 0.876, respectively.
Statistical analyses
All statistical analyses were conducted using IBM SPSS version 26 (IBM Corporation, Armonk, NY, USA). Categorial data were presented as frequencies and percentages, while continuous data were presented as mean ± standard deviation (SD). Multiple linear regression analysis was performed to identify the independent factors associated with anxiety, depression, and insomnia, including social support, coping styles, emotional regulation, and demographic variables. The enter method was used for linear regression. For all statistical analyses, a threshold of p < 0.01 was established to denote statistical significance.
Results
Demographic and clinical characteristics
A total of 407 patients with COVID-19 participated were initially enrolled in this study, and 387 of them completed the survey, resulting in an effective response rate of 95%. Table 1 presents the demographic and clinical characteristics of the participants. The mean age was 41 years (SD = 14 years). More than half the patients were male (53.20%), married (69.80%), and employed (75.50%).
Assessment of mental health status
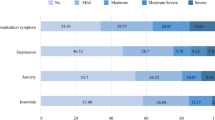
The mean scores of GAD_7, PHQ_9, and AIS were 9.56 (SD = 4.48), 12.61 (SD = 5.30), and 12.02 (SD = 4.91), respectively. Figure 1 presents the distribution of participants across the three levels of severity for anxiety, depression, and insomnia. According to the PHQ-9, 25.60% of patients had moderate to severe depression, with 33 (8.50%) falling into the severe category. Using the GAD-7,190 patients (49.0%) were classified as having moderate to severe anxiety. For the AIS, 36.30% of patients reported normal sleep patterns, while 63.80% experienced insomnia.
Factors associated with mental health status
Figure 2 displays the outcomes of the univariate analyses conducted on the patient sample. The results indicated that patients possessing higher levels of education, such as a college degree or above, reported poorer sleep quality compared to those with only primary and junior school education (t = 3.774, p < 0.01; t = 4.799, p < 0.01). Furthermore, patients perceiving their disease as severe or very severe manifested elevated levels of anxiety (t = 3.271, p < 0.01; t = 3.858, p < 0.01) and depression (t = 3.981, p < 0.01; t = 3.429, p < 0.01), in contrast to those with a normal disease perception. Similarly, those reporting a severe to very severe disease perception experienced more pronounced sleep disturbances than individuals perceiving their disease as normal (t = 2.267, p = 0.008; t = 2.350, p = 0.007).
Table 2 illustrates the results from the multiple linear regression models pertaining to GAD_7, PHQ_9, and AIS scores. Notably, certain variables consistently exhibited significance within the regression model. Specifically, both objective support and positive coping style were inversely related to GAD_7 scores (Beta = -0.159, t = 2.722, p = 0.007; Beta = -0.258, t = 3.759, p < 0.01 ), PHQ_9 scores (Beta = -0.170, t = 2.940, p = 0.003; Beta = -0.303, t = 4.456, p < 0.01), and AIS scores (Beta = -0.215, t = 3.176, p = 0.002). Contrastingly, a negative coping strategy was positively associated with GAD_7 scores (Beta = 0.152, t = 2.709, p = 0.007) and PHQ_9 scores (Beta = 0.184, t = 3.303, p = 0.001). Additionally, self-perceived disease severity and education level emerged as substantial predictors of anxiety symptoms (Beta = 0.181, t = 3.630, p < 0.01; Beta = 0.191, t = 3.516, p < 0.01), depression symptoms (Beta = 0.161, t = 3.200, p = 0.001; Beta = 0.188, t = 3.492, p = 0.001), and insomnia (Beta = 0.114, t = 2.240, p = 0.026) among the patients. However, emotion regulation strategies did not demonstrate associations with GAD_7 scores, PHQ_9 scores, or AIS scores in these models.
Discussion
The present study investigated the mental health status and identified related factors in COVID-19 patients. The findings revealed that anxiety and depression were the most prevalent psychological distress, accompanied by a high prevalence of insomnia. Factors that negatively affected the mental health of patients included negative coping style, higher levels of education, and self-perceived illness severity. On the other hand, objective support and positive coping style were found to be protective factors against psychological distress. These findings contribute to our understanding of the factors associated with psychological stress in COVID-19 patients and provide valuable insights into the mental health status of patients during quarantine periods.
