Abstract
Background
Psychotherapy is considered central to the effective treatment of eating disorders—focusing on behavioural, psychological, and social factors that contribute to the illness. Research indicates psychotherapeutic interventions out-perform placebo, waitlist, and/or other treatments; but, outcomes vary with room for major improvement. Thus, this review aims to (1) establish and consolidate knowledge on efficacious eating disorder psychotherapies; (2) highlight select emerging psychotherapeutic interventions; and (3) identify knowledge gaps to better inform future treatment research and development.
Methods
The current review forms part of a series of Rapid Reviews published in a special issue in the Journal of Eating Disorders to inform the development of the Australian-government-funded National Eating Disorder Research and Translation Strategy 2021–2031. Three databases were searched for studies published between 2009 and 2023, published in English, and comprising high-level evidence studies (meta-analyses, systematic reviews, moderately sized randomised controlled studies, moderately sized controlled-cohort studies, and population studies). Data pertaining to psychotherapies for eating disorders were synthesised and outlined in the current paper.
Results
281 studies met inclusion criteria. Behavioural therapies were most commonly studied, with cognitive-behavioural and family-based therapies being the most researched; and thus, having the largest evidence-base for treating anorexia nervosa, bulimia nervosa, and binge eating disorder. Other therapies, such as interpersonal and dialectical behaviour therapies also demonstrated positive treatment outcomes. Emerging evidence supports specific use of Acceptance and Commitment; Integrative Cognitive Affective; Exposure; Mindfulness; and Emotionally-Focused therapies; however further research is needed to determine their efficacy. Similarly, growing support for self-help, group, and computer/internet-based therapeutic modalities was noted. Psychotherapies for avoidant/restrictive food intake disorder; other, and unspecified feeding and eating disorders were lacking evidence.
Conclusions
Currently, clinical practice is largely supported by research indicating that behavioural and cognitive-behavioural psychotherapies are most effective for the treatment of eating disorders. However, the efficacy of psychotherapeutic interventions varies across studies, highlighting the need for investment and expansion of research into enhanced variants and novel psychotherapies to improve illness outcomes. There is also a pressing need for investigation into the whole range of eating disorder presentations and populations, to determine the most effective interventions.
Plain English Summary
Evaluating the efficacy of treatment options for eating disorders (EDs) is important and necessary to inform both treatment guidelines and clinical practice. However, treatment outcomes in studies, and in clinical practice, can vary widely. Therefore, this review aimed to pool evidence related to a wide range of psychological treatments to help better understand what gaps in treatment need to be addressed. Using a rapid review method, three academic databases were searched, and 281 articles were identified and analysed. Results indicated that cognitive-behavioural approaches had the most evidence for well-defined EDs (such as anorexia nervosa, bulimia nervosa, and binge eating disorder). However, little research was found on other types of EDs. There was emerging evidence that provided support for self-help, group, and computer/internet-based therapies. Overall, the findings highlighted that more research is required on novel eating disorder treatments beyond what is currently available and being used as ‘gold standard’.
Similar content being viewed by others
Introduction
Eating disorders (EDs) are serious mental illnesses with significant psychiatric and medical morbidity and mortality [1]. They are one of the most challenging of the mental illnesses to treat, attributed primarily to their complex biopsychosocial aetiology, ego-syntonic features and resistance to treatment [2]. Psychotherapy, or talk therapy, is a first-line treatment intervention for EDs as it targets psychological and social factors that contribute to disease onset and maintenance [3].
The mechanisms underlying ED symptomatology and diagnoses are multi-factorial, leading to a range of potential therapeutic targets [4]. EDs encompass a broad range of diagnostic presentations requiring different therapeutic foci and, as such, some psychotherapies have been adapted according to specific ED diagnoses in order to provide a more focussed treatment [4]. Independent variables considered critical in the development and maintenance of EDs represent potential therapeutic targets. Psychotherapies target maladaptive behaviours, personality traits and negative affect, which typically span the ED spectrum [4].
Significant advancements to psychotherapeutic interventions for EDs have been made over the past 2 decades, and an extensive evidence base evaluating their efficacy has developed [5]. However, these advances are relative in that they represent some, but not profound, improvements in the effectiveness of available treatments, which may still be improved further. This is particularly important to consider in the context of clinical outcomes, health system resourcing, and research funding which significantly relies on the evidence-base to make informed-decisions and to inform policy.
Results from randomised controlled trials (RCTs) are often used to determine which treatments are recommended in national guidelines. The UK’s National Institute for Clinical Excellence (NICE) [6] guidelines for EDs, consistent with other international guidelines [5, 7], endorse enhanced cognitive-behavioural therapy (CBT-E), Maudsley Anorexia Treatment for Adults (MANTRA) and specialist supportive clinical management (SSCM) for adult Anorexia Nervosa (AN), and family-based therapy (FT-AN) for children and adolescents with AN. For the treatment of adult Bulimia Nervosa (BN), BN-focused guided self-help programs incorporating cognitive-behavioural self-help materials supplemented with brief supportive sessions are recommended. For child and adolescent BN, BN-focused family therapy (FT-BN) is suggested as the primary treatment. For treating Binge Eating Disorder (BED) in adults and children, a BED-focused guided self-help program utilising cognitive-behavioural materials and brief supportive sessions is the recommended approach. For Other Specified Feeding and Eating Disorder (OSFED) and Unspecified Feeding or Eating Disorder (UFED), evidence-based recommendations cannot be made according to NICE guidelines due to a lack of research. In the absence of adequate evidence, NICE suggests a consideration of the presenting symptoms and application of the recommended therapy for the ED it most closely resembles. The guidelines do not provide recommendations for the treatment of Avoidant Restrictive Food Intake Disorder (ARFID).
Despite substantial research into ED aetiology and pathology, few theories have been translated into effective interventions [3]. Considering high rates of relapse among individuals with an ED, and an estimated 50% of cases progressing to a severe and enduring illness, the low efficacy of current treatments is concerning [8]. This is further compounded by the high rates of treatment drop-out commonly observed among patients with an ED [9]. Thus, the current review aims to (1) establish and consolidate the evidence-base of psychotherapies and efficacy for treating eating disorders in order to understand the ED treatment landscape; and (2) identify gaps in research and highlight emerging treatments that warrant further research investment.
Methods
Overview and rationale
The Australian Government funded the InsideOut Institute for Eating Disorders (IOI) to develop the Australian Eating Disorders Research and Translation Strategy 2021–2031, [10] in partnership with state and national stakeholders including clinicians, service providers, researchers, and experts by lived experience (including consumers and families/carers). Developed through a 2-year national consultation and collaboration process, the strategy provides the roadmap to establishing EDs as a national research priority and is the first disorder-specific strategy to be developed in consultation with the National Mental Health Commission. To inform the strategy, IOI commissioned Healthcare Management Advisors (HMA) to conduct a series of rapid reviews (RRs) to broadly assess all available peer-reviewed literature on the six DSM-5 listed EDs.
A RR Protocol [11] was utilised to swiftly synthesise evidence in order to guide public policy and decision-making [12]. This approach has been adopted by several leading health organisations including the World Health Organisation [10] and the Canadian Agency for Drugs and Technologies in Health Rapid Response Service [13], to build a strong evidence base in a timely and accelerated manner, without compromising quality. A RR is not designed to be as comprehensive as a systematic review—it is purposive rather than exhaustive and provides actionable evidence to guide health policy [14].
Search strategy
The RR is a narrative synthesis and follows the PRISMA guidelines [15]. It is divided by topic area and presented as a series of papers. Three research databases were searched: ScienceDirect, PubMed and Ovid/Medline. To establish a wide understanding of the progress made in the field of psychotherapeutic approaches in EDs, the search strategy and eligibility criteria were kept relatively broad.
Eligibility criteria
Therefore, included studies were published between 2009 and 2023, in English, and conducted within Western healthcare systems or health systems comparable to Australia in terms of structure and resourcing. The initial search and review process was conducted by three reviewers between 5 December 2019 and 16 January 2020. The search was re-run for dates spanning 16 January 2020 until 28th January 2023 and was conducted by two reviewers.
Study sampling and included studies
The RR had a translational research focus with the objective of identifying evidence relevant to developing optimal care pathways. Searches therefore used a Population, Intervention, Comparison, Outcome (PICO) approach to identify literature relating to population impact, prevention and early intervention, treatment, and long-term outcomes. Discretionary, purposive sampling predominantly focused on high-level evidence studies such as: meta-analyses; systematic reviews; moderately sized randomised controlled studies (RCTs) (n > 50); moderately sized controlled-cohort studies (n > 50), and population studies (n > 500). However, the diagnoses ARFID and UFED necessitated a less stringent eligibility criterion due to a paucity of published articles. As these diagnoses are newly captured in the DSM-5 (released in 2013, within the allocated search timeframe), the evidence base is emerging and fewer studies have been conducted. Thus, smaller studies (n ≤ 20) and narrative reviews were also considered and included. Grey literature, such as clinical or practice guidelines, protocol papers (without results) and Masters’ theses or dissertations, was excluded. Other sources (which may not be replicable when applying the current methodology) included the personal libraries of authors. This extra step was conducted in line with the PRISMA-S: an extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews [16].
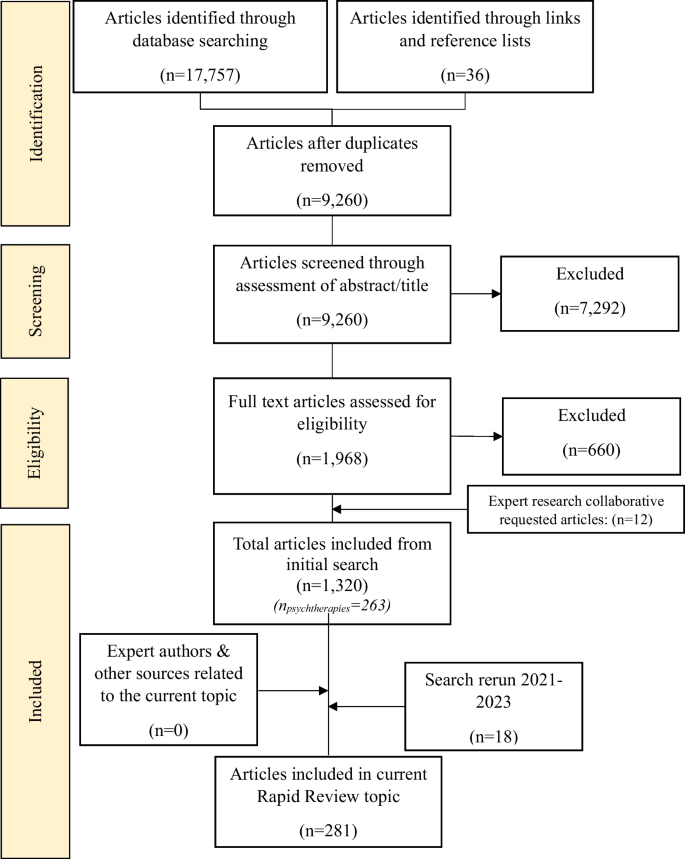
Full methodological details including eligibility criteria, search strategy and terms and data analysis are published in a separate protocol paper due to the broad scope of the RR, which included a total of 1320 initial studies [17] (see Fig. 1 for PRISMA flow diagram). Data from included studies relating to psychotherapies were synthesised and are presented in the current review.
Results
The search identified 281 studies for inclusion in this paper (see Fig. 1 and Table 2). The proceeding section will (1) overview the characteristics of studies found and highlight the most common ED treatment approaches found by the current review; (2) summarise the key findings of the studies; and (3) outline particular psychotherapies targeting specific EDs. Results are presented in the following order: (1) study characteristics and a summary of key findings; (2) overview of common individual-based psychotherapies across a number of eating disorders; (3) an examination of groups-based therapies and (4) technology-based interventions; and finally, (5) an overview of interventions for carers supporting someone living with an ED.
Study characteristics
Studies focusing on cognitive behavioural therapy (CBT) comprised the largest proportion (30%), followed by family based therapy (FBT) (12%), exposure-based therapies (5%), interpersonal therapy (IPT), dialectical behaviour therapy (DBT), acceptance and commitment therapy (ACT), integrative cognitive affective therapy (ICAT) (all 3%), and other psychotherapies, including mindfulness, emotionally-focused, self-compassion, self-identification, motivational interviewing (MI) and body movement and awareness therapies (2%). Studies investigating self-help, group and technology-based psychotherapy delivery modalities were also included.
Differences in body mass index (BMI), Eating Disorder Examination (EDE) [18], global scores, ED psychopathology, maintenance mechanisms and affect measured pre- and post-treatment were the most commonly measured treatment outcomes. The majority of studies investigated outcomes for the client, who were predominantly female, adult, clinical populations in outpatient settings (Table 1).
A small proportion of included studies (7%) examined therapeutic outcomes for the carer of someone with an ED and the indirect effect on client outcomes. A full list of included studies is available in Table 2. Results are divided into three sections: (1) psychotherapies, (2) psychotherapeutic delivery modalities, and (3) carers. Within some of the psychotherapies, results are sub-divided into ED presentations AN, BN, BED, ARFID, OSFED and UFED. A summary of key findings can be found in Table 1.
Psychotherapies
Cognitive behavioural therapy
A total of 30 studies were identified as providing evidence for the efficacy of CBT, the highest number of any psychotherapy in the RR. Of the psychotherapies, CBT has been the most rigorously scrutinised and therefore has the most empirical evidence [162]. Much of the research on CBT has been conducted with individuals with BN and BED, such that CBT utilising a manualised treatment [18] is generally considered the leading psychotherapy for BN (CBT-BN) [162].
Development of CBT has resulted in an enhanced form (CBT-E), delivered either as a version that focuses exclusively on ED psychopathology (CBT-Ef), or a broad form (CBT-Eb) that also targets mood intolerance, perfectionism, self-esteem and interpersonal difficulties [18, 81, 167]. Evidence suggests that CBT may help to reduce binge/purge symptomatology and support regular eating [69, 167]. Furthermore, CBT has been proposed to have clinical utility as a transdiagnostic intervention for multiple diagnoses including AN and BN in general [69, 167]; as well as for more specific AN subtypes such as AN-binge purge (AN-BP), and for EDs in the presence of comorbidities, such as personality disorders [69, 167]. It should be noted that in RCTs examining this type of CBT intervention across ED diagnostic categories, a significantly greater number of sessions are required for CBT for AN compared with CBT for BN. Studies have also generally been based in outpatient settings; and thus, predominantly recruited participants with AN and a BMI at or above 14.5 [163] so it is unclear whether this treatment works across the AN spectrum to include those with a BMI below 14.5.
Several studies have identified the importance of the therapeutic alliance on the effectiveness of CBT on treatment outcomes. Establishing a good therapeutic alliance increased chances of weight recovery for patients with AN, with 80% of the cohort achieving target weight [290]. Strong therapeutic alliance in a group of adolescents with BED was associated with fewer loss of control eating episodes [215]. Additionally, in a group of participants with BN, stronger alliance was related to a greater reduction in bulimic behaviours, regardless of the treatment [integrative cognitive-affective therapy (ICAT) or CBT-E] [21]. In a group of patients with severe and enduring AN, positive therapeutic alliance established later in treatment predicted reductions in ED and depressive symptoms, which was considered to be particularly significant due to the treatment resistant nature of the disorder [248].
Other studies have produced conflicting results; therapeutic alliance in a group of patients with BN was not shown to be associated with treatment outcomes achieved from CBT-E [219]. It was suggested that although therapeutic alliance was strong throughout treatment, it was not a reliable predictor of patient drop-out or reduction in ED symptoms. In another study, therapeutic alliance was unable to predict a reduction in ED symptoms for adults with AN, BN and OSFED [266]. Daniel et al. [71] and Folke et al. [92] have suggested that individual attachment style plays a role in therapeutic alliance in patients with BN, with secure attachment being associated with stronger therapeutic alliance; however, the impact of alliance and attachment on reduction in ED symptomologies was limited.
Another study examining the relationship between therapeutic alliance and weight gain during CBT for AN found that early alliance was not related to subsequent weight gain, albeit early and late weight gain were positively associated with the strength of subsequent alliance, suggesting that weight gain techniques should be focused on early in treatment rather than rely on the therapeutic alliance to action change [45].
Anorexia nervosa
In people with AN, CBT has been shown to positively impact emotional regulation, increase set-shifting skills, improve ED pathology, lower global EDE scores, reduce subjective feelings of incompetence and, in combination with nutritional rehabilitation, produce significant weight gain [68, 132, 254, 289]. Despite established evidence of its efficacy, researchers consider a need for more RCTs using larger sample sizes to not only determine the generalisability of effectiveness across a much broader representation of the general population; but to further understand CBTs efficacy in treating different sub-types of the same disorder [162]. One specific area of uncertainty reflects the differences in underlying symptomatology between anorexia nervosa-restricting (AN-R) and anorexia nervosa-binge-eating/purging (AN-BP) subtypes, such that CBT show differential efficacy across subtypes. For example, CBT was delivered to outpatients for 40 weeks, with significant reductions in emotional eating scores for participants with AN-BP and BN post-treatment, but no significant change in those with AN-R; this differential effect was sustained at 6-year follow up [87].
A recent meta-analysis assessing the efficacy of stand-alone psychological interventions for adult outpatients with AN on change in BMI and clinical symptoms, did not find CBT or any of the treatments to outperform TAU [238]. Further, no reliable evidence demonstrated clear superiority or inferiority of a specific treatment, underscoring an urgent need to develop and improve psychotherapies for adults with AN [238]. In an RCT, comparison of CBT-E to active comparators focal psychodynamic therapy (FPT) and optimised TAU found no significant differences in weight gain at post-treatment and 12-month follow-up, although both therapies were more effective than TAU [78]. Zipfel et al. [289] suggested that the equivalent benefit derived from FPT is due to its less directive approach, which is sensitive to difficulties in autonomy experienced by individuals with AN.
In the UK, research into the applicability of outpatient CBT in ‘real-world’ settings for AN and Atypical-Anorexia Nervosa (A-AN), found treatment to be efficacious, with just under half of the study sample achieving full or partial remission, in the short-term, at end of treatment [132]. A systematic review from 2012 conducted on psychotherapeutic treatments for severe and enduring AN highlighted the limited evidence base for CBT as a treatment for AN over the long-term [116]. Research has shown that while specialist ED psychotherapy may have some advantage over TAU, long-term outcomes for AN and BN patients treated with CBT-E is far from adequate, with long-term remission rates far lower than short-term remission [291, 292].
With the recognition of body shape and weight being a core pathological feature of EDs, a phenomenological perspective has emerged which describes a disorder of embodiment [227]. The embodiment disorder has been posited as a combination of apprehension towards the physical form of the body and a loss of experiencing the body from within; instead, drawing on others perceptions to determine how on sees and experiences their own body [227]. A study investigating the role of the embodiment disorder as a possible mediator of CBT-E efficacy on ED symptomatology found that higher presence of embodiment disorder predicted diagnostic instability and mediated the decrease in overall ED psychopathology [227]. These findings highlight the role of disordered embodiment as a maintaining factor and possible contributor to enduring EDs, supporting an integration of CBT-E with the phenomenological perspective, which may serve to increase remission rates.
Bulimia nervosa and binge eating disorder
CBT has consistently outperformed active, inactive, and pharmacological treatment trials of BN and BED [162,163,164]. CBT-BN has demonstrated the ability to decrease binge/purge behaviours by reducing dietary restraint and normalising eating behaviour or reducing weight/shape concern resulting in a decreased desire to diet [167]; it has also been shown to have a positive impact on emotional regulation [180], self-esteem [168] and reduction of negative feelings such as depressive symptoms [114, 152, 164, 168, 254, 290].
