Abstract
Background
Eating disorders (EDs) are severe mental illnesses associated with significant morbidity and mortality. EDs are more prevalent among females and adolescents. Limited research has investigated Canadian trends of ED hospitalizations prior to the COVID-19 pandemic, however during the pandemic, rates of ED hospitalizations have increased. This study examined rates of ED hospitalizations among children and youth in Canada from 2010 to 2022, by sex, age, province/territory, length of stay, discharge disposition and ED diagnosis.
Methods
Cases of ED hospitalizations among children and youth, ages 5 to 17 years, were identified using available ICD-10 codes in the Discharge Abstract Database from the 2010/11 to 2022/23 fiscal years. The EDs examined in this study were anorexia nervosa (F50.0), atypical anorexia nervosa (F50.1), bulimia nervosa (F50.2), other EDs (F50.3, F50.8) and unspecified EDs (F50.9). Both cases of total and first-time ED hospitalizations were examined. Descriptive statistics and trend analyses were performed.
Results
Between 2010/11 and 2022/23, 18,740 children and youth were hospitalized for an ED, 65.9% of which were first-time hospitalizations. The most frequent diagnosis was anorexia nervosa (51.3%). Females had significantly higher rates of ED hospitalization compared to males (66.7/100,000 vs. 5.9/100,000). Youth had significantly higher rates compared to children. The average age of ED hospitalization was 14.7 years. Rates of ED hospitalizations were relatively stable pre-pandemic, however during the pandemic (2020–2021), rates increased.
Interpretation
Rates of pediatric ED hospitalizations in Canada increased significantly during the pandemic, suggesting that there may have been limited access to alternative care for EDs or that ED cases became more severe and required hospitalization. This emphasizes the need for continued surveillance to monitor how rates of ED hospitalizations evolve post-pandemic.
Plain English summary
Eating disorders disproportionally affect children and youth, however, literature investigating long-term trends of eating disorder hospitalizations among children and youth in Canada is limited. We conducted a retrospective surveillance study, examining eating disorder hospitalizations among children and youth in Canada, from 2010 to 2022, by sex, age group, geography and eating disorder diagnosis. More than half of eating disorder hospitalizations examined during our study period were first-time hospitalizations. The most common eating disorder diagnoses were anorexia nervosa, followed by unspecified eating disorders. Youth had higher rates of eating disorders compared to younger children and females had higher rates compared to males. In Canada, rates of pediatric eating disorder hospitalizations increased during the pandemic. These results emphasize the need for continued surveillance to monitor how ED hospitalizations evolve post-pandemic, as well as prioritizing early intervention and treatment to help reduce the number of children and youth requiring hospitalization.
Similar content being viewed by others
Background
Eating disorders (EDs) are life-threatening mental illnesses with some of the highest mortality rates among psychiatric disorders [1,2,3,4]. EDs often co-occur with other psychiatric or medical disorders, adding to treatment complexity [5]. Generally, EDs are characterized by disturbances in eating behaviours and preoccupation with body appearance and weight; however, these concerns vary by gender, age and ED diagnosis [2, 6]. EDs can occur across gender, age and sociodemographic groups. [2, 6, 7]
EDs are more prevalent among females [6, 8, 9]. Research estimates that the lifetime prevalence of anorexia nervosa (AN) is up to 4% in females and 0.3% in males, whereas the prevalence of bulimia nervosa (BN) can be up to 3% in females and 1% in males [7, 10]. Surveillance studies indicate that the prevalence of EDs in younger children (less than 11 years) is low, however estimates vary [11, 12]. The age of onset differs across EDs; AN is more frequent in adolescence (16–19 years) and rarely diagnosed after the age of 30 [10, 11, 13,14,15]. However, the age of onset of AN has decreased during the past decade, with some of the youngest reported cases now seen among children under the age of 10 [2, 8, 13,14,15]. The prevalence of BN onset is higher in young adults (20–29 years), with more cases continuing to be diagnosed into adulthood [14]. EDs can be difficult to treat, especially if not identified early and treated within the first three years of symptom onset [2, 16, 17].
Recent research has shown that the COVID-19 pandemic has contributed to an increase in ED hospitalizations among children and youth [17,18,19,20,21]. This increase may have resulted from changes in everyday routine, online schooling, social isolation and loneliness, increased social media use and disruptions to regular medical care [17, 22, 23].