The present study revealed significant psychological distress among COVID-19 patients, with high morbidity of anxiety (25.6%), depression (49.0%), and insomnia (63.8%). These findings align with previous survey [7] and research conducted during other epidemics [43], such as severe acute respiratory syndrome (SARS), Ebola virus, and middle east respiratory syndrome (MERS), where patients also experienced elevated levels of anxiety, depression, and sleep problems [44,45,46]. The observed correlation between patients’ self-perception of COVID-19 severity and increased symptoms of anxiety, depression, and sleep disturbances underscores the significant psychological burden associated with the pandemic. The heightened anxiety and depression symptoms among patients perceiving their COVID-19 disease severity as high might be primarily attributable to the elements of fear and uncertainty. Fear regarding the potential outcomes of a severe illness, such as enduring disability or mortality, can evoke considerable emotional distress [47]. Concurrently, uncertainty surrounding the progression and prognosis of COVID-19, especially in severe cases, may incite anticipatory anxiety and concern, leading to depressive symptoms [48]. The association between perceived disease severity and sleep disruptions can be interpreted within the framework of stress-induced insomnia. It is well documented that stress, especially chronic or intense, can lead to sleep disturbances or insomnia [49]. Inherently, perceiving one’s disease as severe can be a source of significant stress, and the cognitive arousal it evokes – encompassing intrusive thoughts and excessive worrying – can hinder sleep onset or maintenance. Such cognitive arousal tends to peak at bedtime, a period marked by fewer distractions and increased solitude, thereby leading to deteriorated sleep quality and insomnia [50].
Intriguingly, this study revealed that COVID-19 patients with higher education levels (college or above) experienced more severe sleep disturbances than those with primary or junior school education. This may initially seem counterintuitive as a higher education level is generally associated with improved health outcomes [51]. However, when interpreted in the context of a pandemic, the relationship between educational attainment and sleep disturbances becomes multifaceted. A plausible explanation could be the degree of information exposure and consumption. Individuals with higher educational qualifications are likely to follow updates about COVID-19 more closely and comprehend the evolving scientific discourse surrounding the virus, which often contains distressing information. Exposure to such pandemic-related news has been linked to sleep disturbances [52]. Cognitive processes might also contribute to this phenomenon. Higher educational attainment is often associated with increased cognitive rumination, characterized by repetitive thinking about one’s problems and associated emotions. In the context of negative or stressful situations, such as a pandemic, rumination can intensify emotional responses, contributing to sleep difficulties [53]. Nonetheless, these interpretations are preliminary, and this unexpected finding merits further research to uncover the underlying mechanisms.
It is indeed intriguing that objective support, rather than subjective support or support utilization, was found to significantly alleviate the level of anxiety, depression, and insomnia in patients. Previous studies have consistently demonstrated the positive effects of social support on improving psychological well-being. Social support can enhance the individuals’ sense of self-protection [54] and effectively mitigate the negative impact of stressful events on the mental health. During the COVID-19 pandemic, an enforced lockdown policies and restrictions limited the availability of subjective support from family and friends. Therefore, receiving tangible and concrete support (e.g., objective support) from the government agencies, non-government organizations, and local community [55], or through online platforms and social media [56] became crucial in helping patients cope with stress and improve their mental health. Particularly, support from social media and online communication platforms can provide access to health information [57] and facilitate interactions with others in the similar condition [58], which plays an important role in how patients respond to COVID-19. The findings of this study suggest that patients who reported higher levels of objective social support were less likely to experience symptoms of anxiety, depression, and insomnia. This highlights the significance of actual social support as a protective factor for the mental health of patients with COVID-19 in isolated environments. By receiving visible and tangible support, patients can feel more supported and connected, which can buffer the psychological impact of the pandemic and promote better mental well-being.