A systematic review of CBT for BN and BED included comparisons with active psychotherapy alternatives and demonstrated superiority of CBT in terms of efficacy and long-term effects, when there was adherence to the CBT manual and protocol [162]. Findings reinforce those of an earlier meta-analysis of 53 studies, whereby CBT outperformed other therapies (IPT, group therapy, and FBT) for both BN and BED [114, 239], and of a systematic review of seven CBT-E studies the efficacy of CBT-E for BED as well as transdiagnostic EDs was supported [73].
An outpatient study sought to determine the efficacy of CBT for individuals with BN and Subclinical Bulimia Nervosa (S-BN, classified as OSFED) [282]. Findings supported the contention that CBT is equally efficacious in ‘real-world’ clinical settings as in RCTs [282]. Testing of ‘real-world’ efficacy was also conducted using a larger sample size of individuals with BN and OSFED accessing NHS services with significant improvements observed at post-treatment in terms of global EDE scores [148].
An RCT examining the effectiveness of CBT-BN and psychodynamic therapy (PDT) for adolescents with BN or S-BN found both interventions to be beneficial to patients, with no significant differences in remission rates between intervention groups [242]. Assessment of EDE scores also found binge/purge behaviours to be significantly reduced at post-treatment and 12-month follow up for both groups, with medium to large effect sizes.
Post-treatment binge/purge abstinence rates have been found to be maintained over long-term follow-up periods for CBT-BN compared with other psychotherapies [167]. A meta-analysis of 27 studies found that delivery of CBT resulted in a binge-purge abstinence rate of 42.1% for treatment-completers and 34.6% in an intention-to-treat analysis [167]. At follow-up, mean abstinence rates were 47.3%. Linardon et al. [167] considered these rates to be comparable to results reported by RCTs and therefore findings from RCTs to be applicable in real-world treatment settings. Individuals with more severe binge/purge symptomatology are considered to respond better to CBT and CBT-E through the targeting of self-esteem as a factor for disorder maintenance [283].
A reduction in binge/purge frequency and depressive symptoms in response to CBT at 4 weeks has been associated with a greater chance of remission at discharge among BN patients [261]. However, some studies have indicated that CBT does not improve feelings of shame and self-criticism [95], and it was not able to demonstrate superiority over other psychotherapies for improving self-esteem or reducing depression symptoms in either BN or BED patients [114, 168]. Gale et al. [95] argued that integration of Compassion-Focused Therapy (CFT) into CBT treatment may be effective in targeting these additional aspects of EDs, leading to better outcomes for patients with AN, BN and Eating Disorder Not Otherwise Specified (EDNOS).
A rapid response to treatment is associated with favourable outcomes in individuals with EDs [31, 271, 276], supporting the application of CBT for this cohort, amongst whom it has demonstrated rapid response in a number of trials. For example, a brief CBT intervention was added to routine outpatient ED treatment to facilitate rapid response among women with BN and Purging Disorder (PD) and was highly effective when compared to motivational interviewing (MI); there was no significant difference between MI and TAU [177]. After 4 weeks, 95.6% of patients receiving CBT had responded to treatment compared with 71.4% of patients in the MI group.
Conversely, a comparison of CBT to motivational enhancement therapy (MET), a form of MI, performed in a clinical outpatient setting during a two-phase RCT found no significant difference for patients with BN and OSFED in terms of benefit, treatment adherence, or self-monitoring [144].
A RCT of 154 individuals with BN or OSFED compared efficacy of focused CBT-E (CBT-Ef) to broad CBT-E (CBT-Eb) and found no significant differences between the interventions at post-treatment or 60-week follow-up; showing efficacy in reducing eating pathology scores, though CBT-Eb should be the default treatment due to ease of delivery [18]. However, CBT-Ef was found to be more effective for individuals with less severe Borderline Personality Disorder (BPD), comorbid with BN; while CBT-Eb produced better results in individuals with more severe BPD [262].
Length of treatment may be an influencing factor, with individuals with BED receiving up to 16 weeks of treatment showing the greatest reduction in binge eating symptoms compared to participants receiving up to 8 weeks of treatment [30]. A comparison of CBT-E to IPT for individuals with BN, BED and other EDs found that whilst both groups displayed significant improvements, participants receiving CBT-E had significantly higher rates of remission at 60-week follow up [82]. Both CBT and IPT have been found to be effective transdiagnostically across EDs in the long-term, and individuals who receive CBT tend to have faster response rates to treatment [82].
A meta-analysis of 21 RCTs assessing treatment options for adults with BN suggested individualised CBT, specifically developed for EDs, continues to be the most efficacious treatment in terms of its ability to achieve full remission in patients, followed by guided CBT self-help [236]. Research into the cost-effectiveness of CBT-BN for treatment of adults in Australia, including manualised treatment [18] delivered by a clinical psychologist, was deemed to be 98% cost-effective [156].
Benefits of participating in CBT interventions have been shown to be maintained long-term, as demonstrated in studies at 2 years [214] and 6 years [194] post-treatment. In the study by Poulsen et al. [214], CBT-E for BN was compared to psychoanalytic therapy specifically developed for individuals with BN. At 2-year follow-up, 44% of participants receiving CBT-E had stopped engaging in binge/purge behaviours compared with 15% of participants who received psychoanalytic therapy. Similarly, delivery of CBT to obese individuals with BED resulted in significant remission at 6-year follow-up as their improvement was maintained compared to pre-treatment scores [194]. However, no significant differences were observed between the group receiving CBT and the group receiving behavioural weight loss therapy (BWLT), suggesting equivalent efficacy of both interventions in the treatment of individuals with BED [194]. Comparative advantage of CBT over BWLT at 6-year follow-up was observed for CBT in terms of fewer binge eating episodes and although participants who received the BWLT had a lower BMI at post-treatment, the BMI reduced more in CBT compared to BWLT during follow-up [194].
Despite evidence regarding the superiority of CBT over other available treatments for BN and BED, non-response to treatment in some individuals has prompted the development of novel therapies. An RCT conducted on a sample of women with transdiagnostic binge eating compared traditional CBT for EDs, an appetite focused CBT (CBT-A)—which incorporates strategies for dietary normalisation and food education—and schema therapy, a form of CBT that focuses on early life exposures and their contribution to ED psychopathology [189]. All interventions were able to produce significant reductions in frequency of binge eating; however, those diagnosed with BED rather than BN, showed greater symptom reduction. No significant differences were observed between interventions at post-treatment or follow-up, indicating equivalent efficacy. Treatment of transdiagnostic binge/purge behaviours using CBT-E was also found to be effective in a sample of adolescents, with half of all participants abstaining from any binge/purge behaviours post-treatment and a significant reduction in global EDE scores [262].
Sodersten et al. [237] argue that there has been little improvement in outcomes of CBT over time despite expansion of the intervention to target other emotional aspects of EDs. The authors present the argument that normalisation of eating patterns and behaviours is a critical component of successful CBT and greater focus is required on the behavioural aspects of BN during treatment rather than the emotional and cognitive aspects that appear to be at the forefront of current CBT treatments. Conversely, a study found that people with BN have central coherence and set-shifting inefficiencies which do not differ from those with AN [145]. This suggests that BN patients may benefit from adjunctive approaches, such as cognitive remediation therapy (CRT) to address these inefficiencies [145].
Unsatisfactory outcomes for CBT for some individuals with BN may indicate a need to better tailor treatment to the different personality structures in such individuals. This was assessed in an RCT examining the efficacy of CBT-E against integrative cognitive affective therapy for BN (ICAT-BN) [82]. Results indicated that over-controlled personality types, associated with elevated shyness, self-consciousness and perfectionism, responded more favourably to CBT-E. Patients with an under-controlled personality type, linked to a lack of impulse control, aggression and emotional dysregulation, exhibited lower rates of purging following ICAT-BN [82]. Assessment of mechanisms of action for psychotherapy interventions based on personality traits was investigated by Daniel et al. [71], who compared CBT to Positive Psychotherapy (PPT) and found that attachment styles were strongly associated with binge frequency. However, no significant differences were found between treatment groups for changes in attachment styles or binge frequency at post-treatment.
Additionally, difference in response to CBT has been observed between genders. Analysis of response to CBT by sex in a sex-balanced sample of patients with EDs found that males with BN or OSFED were more likely to achieve remission than females with the same diagnosis. However, males with BN were also more likely to drop out of treatment than females [236].
Behavioural weight loss therapy in integrated approaches
Studies have shown that CBT when compared to BWLT can reduce binge eating frequency, but not weight in patients with BED [49, 184, 194]. Pacanowski et al. [199] found some BED patients gained weight when treated with CBT despite decreases in psychological ED symptomatology. Other studies have been unable to demonstrate any significant differences between CBT and BWLT groups in treatment outcomes [109, 194, 200].
Mason et al. [185] conducted an RCT comparing CBT to a waitlist control for patients with BED. It was found that whilst CBT was effective in targeting psychosocial aspects and ED symptomatology, integration of exercise therapy led to improved weight loss and subsequent improvement in weight-related quality of life (QoL) [185]. Integration of physical activity and CBT interventions to treatment of patients with BED was supported by evidence from a systematic review which indicated that exercise may decrease food cravings and negative affect, increasing the efficiency of CBT treatment [37].
A recent RCT compared the efficacy of introducing a BWLT—the Health Approach to Weight Management and Food in Eating Disorders (HAPIFED)—with CBT-E for the treatment of individuals with recurrent binge eating and BMI ≥ 27 kg/m2 [200]. A significant reduction in ED symptoms was observed in both the HAPIFED and CBT-E groups and was sustained at 12-month follow-up. No differences between groups were observed for weight loss; however, a greater reduction in purging behaviours and binge remission rates at 12-month follow-up were demonstrated with HAPIFED.
Avoidant/restrictive food intake disorder
As a recently characterised disorder, ARFID has significantly less research than other EDs presented in this RR. Research on CBT as a treatment for ARFID is limited to case series, case reports and retrospective chart reviews, with only a few RCTs conducted on young children [258]. A protocol paper by Thomas and colleagues, describes the development of a modified CBT for ARFID in children, adolescents and adults, and an open trial which compares the therapy to FBT approaches [257].
A pilot trial titled “Supportive Parenting for Anxious Childhood Emotions adapted for ARFID” (SPACE-ARFID)[235] evaluated program outcomes related to a parent-based intervention for ARFID, which focusses on parent response to problematic eating and aims to increase food flexibility. Fifteen families of young people with ARFID aged 6–14 years old were recruited into the program. There was a 93% completion rate, high satisfactory rating of treatment, significant reductions in symptom severity, impairment and family accommodation, representing promising preliminary evidence for feasibility, acceptability, and potential for improvement in outcomes [235].
Other specified feeding or eating disorder
Although there is evidence to suggest that CBT may be an effective treatment for the full range of EDs due to its targeting of transdiagnostic symptomatologies, it is consistently under-researched for ‘non-core’ disorders [18, 204]. Only one publication was identified by the RR assessing the effectiveness of group CBT in a sample population of individuals with OSFED [204]. No studies were identified that addressed CBT treatment for Night Eating Syndrome (NED). In a longitudinal study of adolescents, Thompson-Brenner et al. [260] suggested a potential treatment gap for OSFED, as patients with this diagnosis were less likely to receive CBT than patients with AN or BN.
Family based therapy
Evidence for the effectiveness of FBT currently exists primarily for the treatment of adolescents with AN. Trials have been expanding and include protocols for new populations and diagnoses, including BN, with clinical guidelines now recommending an ED-specific FBT as the first-line treatment for adolescents with AN, and as a recommended intervention for adolescents with BN [100].
Four publications were identified relating to BN [59, 67, 196, 267], while no studies of FBT for the treatment of BED or ARFID were identified. Loeb et al. [172] argued that FBT’s targeting of family issues, including blame, internalisation of illness and parental response to the ED, suggests transdiagnostic utility, but further research in samples with diagnoses other than AN are required to evaluate this.
Researchers assessed studies on FBT (FT-AN and FT-BN) including multi-family therapy (MFT) and group therapy involving several families of individuals with AN or BN, finding that successful treatments: (1) use the family as a resource to promote changes in ED behaviours and symptomatology early on in treatment; (2) are delivered by clinicians with expertise in EDs, preferably within a multidisciplinary team; (3) are delivered in a consistent manner, ideally adhering to treatment manuals but remaining flexible enough to meet the individual needs of families; and (4) develop a therapeutic alliance with adolescents and parents, facilitating learning and behaviour modification [133].
Evidence from a systematic review of six RCTs assessing the effectiveness of FBT for adolescents with AN, BN and OSFED found that whilst no significant post-treatment differences were observed between FBT groups and those receiving individual treatment, FBT was superior at sustaining treatment effects for all EDs at 6 and 12-month follow-up [67].
A number of variations to the FBT protocol have been developed and have demonstrated varying treatment outcomes. Whilst most trials of adaptations to the traditional FBT format reported favourable outcomes for patients, Richards et al. found that very few of these studies used FBT as an active comparator; thus, limiting support for the efficacy of FBT protocol augmentations [222].
Anorexia nervosa
Guidelines indicate FBT is the leading treatment for AN, and suggest its use for the treatment of adolescents with other EDs [65, 67]. FBT has demonstrated effectiveness in reducing symptomatology following treatment for AN, sustained [65, 196, 293] at 6 and 12-month follow-up [171]. Decisive parental action and involvement early on in treatment have been associated with positive outcomes for restrictive type EDs [181]. Rapid response to treatment has been found to be strongly associated with a positive prognosis, with early weight gain predicting greater weight gain and remission at the end of treatment, as well as improvements in other ED measures [20].
Involvement of parents and siblings in FBT has been found to be associated with better outcomes, with results indicating that sustained involvement of fathers over a 6-month period was associated with higher rates of remission [65, 130]. To try to prevent poor outcomes in adolescents who did not have a rapid response to treatment following their first four sessions, Lock et al. [171] developed a novel adaptation to standard FBT. This treatment provides intensive coaching to parents on self-efficacy and refeeding, resulting in weight restoration at post-treatment comparable to rapid responders [171]. However, findings from this study are limited by a small sample size (n = 45), particularly the comparator group (n = 10) [171]. Whilst greater parental self-efficacy is a known predictor of favourable FBT outcomes, further research is required to understand the impact of intensive parental coaching on treatment response [225].
A variant of FBT, parent-focused therapy (PFT) in which sessions involve primarily parents with limited contact between the therapist and adolescent, was found by Le Grange et al. [160] to produce rapid response in adolescents with AN. At post-treatment, adolescents in the PFT group were three times more likely to achieve remission than those receiving FBT. These differences were no longer statistically significant between groups at 6- and 12-month follow-up despite higher remission rates for PFT compared to FBT. PFT therefore represents a viable alternative to FBT that can produce rapid response in adolescents with AN. However, findings indicate that it is not more effective than FBT in the longer-term [160].
Systemic family therapy (SyFT), a further variant of FBT, has a focus on the relationships and interactions present within the family system [22]. Unlike FBT, there is no family meal component or emphasis on normalisation of eating. Results from a randomised parallel study indicated no significant differences in outcomes between FBT and SyFT, suggesting they are equally effective. However, researchers noted that SyFT may be more effective in adolescents with more obsessive–compulsive symptomatology or comorbidity, known to predict lower response to treatment [22].
Increasing the effectiveness of FBT treatment through additional support provided by a network of families with children or adolescents undergoing treatment for AN is explored through multi-family therapy (MFT). In an RCT comparing FBT-AN to MFT-AN, benefits were observed in both groups at 18-month follow-up, with a significant difference in increases to BMI for the MFT-AN group [79].
A meta-analysis including 19 RCTs synthesised the best available evidence of non-pharmacological face-to-face interventions on BMI, body dissatisfaction, depression and anxiety among AN individuals [94]. Behavioural family system therapy (BFST) was found to be more effective than ego-oriented individual therapy in enhancing BMI, and conjoint family therapy (CFT) more effective than separated family therapy in reducing depression, with combined family and individual therapy producing larger effect sizes than individual therapy alone [94]. Conversely, results from RCTs consider FBT and adolescent-focused individual therapy (AFT) to be equally beneficial in terms of clinical outcomes relating to weight gain, reduction of ED behaviours, and depressive symptomatology [94, 130]. Based on results from a multi-site RCT, Le Grange et al. [158] argued that FBT is more effective than AFT for AN patients with more severe symptomatology. Moreover, FBT has been demonstrated as a cost-effective approach to treating adolescents with AN [20, 157].
A comparative analysis of psychotherapy modalities by Brauhardt et al. [40] found that the evidence supports the effectiveness of FBT over individual therapy for adolescents with EDs, but not adults. Similarly, a recent Cochrane Review [88] of FBT for AN included 25 trials in adults as well as adolescents and was also unable to find any significant benefit of the approach over other therapies, particularly in terms of achieved remission or weight gain [88].
ED drop-out rates are a significant issue, with up to 50% of inpatients and 57% of outpatients being treated for AN not completing FBT [102]. A systematic review and meta-analysis of 27 studies found that factors which predicted family therapy treatment drop-out in adolescents with AN included having AN-BP, low BMI, and low motivation, which should be assessed at commencement and actively addressed over the course of treatment [40]. These high dropout rates may reflect expert consensus that family therapies such as FBT are only suitable for some families and some presentations, and highlight the need to develop a number of alternate evidence-based therapies suitable for children and adolescents with AN.
Bulimia nervosa and binge eating disorder
Studies exploring BN-focused FBT are limited, and no studies investigating FBT for BED were identified as part of this RR. In an RCT comparing FBT-BN to CBT for adolescents (CBT-A), FBT-BN was found to be significantly superior to CBT-A at post-treatment and 6-month follow-up in terms of reducing bulimic symptomatology, with a significant proportion of the FBT-BN group abstinent from bingeing/purging compared with the CBT-A group [159]. There were, however, no significant differences at 12-month follow-up. These results indicate that FBT-BN has the capacity to produce a rapid response in adolescents with BN and it has been suggested that it may be a better alternative for individuals with more severe bulimic symptomatology [159].
Investigations into the impact of FBT for comorbid depression and self-esteem in the same sample population was published in a subsequent study [267]. Results indicated FBT-BN and CBT-A to be equally effective at reducing depressive symptomatology and increasing self-esteem in adolescents with BN without any significant differences between treatment groups at post-treatment or follow-up. Of note, depressive symptomatology was found to decrease in both treatment groups between post-treatment and 12-month follow-up [267]. These studies indicate that FBT-BN is a viable alternative to CBT for the treatment of BN in adolescents.
In an RCT, FBT was compared to individual focused supportive psychotherapy for patients with either BN or S-BN; the interventions were found to be equally efficacious in reducing ED symptoms including binge/purge frequency at end of treatment and 6-month follow-up [59].
A small study investigating an integrated FBT-DBT approach found promising results [274]. FBT-DBT targets emotional regulation aspects of BN and this is thought to mediate reduction in binge/purge symptomatology [274]. Although the intervention was able to produce significant reductions in bulimic symptomatology, it is a comprehensive and intensive treatment potentially only required in severe and complex cases. Findings are also limited by the small sample size, absence of a control group and follow-up data [274].
Avoidant restrictive feeding intake disorder
No published studies were identified that assessed FBT treatment for ARFID; however, several trials are currently being conducted [259]. FBT for ARFID is considered to work on the same premise as FBT-AN. In addition to the parent encouraging the child or adolescent to increase the volume of food consumed, a focus is also placed on the variety of foods eaten [259].