Although there is research examining EDs in the pediatric population in Canada during the COVID-19 pandemic, there is minimal research examining long-term trends of ED hospitalizations. Ongoing surveillance of EDs is needed to identify changes in the prevalence and characteristics of existing and new patients requiring hospitalization. This can help inform future resource needs in hospitals as well as prioritize alternative forms of care that patients can access. Lastly, understanding how trends in ED hospitalizations changed during the pandemic compared to pre-pandemic can aid in future pandemic planning and post-pandemic recovery [17]. The objective of this study was to examine rates of ED hospitalizations among children and youth in Canada by age, sex, year, geography, length of stay, discharge disposition and ED diagnosis from 2010 to 2022.
Methods
Data sources and case selection
This work utilized the Discharge Abstract Database (DAD), a national administrative database managed by the Canadian Institute for Health Information (CIHI), which collects clinical and administrative information on hospital separations/discharges from all provinces and territories, excluding Quebec. This study did not include Quebec due to the Public Health Agency of Canada’s (PHAC) data sharing agreements with CIHI. This study was based on de‐identified data and conducted under PHAC’s surveillance mandate, therefore no ethics approval from an Institutional Review Board was necessary. The results of this study are reported in accordance with the Reporting of studies Conducted using Observational Routinely-collected Data guidelines [24].
This study analyzed acute care inpatient hospital discharge records. Uncertain and secondary ED diagnoses were excluded. These are diagnoses where there may have been some uncertainty and an exact diagnosis could not be provided or when the diagnosis was deemed non-significant to the episode of care.
The DAD uses the International Statistical Classification of Diseases and Related Health Problems, 10th revision, Canada (ICD-10) to classify diagnoses [25,26,27]. ED diagnoses were categorized with the following ICD-10 codes: AN (F50.0), atypical anorexia nervosa (AAN) (F50.1), BN (F50.2), other EDs (F50.3 and F50.8) and unspecified EDs (F50.9). The F50.8 code includes binge eating disorder, avoidant/restrictive food intake disorder (ARFID) and other EDs, however, we were unable to parse out these diagnoses from the F50.8 code as medical institutions in Canada do not specify the exact diagnosis in this category.
Figure 1 summarizes the inclusion criteria of pediatric patients in our cohort. To identify ED hospitalizations during the study period, all 25 diagnostic fields in the DAD were searched from 2010 to 2022 using the selected ICD-10 codes. To minimize misclassification, patients with two or more ED diagnostic codes reported in a single episode of care (n = 88) were recategorized using the most responsible diagnostic code. In cases where this was not possible, patients were excluded (n = 18, 0.1%). Other ICD-10 codes related to disordered eating behaviours (F50.4, F50.5, F98.2, F98.3 and R63.0, R63.2 to R63.6) were not included in this study, as these codes are primarily used when diagnosing feeding disorders or indicating signs and symptoms concerning food intake.
Using the prevalence cohort, we identified first-time ED hospitalizations during the study period, using the patient’s scrambled health card number. A total of 8,933 patients had only one hospitalization during the study period and 3,343 patients had multiple hospitalizations. Among those with multiple hospitalizations, only the first documented hospitalization was included. Additionally, health card numbers were searched in a pre-study period (2001–2009) to ensure that patients were not hospitalized prior to our study period. Patients who also had an ED hospitalization in the pre-study period were not included as having a first-time hospitalization during the study period. The years 2001 to 2009 were selected as the pre-study period, as this was the earliest data available using ICD-10 coding. We analyzed first-time ED hospitalizations to compare how characteristics of first-time hospitalization differed from total hospitalizations, especially in-terms of length of stay, discharge disposition, age at hospitalization and ED diagnosis.
Study population and time period
ED hospitalizations were searched over a 13-year period starting in the 2010/11 fiscal year and ending in the 2022/23 fiscal year, beginning on April 1st and ending on March 31st the following year. Only patients between the ages of 5 and 17 years, inclusive, at the time of discharge were included.