Indeed, coping styles play an important role in mental health outcomes [59]. Positive coping style, characterized by problem-focused coping strategies such as seeking advice from others or finding multiple solutions to problem, has been associated with better mental health outcomes [60]. On the other hand, negative coping style, which emphasize helplessness and passivity, tends to be associated with increased feelings of depression and anxiety [61]. In line with the previous studies, the current study found that a higher found positive coping style was associated with fewer symptoms of anxiety, depression, and insomnia, while negative coping style showed the opposite pattern. These findings suggested that adopting a positive coping style, focusing on active problem-solving and seeking support, serves was a protective factor for the mental health of patients. Additionally, the study identified higher education levels, being divorced, and self-perceived illness severity as risk factors for anxiety, depression, and insomnia. As mentioned above, individuals with higher education levels or who are divorced and self-perceived illness severity are particularly vulnerable to developing mental health problems during the COVID-19 pandemic [62,63,64], This suggests that patients with higher education levels or those who are divorced and perceive their illness as more severity may experience exacerbated mental health difficulties in the context of the pandemic.
Cognitive reappraisal and expressive suppression are two commonly unitized emotion regulation methods. Cognitive reappraisal has been shown to enhance positive emotions and prevent distress [65]. Conversely, expressive suppression can intensify negative emotions and increase distress [66]. Surprisingly, the current survey did not find an association between emotion regulation and the mental health status of patients with COVID-19. This finding may be attributed to the unique circumstances faced by COVID-19 patients, such as enforced quarantine and the perceived threat to life. Under these circumstances, strategies like changing the meaning of a situation and inhibiting emotional expression may be ineffective. The high prevalence of anxiety and depression among patients provides indirect evidence supporting this notion.
There are a few limitations to our study that should be acknowledged. Firstly, the study design was cross-sectional, which limits our ability to establish causal relationships between mental health issues and the related factors. Longitudinal studies would provide a stronger basis for understanding the temporal dynamics and determining causal links between variables. Secondly, our study was conducted exclusively among COVID-19 patients treated in designated hospitals. Therefore, caution should be exercised when generalizing the results to the general population or individuals with different demographic or clinical characteristics. Future research should consider including a more diverse and representative sample to enhance the external validity of the findings. Thirdly, our study lacked the collection of socioeconomic and biochemical indices, such as household income and inflammatory markers. Future research is needed to collect these additional measures, which provide a more comprehensive understanding of mental health-related factors.
Conclusions
The present study conducted a cross-section analysis of the mental status and influencing factors in patients with COVID-19. The finding revealed that COVID-19 patients experience psychological distress and sleep disturbances, and identified critical factors including objective support and coping styles as associated factors. These findings provide valuable insights into the mental health status of COVID-19 patients and highlight potential areas for psychological intervention in future outbreaks. By understanding the specific factors that contribute to psychological distress, healthcare professionals can develop targeted interventions to support the mental well-being of patients in similar circumstances.
Data Availability
All data is freely available upon request from the corresponding author. Data are not publicly available due to privacy and ethical constraints.
References
Cheng ZJ, Shan J. 2019 Novel coronavirus: where we are and what we know. Infection. 2020;48(2):155–63.
Guo Q, Zheng Y, Shi J, Wang J, Li G, Li C, Fromson JA, Xu Y, Liu X, Xu H, et al. Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: a mixed-method study. Brain Behav Immun. 2020;88:17–27.
Li DP, Liao XJ, Ma ZH, Zhang LN, Dong JK, Zheng GQ, Zi M, Peng WJ, Wei LL, Li ZY et al. Clinical status of patients 1 year after hospital discharge following recovery from COVID-19: a prospective cohort study. Ann Intensiv Care 2022, 12(1).
Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729.
Fu W, Wang C, Zou L, Guo Y, Lu Z, Yan S, Mao J. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Translational Psychiatry. 2020;10(1):225.
Mazza C, Ricci E, Biondi S, Colasanti M, Ferracuti S, Napoli C, Roma P. A nationwide survey of psychological distress among italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res public health vol. 2020;17:E3165.
Krishnamoorthy Y, Nagarajan R, Saya GK, Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2020;293(8):113382.
Zhang J, Lu H, Zeng H, Zhang S, Du Q, Jiang T, Du B. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav Immun. 2020;87(4):49–50.
Jiang ZY, Zhu PP, Wang LY, Hu Y, Pang MF, Ma SS, Tang X. Psychological distress and sleep quality of COVID-19 patients in Wuhan, a lockdown city as the epicenter of COVID-19. J Psychiatr Res. 2021;136(10):595–602.