Other specified feeding eating disorders
Two studies [252, 293] were identified with a focus on FBT for adolescents with A-AN and restricting type ED symptomatology that were considered to be classified as either other OSFED or UFED. Results from these studies indicated that benefits for adolescents undergoing FBT were similar for both AN and A-AN. This is despite the primary goal of FBT being weight gain, with up to 52% remission and a significant reduction in EDE scores and purging behaviours post-treatment[293], and up to 53% remission and a significant reduction in EDE scores at 12-month follow-up [252].
Dialectical behavioural therapy
Originally developed to treat Borderline Personality Disorder (BPD), particularly symptoms relating to suicidality and self-harming behaviour [294], DBT has been adapted for the treatment of EDs with some success, in particular in the EDs with bingeing as core symptomatology. However, RCTs, particularly large RCTs, investigating the effectiveness of DBT are few [162] and some such studies have been uncontrolled [32].
Studies focusing on DBT and DBT adapted for BED (DBT-BED) have indicated that this approach may be successful in reducing the frequency of binge-eating [58, 217]. Sixty women with BED were provided 20 2-h sessions of DBT across 10 weeks, and results post-treatment showed a significant reduction in BMI and binge eating occurrences, as well as improvements to emotional regulation [217] Similarly, a study of 109 women with BN and BED were administered weekly DBT sessions over a 6-month period and improvements in ED symptomatology were observed for all participants at post-treatment. At 12-month follow-up those treated with DBT had significantly less objective binge eating than those in CBT guided self-help (CBTgsh) group [58].
Results from an open trial of DBT involving women with comorbid ED (AN and BN) and BPD who did not respond to previous, non-DBT oriented treatment, resulted in a remission rate of 54% in BN (fewer binge-eating episodes) and 33% with AN (increased weight) at 15-month follow-up; however, the study’s definition of ‘remission’ was not made clear [150]. Further, it should be noted that 44% of individuals with AN converted to BN at follow-up [150].
Development of an adapted DBT for BN was explored in a study which incorporated appetite awareness training (AAT) with DBT to produce appetite-focused DBT (DBT-AF) [171]. Compared to CBT—which monitors volume and type of food, AAT seeks to increase awareness of internal appetite signals [124]. In this study involving 32 women with BN and S-BN receiving DBT-AF for 12 weeks, positive results were observed at post-treatment, with 61% of participants achieving full remission, and 27% binge/purge abstinence compared to waitlist controls who reported higher objective binges/purges and higher scores on EDE-Q. However, the researchers draw specific attention to the limited sample size and suggest findings should be interpreted with caution [124].
Interpersonal therapy
Considered a less directive approach to therapy than CBT, IPT focuses on interpersonal problems and their relationship to psychological symptoms [295]. The IPT-ED model seeks to help the individual establish a sense of social acceptance that negates the need to engage in ED behaviours [223]. A small number of studies were identified relating to IPT for EDs. IPT is more commonly mentioned in the literature for EDs as an active comparator to CBT interventions. While this psychotherapy is considered a viable and effective treatment for EDs, many researchers consider CBT superior than IPT in producing rapid response, which may have led to a lack of recent research investigating this intervention [167].
In a recent systematic review on IPT for EDs, IPT was shown to be the least effective for AN in respect to overall global scores when compared with CBT and nonspecific SSCM at post-treatment [295]. However, at 5-year follow-up, those initially randomised to IPT demonstrated the greatest global outcome rating, with a “lag” effect occuring over time, with only 29% of the followed-up sample (n = 56) having accessed additional ED support in this period [296]. Similarly, following treatment, IPT was less effective than CBT-BN and behavioural therapy (BT) for reducing BN symptoms [295]. However, when participants were evaluated at 8-month follow-up, the IPT group showed further improvements [295]. Comparatively, BT was least effective overall with significant post-treatment relapse rates [295]. At 6-year follow-up, IPT and CBT-BN demonstrated equivalent and enduring reductions in general psychiatric features and improved social functioning/self-esteem [295, 296]. The results suggest efficacy for CBT-BN and IPT over the intermediate term (months), and particular advantages for IPT over the longer term (years).
A RCT investigated the efficacy of IPT in producing a rapid response in adults with BED, against two active comparators: BWLT and CBTgsh [122]. IPT was found to be the least effective of the interventions with 65% of participants showing a rapid response rate compared with 74% for CBTgsh and 73% for BWLT [122]. Rapid response in the CBTgsh group was found to predict greater remission in binge eating. However, this effect was not observed in the IPT or BWLT groups. These results indicate that although IPT is not effective in generating a rapid response to treatment in adults with BED, this has limited impact on its effectiveness in producing symptom remission [122].
A review of IPT-ED confirmed that while it can be recommended for BED and BN, IPT could not be recommended as a treatment for AN and identified a gap in the evidence regarding use of IPT for EDs not otherwise specified [195].
Acceptance and commitment therapy and integrative cognitive affective therapy
Juarascio et al. [136] presented the argument that ACT may be more effective than CBT at targeting key features contributing to ED maintenance, including experiential avoidance, awareness and lack of motivation to change, which are particularly relevant for individuals with AN. To test this proposed mechanism for behaviour change, Juarascio et al. [139] conducted an RCT in a sample of college students with diagnosed EDs or sub-clinical ED symptomatology, comparing ACT to CBT. While results from the trial indicated that ACT was more effective than CBT at reducing ED symptomatology, the study is limited by its delivery of non-manualised therapy and the very small number of individuals (n = 55) with a diagnosed disorder.
A subsequent RCT of ACT, in an inpatient ED setting had a more rigorous methodology, employed a TAU control, and included follow-up assessments [202]. This study was unable to demonstrate an advantage for ACT over TAU in reducing ED symptoms. While the intervention had a moderate effect on symptomatology, differences between groups did not reach statistical significance [202]. An additional comparison of ACT to TAU in an RCT was also unable to demonstrate the superiority of ACT over the control condition [202].
An RCT conducted by Wonderlich et al. assessed the efficacy of Integrative Cognitive-Affective Therapy (ICAT) for BN, delivered over 19 weeks [287]. ICAT proved to be as effective as CBT-E in producing a moderate to large effect on bulimic symptomatology, with no significant differences between groups as measured at post-treatment or follow-up. This finding was supported in a subsequent study by Peterson et al. where the treatment period was extended to 21 weeks [208].
Recognising the need for innovative treatments for BED, an RCT compared ICAT-BED with CBTgsh [209]. Binge eating frequency showed significant reductions post-treatment and at 6-month follow up, with no differences between therapy groups [209]. Maintenance mechanisms and measures of associated ED psychopathology, negative affect, depression and anxiety showed improvement post-treatment and at follow-up, with no differences between therapies. Treatment retention was significantly higher for ICAT-BED participants than for CBTgsh.
A subsequent RCT examined predictors and moderators of frequency of binge episodes associated with ICAT and CBTgsh for BED, finding the predictor actual-ideal self-discrepancy interacted with the treatment type to differentially predict binge episode frequency post-treatment and at 6-month follow-up [29]. Thus, ICAT-BED may produce specific and long-lasting improvements in binge frequencies among those with high actual-ideal self-discrepancy.
Exposure-based therapies
Exposure-based therapies work to establish, through experiential learning, that negative consequences do not occur when the individual is exposed to a feared stimulus [245]. These are not standalone treatments but often used in conjunction with other interventions, most commonly CBT, to increase the effectiveness of treatment and target aspects not covered by routine psychotherapy.
A recent systematic review on exposure interventions for AN, BN and BED included 60 studies on exposure and response prevention (ERP), mirror exposure, in vivo feared food exposure, family-based treatment with exposure, and virtual reality exposure therapy [47]. In vivo exposure to feared foods was found to increase caloric intake and BMI, and reduce state anxiety, although the research was limited. Likewise, mirror exposure regardless if conducted in the context of CBT treatment, was found to reduce body dissatisfaction and marginally improve binge/purge cues when treated using ERP compared with CBT [47]. However, a majority of these conclusions were based on lower-quality RCTs (n < 50), limiting their generalisability. In a separate study, Diaz-Ferrer et al. assessed the effectiveness of mirror exposure in patients with BN [75]. Results indicated that both guided and unguided or ‘pure’ mirror exposure had clinical utility for this group for reducing body dissatisfaction [75].
Evidence from other reviews have indicated that mirror and body exposure techniques in combination with CBT can help restructure negative beliefs in individuals with EDs [104, 245, 253]. A small RCT comparing ERP to Cognitive Remediation Therapy (CRT) in an inpatient group with AN found that ERP was significantly more effective at increasing participant food intake). A systematic review investigated the application of ERP strategies into treatment protocols and their effectiveness for binge eating [179]. Around 50% of those receiving CBT for binge eating fail to recover, identifying the need for this investigation to extend into additional exposure strategies. ERP was found to effectively reduce binge eating episodes in the included studies, with the effect sizes largest in samples with the most severe binge-eating behaviours.
Moreover, an ≥ 80% reduction in binge frequency occurred between pre- and post-treatment in studies utilising all relevant food cues, in-vivo exposure, occasional reinforcement and exposure practiced in multiple contexts [179]. Results suggested that ERP is more effective than self-control techniques and CBT without ERP, in reducing binge eating in the long term. This outcome was not evident in the short-term, suggesting that ERP may be effective when other treatments have not been successful [179], or may be reflective of longer-term trajectory of outcome of the treatment. Although in-vivo is the recommended method of exposure, ERP delivered through virtual reality (VR) demonstrated a reduction in binge eating by 90%, suggesting this as an effective alternative. However, more research is required comparing these forms of delivery [179].
An RCT sought to evaluate ERP for AN (AN-EXRP) as compared to Cognitive Remediation Therapy (CRT) for hospitalised patients who had restored weight to BMI > 18.5 kg/m2 with treatment outcome assessed by change in caloric intake [246]. Those receiving 12 sessions of AN-EXRP increased average test meal caloric intake from 352 ± 263 kcal to 401 ± 215 kcal post-treatment, while those who received CRT decreased from 501 ± 232 kcal at baseline to 424 ± 221 kcal post-treatment. This increase was significantly associated with improvement in eating-related anxiety.
A 5-year three-arm RCT explored the efficacy of an ERP intervention following treatment with CBT for 135 individuals with BN [188]. The intervention involved two variants of ERP: ERP-pre-binge and ERP-pre-purge; the third group received relaxation therapy following CBT treatment. At 5-year follow-up, both ERP treatments were significantly more effective at producing abstinence from bingeing behaviours compared to relaxation therapy. ERP was also able to reduce purging behaviours, although no significant differences were noted in abstinence rates for this behaviour. This indicates ERP is a useful add-on to routine CBT for BN patients to reduce long-term symptomatology.
The medication D-cycloserine, which has a role in neurotransmission, was thought by Levinson et al. [161] to enhance the benefits of ERP by increasing facilitated experiential learning. A trial supported the efficacy of D-cycloserine, with the active group receiving exposure therapy and pharmacotherapy gaining significantly more weight than the placebo group, who received therapy alone. It should, however, be noted that most people in this study were not underweight upon entering, with 81% having a BMI ≥ 18.5 [161].
The efficacy of approach bias modification (ABM) training as a novel intervention to reduce binge eating in patients with BN and BED has been investigated in an RCT [42]. Participants in the active group were taught to avoid food cues as a means of reducing reactivity to food in subsequent exposures. Results from the trial indicated a significant reduction in objective binge eating episodes with no difference between the active and ‘sham’Footnote 1 control group. However, larger reductions in other ED symptoms were observed in the active group compared to controls [42].
Other psychotherapy approaches
Several other psychotherapy approaches to treating EDs were identified in the RR. These included mindfulness, emotionally focused therapy, self-compassion, self-identification, motivational interviewing (MI), and body movement and body awareness therapies. With the exception of the systematic reviews on mindfulness-based therapies and MI (see below), much of the evidence presented is preliminary and from studies with small sample sizes and should be considered as requiring further examination of their potential use in EDs. Specifically, a cross-sectional study of Australians with diagnosed and undiagnosed EDs (n = 425) suggested that having more widely available and novel interventions for EDs would more likely encourage people to seek help [106].
Evidence from two reviews on mindfulness-based therapies [143, 198] support its capacity to reduce binge eating and emotional eating behaviours in individuals with obesity and BED. Approximately 90% of the mindfulness interventions reviewed by O’Reilly et al. [198] resulted in modest weight loss in participants. Similarly, Katterman et al. [143] reported moderate to large effects on measured binge eating frequency and superiority to BWLT, with no significant differences measured between treatment outcomes from mindfulness training and other active comparators, DBT and IPT.
There is evidence of efficacy for blended mindfulness, compassion and psychoeducation interventions in reducing ED and depressive symptoms in patients with BED compared with waitlist controls [211]. Also, compassion-focused therapies for individuals with BED showed a reduction in weekly binge days and eating and weight concerns compared to a control group [146]. An intervention incorporating aspects of CBT, IPT and DBT treating emotional dysregulation with BED or S-BED achieved significant reductions in ED symptoms as measured by the EDE-Q compared to waitlist controls, and were maintained at 12-month follow-up [60]. However, given the small sample size and a lack of supporting data from other studies using the same approach, further research is required to determine the clinical utility of this intervention. The efficacy of an emotional and social mind training program was assessed against group CBT for patients with BN, with global EDE scores not significantly different across treatment conditions [154].
A novel identity-based intervention was examined in an RCT involving 69 women with AN, A-AN, BN or S-BN [243]. The intervention was developed to target disturbances in self-concept and negative self-schemas common across these diagnoses [243]. The intervention was found to produce a significant reduction in drive for thinness in comparison with a supportive psychotherapy control group. However, no significant differences were observed between groups for other ED symptomologies.
Two RCTs conducted by Boerhaut et al. [38, 39] investigated a novel approach based on psychomotor therapies (brief body and movement-oriented intervention) used in other mental health interventions, such as the treatment of posttraumatic stress disorder. Both studies found significant reductions in ED symptomatology in the intervention group compared with TAU [38, 39]. Another study on body awareness-based strategies for EDs found that it reduced drive for thinness and body dissatisfaction in outpatients with EDs in comparison with outpatient controls [54].
Evidence from a systematic review of 13 studies assessing the use of MI approaches in ED treatment indicated that these interventions were effective at increasing ‘readiness to change’ among study participants [176]. Considering that resistance to treatment is common among individuals with EDs, incorporation of MI may work to increase initial treatment uptake and continued long-term improvement [77, 176]. A review of the effectiveness of motivational interviewing in the treatment of EDs did not find any significant benefits compared to TAU, although increased motivation to change was observed in participants with BED and BN [77].
Psychotherapy delivery modalities
Self-help
Self-help interventions can be delivered with therapist input, guided self-help (GSH), or independently—‘pure’ self-help. All studies identified describing self-help interventions targeted individuals with BN and BED or binge/purge OSFED subtypes. Recent clinical guidelines have recommended GSH as the first-line treatment for non-underweight EDs characterised by recurrent binge eating, namely BED and BN [34, 113]. Evidence for its efficacy in individuals with BED is particularly strong [53, 251, 265, 286]. Self-help interventions are not recommended in the treatment of AN due to the specialist care required for this disorder [286].
GSH is often briefer than traditional clinician-led therapy, and has been specifically developed to be used in non-specialist settings [46]. It has been suggested that the comparative advantages of self-help over therapist-led interventions include increased access, cost-effectiveness and capacity to be delivered by professionals without specialist knowledge in ED treatment [175]. However, an economic analysis of individual CBT compared to CBTgsh found only a non-significant difference in cost-effectiveness between the interventions, with both interventions having an estimated cost under the willingness to pay threshold of approximately $440 AUD per binge free day used in the study [149]. While individual CBT was associated with a slightly greater cost, it also resulted in a higher number of binge free days [149].
An RCT investigated the effectiveness and cost effectiveness of GSH via face-to-face delivery (fGSH), and a more scalable method, providing email support (eGSH) for adults with BED [131]. The primary outcome was improvement in ED psychopathology, and for cost-effectiveness, binge-free days. Both forms of GSH were superior to the waitlist control group in reducing psychopathology and binge eating, and both were cost-effective compared to control [131].
A systematic review and meta-analysis of self-help for BN and BED concluded that professional guidance significantly improved the efficacy of such interventions, with benefits derived primarily from increased program adherence and clinician specialisation in EDs resulting in higher treatment completion rates and larger effect sizes [34]. Evidence from meta-analyses and systematic reviews has found that therapist-led CBT achieves better results for individuals with BED [46].
In settings where there are access issues, CBTgsh can be offered as a first-line treatment [46, 273]. Some RCTs conducted using guided self-help based on CBTgsh have not found any significant differences when compared with full therapist-led individual CBT interventions [286]. ‘Pure’ self-help was not found to be effective compared to usual care in a study of obese individuals with BED [108]. The population involved in this study were from Culturally and Linguistically Diverse (CALD backgrounds, which may have had an impact on the findings. There is evidence to suggest that CBTgsh has demonstrated benefit within the CALD population who may benefit from additional culturally appropriate guidance [286].
Assessment of the efficacy of internet-based CBTgsh compared with traditional workbook CBTgsh found both interventions to be equally effective at reducing BN symptoms [279]. An earlier study of 155 women with BN produced similar findings regarding the comparative effectiveness of internet CBTgsh versus bibliotherapy [278]. Similarly, an RCT found that a digitally delivered CBT self-help intervention for binge-purge EDs was effective in decreasing overall ED psychopathology, compensatory behaviours, depression and clinical impairment compared to controls [89]. A study into attitudes toward online guided self-help among individuals with BN found that it was highly acceptable and identified weekly email, text message or forum support as the most preferred forms [187]. Comparison of CBTgsh with email support from therapists to an intensive outpatient program for BN and S-BN found that, although larger effect sizes were observed in the group receiving intensive face-to-face treatment, both interventions significantly reduced bulimic symptoms [126].
Self-help interventions targeting transdiagnostic binge/purge behaviours common to BN, BED and several OSFEDs have reported no significant differences in efficacy across diagnostic groups [218, 251, 265, 270, 271]. Higher drop-out rates have been observed in individuals with BN compared to BED, with findings of a systematic review and meta-regression suggesting that clinician-guidance during self-help treatment for BN may improve both treatment adherence and outcome [34]. Depending on diagnosis, differences in motivation to persist with self-help interventions may be related to change in weight [34]. Specifically, participants associated BED treatment with weight loss, whereas BN treatment was associated with weight gain [34]. A study investigating potential factors that may contribute to completion of treatment using GSH for BED found that non-completers experienced higher pre-treatment levels of weight concern and depression, and lower levels of general health and energy, with main reasons for discontinuing related to (1) perceptions of the GSH program; (2) program practicalities; and (3) the individuals readiness to change [135].
Investigation into predictors of outcome following CBTgsh for BN identified a need for greater focus on relapse prevention as part of the intervention. Results from this RCT of 87 individuals with BN found that increased global EDE scores at 6-month follow-up were associated with lower levels of binge eating, stress and positive thoughts about eating at post-treatment [240]. Further, it has been suggested that targeting perfectionism and motivation to change early on in ED treatment could lead to improved outcomes for individuals with BN and enhancing an early response to treatment has emerged as the most significant predictor of binge eating remission [240, 271].