Statistical analyses
Results of total and first-time ED hospitalizations were presented as rates, proportions, means and medians, by sex, age group, province/territory, discharge disposition, hospital length of stay and ED diagnosis. Age and sex-specific rates per 100,000 population were calculated, using Statistics Canada national population estimates (excl. QC), over the 13-year period (2010/11 to 2022/23). Age-standardized rates per 100,000 population were standardized to the 2011 Canadian population (excl. QC) by direct standardization. Annual trends were quantified using average annual percent change (AAPC). Age-standardized rates that have significantly changed over the study period, were identified by an AAPC that is significantly different from zero at the alpha = 0.05 level [28]. Linear regression was used to calculate the mean change in length of hospital stay and age at hospitalization during the study period.
SAS EG version 7.1 (SAS Institute Inc., Cary, NC, USA) was used to conduct all descriptive analyses. Joinpoint Regression Program version 5.0.2 (SEERStat, NCI, Bethesda, MD, USA) was used to conduct trend analyses. Cells with small counts between one and four as well as rates that would allow for calculation of small cells have been presented as a range, to reduce potential identification of individuals and comply with CIHI’s data sharing agreements.
Results
Between 2010/11 to 2022/23, there were 18,740 total cases of ED hospitalizations among children and youth, of which, 12,159 (64.9%) patients had a first-time hospitalization for an ED. About half of the total (51.3%) and first-time (47.3%) ED hospitalization cases were diagnosed as AN. Females and males had similar distributions of ED diagnoses, however, males had a higher proportion of other EDs among both total (Male: 23.3% vs. Female: 8.7%) and first-time hospitalizations (Male: 25.5% vs. Female: 9.6%), compared to females (Additional file 1: Table A1).
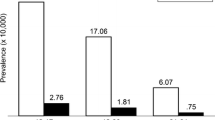
Across all ED diagnoses, females had significantly higher rates of total (Female: 66.7/100,000 vs. Male: 5.9/100,000) and first-time (Female: 42.7/100,000 vs. Male: 4.4/100,000) ED hospitalizations compared to males (Table 1). Youth ages 11 to 17 years had significantly higher rates of ED hospitalizations compared to children ages 5 to 10 years.
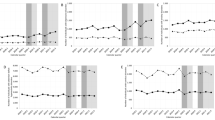
The average age of total ED hospitalizations among children and youth was 14.7 (95% CI: 14.7, 14.7) years and among first-time ED hospitalizations was 14.6 (95% CI: 14.5, 14.6) years. Youth aged 15 and 16 years had the highest rates of first-time and total ED hospitalizations, respectively. (Fig. 2 a & b). Males had significantly earlier average ages (years) of total [Male: 14.0 (95% CI: 13.9, 14.1) vs. Female: 14.8 (95% CI: 14.8, 14.8)] and first-time [Male: 13.9 (95% CI: 13.8, 14.0) vs. Female: 14.6 (95% CI: 14.6, 14.6)] ED hospitalizations. During the study period, the average age of ED hospitalizations significantly decreased, for total cases (2010: 14.8 years vs. 2022: 14.5 years, p < 0.05) and first-time cases (2010: 14.7 years vs. 2022: 14.4 years, p < 0.05).
a and b. Age-specific rates of ED hospitalizations among children and youth, 2010/11 to 2022/23, by diagnosis Data source: Discharge Abstract Database 2010/2011–2022/23. Abbreviations: ED, eating disorder Hospitalization data with small counts between one and four as well as rates that would allow for derivation of small counts have been presented as a range
Between 2010/11 and 2022/23, there was an overall significant increase in total and first-time ED hospitalizations. Rates of total ED hospitalizations increased from 17.7 cases per 100,000 population in 2010/11 to 52.8 cases per 100,000 in 2022/23, this corresponds to an AAPC of 7.8% (3.9, 12.8) (Fig. 3a). Similarly, rates of first-time ED hospitalizations increased from 10.7 to 32.0 cases per 100,000, with an AAPC of 7.5% (3.7, 12.5) (Fig. 3b). Among total ED hospitalization cases, a relative increase of 108.0% occurred from 2010/11 to 2013/14, followed by relatively stable ED hospitalizations between 2013/14 and 2019/20. Between 2019/20 and 2021/22, cases increased again by 84.5%, followed by a decline of 16.5% in 2022/23. Although total ED hospitalization cases began to decline in 2022/23, they remained higher than pre-pandemic (2019/20) (Fig. 3a). Similar trends were observed among first-time ED hospitalization cases with a significant increase from 2010/11 to 2013/14 and from 2019/20 to 2021/22 (Fig. 3b). Although during the study period, there is year-to-year variation in rates of total and first-time ED hospitalizations, overall trends have increased across each ED diagnosis (Additional file 1: Table A2).