Yadav R, Yadav P, Kumar SS, Kumar R. Assessment of depression, anxiety, and sleep disturbance in COVID-19 patients at tertiary care centre of North India. J Neurosciences Rural Pract. 2021;12(02):316–22.
Fu R, Zhang Y. Case report of a patient with suspected COVID-19 with depression and fever in an epidemic stress environment. Gen Psychiatry. 2020;33(3):e100218.
Deng JW, Zhou FW, Hou WT, Silver Z, Wong CY, Chang O, Huang EM, Zuo QK. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci. 2021;1486(1):90–111.
Raffaelli M, Andrade FCD, Wiley AR, Sanchez-Armass O, Edwards LL, Aradillas-Garcia C. Stress, social support, and depression: a test of the stress-buffering hypothesis in a mexican sample. J Res Adolescence. 2013;23(2):283–9.
Yang Y. How does functional disability affect depressive symptoms in late life? The role of perceived social support and psychological resources. J Health Soc Behav. 2006;47(4):355–72.
Kent de Grey RG, Uchino BN, Trettevik R, Cronan S, Hogan JN. Social support and sleep: a meta-analysis. Health Psychol. 2018;37(8):787–98.
Wang J, Mann F, Lloyd-Evans B, Ma R, Johnson S. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry. 2018;18(1):156.
Gurvich C, Thomas N, Thomas EHX, Hudaib A-R, Sood L, Fabiatos K, Sutton K, Isaacs A, Arunogiri S, Sharp G, et al. Coping styles and mental health in response to societal changes during the COVID-19 pandemic. Int J Soc Psychiatry. 2020;67(5):540–9.
Horwitz AG, Czyz EK, Berona J, King CA. Prospective associations of coping styles with depression and suicide risk among psychiatric emergency patients. Behav Ther. 2018;49(2):225–36.
Sim K, Huak Chan Y, Chong PN, Chua HC, Wen Soon S. Psychosocial and coping responses within the community health care setting towards a national outbreak of an infectious disease. J Psychosom Res. 2010;68(2):195–202.
Gross JJ. Emotion regulation: current status and future prospects. Psychol Inq. 2015;26(1):1–26.
Kobylinska D, Kusev P. Flexible emotion regulation: how situational demands and individual differences influence the effectiveness of regulatory strategies. Front Psychololgy. 2019;10(2):72.
Akdeniz B, Gunduz M. The mediating role of non-adaptive emotion regulation strategies in the relationship between perceived social support and anxiety in the COVID-19 pandemic. Psychiatry and Behavioral Sciences. 2022;12(3):106–13.
Ye BJ, Zhao SY, Zeng YD, Chen CS, Zhang YZ. Perceived parental support and college students’ depressive symptoms during the COVID-19 pandemic: the mediating roles of emotion regulation strategies and resilience. Curr Psychol. 2022;1163(4):1–12.
Niu XN, Snyder HR. The role of maladaptive emotion regulation in the bidirectional relation between sleep and depression in college students during the COVID-19 pandemic. Anxiety Stress Coping 2022(2):1–14.
Costa S, Canale N, Mioni G, Cellini N. Maintaining social support while social distancing: the longitudinal benefit of basic psychological needs for symptoms of anxiety during the COVID-19 outbreak. J Appl Soc Psychol. 2022;52(6):439–48.
Dimanova P, Borbas R, Schnider CB, Fehlbaum LV, Raschle NM. Prefrontal cortical thickness, emotion regulation strategy use and COVID-19 mental health. Soc Cognit Affect Neurosci. 2022;17(10):877–89.
Riaz M, Abid M, Bano Z. Psychological problems in general population during covid-19 pandemic in Pakistan: role of cognitive emotion regulation. Ann Med. 2021;53(1):189–96.
Labrague LJ. Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: a systematic review of quantitative studies. J Nurs Adm Manag. 2021;29(7):1893–905.
Alnazly E, Khraisat OM, Al-Bashaireh AM, Bryant CL. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among jordanian healthcare workers. PLoS ONE. 2021;16(3):e0247679.