Although GSH is not a recommended treatment for AN, it has clinical utility for this group as a tool for increasing engagement in routine treatment. Brewin and colleagues examined the effectiveness of Motivation and Psycho-educational guided self-help intervention for people with Eating Disorders (MOPED), an MI-based approach [41]. MOPED was unable to increase completion rates in patients with BN spectrum disorders (62%) compared to TAU (51%). However, among AN patients the intervention was highly effective, resulting in 63% of those receiving the GSH-MOPED intervention completing routine treatment compared with 29% of the TAU group. Another RCT assessing the utility of providing MI in addition to ‘pure’ self-help resulted in greater readiness to change and self-efficacy compared to the group receiving psychoeducation and self-help [272]. Both interventions were found to reduce binge eating in the study population.
Group therapies
The majority of group-based studies in this RR were in people with BED, indicating that group therapies may be more effective or acceptable for individuals with this disorder. Several studies were conducted on BED, BN, and subthreshold BED (e.g., OSFED) group treatment, with some promising results [221, 247].
Research findings are consistent regarding the effectiveness of CBT for reducing binge/purge behaviours in BN and BED with a considerable body of evidence supporting its delivery in a group format [24, 66, 134, 233]. Aguera et al. [24] noted that CBT delivered in a group format was considerably more effective for individuals with BED than those with BN, with 70% of BED participants achieving full remission compared with between 31 and 36% in the BN groups.
A study making direct comparison of individual and group CBT in patients with BED found that, while only individual CBT was able to reduce core ED symptoms such as weight/shape concern, both modalities achieved significant reductions in binge eating frequency, with similar rates of remission at 3-year follow-up. Variation in the length of active group CBT treatment has been found to contribute to remission rates. At 125-month follow-up > 99% of individuals receiving 16 sessions (CBT-L) achieving full remission compared with 64% of those receiving 8 sessions (CBT-S) [233].
In an analysis of the impact of group dynamics on treatment outcomes between therapist-led, therapist-assisted, GSH and group CBT, in a sample of individuals with BED, benefit was found for all intervention types, with no association between group dynamic and reduction in ED symptoms [212]. A separate analysis of the impact of group settings found benefit, specifically showing that participation in group IPT improved self-esteem for women with BED by reducing negative self-view through the feedback offered by other participants [96].
Meta-analyses investigating group therapies for BN have not found sufficient evidence to support the theory that group CBT has a clinical advantage over individual CBT or other therapies [213]. Research findings are consistent regarding the effectiveness of CBT for transdiagnostic binge/purge behaviours in BN and BED with a considerable body of evidence regarding its delivery in a group format [24, 66]. A CBT group intervention with incorporated physical activity counselling resulted in significantly increased physical activity and Health-Related Quality of Life (HRQoL) in participants, as well as significant reduction in binge eating frequency and BMI [269]. These results are encouraging, especially in light of HRQoL in obese patients with BED being consistently worse than in obese controls without BED and non-obese individuals [268]. However, the study did not include a control group, and large-scale RCTs are required.
In a study of patients with OSFED, Riesco et al. [224] assessed the effectiveness of group CBT and the potential impact of clinical heterogeneity on outcomes in women with A-AN, PD and S-BN. Participants were assigned to groups with a mix of diagnoses. Between 10 and 22% of participants achieved full remission following the intervention with no significant difference between diagnostic groups; drop-out rates were also similar across diagnostic groups. While these findings indicate that CBT may have clinical utility across OSFED diagnoses, full remission achieved by participants in the study was considered low. Riesco et al. [224] argued this may be attributable to low motivation to change, typical across OSFEDs. Therefore, treatment for OSFEDs may require additional features to address this issue.
Studies investigating psychotherapies other than CBT delivered to groups have shown mixed results for people with EDs [147]. Non-CBT interventions that were found to have benefit included IPT, emotionally-focused group therapy (EFGT) for individuals with BED, CD-Rom group therapy, and self-esteem and social skills therapy for adolescents with AN and BN. Deficiencies in social and interpersonal skills are highly associated with having an ED within clinical samples [219].
Group IPT for BED has emerged more recently than group CBT and is empirically associated with the management of negative emotions as dysfunctional responses to interpersonal stressors [295]. A recent systematic review included a study comparing the efficacy of group CBT, group IPT and waitlist on non-purging BN and found significant reductions in binge eating at post-treatment for CBT and IPT groups, which remained below baseline at 6-month and 1-year follow-up [295]. Similarly, group CBT and group IPT produced similar outcomes for patient recovery rates post-treatment (79% for CBT vs 73% for IPT) and at 1-year follow-up (59% for CBT vs 62% for IPT), with the frequency of binge eating remaining below baseline [223]. At 4-year follow-up, a significant and long-lasting benefit for CBT and IPT was shown, and a comparable remission rate to a subclinical level of BED [122]. For IPT patients, abstinence from binge eating remained stable and reduction of psychopathology was maintained or improved, whereas CBT patients had a significant tendency to relapse and psychopathology worsened during 1-year and 4-year follow-up compared to those treated with IPT.
Two studies found EFTG and EFTG in combination with dietary counselling to be highly effective in reducing ED symptomatology and weight in individuals with BED [61, 62]. Dissonance-based group therapy was compared to a supportive mindfulness group intervention for women with a diagnosed ED and no differences were found in ED symptoms between groups; however, the dissonance-based treatment group demonstrated a higher rate of remission than the supported mindfulness group [247].
In a child and adolescent population study, social skills group therapy and self-esteem group therapy were effective for individuals with AN-type disorders and BN-type disorders, with no significant differences between groups on measures of self-esteem [155]. Social skills group therapy was more effective in the BN-type group. Emerging evidence into the delivery of group-oriented FBT appears to be yielding promising results particularly as a support network for families with children in treatment, with MFT-AN leading to significant increases in BMI compared with individual FBT [79].
Technology-based interventions
The largest proportion of studies in the RR investigating technology-based interventions relate to the online delivery of CBT (iCBT). iCBT interventions have been found to result in significant reductions in ED symptoms compared with controls among individuals with BN, BED and OSFED [255, 278]. iCBT produced significant improvements in ED symptoms among participants with BN and S-BN [52], and the efficacy of iCBT for participants with BN and OSFED has also been supported [229, 250]. An RCT of iCBT with GSH for BED found that while it was inferior to individual face-to-face CBT in reduction of binge eating at 4-month follow-up, there were no differences between the online and face-to-face interventions at 18-month follow-up [250]. This suggests that iCBT with GSH is a viable alternative to face-to-face therapy, in addition to being easier to access and more affordable.
A systematic review of five studies on iCBT for BN, S-BN and OSFED concluded that iCBT has the capacity to reduce binge/purge behaviours but has not demonstrated superiority over bibliotherapies or waitlist conditions [297]. This finding reinforced an earlier systematic review of 21 computer-based ED interventions which was unable to determine whether interventions were superior to waitlist control groups [19]. It was found that computer-based interventions were effective, and more so for participants with binge/purge rather than restrictive ED symptoms. Thus, while the internet is a promising delivery modality for treatment of EDs, more research is required particularly involving a comparison with face-to-face delivery.
A systematic review evaluating the efficacy of internet-based interventions found that CBTgsh produced a significant improvement in primary and secondary outcomes related to eating behaviour and abstinence, across the six studies [76]. In addition, medium to high effect sizes were found within groups and between groups following utilisation of CBTgsh programs or a self-help book with supportive emails. The two studies utilising a specific writing task or email therapy not following a structured therapy program did not find any significant treatment effects.
A recent systematic review analysed the effectiveness of e-health interventions for the treatment of EDs [26]. The ED being investigated and the e-health intervention used varied across studies. Four studies reported higher effectiveness of e-health in comparison with control groups including waitlist, other psychotherapies, and TAU. A further systematic review found digital interventions to be more effective in reducing symptoms in prevention and established risk factors; however, few trials compared a digital intervention to a face-to-face intervention, limiting the conclusions that can be drawn [165].
High drop-out rates have been raised as a significant issue in internet-delivered treatments for EDs, with rates of dropout reported to be higher than that of face-to-face delivery, and an increased risk of drop-out being associated with more severe binge/purge and depressive symptoms [275]. These findings indicate that online interventions are better suited to individuals with less advanced EDs. For patients with BN who are motivated to change, iCBT may provide a more cost-effective intervention. Estimated cost per QALY was $59,540 (USD) compared with $73,618 for face-to-face CBT. This cost reduced further at 1-year follow-up to $38,715 per QALY for iCBT and $56,801 per QALY for face-to-face [285].
An RCT investigated the clinical efficacy of a combined mHealth intervention for EDs based on CBT and a mobile intervention through an application “TCApp” [28]. The study revealed that CBT can reduce ED symptoms regardless of its form of delivery. Another study examined the efficacy of a transdiagnostic cognitive-behavioural intervention for ED psychopathology delivered through a smartphone application [166]. Participants receiving the intervention reported greater reductions in EDE global psychopathology scores and ED symptoms, impairment and distress compared with the waitlist group.
A comparison of online CBT (CBT4BN) and face-to-face group CBT (CBTF2F) found online delivery to be inferior to face-to-face delivery at achieving binge/purge abstinence post-treatment [288]. However, this difference was no longer present at 12-month follow-up, indicating a ‘catch-up’ effect in the CBT4BN group. To address the issue of long waiting times experienced by patients with EDs between assessment and initial treatment session, Graham and Walton delivered a computer-based CBT intervention to outpatients with BN and BED prior to their first individual CBT program, finding it effective at reducing ED symptoms [101]; however, overall abstinence rates for both interventions were low at between 14 and 30% [101, 284]. Predictors for drop-out in this study included failure to engage, low perceived treatment credibility, previous experience with CBT, and randomisation to participant non-preferred format [284].
An RCT sought to investigate whether adding a brief online intervention, RecoveryMANTRA, which focuses on improving motivation to change and the development of a recover identity, would improve treatment outcomes for adults with AN [51]. No differences between the RecoveryMANTRA and TAU group were observed for BMI or ED symptoms. However, the RecoveryMANTRA group had significantly higher levels of confidence in own ability to change and therapeutic alliance with the therapist at the outpatient service, compared to TAU group without the online intervention [51].
In a systematic review, guided computer-based interventions (CBIs) for BN were found to lead to improvements in binge eating and purging behaviours, and global ED psychopathology, with those receiving guided CBIs improving more than controls and demonstrating similar efficacy to guided bibliography [83]. One study found CBIs to be potentially useful for relapse prevention of AN, but further empirical evidence is needed. Some studies suggest that CBIs may be an efficacious treatment option for adolescents with BN; however, more RCTs are required. Preliminary evidence suggested mobile interventions may be useful as an adjunct to therapy. Although most studies were able to demonstrate efficacy of CBIs, high rates of non-compliance, non-take-up and dropout across the included studies impede the validity of the results.
An RCT investigating the efficacy of a technology intervention delivered via text messaging after discharge from inpatient treatment for BN or OSFED found a significant difference between the intervention group (SMS-based maintenance intervention) and TAU in enhancing treatment outcomes [33]. An RCT conducted by Mitchell et al. [298] found CBT delivered face-to-face or via telemedicine to be equally efficacious in the treatment of in BN and OSFED. Taking this further, Ertelt et al. [80] sought to examine therapist and patient ratings of therapeutic alliance in both face-to-face and tele-delivery of CBT. Despite therapists indicating a stronger preference for face-to-face modalities and patients having no specific preference for treatment modality, ratings of perceived success and sustainability of treatment indicated strong therapeutic-relationships may be formed regardless of treatment delivery method [80].
Virtual reality
VR involves digital simulations of real-world situations where the participant is immersed in a scenario with visual and auditory stimuli [84]. It provides the opportunity to develop novel interventions to address body image and eating disturbance aspects of ED by simulating real world situations that would otherwise be difficult to replicate or control [55, 84,85,86, 173, 182, 203, 207].
A recent meta-analysis examining the efficacy of VR-enhanced CBT compared with CBT in the treatment of binge-purging type EDs found a significant reduction in binge frequency for those in the VR-enhanced CBT group compared with CBT group [173]. There were also significantly greater decreases in situation-induced body dissatisfaction in the VR-enhanced CBT group compared to CBT. However, there were no statistically significant differences in change in BMI or purge frequency, and no significant difference in improvement of overall body satisfaction [173]. Results highlight the possibility of VR in assisting patients in the development of coping strategies to triggers.
A randomised parallel study tested Cue Exposure Therapy (CET) in VR as an adjunct to CBT in individuals with BN and BED who required further treatment following their initial course [86]. CET in VR was superior to traditional CBT in terms of achieving binge/purge abstinence as well as reductions in core ED symptoms. Changes were maintained at follow-up, with abstinence rates remaining almost identical to post-treatment levels. These changes were well maintained in the same population group at 6-month follow-up, with abstinence rates remaining almost identical to post-treatment levels [85]. In a 1-year follow-up study of a VR-enhanced CBT intervention for treatment of body image disturbances in patients with ED, participants randomised to CBT + VR had a much faster response to CBT with improvements to ED psychopathologies maintained at follow-up [182].
A VR intervention targeting negative body memory in women with BED was found to be superior to CBT for weight loss in participants at 1-year follow-up [55]. A small (n = 38) RCT indicated that adjunctive therapy through use of a video game may improve treatment adherence in patients with BN [83]. VR was further investigated as a tool for reducing engagement in excessive exercising in patients with AN and BN, and was found to be effective at reducing urge to be physically active from levels measured at baseline [203].
Carer/support interventions
Studies have shown that carers of patients with EDs can experience substantial distress, anxiety and depressive symptoms [63, 226, 241]; these are most prevalent among carers of individuals with AN [234, 241]. These symptoms have been shown to lead to maladaptive behaviours and contribute to disorder maintenance in the patient [63, 111], with higher perceived burden impacting successful implementation of therapy [186, 281].
Considering the complex and often enduring nature of EDs, there is an emerging evidence base regarding the importance of support for carers and a potential role for mentoring. Greater available support for individuals with EDs is associated with more positive outcomes for both carer and patient [91], and is particularly important considering the high amounts of perceived stigmatisation experienced by this group [63, 105, 183].
Interventions for carers such as online CBT, psycho-education and self-help programs, peer-mentoring and group workshops, have been found to be effective at reducing carer anxiety and depressive symptoms, and have been associated with improved treatment outcomes for patients [111, 121, 125, 128, 205, 206, 216]. The Collaborative Care Skills workshop [234], developed in the UK, and delivered to Australian carers in two studies, reported a significant reduction in maladaptive coping and expressed emotions [206]. This was maintained at 8-week and 6-month follow-up, along with an increased confidence that their loved ones could change, which was considered a contributor to measured decreases in psychological distress.
Discussion
The primary aim of the RR was to identify, summarise and consolidate the evidence-base for psychotherapies and their effectiveness in the treatment of EDs. The secondary aim was to identify gaps in the research and highlight emerging psychotherapeutic treatments. In total, 263 studies met broad eligibility criteria. Of these, 30% focused on CBT, 12% on FBT, 5% on exposure-based therapies, 3% on IPT, DBT, ACT, and ICAT, and 2% on other psychotherapies. CBT was considerably the most widely researched, and behavioural therapies in general comprised at least two-thirds of the examined literature.
Much of the research examining CBT and its variations has focused on the treatment of BN, BED, and AN, and it is currently suggested to be the leading treatment for individuals with BN and BED. There is general consensus in the field regarding the transdiagnostic therapeutic effectiveness of CBT across different ED diagnoses given its ability to target illness-maintaining features and reduce binge/purge symptomatology [69, 167], although the evidence is greater for use in BN and BED as well as their sub-clinical variants. Moreover, emerging evidence suggests that CBT may be effective when administered using group therapy [24, 66, 134], guided self-help [46, 89, 273, 279] and technology-based delivery modalities [52, 76, 229, 250, 255, 280, 297]. Despite the high number of included studies, few investigated the efficacy of CBT for OSFED and ARFID.
Currently, FBT should be considered in the first instance when treating children and adolescents with AN (including atypical presentations, OSFED/UFED) [100]. It is the most consistently effective treatment for child and adolescent AN and has been found to be highly cost-effective in an Australian context [20, 157]. However, non-response to treatment and high drop-out rates have resulted in several adaptive variants to the intervention, including multi-family, parent-focused and systematic family therapies, with varying degrees of effectiveness. Whilst much less evidence exists on the use of FBT to treat adolescent BN than AN, there is a developing evidence-base for treatment of BN and BED with FBT [159]. Factors associated with higher remission rates include sustained involvement by fathers in therapy and early weight gain in response to treatment [130]. Preliminary evidence suggests that FBT may be a viable option to treat ARFID in children and adolescents [259].
IPT has been considered an effective and viable alternative treatment for BN and BED, however, opinions in the field regarding its inferiority to CBT in being able to produce a rapid treatment response may have contributed to a lack of research on the intervention [81]. IPT has demonstrated similar treatment outcomes to both individual and group CBT. Most improvements from IPT have been observed at follow-up, suggesting its efficacy in long-term reductions and remission of symptoms [195, 230, 295, 299]. IPT for the prevention of excess weight gain may be efficacious for reducing loss of control eating and weight gain in overweight youth [223].
There is preliminary evidence to suggest therapies involving exposure to stimuli eliciting ED behaviours and the subsequent restructuring of these responses could be helpful in increasing long-term effectiveness when delivered as a supplement to CBT [104, 245, 253]. Pharmacotherapy may enhance the effects of exposure therapy in individuals with AN [161].
Novel psychotherapeutic approaches as an alternative to CBT are being trialled in RCTs [208, 287]. From the small number of studies identified, neither ICAT or ACT have proven to be more effective than an active comparator (CBT) or TAU for patients with AN or BN. However, emerging evidence suggests that ICAT may be equally as effective as CBT-E and guided self-help at reducing symptoms of bulimia nervosa [208, 287].
Overall, the available evidence for psychotherapies delivered in a group format suggests that the type of therapy rather than its delivery in individual or group settings contributes more to the effectiveness of the intervention. Although there is some evidence to suggest that MFT may be more effective than standard FBT in producing changes on outcomes due to its networking and support aspects, evidence for the advantages of group over individual for other types of psychotherapies is inconclusive. On the other hand, the available evidence does not appear to show dilution of therapeutic effect when delivering psychotherapy interventions to groups, and this alternative modality may have significantly reduced resource implications.
Research suggests GSH as the first-line treatment for non-underweight EDs characterised by recurrent binge eating, namely BED and BN [208]. Evidence for its effectiveness on individuals with BED is particularly strong [53, 243, 265, 286]. Self-help interventions are not recommended in the treatment of AN due to the specialist care required for this disorder [286]. It has been suggested that the comparative advantages of self-help over therapist-led interventions include increased access, cost-effectiveness and capacity to be delivered by professionals without specialist knowledge in ED treatment [175, 286].
Studies have found technology-based CBT interventions to result in significant reductions in ED symptoms compared with controls among individuals with BN, BED and OSFED [173, 255]. At 4-month follow-up iCBT with GSH was found to be inferior to individual face-to-face CBT in reducing binge eating in patients with BED [33, 74]. However, no differences between online and face-to-face interventions were reported at 18-month follow-up, suggesting that iCBT with GSH—which may be easier to access and more affordable—may be a viable alternative over longer-term face-to-face therapy [33, 74]. High drop-out rates have been raised as a significant issue in internet-delivered treatments for EDs [155, 275]. These findings indicate that online interventions may be better suited to individuals with less advanced trajectories of EDs.
This review has highlighted that CBT delivered face-to-face or via telemedicine to BN or OSFED patients has been found to be equally efficacious in terms of treatment outcomes. Therapists tend to favour face-to-face CBT over tele-delivery, however patients do not show a strong preference for either delivery modality with little to no impact on the therapeutic alliance [80].