a and b. Age-standardized rates of total and first-time ED hospitalizations among children and youth, 2010/11 to 2022/23, by year and diagnosis Data source: Discharge Abstract Database 2010/2011–2022/23. Abbreviations: CI, confidence interval; AAPC, average annual percent change; ED, eating disorder. Notes: Age-standardized rates per 100,000 population are standardized to the 2011 Canadian population (excl. Quebec) using direct standardization
Ontario and British Columbia had significantly higher rates of total and first-time ED-hospitalizations whereas Nova Scotia, New Brunswick, Manitoba, Saskatchewan, Alberta and Northwest Territories all had significantly lower rates, compared to the rest of Canada (Fig. 4).
Crude rates of ED hospitalizations, 2010/11 to 2022/23, by provinces and territories Data source: Discharge Abstract Database 2010/2011–2022/23 Abbreviations: ED, eating disorder. Notes: The rate for each province/territory was compared to the national rate minus the province/territory being compared. *P < 0.05 Hospitalization data with small counts between one and four as well as rates that would allow for derivation of small counts have been presented as a range
Among cases of total and first-time ED hospitalizations, those diagnosed with AN had a significantly longer average length of stay (LOS) compared to all other EDs examined (Table 2).
From 2010 to 2022, the LOS for total and first-time ED hospitalizations significantly declined. Patients hospitalized for an ED were most frequently discharged home, either with or without support services (Table 3). Fewer patients were transferred to other inpatient hospital care, left against medical advice, were transferred to continuing care or died while in care.
Discussion
In Canada between 2010/11 and 2022/23 there were 18,740 ED hospitalizations among children and youth, with 64.9% being first-time hospitalizations. The majority of ED hospitalizations in Canada were among females and youth. The rates of total and first-time ED hospitalizations significantly increased during the study period, with the highest rates reported in 2021. Across Canada, Ontario and British Columbia had the highest rates of ED hospitalizations.
Rates of ED hospitalizations were significantly higher among females compared to males, across all ages and diagnoses, in our study. Higher rates of EDs among females is well documented in the literature, however, there are still a considerable number of males with EDs [6, 8, 9, 11, 12, 15, 20, 29]. The distribution of ED diagnoses was similar between males and females in our study, however, males had a higher proportion of other EDs compared to females. This difference may be due to males not meeting the diagnostic criteria or having different clinical presentations for EDs, and therefore are being captured in the other ED category [9, 29, 30].Additionally, males are more likely than females to present with ARFID [29,30,31,32,33], which falls into our category of other EDs.
Youth had significantly higher rates of ED hospitalizations compared to children in our study. Throughout adolescence the rates of ED hospitalizations increased, with a peak at ages 15 and 16 years. The age at onset for most EDs occurs during adolescence (ages 14 to 18) [2, 8, 13, 15, 34], however, several studies have reported that the age of onset for many EDs has decreased over the past decade, with more children under the age of 10 years being diagnosed [2, 8, 13,14,15]. In our study, the mean age for an ED hospitalization significantly decreased from 2010 to 2022, with the lowest average ages seen during the pandemic period. There are many factors that may influence the shifting age at hospitalization, including changes to cultural or personal norms, earlier access to social media, and participation in weight or body-image centered sports/activities [2, 3, 8, 14]. During the pandemic, children spent more time at home, which may have led to caregivers being more aware of the child’s eating behaviours and cognition, potentially resulting in earlier encounters with the healthcare system [21, 35]. Males in our study were hospitalized for an ED at significantly younger ages than females. Some research confirms this finding [11, 15], whereas other studies report no clear sex-differences of age of onset [7, 31]. Additionally, males are more frequently diagnosed with ARFID, which is an ED that is typically diagnosed earlier than AN or BN, [29,30,31,32,33] which may explain the younger age of hospitalization among males in our study.