Wang Q-Q, Fang Y-Y, Huang H-L, Lv W-J, Wang X-X, Yang T-T, Yuan J-M, Gao Y, Qian R-L, Zhang Y-H. Anxiety, depression and cognitive emotion regulation strategies in chinese nurses during the COVID-19 outbreak. J Nurs Adm Manag. 2021;29(5):1263–74.
Diagnosis and Treatment Guideline for COVID-19., eighth edition [http://www.nhc.gov.cn/yzygj/s7653p/202002/d4b895337e19445f8d728fcaf1e3e13a.shtml].
Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Enomoto K, Adachi T, Yamada K, Inoue D, Nakanishi M, Nishigami T, Shibata M. Reliability and validity of the Athens Insomnia Scale in chronic pain patients. J Pain Res. 2018;11(4):793–801.
Kalkbrenner MT, Ryan AF, Hunt AJ, Rahman SR. Internal consistency reliability and internal structure validity of the English versions of the patient health questionnaire-9 and the generalized anxiety disorder-7: a psychometric synthesis. Meas Evaluation Couns Dev. 2023;56(2):124–37.
Manzar MD, Albougami A, Hassen HY, Sikkandar MY, Pandi-Perumal SR, Bahammam AS. Psychometric validation of the Athens insomnia scale among nurses: a robust approach using both classical theory and rating scale model parameters. Nat Sci Sleep. 2022;14(4):725–39.
Ganster DC, Victor B. The impact of social support on mental and physical health. Br J Med Psychol. 1988;61(1):17–36.
Xu J, Ou L. Resilience and quality of life among Wenchuan earthquake survivors: the mediating role of social support. Public Health. 2014;128(5):430–7.
Xie Y. Reliability and validity of the simplified coping style questionnaire. Chin J Clin Psychol. 1998;6(2):114–5.
Wang Y, Yang Y, Xiao W-T, Su Q. Validity and reliability of the chinese version of the cognitive flexibility inventory in college students. Chin Mental Health J. 2016;30(1):58–62.
Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol. 2003;85(2):348–62.
Preece DA, Becerra R, Robinson K, Gross JJ. The emotion regulation questionnaire: psychometric properties in general community samples. J Pers Assess. 2020;102(3):348–56.
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet. 2020;395(10227):912–20.
Chua SE, Cheung V, McAlonan GM, Cheung C, Wong JWS, Cheung EPT, Chan MTY, Wong TKW, Choy KM, Chu CM, et al. Stress and psychological impact on SARS patients during the outbreak. Can J Psychiatry. 2004;49(6):385–90.
Jeong H, Yim HW, Song Y-J, Ki M, Min J-A, Cho J, Chae J-H. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol Health. 2016;38(11):e2016048–2016040.
Keita MM, Taverne B, Sy Savané S, March L, Doukoure M, Sow MS, Touré A, Etard JF, Barry M, Delaporte E, et al. Depressive symptoms among survivors of Ebola virus disease in Conakry (Guinea): preliminary results of the PostEboGui cohort. BMC Psychiatry. 2017;17(1):127.
Asmundson GJG, Taylor S. Coronaphobia: fear and the 2019-nCoV outbreak. J Anxiety Disord. 2020;70(2):102196.
Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: mental health consequences and target populations. J Neuropsychiatry Clin Neurosci. 2020;74(4):281–2.
Kalmbach DA, Anderson JR, Drake CL. The impact of stress on sleep: pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. J Sleep Res. 2018;27(6):e12710.
Riemann D, Spiegelhalder K, Feige B, Voderholzer U, Berger M, Perlis M, Nissen C. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. 2010;14(1):19–31.
Marmot M. Social determinants of health inequalities. The Lancet. 2005;365(9464):1099–104.
Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288(6):112954.
Zoccola PM, Dickerson SS, Lam S. Rumination predicts longer sleep onset latency after an acute psychosocial stressor. Psychosom Med. 2009;71(7):771–5.
Ozbay F, Johnson DC, Dimoulas E, Morgan CA, Charney D, Southwick S. Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry. 2007;4(5):35–40.