Overall, the evidence supports the augmentation of CBT with VR to increase effectiveness and time to response in individuals with ED [173]. However, the practicality of providing these novel interventions must be considered, as it is unlikely that many therapists would currently have or could gain the relevant expertise to deliver VR-based therapy.
Evidence is limited in terms of ED carer support, nonetheless, there is a growing need to support individuals caring for people with an ED [93, 111]. Further research and investment in mentoring programs for carers of someone with an ED may be warranted as part of a ‘stepped care’ approach, delivered in a similar way to mental health services in Australia, however, evidence on effect is still in its infancy.
There is very limited evidence addressing treatment for ARFID. Available literature consists of case reports and case series. Some evidence exists for ‘feeding disorder of infancy and early childhood,’ a DSM-IV disorder now encompassed by ARFID. However, these lack applicability to adolescents and adults.
Strengths and limitations
Inherent limitations associated with the RR methodology aside, the current review faced a number of unique challenges. Firstly, the broad eligibility criteria, particularly for the large topic of psychotherapies, meant that a significant number of identified studies focused on small variations of the same core psychotherapy; thus, lacking diversity in ED treatment types. For example, several studies investigated versions of CBT, such as CBT-L, and CBT-S, where the core tenets of the psychotherapeutic approach were much the same as the therapy they were based on. Secondly, there appeared to be a large proportion of literature that was not captured or was considered ‘ineligible’ for inclusion, which may have led to a skewed representation of the evidence-base related to specific therapies. Finally, much of the literature examined for the RR centred on clinical samples in Westernised, Educated, Industrialised, Rich, and Democratic (WEIRD) countries. This may suggest a bias in the research and may limit the generalisability of the findings and conclusions of the RR to countries and populations not captured in the studies.
Despite these limitations, this review enabled a broad investigation into the current evidence-base whilst highlighting areas that are lacking research. Further, it offers a springboard for clinical and academic discussion to move the field forward and improve clinical outcomes and care.
Future studies
Considerably more research is needed to critically and meaningfully consider other third-wave therapies that may be able to demonstrate greater therapeutic outcomes over traditional psychotherapies, such as CBT [162]. CBT has emerged as the most empirically researched psychotherapy, yet it has not been able to demonstrate greater propensity to remit EDs. Specifically, non-response to treatment in some groups, such as AN, and lack of improvement in remission rates have necessitated exploration of alternative approaches. Future research into alternatives which consider complex presentations and treatments that address both the high dropout rates, such as those seen in FBT for children and adolescents, would greatly benefit the field of EDs. Additionally, variations in outcome measurements may impact comparability of studies and the ability for appropriate evaluation of treatment effectiveness across psychotherapies. Lastly, investigation into treatments that focus on emerging disorders, notably ARFID and OSFED, would aid in supporting patients, families, and clinicians by addressing the paucity in evidence-based interventions available for these types of EDs.
Conclusions
The current evidence suggests that a number of psychotherapies are effective in improving ED symptomatology. Specifically, interventions based on cognitive-behavioural approaches, such as CBT, FBT, and IPT, have the most demonstratable evidence supporting their efficacy as treatments for EDs. The RR indicated that there is emerging evidence for novel approaches including ACT, DBT, cognitive remediation therapy (CRT), and exposure and response (ERP) therapies demonstrating varying efficacy. It also highlighted emerging evidence supporting technology-based delivery of psychotherapies. Finally, this review has served to highlight the notion that every treatment approach is subject to its strengths and shortcomings and given the complexity of EDs and the influence of individual factors, there is very unlikely to ever be a ‘one-size fits all’ treatment. Nonetheless, this review starkly highlights that more needs to be done in order to improve ED outcomes, and related impacts and burden.
Availability of data and materials
Not applicable—all citations provided.
Notes
A sham procedure without active neuro modulation.
Abbreviations
- AAT:
-
Appetite Awareness Therapy
- ABM:
-
Approach bias modification
- ACT:
-
Acceptance and commitment therapy
- AFT:
-
Adolescent-focused individual therapy
- AN:
-
Anorexia nervosa
- AN-BP:
-
Anorexia nervosa binge/purge subtype
- AN-BP:
-
Anorexia nervosa-borderline personality
- AN-EXRP:
-
Exposure response therapy for anorexia nervosa
- AN-R:
-
Anorexia nervosa restrictive subtype
- ARFID:
-
Avoidant restrictive food intake disorder
- BED:
-
Binge eating disorder
- BFST:
-
Behavioural family system therapy
- BMI:
-
Body mass index
- BN:
-
Bulimia nervosa
- BPD:
-
Borderline personality disorder
- BT-BN:
-
Bulimia nervosa-focused family therapy
- BWLT:
-
Behavioural weight loss therapy
- CALD:
-
Culturally and Linguistically Diverse
- CBI:
-
Computer based intervention
- CBT:
-
Cognitive behavioural therapy
- CBT-A:
-
Appetite-focused cognitive behavioural therapy
- CBT-A:
-
Cognitive behavioural therapy for adolescents
- CBT-BN:
-
Cognitive behavioural therapy for bulimia nervosa
- CBT-E:
-
Enhanced cognitive behavioural therapy
- CBTgsh:
-
Cognitive behavioural therapy guided self-help
- CBT-L:
-
Cognitive behavioural therapy-long
- CBT-S:
-
Cognitive behavioural therapy-short
- CET:
-
Cue exposure therapy
- CFT:
-
Conjoint family therapy
- CRT:
-
Cognitive remediation therapy
- CRT:
-
Cognitive remediation therapy
- DBT:
-
Dialectical behavioural therapy
- DBT-BED:
-
Dialectical behavioural therapy for binge eating disorder
- DBT-AF:
-
Appetite focused dialectical behavioural therapy
- ED:
-
Eating disorder
- EDE:
-
Eating disorder examination
- EDE-Q:
-
Eating disorder examination questionnaire
- EDNOS:
-
Eating disorder not otherwise specified
- EFTG:
-
Emotionally-focused group therapy
- eGSH:
-
Email guided self-help
- ERP:
-
Exposure response therapy
- FBT:
-
Family based therapy
- FBT-AN:
-
Family based therapy for anorexia nervosa
- FBT-BN:
-
Family based therapy for bulimia nervosa
- FPT:
-
Focal psychodynamic therapy
- FT-AN:
-
Family based therapy for anorexia nervosa
- GSH:
-
Guided self-help
- HAPIFED:
-
Health approach to weight management and food in eating disorders
- HRQoL:
-
Health-related quality of life
- ICAT:
-
Integrative cognitive affective therapy
- ICAT-BED:
-
Integrative cognitive affective therapy for binge eating disorder
- ICAT-BN:
-
Integrative cognitive affective therapy for bulimia nervosa
- iCBT:
-
Online delivery of cognitive behavioural therapy
- IPT:
-
Interpersonal therapy
- LOC:
-
Loss of control
- MANTRA:
-
Maudsley anorexia treatment for adults
- MET:
-
Motivational enhancement therapy
- MFT-AN:
-
Multi-family therapy for anorexia nervosa
- MI:
-
Motivational interviewing
- MOPED:
-
Motivation and psycho-educational guided self-help intervention for people with eating disorders
- NED:
-
Night Eating Syndrome
- NHS:
-
National Health Service
- NICE:
-
National Institute for Clinical Excellence
- OSFED:
-
Other Specified Feeding and Eating Disorder
- PDT:
-
Psychodynamic therapy
- PFT:
-
Parent focused therapy
- PPT:
-
Positive psychology
- RCT:
-
Randomised clinical trial
- RR:
-
Rapid review
- S-BED:
-
Subclinical binge eating disorder
- S-BN:
-
Subclinical Bulimia Nervosa
- SPACE-ARFID:
-
Supportive parenting for anxious childhood emotions adapted for avoidant/restrictive food intake disorder
- SyFT:
-
Systemic family therapy
- TAU:
-
Treatment as usual
- UFED:
-
Unspecified feeding or eating disorder
- VR:
-
Virtual reality
- WEIRD:
-
Westernised, educated, industrialised, rich, democratic (countries)
References
van Hoeken D, Hoek HW. Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Curr Opin Psychiatry. 2020;33(6):521–7.
Fassino S, Abbate-Daga G. Resistance to treatment in eating disorders: a critical challenge. BMC Psychiatry. 2013;13(1):282.
Pennesi J-L, Wade TD. A systematic review of the existing models of disordered eating: do they inform the development of effective interventions? Clin Psychol Rev. 2016;43:175–92.
Kass AE, Kolko RP, Wilfley DE. Psychological treatments for eating disorders. Curr Opin Psychiatry. 2013;26(6):549–55.
Jansingh A, Danner UN, Hoek HW, van Elburg AA. Developments in the psychological treatment of anorexia nervosa and their implications for daily practice. Curr Opin Psychiatry. 2020;33(6):534–41.
National Institute for Health Care Excellence. Eating disorders: recognition and treatment. UK: The National Institute for Health and Care Excellence (NICE); 2017. Accessed 4 Aug 2023.
Hilbert A, Hoek HW, Schmidt R. Evidence-based clinical guidelines for eating disorders: international comparison. Curr Opin Psychiatry. 2017;30(6):423.
Treasure J, Cardi V, Leppanen J, Turton R. New treatment approaches for severe and enduring eating disorders. Physiol Behav. 2015;152:456–65.
Watson HJ, Fursland A, Byrne S. Treatment engagement in eating disorders: who exits before treatment? Int J Eat Disord. 2013;46(6):553–9.
Baudinet J, Eisler I, Dawson L, Simic M, Schmidt U. Multi-family therapy for eating disorders: a systematic scoping review of the quantitative and qualitative findings. Int J Eat Disord. 2021;54(12):2095–120.
Cyrus J. Research guides: rapid review protocol: steps: rapid review USA. Virginia Commonwealth University; 2021 [updated 2021; cited 2023]. https://guides.library.vcu.edu/rapidreview. Accessed 4 Aug 2023.
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–20.
Canada's Drug and Health Technology Agency (CDHTA). About the rapid response service Canada: CDHTA; 2021 [updated 2021]. https://www.cadth.ca/about-rapid-response-service.
Hamel C, Michaud A, Thuku M, Skidmore B, Stevens A, Nussbaumer-Streit B, et al. Defining rapid reviews: a systematic scoping review and thematic analysis of definitions and defining characteristics of rapid reviews. J Clin Epidemiol. 2021;129:74–85.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ Br Med J. 2009;339(7716):332–6.
Rethlefsen ML, Kirtley S, Waffenschmidt S, Ayala AP, Moher D, Page MJ, et al. PRISMA-S: an extension to the PRISMA statement for reporting literature searches in systematic reviews. J Med Libr Assoc. 2021;109(2):174–201.
Aouad P, Bryant E, Maloney D, Marks P, Le A, Russell H, et al. Informing the development of Australia’s National Eating Disorders Research and Translation Strategy: a rapid review methodology. J Eat Disord. 2022;10(1):31.
Fairburn CG, Cooper Z, Doll HA, O’Connor ME, Bohn K, Hawker DM, et al. Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: a two-site trial with 60-week follow-up. Am J Psychiatry. 2009;166(3):311–9.
Aardoom JJ, Dingemans AE, Spinhoven P, Van Furth EF. Treating eating disorders over the internet: a systematic review and future research directions. Int J Eat Disord. 2013;46(6):539–52.
Accurso EC, Ciao AC, Fitzsimmons-Craft EE, Lock JD, Le Grange D. Is weight gain really a catalyst for broader recovery?: The impact of weight gain on psychological symptoms in the treatment of adolescent anorexia nervosa. Behav Res Ther. 2014;56:1–6.
Accurso EC, Fitzsimmons-Craft EE, Ciao A, Cao L, Crosby RD, Smith TL, et al. Therapeutic alliance in a randomized clinical trial for bulimia nervosa. J Consult Clin Psychol. 2015;83(3):637–42.
Agras WS, Lock J, Brandt H, Bryson SW, Dodge E, Halmi KA, et al. Comparison of 2 family therapies for adolescent anorexia nervosa: a randomized parallel trial. JAMA Psychiat. 2014;71(11):1279–86.
Agras WS, Fitzsimmons-Craft EE, Wilfley DE. Evolution of cognitive-behavioral therapy for eating disorders. Behav Res Ther. 2017;88:26–36.
Agüera Z, Riesco N, Jiménez-Murcia S, Islam MA, Granero R, Vicente E, et al. Cognitive behaviour therapy response and dropout rate across purging and nonpurging bulimia nervosa and binge eating disorder: DSM-5 implications. BMC Psychiatry. 2013;13(1):285.
Agüera Z, Sánchez I, Granero R, Riesco N, Steward T, Martín-Romera V, et al. Short-term treatment outcomes and dropout risk in men and women with eating disorders. Eur Eat Disord Rev. 2017;25(4):293–301.
Ahmadiankalati M, Steins-Loeber S, Paslakis G. Review of randomized controlled trials using e-health interventions for patients with eating disorders. Front Psychiatry. 2020;11:568.
Alfonsson S, Parling T, Ghaderi A. Group behavioral activation for patients with severe obesity and binge eating disorder: a randomized controlled trial. Behav Modif. 2015;39(2):270–94.
Anastasiadou D, Folkvord F, Brugnera A, Cañas Vinader L, SerranoTroncoso E, Carretero Jardí C, et al. An mHealth intervention for the treatment of patients with an eating disorder: a multicenter randomized controlled trial. Int J Eat Disord. 2020;53(7):1120–31.
Anderson LM, Smith KM, Schaefer LM, Crosby RD, Cao L, Engel SG, et al. Predictors and moderators of treatment outcome in a randomized clinical trial for binge-eating disorder. J Consult Clin Psychol. 2020;88(7):631–42.
Ariel AH, Perri MG. Effect of dose of behavioral treatment for obesity on binge eating severity. Eat Behav. 2016;22:55–61.
Austin A, Flynn M, Shearer J, Long M, Allen K, Mountford VA, et al. The first episode rapid early intervention for eating disorders—upscaled study: clinical outcomes. Early Interv Psychiatry. 2022;16(1):97–105.
Bankoff SM, Karpel MG, Forbes HE, Pantalone DW. A systematic review of dialectical behavior therapy for the treatment of eating disorders. Eat Disord. 2012;20(3):196–215.
Bauer S, Okon E, Meermann R, Kordy H. Technology-enhanced maintenance of treatment gains in eating disorders: efficacy of an intervention delivered via text messaging. J Consult Clin Psychol. 2012;80:700–6.
Beintner I, Jacobi C, Schmidt UH. Participation and outcome in manualized self-help for bulimia nervosa and binge eating disorder—a systematic review and metaregression analysis. Clin Psychol Rev. 2014;34(2):158–76.
Bentz M, Pedersen SH, Moslet U. An evaluation of family-based treatment for restrictive-type eating disorders, delivered as standard care in a public mental health service. J Eat Disord. 2021;9(1):141.
Berking M, Eichler E, Naumann E, Svaldi J. The efficacy of a transdiagnostic emotion regulation skills training in the treatment of binge-eating disorder-Results from a randomized controlled trial. Br J Clin Psychol. 2022;61(4):998–1018.
Blanchet C, Mathieu M-È, St-Laurent A, Fecteau S, St-Amour N, Drapeau V. A systematic review of physical activity interventions in individuals with binge eating disorders. Curr Obes Rep. 2018;7(1):76–88.
Boerhout C, Swart M, Van Busschbach JT, Hoek HW. Effect of aggression regulation on eating disorder pathology: RCT of a brief body and movement oriented intervention. Eur Eat Disord Rev. 2016;24(2):114–21.
Boerhout C, Swart M, Voskamp M, Troquete NAC, van Busschbach JT, Hoek HW. Aggression regulation in day treatment of eating disorders: two-centre RCT of a brief body and movement-oriented intervention. Eur Eat Disord Rev. 2017;25(1):52–9.
Brauhardt A, de Zwaan M, Hilbert A. The therapeutic process in psychological treatments for eating disorders: a systematic review. Int J Eat Disord. 2014;47(6):565–84.
Brewin N, Wales J, Cashmore R, Plateau CR, Dean B, Cousins T, et al. Evaluation of a motivation and psycho-educational guided self-help intervention for people with eating disorders (MOPED). Eur Eat Disord Rev. 2016;24(3):241–6.
Brockmeyer T, Friederich H-C, Küppers C, Chowdhury S, Harms L, Simmonds J, et al. Approach bias modification training in bulimia nervosa and binge-eating disorder: a pilot randomized controlled trial. Int J Eat Disord. 2019;52(5):520–9.
Brockmeyer T, Friederich H-C, Schmidt U. Advances in the treatment of anorexia nervosa: a review of established and emerging interventions. Psychol Med. 2018;48(8):1228–56.
Brockmeyer T, Schmidt H, Leiteritz-Rausch A, Zimmermann J, Wünsch-Leiteritz W, Leiteritz A, et al. Cognitive remediation therapy in anorexia nervosa-a randomized clinical trial. J Consult Clin Psychol. 2021;89(10):805–15.
Brown A, Mountford V, Waller G. Therapeutic alliance and weight gain during cognitive behavioural therapy for anorexia nervosa. Behav Res Ther. 2013;51(4):216–20.
Brownley KA, Berkman ND, Peat CM, Lohr KN, Cullen KE, Bann CM, et al. Binge-eating disorder in adults. Ann Intern Med. 2016;165(6):409–20.
Butler RM, Heimberg RG. Exposure therapy for eating disorders: a systematic review. Clin Psychol Rev. 2020;78: 101851.
Buerger A, Vloet TD, Haber L, Geissler JM. Third-wave interventions for eating disorders in adolescence—systematic review with meta-analysis. Borderline Personal Disord Emot Dysregulation. 2021;8(1):20.
Byrne SM, Fursland A, Allen KL, Watson H. The effectiveness of enhanced cognitive behavioural therapy for eating disorders: an open trial. Behav Res Ther. 2011;49(4):219–26.
Calugi S, Dametti L, Chimini M, Dalle Grave A, Dalle GR. Change in eating-disorder psychopathology network structure in patients with anorexia nervosa treated with intensive cognitive behavior therapy. Int J Eat Disord. 2021;54(10):1800–9.
Cardi V, Albano G, Ambwani S, Cao L, Crosby RD, Macdonald P, et al. A randomised clinical trial to evaluate the acceptability and efficacy of an early phase, online, guided augmentation of outpatient care for adults with anorexia nervosa. Psychol Med. 2020;50(15):2610–21.
Carrard I, Fernandez-Aranda F, Lam T, Nevonen L, Liwowsky I, Volkart AC, et al. Evaluation of a guided internet self-treatment programme for bulimia nervosa in several European countries. Eur Eat Disord Rev. 2011;19(2):138–49.
Carrard I, Crépin C, Rouget P, Lam T, Golay A, Van der Linden M. Randomised controlled trial of a guided self-help treatment on the Internet for binge eating disorder. Behav Res Ther. 2011;49(8):482–91.
Catalan-Matamoros D, Helvik-Skjaerven L, Labajos-Manzanares MT, Martínez-de-Salazar-Arboleas A, Sánchez-Guerrero E. A pilot study on the effect of Basic body awareness therapy in patients with eating disorders: a randomized controlled trial. Clin Rehabil. 2011;25(7):617–26.
Cesa GL, Manzoni GM, Bacchetta M, Castelnuovo G, Conti S, Gaggioli A, et al. Virtual reality for enhancing the cognitive behavioral treatment of obesity with binge eating disorder: randomized controlled study with one-year follow-up. J Med Internet Res. 2013;15(6): e113.