Our trend analysis showed an initial increase in ED hospitalizations from 2010/11 to 2013/14 after which, trends remained stable until 2019/20, followed by a spike from 2020/21 to 2022/23. In 2013, the Diagnostic and Statistical Manual of Mental Disorders (DSM), was updated, with several changes made to the ED diagnostic criteria [36]. Although ICD-10 codes did not change during this time, physicians base their diagnoses on the criteria in the DSM-5. The new, broader criteria in the DSM-5 may have lead to more patients being diagnosed with AN and fewer patients being diagnosed with unspecified EDs, around that time [36, 37]. Several studies highlight the increase in ED cases during the pandemic period [18,19,20,21, 35, 38,39,40]. Results have shown that hospitalization rates for EDs in 2022 started to decline, but are still higher than pre-pandemic [21, 38, 41]. This trend may be due to public health measures such as lockdowns and school closures causing increased isolation [17, 18], as well as longer wait times or changes to treatment during the pandemic [17]. Additionally, it is reported that during the pandemic, there was an increased preoccupation with fitness, weight gain and social media, which may have contributed to new cases of disordered eating, as well as worsening symptoms among those already diagnosed [42]. These results, emphasize the need for early screening and monitoring of children and youth presenting with disordered eating behaviours, in order to implement early and consistent treatment, which may aid in minimizing cases of inpatient hospitalization for EDs.
Across provinces/territories, Ontario and British Columbia had significantly higher rates of both total and first-time ED hospitalizations. There is limited Canadian research examining ED epidemiology at the provincial/territorial level, however one recent study, of five provinces, noted that hospitalizations for EDs were higher in hospitals in Ontario, Quebec and British Columbia compared to hospitals in Alberta and Newfoundland and Labrador [18]. Inequitable access to specialized hospital-based ED units across Canadian provinces/territories may in part explain hospitalization patterns in British Columbia and Ontario, where there is greater accessibility to specialized ED units compared to the rest of the country (excluding Quebec) [43].
Patients hospitalized for AN had significantly longer average LOS compared to those hospitalized for other EDs. We found that from 2010 to 2022, the average LOS for patients with an ED decreased significantly. Among the limited research available on hospital LOS, results vary from about 12 days to over 200 days, [44,45,46] with LOS decreasing over the last several years [44]. Several factors such as presence of comorbid conditions, severity of the ED, hospital resources, access to outpatient treatments and the COVID-19 pandemic may have an influence on LOS [44, 45]. The majority of patients in our study were discharged home following hospitalization. One study found that more than half of patients were discharged to a medical practitioner, and about 20% were referred to outpatient care. [47]
Limitations
This study has several limitations inherent to administrative data. The DAD is unable to report sociodemographic characteristics or gender, which would have strengthened our study as certain population groups are disproportionately affected by EDs [17, 48]. Results from Quebec could not be reported due to data sharing agreements. Lastly, our results may be biased towards more severe ED cases, as we only captured acute inpatient hospitalizations.
There may be some misclassification of first-time ED hospitalizations. Scrambled health card numbers were used to identify ED hospitalizations across Canada between 2001 and 2022. This method creates challenges in identifying patients who may have received a new health card number during this time.
Additionally, we were unable to present disaggregated results for ARFID and binge eating disorder, due to the limited ICD-10 codes for EDs. The codes available do not capture the full spectrum of ED presentations and several diagnoses are grouped together.
Conclusion
In Canada, between 2010 and 2022, hospitalizations for EDs in the pediatric population increased significantly, with the highest rates reported in 2021. Females and youth comprised the majority of ED hospitalizations. Currently limited research is available, at a national level, examining long-term trends. These results highlight the need for early interventions and screening as well as resource reallocation and preparedness for future pandemics. Further work will explore types of co-occurring diagnoses with EDs, as well as examine how trends are evolving in the post-pandemic era.
Availability of data and materials
Access to programming code and aggregated data can be made available upon request through the corresponding author.
References
Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders A meta-analysis of 36 studies. Arch Gen Psychiatry. 2011;68(7):724–31. https://doi.org/10.1001/archgenpsychiatry.2011.74.
Treasure J, Duarte TA, Schmidt U. Eating disorders. Lancet. 2020;395(10227):899–911. https://doi.org/10.1016/S0140-6736(20)30059-3.
Moskowitz L, Weiselberg E. Anorexia nervosa/atypical anorexia nervosa. Curr Probl Pediatr Adolesc Health Care. 2017;47(4):70–84. https://doi.org/10.1016/j.cppeds.2017.02.003.
Iwajomo T, Bondy SJ, de Oliveira C, Colton P, Trottier K, Kurdyak P. Excess mortality associated with eating disorders: population-based cohort study. Br J Psychiatry. 2021;219(3):487–93. https://doi.org/10.1192/bjp.2020.197.