Viseu J, Leal R, de Jesus SN, Pinto P, Pechorro P, Greenglass E. Relationship between economic stress factors and stress, anxiety, and depression: moderating role of social support. Psychiatry Res. 2018;268(10):102–7.
Cole DA, Nick EA, Zelkowitz RL, Roeder KM, Spinelli T. Online social support for young people: does it recapitulate in-person social support; can it help? Comput Hum Behav. 2017;68(3):456–64.
Liu Y, Ren C, Shi D, Li K, Zhang X. Evaluating the social value of online health information for third-party patients: is uncertainty always bad? Inf Process Manage. 2020;57(5):102259.
Zhao J, Han H, Zhong B, Xie W, Chen Y, Zhi M. Health information on social media helps mitigate Crohn’s disease symptoms and improves patients’ clinical course. Comput Hum Behav. 2021;115(2):106588.
Chew QH, Wei KC, Vasoo S, Chua HC, Sim K. Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: practical considerations for the COVID-19 pandemic. Singap Med J. 2020;61(7):350–6.
Skapinakis P, Bellos S, Oikonomou A, Dimitriadis G, Gkikas P, Perdikari E, Mavreas V. Depression and its relationship with coping strategies and illness perceptions during the COVID-19 lockdown in Greece: a cross-sectional survey of the population. Depress Res Treat. 2020;2020(8):3158954.
Masha’al D, Shahrour G, Aldalaykeh M. Anxiety and coping strategies among nursing students returning to university during the COVID-19 pandemic. Heliyon. 2022;8(1):e08734.
Robb CE, de Jager CA, Ahmadi-Abhari S, Giannakopoulou P, Udeh-Momoh C, McKeand J, Price G, Car J, Majeed A, Ward H, et al. Associations of social isolation with anxiety and depression during the early COVID-19 pandemic: a survey of older adults in London, UK. Front Psychiatry. 2020;11(9):591120.
Deng J, Zhou F, Hou W, Silver Z, Wong CY, Chang O, Drakos A, Zuo QK, Huang E. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;301(7):113863.
Hu Y, Chen Y, Zheng Y, You C, Tan J, Hu L, Zhang Z, Ding L. Factors related to mental health of inpatients with COVID-19 in Wuhan, China. Brain Behav Immun. 2020;89:587–93.
Dryman MT, Heimberg RG. Emotion regulation in social anxiety and depression: a systematic review of expressive suppression and cognitive reappraisal. Clin Psychol Rev. 2018;65(11):17–42.
Gross JJ, Jazaieri H. Emotion, emotion regulation, and psychopathology: an affective science perspective. Clin Psychol Sci. 2014;2(4):387–401.
Acknowledgements
The authors would like to thank all the participants for taking part in the study.
Funding
This study was funded by the Education Reform Research Project of Army Medical University (Grant Number:2019B25), the Clinical Technology Innovation Promotion Project of Army Medical University (Grant Number: CX2019JS211), the Talent Pool Key Support Object of Army Medical University Excellent (Grant Number: 2019R044), and the Program of Shaanxi Provincial Science and Technology Department (Grant Number: 2021JQ-783).
Author information
Authors and Affiliations
Contributions
Conceptualization and funding acquisition, H.Y., and G.M.Z; methodology, H.Y., and H.L.; formal analysis, C.J., and X.Y.J; investigation and data curation, L.L., Z.L., H.X., and Z.Q.L. writing—original draft preparation, H.Y., and X.Y.J.; writing—review and editing, H.Y., and X.Y.J; visualization, H.X.; supervision and project administration, S.J.G. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors have no competing interests as defined by BMC, or any other interests that could be perceived as influencing the results and/or discussion reported in this paper.
Ethics approval and consent to participate
The study was conducted in accordance with ethical guidelines and was approved by the Medical Ethics Committees of the Second Affiliated Hospital of Army Medical University (No.2022-332-01). Prior to their participation, all participants were fully informed about the study’s details and provided written informed consent. The study procedures adhered to the principles outlined in the Declaration of Helsinki.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
He, Y., Huang, L., Chen, J. et al. Mental health status and related influencing factors in patients with COVID-19. BMC Psychol 11, 225 (2023). https://doi.org/10.1186/s40359-023-01254-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40359-023-01254-8