Chami R, Cardi V, Lawrence N, MacDonald P, Rowlands K, Hodsoll J, et al. Targeting binge eating in bulimia nervosa and binge eating disorder using inhibitory control training and implementation intentions: a feasibility trial. Psychol Med. 2022;52(5):874–83.
Chang PG, Delgadillo J, Waller G. Early response to psychological treatment for eating disorders: a systematic review and meta-analysis. Clin Psychol Rev. 2021;86: 102032.
Chen EY, Cacioppo J, Fettich K, Gallop R, McCloskey MS, Olino T, et al. An adaptive randomized trial of dialectical behavior therapy and cognitive behavior therapy for binge-eating. Psychol Med. 2017;47(4):703–17.
Ciao AC, Accurso EC, Fitzsimmons-Craft EE, Le Grange D. Predictors and moderators of psychological changes during the treatment of adolescent bulimia nervosa. Behav Res Ther. 2015;69:48–53.
Clyne C, Latner JD, Gleaves DH, Blampied NM. Treatment of emotional dysregulation in full syndrome and subthreshold binge eating disorder. Eat Disord. 2010;18(5):408–24.
Compare A, Tasca GA. The rate and shape of change in binge eating episodes and weight: an effectiveness trial of emotionally focused group therapy for binge-eating disorder. Clin Psychol Psychother. 2016;23(1):24–34.
Compare A, Calugi S, Marchesini G, Shonin E, Grossi E, Molinari E, et al. Emotionally focused group therapy and dietary counseling in binge eating disorder. Effect on eating disorder psychopathology and quality of life. Appetite. 2013;71:361–8.
Coomber K, King RM. Coping strategies and social support as predictors and mediators of eating disorder carer burden and psychological distress. Soc Psychiatry Psychiatr Epidemiol. 2012;47:789–96.
Coomber K, King RM. A longitudinal examination of burden and psychological distress in carers of people with an eating disorder. Soc Psychiatry Psychiatr Epidemiol. 2013;48(1):163–71.
Costa MB, Melnik T. Effectiveness of psychosocial interventions in eating disorders: an overview of Cochrane systematic reviews. Einstein (São Paulo). 2016;14:235–77.
Courbasson CM, Nishikawa Y, Shapira LB. Mindfulness-action based cognitive behavioral therapy for concurrent binge eating disorder and substance use disorders. Eat Disord. 2010;19(1):17–33.
Couturier J, Kimber M, Szatmari P. Efficacy of family-based treatment for adolescents with eating disorders: a systematic review and meta-analysis. Int J Eat Disord. 2013;46(1):3–11.
Craig M, Waine J, Wilson S, Waller G. Optimizing treatment outcomes in adolescents with eating disorders: the potential role of cognitive behavioral therapy. Int J Eat Disord. 2019;52(5):538–42.
Dakanalis A, Carrà G, Calogero R, Zanetti MA, Gaudio S, Caccialanza R, et al. Testing the cognitive-behavioural maintenance models across DSM-5 bulimic-type eating disorder diagnostic groups: a multi-centre study. Eur Arch Psychiatry Clin Neurosci. 2015;265(8):663–76.
Dalle Grave R, Calugi S, Sartirana M, Fairburn CG. Transdiagnostic cognitive behaviour therapy for adolescents with an eating disorder who are not underweight. Behav Res Ther. 2015;73:79–82.
Daniel SIF, Poulsen S, Lunn S. Client attachment in a randomized clinical trial of psychoanalytic and cognitive-behavioral psychotherapy for bulimia nervosa: outcome moderation and change. Psychotherapy. 2016;53:174–84.
Daniel SIF, Lunn S, Poulsen S. Client attachment and therapist feelings in the treatment of bulimia nervosa. Psychotherapy. 2015;52(2):247.
de Jong M, Schoorl M, Hoek HW. Enhanced cognitive behavioural therapy for patients with eating disorders: a systematic review. Curr Opin Psychiatry. 2018;31(6):436–44.
de Zwaan M, Herpertz S, Zipfel S, Svaldi J, Friederich H-C, Schmidt F, et al. Effect of internet-based guided self-help vs individual face-to-face treatment on full or subsyndromal binge eating disorder in overweight or obese patients: the INTERBED randomized clinical trial. JAMA Psychiat. 2017;74(10):987–95.
Díaz-Ferrer S, Rodríguez-Ruiz S, Ortega-Roldán B, Moreno-Domínguez S, Fernández-Santaella MC. Testing the efficacy of pure versus guided mirror exposure in women with bulimia nervosa: a combination of neuroendocrine and psychological indices. J Behav Ther Exp Psychiatry. 2015;48:1–8.
Dölemeyer R, Tietjen A, Kersting A, Wagner B. Internet-based interventions for eating disorders in adults: a systematic review. BMC Psychiatry. 2013;13(1):1–16.
Dray J, Wade TD. Is the transtheoretical model and motivational interviewing approach applicable to the treatment of eating disorders? A review. Clin Psychol Rev. 2012;32(6):558–65.
Egger N, Wild B, Zipfel S, Junne F, Konnopka A, Schmidt U, et al. Cost-effectiveness of focal psychodynamic therapy and enhanced cognitive-behavioural therapy in out-patients with anorexia nervosa. Psychol Med. 2016;46(16):3291–301.
Eisler I, Simic M, Hodsoll J, Asen E, Berelowitz M, Connan F, et al. A pragmatic randomised multi-centre trial of multifamily and single family therapy for adolescent anorexia nervosa. BMC Psychiatry. 2016;16(1):1–14.
Ertelt TW, Crosby RD, Marino JM, Mitchell JE, Lancaster K, Crow SJ. Therapeutic factors affecting the cognitive behavioral treatment of bulimia nervosa via telemedicine versus face-to-face delivery. Int J Eat Disord. 2011;44(8):687–91.
Fairburn CG, Cooper Z, Doll HA, O’Connor ME, Palmer RL, Dalle GR. Enhanced cognitive behaviour therapy for adults with anorexia nervosa: a UK–Italy study. Behav Res Ther. 2013;51(1):R2–8.
Fairburn CG, Bailey-Straebler S, Basden S, Doll HA, Jones R, Murphy R, et al. A transdiagnostic comparison of enhanced cognitive behaviour therapy (CBT-E) and interpersonal psychotherapy in the treatment of eating disorders. Behav Res Ther. 2015;70:64–71.
Fernandez-Aranda F, Jimenez-Murcia S, Santamaría JJ, Giner-Bartolomé C, Mestre-Bach G, Granero R, et al. The use of videogames as complementary therapeutic tool for cognitive behavioral therapy in bulimia nervosa patients. Cyberpsychol Behav Soc Netw. 2015;18(12):744–51.
Ferrer-García M, Gutiérrez-Maldonado J. The use of virtual reality in the study, assessment, and treatment of body image in eating disorders and nonclinical samples: a review of the literature. Body Image. 2012;9(1):1–11.
Ferrer-Garcia M, Pla-Sanjuanelo J, Dakanalis A, Vilalta-Abella F, Riva G, Fernandez-Aranda F, et al. A randomized trial of virtual reality-based cue exposure second-level therapy and cognitive behavior second-level therapy for bulimia nervosa and binge-eating disorder: outcome at six-month followup. Cyberpsychol Behav Soc Netw. 2019;22(1):60–8.
Ferrer-García M, Gutiérrez-Maldonado J, Pla-Sanjuanelo J, Vilalta-Abella F, Riva G, Clerici M, et al. A randomised controlled comparison of second-level treatment approaches for treatment-resistant adults with bulimia nervosa and binge eating disorder: assessing the benefits of virtual reality cue exposure therapy. Eur Eat Disord Rev. 2017;25(6):479–90.
Fioravanti G, Castellini G, Lo Sauro C, Ianni S, Montanelli L, Rotella F, et al. Course and moderators of emotional eating in anorectic and bulimic patients: a follow-up study. Eat Behav. 2014;15(2):192–6.
Fisher CA, Skocic S, Rutherford KA, Hetrick SE. Family therapy approaches for anorexia nervosa. Cochrane Database Syst Rev. 2019(5).
Fitzsimmons-Craft EE, Taylor CB, Graham AK, Sadeh-Sharvit S, Balantekin KN, Eichen DM, et al. Effectiveness of a digital cognitive behavior therapy-guided self-help intervention for eating disorders in college women: a cluster randomized clinical trial. JAMA Netw Open. 2020;3(8): e2015633.
Fitzsimmons-Craft EE, Laboe AA, McGinnis C, Firebaugh ML, Shah J, Wallendorf M, et al. A pilot randomized controlled trial of a cognitive-behavioral therapy-guided self-help mobile app for the post-acute treatment of anorexia nervosa: a registered report. Int J Eat Disord. 2023;56(3):654–61.
Fogarty S, Ramjan L, Hay P. A systematic review and meta-synthesis of the effects and experience of mentoring in eating disorders and disordered eating. Eat Behav. 2016;21:66–75.
Folke S, Daniel SIF, Poulsen S, Lunn S. Client attachment security predicts alliance in a randomized controlled trial of two psychotherapies for bulimia nervosa. Psychother Res. 2016;26(4):459–71.
Fox JRE, Dean M, Whittlesea A. The experience of caring for or living with an individual with an eating disorder: a meta-synthesis of qualitative studies. Clin Psychol Psychother. 2017;24(1):103–25.
Gan JKE, Wu VX, Chow G, Chan JKY, Klainin-Yobas P. Effectiveness of non-pharmacological interventions on individuals with anorexia nervosa: a systematic review and meta-analysis. Patient Educ Couns. 2022;105(1):44–55.
Gale C, Gilbert P, Read N, Goss K. An evaluation of the impact of introducing compassion focused therapy to a standard treatment programme for people with eating disorders. Clin Psychol Psychother. 2014;21(1):1–12.
Gallagher ME, Tasca GA, Ritchie K, Balfour L, Maxwell H, Bissada H. Interpersonal learning is associated with improved self-esteem in group psychotherapy for women with binge eating disorder. Psychotherapy. 2014;51:66–77.
Garrett AS, Lock J, Datta N, Beenhaker J, Kesler SR, Reiss AL. Predicting clinical outcome using brain activation associated with set-shifting and central coherence skills in Anorexia Nervosa. J Psychiatr Res. 2014;57:26–33.
Godart N, Dorard G, Duclos J, Curt F, Kaganski I, Minier L, et al. Long-term follow-up of a randomized controlled trial comparing systemic family therapy (FT-S) added to treatment as usual (TAU) with TAU alone in adolescents with anorexia nervosa. J Child Psychol Psychiatry. 2022;63(11):1368–80.
Castillo MDG, Pina JAL, Ortuno AIT, Duran AL, Trives JJR. Parental eating disorders symptoms in different clinical diagnoses. Psicothema. 2018;30(4):382–8.
Gorrell S, Loeb KL, Grange DL. Family-based treatment of eating disorders: a narrative review. Psychiatr Clin. 2019;42(2):193–204.
Graham L, Walton M. Investigating the use of CD-Rom CBT for bulimia nervosa and binge eating disorder in an nhs adult outpatient eating disorders service. Behav Cogn Psychother. 2011;39(4):443–56.
Gregertsen EC, Mandy W, Kanakam N, Armstrong S, Serpell L. Pre-treatment patient characteristics as predictors of drop-out and treatment outcome in individual and family therapy for adolescents and adults with anorexia nervosa: a systematic review and meta-analysis. Psychiatry Res. 2019;271:484–501.
Grenon R, Schwartze D, Hammond N, Ivanova I, Mcquaid N, Proulx G, et al. Group psychotherapy for eating disorders: a meta-analysis. Int J Eat Disord. 2017;50(9):997–1013.
Griffen TC, Naumann E, Hildebrandt T. Mirror exposure therapy for body image disturbances and eating disorders: a review. Clin Psychol Rev. 2018;65:163–74.
Griffiths S, Mond JM, Murray SB, Touyz S. The prevalence and adverse associations of stigmatization in people with eating disorders. Int J Eat Disord. 2015;48(6):767–74.
Griffiths S, Rossell SL, Mitchison D, Murray SB, Mond JM. Pathways into treatment for eating disorders: a quantitative examination of treatment barriers and treatment attitudes. Eat Disord. 2018;26(6):556–74.
Grilo CM, Masheb RM, Wilson GT, Gueorguieva R, White MA. Cognitive–behavioral therapy, behavioral weight loss, and sequential treatment for obese patients with binge-eating disorder: a randomized controlled trial. J Consult Clin Psychol. 2011;79(5):675–85.
Grilo CM, White MA, Gueorguieva R, Barnes RD, Masheb RM. Self-help for binge eating disorder in primary care: a randomized controlled trial with ethnically and racially diverse obese patients. Behav Res Ther. 2013;51(12):855–61.
Grilo CM, White MA, Ivezaj V, Gueorguieva R. Randomized controlled trial of behavioral weight loss and stepped care for binge-eating disorder: 12-month follow-up. Obesity. 2020;28(11):2116–24.
Groff SE. Is enhanced cognitive behavioral therapy an effective intervention in eating disorders? A review. J Evid-Inform Soc Work. 2015;12(3):272–88.
Grover M, Naumann U, Mohammad-Dar L, Glennon D, Ringwood S, Eisler I, et al. A randomized controlled trial of an Internet-based cognitive-behavioural skills package for carers of people with anorexia nervosa. Psychol Med. 2011;41(12):2581–91.
Grover M, Williams C, Eisler I, Fairbairn P, McCloskey C, Smith G, et al. An off-line pilot evaluation of a web-based systemic cognitive-behavioral intervention for carers of people with anorexia nervosa. Int J Eat Disord. 2011;44(8):708–15.
Hay PJ, Claudino AM. Bulimia nervosa: online interventions. BMJ Clin Evid. 2015;2015:1009.
Hay PPJ, Bacaltchuk J, Stefano S, Kashyap P. Psychological treatments for bulimia nervosa and binging. Cochrane Database Syst Rev. 2009;2009(4):CD000562.
Hay P, Palavras MA, da Luz FQ, Dos Anjos GS, Sainsbury A, Touyz S, et al. Physical and mental health outcomes of an integrated cognitive behavioural and weight management therapy for people with an eating disorder characterized by binge eating and a high body mass index: a randomized controlled trial. BMC Psychiatry. 2022;22(1):355.
Hay PJ, Touyz S, Sud R. Treatment for severe and enduring anorexia nervosa: a review. Aust N Z J Psychiatry. 2012;46(12):1136–44.
Haynos AF, Pearson CM, Utzinger LM, Wonderlich SA, Crosby RD, Mitchell JE, et al. Empirically derived personality subtyping for predicting clinical symptoms and treatment response in bulimia nervosa. Int J Eat Disord. 2017;50(5):506–14.
Hazzard VM, Crosby RD, Crow SJ, Engel SG, Schaefer LM, Brewerton TD, et al. Treatment outcomes of psychotherapy for binge-eating disorder in a randomized controlled trial: examining the roles of childhood abuse and post-traumatic stress disorder. Eur Eat Disord Rev. 2021;29(4):611–21.
Herbrich-Bowe L, Bentz LK, Correll CU, Kappel V, van Noort BM. Randomized controlled trial of cognitive remediation therapy in adolescent inpatients with anorexia nervosa: neuropsychological outcomes. Eur Eat Disord Rev. 2022;30(6):772–86.
Herzog W, Wild B, Giel KE, Junne F, Friederich H-C, Resmark G, et al. Focal psychodynamic therapy, cognitive behaviour therapy, and optimised treatment as usual in female outpatients with anorexia nervosa (ANTOP study): 5-year follow-up of a randomised controlled trial in Germany. Lancet Psychiatry. 2022;9(4):280–90.
Hibbs R, Rhind C, Leppanen J, Treasure J. Interventions for caregivers of someone with an eating disorder: a meta-analysis. Int J Eat Disord. 2015;48(4):349–61.
Hilbert A, Hildebrandt T, Agras WS, Wilfley DE, Wilson GT. Rapid response in psychological treatments for binge eating disorder. J Consult Clin Psychol. 2015;83:649–54.
Hilbert A, Petroff D, Herpertz S, Pietrowsky R, Tuschen-Caffier B, Vocks S, et al. Meta-analysis of the efficacy of psychological and medical treatments for binge-eating disorder. J Consult Clin Psychol. 2019;87(1):91.
Hill DM, Craighead LW, Safer DL. Appetite-focused dialectical behavior therapy for the treatment of binge eating with purging: a preliminary trial. Int J Eat Disord. 2011;44(3):249–61.
Hodsoll J, Rhind C, Micali N, Hibbs R, Goddard E, Nazar BP, et al. A pilot, multicentre pragmatic randomised trial to explore the impact of carer skills training on carer and patient behaviours: testing the cognitive interpersonal model in adolescent anorexia nervosa. Eur Eat Disord Rev. 2017;25(6):551–61.
Högdahl L, Birgegård A, Björck C. How effective is bibliotherapy-based self-help cognitive behavioral therapy with Internet support in clinical settings? Results from a pilot study. Eat Weight Disord Stud Anorex Bulim Obes. 2013;18(1):37–44.
Hogdahl L, Birgegard A, Norring C, de Man LJ, Franko MA, Bjorck C. Internet-based cognitive behavioral therapy for bulimic eating disorders in a clinical setting: results from a randomized trial with one-year follow-up. Internet Interv. 2023;31: 100598.
Hoyle D, Slater J, Williams C, Schmidt U, Wade TD. Evaluation of a web-based skills intervention for carers of people with anorexia nervosa: a randomized controlled trial. Int J Eat Disord. 2013;46(6):634–8.
Hughes EK, Burton C, Le Grange D, Sawyer SM. The participation of mothers, fathers, and siblings in family-based treatment for adolescent anorexia nervosa. J Clin Child Adolesc Psychol. 2018;47(sup1):S456–66.
Hughes EK, Le Grange D, Court A, Sawyer SM. A case series of family-based treatment for adolescents with atypical anorexia nervosa. Int J Eat Disord. 2017;50(4):424–32.
Jenkins PE, Luck A, Violato M, Robinson C, Fairburn CG. Clinical and cost-effectiveness of two ways of delivering guided self-help for people with an eating disorder: a multi-arm randomized controlled trial. Int J Eat Disord. 2021;54(7):1224–37.
Jenkins PE, Morgan C, Houlihan C. Outpatient CBT for underweight patients with eating disorders: effectiveness within a national health service (NHS) eating disorders service. Behav Cogn Psychother. 2019;47(2):217–29.
Jewell T, Blessitt E, Stewart C, Simic M, Eisler I. Family therapy for child and adolescent eating disorders: a critical review. Fam Process. 2016;55(3):577–94.
Jones A, Clausen L. The efficacy of a brief group CBT program in treating patients diagnosed with bulimia nervosa: a brief report. Int J Eat Disord. 2013;46(6):560–2.
Jones C, Bryant-Waugh R, Turner HM, Gamble C, Melhuish L, Jenkins PE. Who benefits most from guided self-help for binge eating? An investigation into the clinical features of completers and non-completers. Eat Behav. 2012;13(2):146–9.
Juarascio A, Shaw J, Forman E, Timko CA, Herbert J, Butryn M, et al. Acceptance and commitment therapy as a novel treatment for eating disorders: an initial test of efficacy and mediation. Behav Modif. 2013;37(4):459–89.
Juarascio AS, Presseller EK, Srivastava P, Manasse SM, Forman EM. A randomized controlled trial of CBT+: a clinician-controlled, just-in-time, adjunctive intervention for bulimia-spectrum disorders. Behav Modif. 2022:1454455221109434.