Hambleton A, Pepin G, Le A, Maloney D, Aouad P, Barakat S, et al. Psychiatric and medical comorbidities of eating disorders: findings from a rapid review of the literature. J Eat Disord. 2022;10(1):132. https://doi.org/10.1186/s40337-022-00654-2.
Wu J, Liu J, Li S, Ma H, Wang Y. Trends in the prevalence and disability-adjusted life years of eating disorders from 1990 to 2017: results from the Global Burden of Disease Study 2017. Epidemiol Psychiatr Sci. 2020;29:e191. https://doi.org/10.1017/S2045796020001055.
van Eeden AE, van Hoeken D, Hoek HW. Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry. 2021;34(6):515–24. https://doi.org/10.1097/YCO.0000000000000739.
Herpertz-Dahlmann B, Dahmen B. Children in need—diagnostics, epidemiology, treatment and outcome of early onset anorexia nervosa. Nutrients. 2019;11(8):1932. https://doi.org/10.3390/nu11081932.
Murray SB, Nagata JM, Griffiths S, Calzo JP, Brown TA, Mitchison D, et al. The enigma of male eating disorders: a critical review and synthesis. Clin Psychol Rev. 2017;1(57):1–11. https://doi.org/10.1016/j.cpr.2017.08.001.
Hoek HW, van Hoeken D. Review of the prevalence and incidence of eating disorders. Int J Eat Disord. 2003;34(4):383–96. https://doi.org/10.1002/eat.10222.
Javaras KN, Runfola CD, Thornton LM, Agerbo E, Birgegård A, Norring C, et al. Sex- and age-specific incidence of healthcare-register-recorded eating disorders in the complete swedish 1979–2001 birth cohort. Int J Eat Disord. 2015;48(8):1070–81. https://doi.org/10.1002/eat.22467.
Murray SB, Ganson KT, Chu J, Jann K, Nagata JM. The Prevalence of Preadolescent Eating Disorders in the United States. J Adolesc Health. 2022;70(5):825–8. https://doi.org/10.1016/j.jadohealth.2021.11.031.
Volpe U, Tortorella A, Manchia M, Monteleone AM, Albert U, Monteleone P. Eating disorders: what age at onset? Psychiatry Res. 2016;30(238):225–7. https://doi.org/10.1016/j.psychres.2016.02.048.
Steinhausen HC, Jensen CM. Time trends in lifetime incidence rates of first-time diagnosed anorexia nervosa and bulimia nervosa across 16 years in a danish nationwide psychiatric registry study. Int J Eat Disord. 2015;48(7):845–50. https://doi.org/10.1002/eat.22402.
Micali N, Hagberg KW, Petersen I, Treasure JL. The incidence of eating disorders in the UK in 2000–2009: findings from the general practice research database. BMJ Open. 2013;3(5): e002646. https://doi.org/10.1136/bmjopen-2013-002646.
Vo M, Golden N. Medical complications and management of atypical anorexia nervosa. J Eat Disord. 2022;10(1):196. https://doi.org/10.1186/s40337-022-00720-9.
Devoe D, Han A, Anderson A, Katzman DK, Patten SB, Soumbasis A, et al. The impact of the COVID-19 pandemic on eating disorders: a systematic review. Int J Eat Disord. 2023;56(1):5–25. https://doi.org/10.1002/eat.23704.
Agostino H, Burstein B, Moubayed D, Taddeo D, Grady R, Vyver E, et al. Trends in the incidence of new-onset anorexia nervosa and atypical anorexia nervosa among youth during the COVID-19 pandemic in Canada. JAMA Netw Open. 2021;4(12): e2137395. https://doi.org/10.1001/jamanetworkopen.2021.37395.
Otto AK, Jary JM, Sturza J, Miller CA, Prohaska N, Bravender T, et al. Medical admissions among adolescents with eating disorders during the COVID-19 pandemic. Pediatrics. 2021;148(4): e2021052201. https://doi.org/10.1542/peds.2021-052201.
Asch DA, Buresh J, Allison KC, Islam N, Sheils NE, Doshi JA, et al. Trends in US patients receiving care for eating disorders and other common behavioral health conditions before and during the COVID-19 pandemic. JAMA Netw Open. 2021;4(11): e2134913. https://doi.org/10.1001/jamanetworkopen.2021.34913.