Juarascio AS, Srivastava P, Manasse SM, Wilkinson ML, Felonis CR, Drexler SA. Reward retraining: a pilot randomized controlled trial of a novel treatment approach for transdiagnostic binge eating. Int J Eat Disord. 2023;56(3):662–70.
Juarascio AS, Forman EM, Herbert JD. Acceptance and commitment therapy versus cognitive therapy for the treatment of comorbid eating pathology. Behav Modif. 2010;34(2):175–90.
Kaidesoja M, Cooper Z, Fordham B. Cognitive behavioral therapy for eating disorders: a map of the systematic review evidence base. Int J Eat Disord. 2022;56(2):295–313.
Kambanis PE, Thomas JJ. Assessment and treatment of avoidant/restrictive food intake disorder. Curr Psychiatry Rep. 2023;14:14.
Karekla M, Nikolaou P, Merwin RM. Randomized clinical trial evaluating AcceptME-A digital gamified acceptance and commitment early intervention program for individuals at high risk for eating disorders. J Clin Med. 2022;11(7):1775.
Katterman SN, Kleinman BM, Hood MM, Nackers LM, Corsica JA. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: a systematic review. Eat Behav. 2014;15(2):197–204.
Katzman MA, Bara-Carril N, Rabe-Hesketh S, Schmidt U, Troop N, Treasure J. A randomized controlled two-stage trial in the treatment of bulimia nervosa, comparing CBT versus motivational enhancement in phase 1 followed by group versus individual cbt in phase 2. Psychosom Med. 2010;72(7):656–63.
Keegan E, Tchanturia K, Wade TD. Central coherence and set-shifting between nonunderweight eating disorders and anorexia nervosa: a systematic review and meta-analysis. Int J Eat Disord. 2021;54(3):229–43.
Kelly AC, Carter JC. Self-compassion training for binge eating disorder: a pilot randomized controlled trial. Psychol Psychother Theory Res Pract. 2015;88(3):285–303.
Klein AS, Skinner JB, Hawley KM. Targeting binge eating through components of dialectical behavior therapy: preliminary outcomes for individually supported diary card self-monitoring versus group-based DBT. Psychotherapy. 2013;50:543–52.
Knott S, Woodward D, Hoefkens A, Limbert C. Cognitive behaviour therapy for bulimia nervosa and eating disorders not otherwise specified: translation from randomized controlled trial to a clinical setting. Behav Cogn Psychother. 2015;43(6):641–54.
König H-H, Bleibler F, Friederich H-C, Herpertz S, Lam T, Mayr A, et al. Economic evaluation of cognitive behavioral therapy and Internet-based guided self-help for binge-eating disorder. Int J Eat Disord. 2018;51(2):155–64.
Kröger C, Schweiger U, Sipos V, Kliem S, Arnold R, Schunert T, et al. Dialectical behaviour therapy and an added cognitive behavioural treatment module for eating disorders in women with borderline personality disorder and anorexia nervosa or bulimia nervosa who failed to respond to previous treatments. An open trial with a 15-month follow-up. J Behav Ther Exp Psychiatry. 2010;41(4):381–8.
Lammers MW, Vroling MS, Crosby RD, van Strien T. Dialectical behavior therapy compared to cognitive behavior therapy in binge-eating disorder: an effectiveness study with 6-month follow-up. Int J Eat Disord. 2022;55(7):902–13.
Lampard AM, Byrne SM, McLean N, Fursland A. An evaluation of the enhanced cognitive-behavioural model of bulimia nervosa. Behav Res Ther. 2011;49(9):529–35.
Lane-Loney SE, Zickgraf HF, Ornstein RM, Mahr F, Essayli JH. A cognitive-behavioral family-based protocol for the primary presentations of avoidant/restrictive food intake disorder (ARFID): case examples and clinical research findings. Cogn Behav Pract. 2022;29(2):318–34.
Lavender A, Startup H, Naumann U, Samarawickrema N, DeJong H, Kenyon M, et al. Emotional and social mind training: a randomised controlled trial of a new group-based treatment for bulimia nervosa. PLoS ONE. 2012;7(10): e46047.
Lázaro L, Font E, Moreno E, Calvo R, Vila M, Andrés-Perpiñá S, et al. Effectiveness of self-esteem and social skills group therapy in adolescent eating disorder patients attending a day hospital treatment programme. Eur Eat Disord Rev. 2011;19(5):398–406.
Le LK-D, Hay P, Wade T, Touyz S, Mihalopoulos C. The cost-effectiveness of cognitive behavioral therapy for bulimia nervosa in the Australian context. Int J Eat Disord. 2017;50(12):1367–77.
Le LKD, Barendregt JJ, Hay P, Sawyer SM, Hughes EK, Mihalopoulos C. The modeled cost-effectiveness of family-based and adolescent-focused treatment for anorexia nervosa. Int J Eat Disord. 2017;50(12):1356–66.
Le Grange D, Lock J, Agras WS, Moye A, Bryson SW, Jo B, et al. Moderators and mediators of remission in family-based treatment and adolescent focused therapy for anorexia nervosa. Behav Res Ther. 2012;50(2):85–92.
Le Grange D, Lock J, Agras WS, Bryson SW, Jo B. Randomized clinical trial of family-based treatment and cognitive-behavioral therapy for adolescent bulimia nervosa. J Am Acad Child Adolesc Psychiatry. 2015;54(11):886-94.e2.
Le Grange D, Hughes EK, Court A, Yeo M, Crosby RD, Sawyer SM. Randomized clinical trial of parent-focused treatment and family-based treatment for adolescent anorexia nervosa. J Am Acad Child Adolesc Psychiatry. 2016;55(8):683–92.
Levinson CA, Rodebaugh TL, Fewell L, Kass AE, Riley EN, Stark L, et al. d-Cycloserine facilitation of exposure therapy improves weight regain in patients with anorexia nervosa: a pilot randomized controlled trial. J Clin Psychiatry. 2015;76(6):4033.
Linardon J, Fairburn CG, Fitzsimmons-Craft EE, Wilfley DE, Brennan L. The empirical status of the third-wave behaviour therapies for the treatment of eating disorders: a systematic review. Clin Psychol Rev. 2017;58:125–40.
Linardon J, Wade TD, de la Piedad GX, Brennan L. The efficacy of cognitive-behavioral therapy for eating disorders: a systematic review and meta-analysis. J Consult Clin Psychol. 2017;85:1080–94.
Linardon J, Wade T, de la Piedad GX, Brennan L. Psychotherapy for bulimia nervosa on symptoms of depression: a meta-analysis of randomized controlled trials. Int J Eat Disord. 2017;50(10):1124–36.
Linardon J, Shatte A, Messer M, Firth J, Fuller-Tyszkiewicz M. E-mental health interventions for the treatment and prevention of eating disorders: an updated systematic review and meta-analysis. J Consult Clin Psychol. 2020;88(11):994–1007.
Linardon J, Shatte A, Rosato J, Fuller-Tyszkiewicz M. Efficacy of a transdiagnostic cognitive-behavioral intervention for eating disorder psychopathology delivered through a smartphone app: a randomized controlled trial. Psychol Med. 2022;52(9):1679–90.
Linardon J, Messer M, Fuller-Tyszkiewicz M. Meta-analysis of the effects of cognitive-behavioral therapy for binge-eating–type disorders on abstinence rates in nonrandomized effectiveness studies: comparable outcomes to randomized, controlled trials? Int J Eat Disord. 2018;51(12):1303–11.
Linardon J, Kothe EJ, Fuller-Tyszkiewicz M. Efficacy of psychotherapy for bulimia nervosa and binge-eating disorder on self-esteem improvement: meta-analysis. Eur Eat Disord Rev. 2019;27(2):109–23.
Linnet J, Jensen ES, Runge E, Hansen MB, Hertz SPT, Mathiasen K, et al. Text based internet intervention of Binge Eating Disorder (BED): Words per message is associated with treatment adherence. Internet Interv. 2022;28: 100538.
Lock J, Le Grange D, Agras WS, Moye A, Bryson SW, Jo B. Randomized clinical trial comparing family-based treatment with adolescent-focused individual therapy for adolescents with anorexia nervosa. Arch Gen Psychiatry. 2010;67(10):1025–32.
Lock J, Le Grange D, Agras WS, Fitzpatrick KK, Jo B, Accurso E, et al. Can adaptive treatment improve outcomes in family-based therapy for adolescents with anorexia nervosa? Feasibility and treatment effects of a multi-site treatment study. Behav Res Ther. 2015;73:90–5.
Loeb KL, Lock J, Greif R, Le Grange D. Transdiagnostic theory and application of family-based treatment for youth with eating disorders. Cogn Behav Pract. 2012;19(1):17–30.
Low TL, Ho R, Ho C, Tam W. The efficacy of virtual reality in the treatment of binge-purging eating disorders: a meta-analysis. Eur Eat Disord Rev. 2021;29(1):52–9.
Lydecker JA, Grilo CM. Fathers and mothers with eating-disorder psychopathology: associations with child eating-disorder behaviors. J Psychosom Res. 2016;86:63–9.
Lynch FL, Striegel-Moore RH, Dickerson JF, Perrin N, DeBar L, Wilson GT, et al. Cost-effectiveness of guided self-help treatment for recurrent binge eating. J Consult Clin Psychol. 2010;78:322–33.
Macdonald P, Hibbs R, Corfield F, Treasure J. The use of motivational interviewing in eating disorders: a systematic review. Psychiatry Res. 2012;200(1):1–11.
MacDonald DE, McFarlane TL, Dionne MM, David L, Olmsted MP. Rapid response to intensive treatment for bulimia nervosa and purging disorder: a randomized controlled trial of a CBT intervention to facilitate early behavior change. J Consult Clin Psychol. 2017;85(9):896–908.
Madden S, Miskovic-Wheatley J, Wallis A, Kohn M, Hay P, Touyz S. Early weight gain in family-based treatment predicts greater weight gain and remission at the end of treatment and remission at 12-month follow-up in adolescent anorexia nervosa. Int J Eat Disord. 2015;48(7):919–22.
Magson NR, Handford CM, Norberg MM. The empirical status of cue exposure and response prevention treatment for binge eating: a systematic review. Behav Ther. 2021;52(2):442–54.
Mallorquí-Bagué N, Vintró-Alcaraz C, Sánchez I, Riesco N, Agüera Z, Granero R, et al. Emotion regulation as a transdiagnostic feature among eating disorders: cross-sectional and longitudinal approach. Eur Eat Disord Rev. 2018;26(1):53–61.
Månsson J, Parling T, Swenne I. Favorable effects of clearly defined interventions by parents at the start of treatment of adolescents with restrictive eating disorders. Int J Eat Disord. 2016;49(1):92–7.
Marco JH, Perpiñá C, Botella C. Effectiveness of cognitive behavioral therapy supported by virtual reality in the treatment of body image in eating disorders: one year follow-up. Psychiatry Res. 2013;209(3):619–25.
Marcos YQ, Cantero MCT. Assesment of social support dimensions in patients with eating disorders. Span J Psychol. 2009;12(1):226–36.
Masheb RM, Grilo CM, Rolls BJ. A randomized controlled trial for obesity and binge eating disorder: low-energy-density dietary counseling and cognitive-behavioral therapy. Behav Res Ther. 2011;49(12):821–9.
Mason TB, Crosby RD, Kolotkin RL, Grilo CM, Mitchell JE, Wonderlich SA, et al. Correlates of weight-related quality of life among individuals with binge eating disorder before and after cognitive behavioral therapy. Eat Behav. 2017;27:1–6.
Matthews A, Lenz KR, Peugh J, Copps EC, Peterson CM. Caregiver burden and illness perceptions in caregivers of medically hospitalized youth with anorexia nervosa. Eat Behav. 2018;29:14–8.
McClay C-A, Waters L, Schmidt U, Williams C. A survey of attitudes towards computerized self-help for eating disorders within a community-based sample. Behav Cogn Psychother. 2016;44(1):65–78.
McIntosh VVW, Carter FA, Bulik CM, Frampton CMA, Joyce PR. Five-year outcome of cognitive behavioral therapy and exposure with response prevention for bulimia nervosa. Psychol Med. 2011;41(5):1061–71.
McIntosh VVW, Jordan J, Carter JD, Frampton CMA, McKenzie JM, Latner JD, et al. Psychotherapy for transdiagnostic binge eating: a randomized controlled trial of cognitive-behavioural therapy, appetite-focused cognitive-behavioural therapy, and schema therapy. Psychiatry Res. 2016;240:412–20.
Daniela M, Robinson L, Gordon G, Werthmann J, Campbell IC, Schmidt U. The outcomes of mindfulness-based interventions for Obesity and Binge Eating Disorder: a meta-analysis of randomised controlled trials. Appetite. 2021;166: 105464.
Moberg LT, Solvang B, Sæle RG, Myrvang AD. Effects of cognitive-behavioral and psychodynamic-interpersonal treatments for eating disorders: a meta-analytic inquiry into the role of patient characteristics and change in eating disorder-specific and general psychopathology in remission. J Eat Disord. 2021;9(1):74.
Moghimi E, Davis C, Rotondi M. The efficacy of ehealth interventions for the treatment of adults diagnosed with full or subthreshold binge eating disorder: systematic review and meta-analysis. J Med Internet Res. 2021;23(7): e17874.
Monteleone AM, Pellegrino F, Croatto G, Carfagno M, Hilbert A, Treasure J, et al. Treatment of eating disorders: a systematic meta-review of meta-analyses and network meta-analyses. Neurosci Biobehav Rev. 2022;142: 104857.
Munsch S, Meyer AH, Biedert E. Efficacy and predictors of long-term treatment success for cognitive-behavioral treatment and behavioral weight-loss-treatment in overweight individuals with binge eating disorder. Behav Res Ther. 2012;50(12):775–85.
Murphy R, Straebler S, Basden S, Cooper Z, Fairburn CG. Interpersonal psychotherapy for eating disorders. Clin Psychol Psychother. 2012;19(2):150–8.
Murray SB, Anderson LK, Cusack A, Nakamura T, Rockwell R, Griffiths S, et al. Integrating family-based treatment and dialectical behavior therapy for adolescent bulimia nervosa: preliminary outcomes of an open pilot trial. Eat Disord. 2015;23(4):336–44.
Onnink CM, Konstantinidou Y, Moskovich AA, Karekla MK, Merwin RM. Acceptance and commitment therapy (ACT) for eating disorders: a systematic review of intervention studies and call to action. J Context Behav Sci. 2022;26:11–28.
O’Reilly GA, Cook L, Spruijt-Metz D, Black DS. Mindfulness-based interventions for obesity-related eating behaviours: a literature review. Obes Rev. 2014;15(6):453–61.
Pacanowski CR, Mason TB, Crosby RD, Mitchell JE, Crow SJ, Wonderlich SA, et al. Weight change over the course of binge eating disorder treatment: relationship to binge episodes and psychological factors. Obesity. 2018;26(5):838–44.
Palavras MA, Hay P, Santos CA, Claudino A. The efficacy of psychological therapies in reducing weight and binge eating in people with bulimia nervosa and binge eating disorder who are overweight or obese-a critical synthesis and meta-analyses. Nutrients. 2017;9(3):299.
Palavras MA, Hay P, Haider M, et al. Integrated weight loss and cognitive behavioural therapy (CBT) for the treatment of recurrent binge eating and high body mass index: a randomized controlled trial. Eat Weight Disord. 2021;26(1):249–62.
Parling T, Cernvall M, Ramklint M, Holmgren S, Ghaderi A. A randomised trial of acceptance and commitment therapy for anorexia nervosa after daycare treatment, including five-year follow-up. BMC Psychiatry. 2016;16(1):1–13.
Paslakis G, Fauck V, Röder K, Rauh E, Rauh M, Erim Y. Virtual reality jogging as a novel exposure paradigm for the acute urge to be physically active in patients with eating disorders: implications for treatment. Int J Eat Disord. 2017;50(11):1243–6.
Peat CM, Berkman ND, Lohr KN, Brownley KA, Bann CM, Cullen K, et al. Comparative effectiveness of treatments for binge-eating disorder: systematic review and network meta-analysis. Eur Eat Disord Rev. 2017;25(5):317–28.
Pépin G, King R. Collaborative care skill training workshop: how Australian carers support a loved one with an eating disorder. Adv Eat Disord. 2016;4(1):47–58.
Pépin G, King R. Collaborative care skills training workshops: helping carers cope with eating disorders from the UK to Australia. Soc Psychiatry Psychiatr Epidemiol. 2013;48(5):805–12.
Perpiñá C, Roncero M, Fernández-Aranda F, Jiménez-Murcia S, Forcano L, Sánchez I. Clinical validation of a virtual environment for normalizing eating patterns in eating disorders. Compr Psychiatry. 2013;54(6):680–6.
Peterson CB, Berg KC, Crosby RD, Lavender JM, Accurso EC, Ciao AC, et al. The effects of psychotherapy treatment on outcome in bulimia nervosa: examining indirect effects through emotion regulation, self-directed behavior, and self-discrepancy within the mediation model. Int J Eat Disord. 2017;50(6):636–47.
Peterson CB, Engel SG, Crosby RD, Strauman T, Smith TL, Klein M, et al. Comparing integrative cognitive-affective therapy and guided self-help cognitive-behavioral therapy to treat binge-eating disorder using standard and naturalistic momentary outcome measures: a randomized controlled trial. Int J Eat Disord. 2020;53(9):1418–27.
Philipp J, Franta C, Zeiler M, Truttmann S, Wittek T, Imgart H, et al. Does a skills intervention for parents have a positive impact on adolescents’ anorexia nervosa outcome? Answers from a quasi-randomised feasibility trial of SUCCEAT. Int J Environ Res Public Health. 2021;18(9):4656.
Pinto-Gouveia J, Carvalho SA, Palmeira L, Castilho P, Duarte C, Ferreira C, et al. BEfree: a new psychological program for binge eating that integrates psychoeducation, mindfulness, and compassion. Clin Psychol Psychother. 2017;24(5):1090–8.
Pisetsky EM, Durkin NE, Crosby RD, Berg KC, Mitchell JE, Crow SJ, et al. Examination of early group dynamics and treatment outcome in a randomized controlled trial of group cognitive behavior therapy for binge eating disorder. Behav Res Ther. 2015;73:74–8.
Polnay A, James VAW, Hodges L, Murray GD, Munro C, Lawrie SM. Group therapy for people with bulimia nervosa: systematic review and meta-analysis. Psychol Med. 2014;44(11):2241–54.
Poulsen S, Lunn S, Daniel SIF, Folke S, Mathiesen BB, Katznelson H, et al. A randomized controlled trial of psychoanalytic psychotherapy or cognitive-behavioral therapy for bulimia nervosa. Am J Psychiatry. 2014;171(1):109–16.
Puls H-C, Schmidt R, Hilbert A. Therapist adherence and therapeutic alliance in individual cognitive-behavioural therapy for adolescent binge-eating disorder. Eur Eat Disord Rev. 2019;27(2):182–94.
Quadflieg N, Schädler D, Naab S, Fichter MM. RCT of a video-based intervention program for caregivers of patients with an eating disorder. Eur Eat Disord Rev. 2017;25(4):283–92.
Rahmani M, Omidi A, Asemi Z, Akbari H. The effect of dialectical behaviour therapy on binge eating, difficulties in emotion regulation and BMI in overweight patients with binge-eating disorder: a randomized controlled trial. Ment Health Prev. 2018;9:13–8.