Toulany A, Kurdyak P, Guttmann A, Stukel TA, Fu L, Strauss R, et al. Acute care visits for eating disorders among children and adolescents after the onset of the COVID-19 pandemic. J Adolesc Health Off Publ Soc Adolesc Med. 2022;70(1):42–7. https://doi.org/10.1016/j.jadohealth.2021.09.025.
Schlissel AC, Richmond TK, Eliasziw M, Leonberg K, Skeer MR. Anorexia nervosa and the COVID-19 pandemic among young people: a scoping review. J Eat Disord. 2023;11(1):122. https://doi.org/10.1186/s40337-023-00843-7.
Muth L, Leven KH, Moll G, Kratz O, Horndasch S. Effects of the COVID-19 restrictions on eating behaviour and eating disorder symptomology in female adolescents. Int J Environ Res Public Health. 2022;19(14):8480. https://doi.org/10.3390/ijerph19148480.
Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12(10): e1001885. https://doi.org/10.1371/journal.pmed.1001885.
International Statistical Classification of Diseases and Related Health Problems: Tenth Revision, Canada. 2018.
Canadian Institute for Health Information. Codes and Classifications [Internet]. [cited 2023 Mar 20]. Available from: https://www.cihi.ca/en/submit-data-and-view-standards/codes-and-classifications
Canadian Institute for Health Information. Discharge Abstract Database metadata (DAD) [Internet]. [cited 2023 Mar 20]. Available from: https://www.cihi.ca/en/discharge-abstract-database-metadata-dad
National Cancer Institute. Average Annual Percent Change (AAPC) and Confidence Interval [Internet]. [cited 2023 Mar 20]. Available from: https://surveillance.cancer.gov/help/joinpoint/setting-parameters/method-and-parameters-tab/apc-aapc-tau-confidence-intervals/average-annual-percent-change-aapc#:~:text=Average%20Annual%20Percent%20Change%20(AAPC)%20is%20a%20summary%20measure%20of,in%20trends%20during%20those%20years.
Gorrell S, Murray SB. Eating disorders in males. Child Adolesc Psychiatr Clin N Am. 2019;28(4):641–51. https://doi.org/10.1016/j.chc.2019.05.012.
Kinasz K, Accurso EC, Kass AE, Le Grange D. Does sex matter in the clinical presentation of eating disorders in youth? J Adolesc Health. 2016;58(4):410–6. https://doi.org/10.1016/j.jadohealth.2015.11.005.
Timko CA, DeFilipp L, Dakanalis A. Sex differences in adolescent anorexia and bulimia nervosa: beyond the signs and symptoms. Curr Psychiatry Rep. 2019;21(1):1. https://doi.org/10.1007/s11920-019-0988-1.
Sanchez-Cerezo J, Nagularaj L, Gledhill J, Nicholls D. What do we know about the epidemiology of avoidant/restrictive food intake disorder in children and adolescents? A systematic review of the literature. Eur Eat Disord Rev. 2023;31(2):226–46. https://doi.org/10.1002/erv.2964.
Couturier J, Gayowsky A, Findlay S, Webb C, Sami S, Chan A, et al. A diagnostic subgroup comparison of health care utilization patterns in individuals with eating disorders diagnosed in childhood and/or adolescence. Int J Eat Disord. 2023. https://doi.org/10.1002/eat.24024.
Canadian Paediatric Surveillance Program: 2022 Results [Internet]. Ottawa (ON): Canadian Paediatric Surveillance Program; [cited 2023 Sep 8]. Available from: https://cpsp.cps.ca/uploads/publications/CPSPResults22.pdf
Auger N, Steiger H, Luu TM, Chadi N, Low N, Bilodeau-Bertrand M, et al. Shifting age of child eating disorder hospitalizations during the Covid-19 pandemic. J Child Psychol Psychiatry. 2023;64(8):1176–84. https://doi.org/10.1111/jcpp.13800.
Lindvall Dahlgren C, Wisting L, Rø Ø. Feeding and eating disorders in the DSM-5 era: a systematic review of prevalence rates in non-clinical male and female samples. J Eat Disord. 2017;5(1):56. https://doi.org/10.1186/s40337-017-0186-7.
Fisher M, Gonzalez M, Malizio J. Eating disorders in adolescents: how does the DSM-5 change the diagnosis? Int J Adolesc Med Health. 2015;27(4):437–41. https://doi.org/10.1515/ijamh-2014-0059.
Trafford AM, Carr MJ, Ashcroft DM, Chew-Graham CA, Cockcroft E, Cybulski L, et al. Temporal trends in eating disorder and self-harm incidence rates among adolescents and young adults in the UK in the 2 years since onset of the COVID-19 pandemic: a population-based study. Lancet Child Adolesc Health. 2023;7(8):544–54. https://doi.org/10.1016/S2352-4642(23)00126-8.
Vyver E, Han AX, Dimitropoulos G, Patten SB, Devoe DJ, Marcoux-Louie G, et al. The COVID-19 pandemic and canadian pediatric tertiary care hospitalizations for anorexia nervosa. J Adolesc Health. 2023;72(3):344–51. https://doi.org/10.1016/j.jadohealth.2022.07.003.
Giacomini G, Elhadidy HSMA, Paladini G, Onorati R, Sciurpa E, Gianino MM, et al. Eating disorders in hospitalized school-aged children and adolescents during the COVID-19 pandemic: a cross-sectional study of discharge records in developmental ages in Italy. Int J Environ Res Public Health. 2022;19(20):12988. https://doi.org/10.3390/ijerph192012988.
ICES. Mental Health Dashboard [Internet]. Mental Health Dashboard. [cited 2023 Sep 9]. Available from: https://www.ices.on.ca/dashboards/mental-health-dashboard/
Fernández-Aranda F, Casas M, Claes L, Bryan DC, Favaro A, Granero R, et al. COVID-19 and implications for eating disorders. Eur Eat Disord Rev. 2020;28(3):239–45. https://doi.org/10.1002/erv.2738.
Allen KL, Mountford VA, Elwyn R, Flynn M, Fursland A, Obeid N, et al. A framework for conceptualising early intervention for eating disorders. Eur Eat Disord Rev. 2023;31(2):320–34. https://doi.org/10.1002/erv.2959.
Kim M, Holton M, Sweeting A, Koreshe E, McGeechan K, Miskovic-Wheatley J. Using health administrative data to model associations and predict hospital admissions and length of stay for people with eating disorders. BMC Psychiatry. 2023;23(1):326. https://doi.org/10.1186/s12888-023-04688-x.
Morris J, Simpson AV, Voy SJ. Length of stay of inpatients with eating disorders. Clin Psychol Psychother. 2015;22(1):45–53. https://doi.org/10.1002/cpp.1865.
Kan C, Hawkings YR, Cribben H, Treasure J. Length of stay for anorexia nervosa: systematic review and meta-analysis. Eur Eat Disord Rev. 2021;29(3):371–92. https://doi.org/10.1002/erv.2820.
Li A, Cunich M, Miskovic-Wheatley J, Maloney D, Madden S, Wallis A, et al. Factors related to length of stay, referral on discharge and hospital readmission for children and adolescents with anorexia nervosa. Int J Eat Disord. 2021;54(3):409–21. https://doi.org/10.1002/eat.23399.
Simone M, Telke S, Anderson LM, Eisenberg M, Neumark-Sztainer D. Ethnic/racial and gender differences in disordered eating behavior prevalence trajectories among women and men from adolescence into adulthood. Soc Sci Med. 2022;1(294): 114720. https://doi.org/10.1016/j.socscimed.2022.114720.
Acknowledgements
The authors would like to thank Anne-Marie Robert, Murray Weeks, Annalise Ferro and Jingxuan Zhang for their contributions throughout the course of the project.
Funding
Open Access funding provided by Health Canada. This study did not receive any funding.
Author information
Authors and Affiliations
Contributions
All authors conceived and designed the study. ST conducted the analysis and drafted the manuscript. ST and SRM provided interpretation of results. DK and EV provided clinical expertise throughout the project. All authors have reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no competing interests to disclose. The content expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Proportion of ED hospitalizations, by sex and diagnosis.
Additional file 2
. Age-standardized rates of ED hospitalizations, by year and diagnosis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Toigo, S., Katzman, D.K., Vyver, E. et al. Eating disorder hospitalizations among children and youth in Canada from 2010 to 2022: a population-based surveillance study using administrative data. J Eat Disord 12, 3 (2024). https://doi.org/10.1186/s40337-023-00957-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40337-023-00957-y