Ramklint M, Jeansson M, Holmgren S, Ghaderi A. Guided self-help as the first step for bulimic symptoms: implementation of a stepped-care model within specialized psychiatry. Int J Eat Disord. 2012;45(1):70–8.
Raykos BC, McEvoy PM, Erceg-Hurn D, Byrne SM, Fursland A, Nathan P. Therapeutic alliance in enhanced cognitive behavioural therapy for bulimia nervosa: probably necessary but definitely insufficient. Behav Res Ther. 2014;57:65–71.
Raykos BC, McEvoy PM, Carter O, Fursland A, Nathan P. Interpersonal problems across restrictive and binge-purge samples: data from a community-based eating disorders clinic. Eat Behav. 2014;15(3):449–52.
Ricca V, Castellini G, Mannucci E, Lo Sauro C, Ravaldi C, Rotella CM, et al. Comparison of individual and group cognitive behavioral therapy for binge eating disorder. A randomized, three-year follow-up study. Appetite. 2010;55(3):656–65.
Richards IL, Subar A, Touyz S, Rhodes P. Augmentative approaches in family-based treatment for adolescents with restrictive eating disorders: a systematic review. Eur Eat Disord Rev. 2018;26(2):92–111.
Rieger E, Van Buren DJ, Bishop M, Tanofsky-Kraff M, Welch R, Wilfley DE. An eating disorder-specific model of interpersonal psychotherapy (IPT-ED): causal pathways and treatment implications. Clin Psychol Rev. 2010;30(4):400–10.
Riesco N, Agüera Z, Granero R, Jiménez-Murcia S, Menchón JM, Fernández-Aranda F. Other Specified Feeding or Eating Disorders (OSFED): clinical heterogeneity and cognitive-behavioral therapy outcome. Eur Psychiatry. 2018;54:109–16.
Robinson AL, Strahan E, Girz L, Wilson A, Boachie A. ‘I know i can help you’: parental self-efficacy predicts adolescent outcomes in family-based therapy for eating disorders. Eur Eat Disord Rev. 2013;21(2):108–14.
Romero-Martínez Á, Ruiz-Robledillo N, Moya-Albiol L. Depressive mood and testosterone related to declarative verbal memory decline in middle-aged caregivers of children with eating disorders. Int J Environ Res Public Health. 2016;13(3):286.
Rossi E, Castellini G, Cassioli E, Sensi C, Mancini M, Stanghellini G, et al. The role of embodiment in the treatment of patients with anorexia and bulimia nervosa: a 2-year follow-up study proposing an integration between enhanced cognitive behavioural therapy and a phenomenological model of eating disorders. Eat Weight Disord Stud Anorex Bulim Obes. 2021;26(8):2513–22.
Rozakou-Soumalia N, Darvariu S, Sjogren JM. Dialectical behaviour therapy improves emotion dysregulation mainly in binge eating disorder and bulimia nervosa: a systematic review and meta-analysis. J Pers Med. 2021;11(9):18.
Sánchez-Ortiz VC, Munro C, Startup H, Treasure J, Schmidt U. The role of email guidance in internet-based cognitive-behavioural self-care treatment for bulimia nervosa. Eur Eat Disord Rev. 2011;19(4):342–8.
Scanferla E, Pachoud B, Gorwood P. Experiencing eight psychotherapy approaches devoted to eating disorders in a single-day workshop increases insight and motivation to engage in care: a pilot study. Eat Weight Disord. 2022;27(6):2213–22.
Schag K, Rennhak SK, Leehr EJ, Skoda E-M, Becker S, Bethge W, et al. IMPULS: impulsivity-focused group intervention to reduce binge eating episodes in patients with binge eating disorder–a randomised controlled trial. Psychother Psychosom. 2019;88(3):141–53.
Schlegl S, Bürger C, Schmidt L, Herbst N, Voderholzer U. The potential of technology-based psychological interventions for anorexia and bulimia nervosa: a systematic review and recommendations for future research. J Med Internet Res. 2015;17(3): e85.
Schlup B, Meyer AH, Munsch S. A non-randomized direct comparison of cognitive-behavioral short- and long-term treatment for binge eating disorder. Obes Facts. 2010;3(4):261–6.
Schwarte R, Timmesfeld N, Dempfle A, Krei M, Egberts K, Jaite C, et al. Expressed emotions and depressive symptoms in caregivers of adolescents with first-onset anorexia nervosa—a long-term investigation over 2.5 years. Eur Eat Disord Rev. 2017;25(1):44–51.
Shimshoni Y, Silverman WK, Lebowitz ER. SPACE-ARFID: a pilot trial of a novel parent-based treatment for avoidant/restrictive food intake disorder. Int J Eat Disord. 2020;53(10):1623–35.
Slade E, Keeney E, Mavranezouli I, Dias S, Fou L, Stockton S, et al. Treatments for bulimia nervosa: a network meta-analysis. Psychol Med. 2018;48(16):2629–36.
Södersten P, Bergh C, Leon M, Brodin U, Zandian M. Cognitive behavior therapy for eating disorders versus normalization of eating behavior. Physiol Behav. 2017;174:178–90.
Solmi M, Wade TD, Byrne S, Del Giovane C, Fairburn CG, Ostinelli EG, et al. Comparative efficacy and acceptability of psychological interventions for the treatment of adult outpatients with anorexia nervosa: a systematic review and network meta-analysis. Lancet Psychiatry. 2021;8(3):215–24.
Spielmans GI, Benish SG, Marin C, Bowman WM, Menster M, Wheeler AJ. Specificity of psychological treatments for bulimia nervosa and binge eating disorder? A meta-analysis of direct comparisons. Clin Psychol Rev. 2013;33(3):460–9.
Steele AL, Bergin J, Wade TD. Self-efficacy as a robust predictor of outcome in guided self-help treatment for broadly defined bulimia nervosa. Int J Eat Disord. 2011;44(5):389–96.
Stefanini MC, Troiani MR, Caselli M, Dirindelli P, Lucarelli S, Caini S, et al. Living with someone with an eating disorder: factors affecting the caregivers’ burden. Eat Weight Disord. 2019;24(6):1209–14.
Stefini A, Salzer S, Reich G, Horn H, Winkelmann K, Bents H, et al. Cognitive-behavioral and psychodynamic therapy in female adolescents with bulimia nervosa: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2017;56(4):329–35.
Stein KF, Corte C, Chen D-G, Nuliyalu U, Wing J. A randomized clinical trial of an identity intervention programme for women with eating disorders. Eur Eat Disord Rev. 2013;21(2):130–42.
Steinberg D, Perry T, Freestone D, Bohon C, Baker JH, Parks E. Effectiveness of delivering evidence-based eating disorder treatment via telemedicine for children, adolescents, and youth. Brunner-Mazel Eat Disord Monogr Ser. 2023;31(1):85–101.
Steinglass JE, Sysko R, Glasofer D, Albano AM, Simpson HB, Walsh BT. Rationale for the application of exposure and response prevention to the treatment of anorexia nervosa. Int J Eat Disord. 2011;44(2):134–41.
Steinglass JE, Albano AM, Simpson HB, Wang Y, Zou J, Attia E, et al. Confronting fear using exposure and response prevention for anorexia nervosa: a randomized controlled pilot study. Int J Eat Disord. 2014;47(2):174–80.
Stice E, Rohde P, Shaw H, Gau JM. Randomized trial of a dissonance-based group treatment for eating disorders versus a supportive mindfulness group treatment. J Consult Clin Psychol. 2019;87:79–90.
Stiles-Shields C, Touyz S, Hay P, Lacey H, Crosby RD, Rieger E, et al. Therapeutic alliance in two treatments for adults with severe and enduring anorexia nervosa. Int J Eat Disord. 2013;46(8):783–9.
Stiles-Shields C, Rienecke Hoste R, M. Doyle P, Le Grange D. A review of family-based treatment for adolescents with eating disorders. Rev Recent Clin Trials. 2012;7(2):133–40.
Strandskov SW, Ghaderi A, Andersson H, Parmskog N, Hjort E, Wärn AS, et al. Effects of tailored and ACT-influenced internet-based CBT for eating disorders and the relation between knowledge acquisition and outcome: a randomized controlled trial. Behav Ther. 2017;48(5):624–37.
Striegel-Moore RH, Wilson GT, DeBar L, Perrin N, Lynch F, Rosselli F, et al. Cognitive behavioral guided self-help for the treatment of recurrent binge eating. J Consult Clin Psychol. 2010;78:312–21.
Swenne I, Parling T, Ros HS. Family-based intervention in adolescent restrictive eating disorders: early treatment response and low weight suppression is associated with favourable one-year outcome. BMC Psychiatry. 2017;17(1):1–10.
Tatham M. The role of imagery-based techniques in cognitive–behavioural therapy for adults with eating disorders. Clin Psychol Rev. 2011;31(7):1101–9.
Tecuta L, Tomba E. Subjective incompetence as a predictor of treatment outcomes in eating disorder outpatients. Psychiatry Res. 2018;266:193–8.
ter Huurne ED, de Haan HA, Postel MG, van der Palen J, VanDerNagel JEL, DeJong CAJ. Web-based cognitive behavioral therapy for female patients with eating disorders: randomized controlled trial. J Med Internet Res. 2015;17(6):3946.
Ter Huurne ED, de Haan HA, Postel MG, DeJong CAJ, VanDerNagel JEL, van der Palen J. Long-term effectiveness of web-based cognitive behavioral therapy for patients with eating disorders. Eat Weight Disord. 2021;26(3):911–9.
Thomas JJ, Lawson EA, Micali N, Misra M, Deckersbach T, Eddy KT. Avoidant/restrictive food intake disorder: a three-dimensional model of neurobiology with implications for etiology and treatment. Curr Psychiatry Rep. 2017;19(8):54.
Thomas JJ, Becker KR, Breithaupt L, Murray HB, Jo JH, Kuhnle MC, et al. Cognitive-behavioral therapy for adults with avoidant/restrictive food intake disorder. J Behav Cogn Ther. 2021;31(1):47–55.
Thomas JJ, Wons OB, Eddy KT. Cognitive–behavioral treatment of avoidant/restrictive food intake disorder. Curr Opin Psychiatry. 2018;31(6):425–30.
Thompson-Brenner H, Boisseau CL, Satir DA. Adolescent eating disorders: treatment and response in a naturalistic study. J Clin Psychol. 2010;66(3):277–301.
Thompson-Brenner H, Shingleton RM, Sauer-Zavala S, Richards LK, Pratt EM. Multiple measures of rapid response as predictors of remission in cognitive behavior therapy for bulimia nervosa. Behav Res Ther. 2015;64:9–14.
Thompson-Brenner H, Shingleton RM, Thompson DR, Satir DA, Richards LK, Pratt EM, et al. Focused vs. broad enhanced cognitive behavioral therapy for bulimia nervosa with comorbid borderline personality: a randomized controlled trial. Int J Eat Disord. 2016;49(1):36–49.
Thompson-Brenner H, Singh S, Gardner T, Brooks GE, Smith MT, Lowe MR, et al. The renfrew unified treatment for eating disorders and comorbidity: long-term effects of an evidence-based practice implementation in residential treatment. Front Psychiatry. 2021;12: 641601.
Traviss GD, Heywood-Everett S, Hill AJ. Guided self-help for disordered eating: a randomised control trial. Behav Res Ther. 2011;49(1):25–31.
Traviss-Turner GD, West RM, Hill AJ. Guided self-help for eating disorders: a systematic review and metaregression. Eur Eat Disord Rev. 2017;25(3):148–64.
Turner H, Bryant-Waugh R, Marshall E. The impact of early symptom change and therapeutic alliance on treatment outcome in cognitive-behavioural therapy for eating disorders. Behav Res Ther. 2015;73:165–9.
Valenzuela F, Lock J, Le Grange D, Bohon C. Comorbid depressive symptoms and self-esteem improve after either cognitive-behavioural therapy or family-based treatment for adolescent bulimia nervosa. Eur Eat Disord Rev. 2018;26(3):253–8.
Vancampfort D, Probst M, Adriaens A, Pieters G, De Hert M, Stubbs B, et al. Changes in physical activity, physical fitness, self-perception and quality of life following a 6-month physical activity counseling and cognitive behavioral therapy program in outpatients with binge eating disorder. Psychiatry Res. 2014;219(2):361–6.
Vancampfort D, De Herdt A, Vanderlinden J, Lannoo M, Soundy A, Pieters G, et al. Health related quality of life, physical fitness and physical activity participation in treatment-seeking obese persons with and without binge eating disorder. Psychiatry Res. 2014;216(1):97–102.
Vaz AR, Conceição E, Machado PPP. Guided self-help CBT treatment for bulimic disorders: effectiveness and clinically significant change. Psychother Res. 2013;23(3):324–32.
Vaz AR, Conceição E, Machado PPP. Early response as a predictor of success in guided self-help treatment for bulimic disorders. Eur Eat Disord Rev. 2014;22(1):59–65.
Vella-Zarb RA, Mills JS, Westra HA, Carter JC, Keating L. A randomized controlled trial of motivational interviewing + self-help versus psychoeducation + self-help for binge eating. Int J Eat Disord. 2015;48(3):328–32.
Vocks S, Tuschen-Caffier B, Pietrowsky R, Rustenbach SJ, Kersting A, Herpertz S. Meta-analysis of the effectiveness of psychological and pharmacological treatments for binge eating disorder. Int J Eat Disord. 2010;43(3):205–17.
Vogel EN, Singh S, Accurso EC. A systematic review of cognitive behavior therapy and dialectical behavior therapy for adolescent eating disorders. J Eat Disord. 2021;9(1):131.
von Brachel R, Hötzel K, Hirschfeld G, Rieger E, Schmidt U, Kosfelder J, et al. Internet-based motivation program for women with eating disorders: eating disorder pathology and depressive mood predict dropout. J Med Internet Res. 2014;16(3):3104.
Wade TD, Allen K, Crosby RD, Fursland A, Hay P, McIntosh V, et al. Outpatient therapy for adult anorexia nervosa: early weight gain trajectories and outcome. Eur Eat Disord Rev. 2021;29(3):472–81.
Wade TD, Ghan C, Waller G. A randomized controlled trial of two 10-session cognitive behaviour therapies for eating disorders: an exploratory investigation of which approach works best for whom. Behav Res Ther. 2021;146: 103962.
Wagner G, Penelo E, Wanner C, Gwinner P, Trofaier M-L, Imgart H, et al. Internet-delivered cognitive-behavioural therapy v. conventional guided self-help for bulimia nervosa: long-term evaluation of a randomised controlled trial. Br J Psychiatry. 2013;202(2):135–41.
Wagner G, Penelo E, Nobis G, Mayrhofer A, Wanner C, Schau J, et al. Predictors for good therapeutic outcome and drop-out in technology assisted guided self-help in the treatment of bulimia nervosa and bulimia like phenotype. Eur Eat Disord Rev. 2015;23(2):163–9.
Wagner B, Nagl M, Dölemeyer R, Klinitzke G, Steinig J, Hilbert A, et al. Randomized controlled trial of an internet-based cognitive-behavioral treatment program for binge-eating disorder. Behav Ther. 2016;47(4):500–14.
Walker G, Bryant W. Peer support in adult mental health services: a metasynthesis of qualitative findings. Psychiatr Rehabil J. 2013;36(1):28–34.
Waller G, Gray E, Hinrichsen H, Mountford V, Lawson R, Patient E. Cognitive-behavioral therapy for bulimia nervosa and atypical bulimic nervosa: effectiveness in clinical settings. Int J Eat Disord. 2014;47(1):13–7.
Watson HJ, Steele AL, Bergin JL, Fursland A, Wade TD. Bulimic symptomatology: the role of adaptive perfectionism, shape and weight concern, and self-esteem. Behav Res Ther. 2011;49(9):565–72.
Watson HJ, Levine MD, Zerwas SC, Hamer RM, Crosby RD, Sprecher CS, et al. Predictors of dropout in face-to-face and internet-based cognitive-behavioral therapy for bulimia nervosa in a randomized controlled trial. Int J Eat Disord. 2017;50(5):569–77.
Watson H. Internet-based CBT cost effective for bulimia nervosa. PharmacoEconomics Outcomes News. 2018;794:18–23.
Wilson GT, Zandberg LJ. Cognitive–behavioral guided self-help for eating disorders: effectiveness and scalability. Clin Psychol Rev. 2012;32(4):343–57.
Wonderlich SA, Peterson CB, Crosby RD, Smith TL, Klein MH, Mitchell JE, et al. A randomized controlled comparison of integrative cognitive-affective therapy (ICAT) and enhanced cognitive-behavioral therapy (CBT-E) for bulimia nervosa. Psychol Med. 2014;44(3):543–53.
Zerwas SC, Watson HJ, Hofmeier SM, Levine MD, Hamer RM, Crosby RD, et al. CBT4BN: a randomized controlled trial of online chat and face-to-face group therapy for bulimia nervosa. Psychother Psychosom. 2017;86(1):47–53.
Zipfel S, Wild B, Groß G, Friederich H-C, Teufel M, Schellberg D, et al. Focal psychodynamic therapy, cognitive behaviour therapy, and optimised treatment as usual in outpatients with anorexia nervosa (ANTOP study): randomised controlled trial. Lancet. 2014;383(9912):127–37.
Bourion-Bedes S, Baumann C, Kermarrec S, Ligier F, Feillet PDF, Bonnemains C, et al. Prognostic value of early therapeutic alliance in weight recovery: a prospective cohort of 108 adolescents with anorexia nervosa—ClinicalKey. J Adolesc Health. 2013;53(3):344–50.
Agras WS, Walsh T, Fairburn CG, Wilson GT, Kraemer HC. A multicenter comparison of cognitive-behavioral therapy and interpersonal psychotherapy for bulimia nervosa. Arch Gen Psychiatry. 2000;57(5):459–66.
Calugi S, El Ghoch M, Dalle GR. Intensive enhanced cognitive behavioural therapy for severe and enduring anorexia nervosa: a longitudinal outcome study. Behav Res Ther. 2017;89:41–8.
Hughes EK, Le Grange D, Court A, Yeo M, Campbell S, Whitelaw M, et al. Implementation of family-based treatment for adolescents with anorexia nervosa. J Pediatr Health Care. 2014;28(4):322–30.
Paris J. Suicidality in borderline personality disorder. Medicina. 2019;55(6):223.
Miniati M, Callari A, Maglio A, Calugi S. Interpersonal psychotherapy for eating disorders: current perspectives. Psychol Res Behav Manag. 2018;11:353–69.
Carter FA, Jordan J, McIntosh VV, Luty SE, McKenzie JM, Frampton CM, et al. The long-term efficacy of three psychotherapies for anorexia nervosa: a randomized, controlled trial. Int J Eat Disord. 2011;44(7):647–54.
Pittock A, Hodges L, Lawrie SM. The effectiveness of internet-delivered cognitive behavioural therapy for those with bulimic symptoms: a systematic review. BMC Res Notes. 2018;11(1):748.
Mitchell JE, Crosby RD, Wonderlich SA, Crow S, Lancaster K, Simonich H, et al. A randomized trial comparing the efficacy of cognitive–behavioral therapy for bulimia nervosa delivered via telemedicine versus face-to-face. Behav Res Ther. 2008;46(5):581–92.
Wilfley DE, Welch RR, Stein RI, Spurrell EB, Cohen LR, Saelens BE, et al. A randomized comparison of group cognitive-behavioral therapy and group interpersonal psychotherapy for the treatment of overweight individuals with binge-eating disorder. Arch Gen Psychiatry. 2002;59(8):713–21.
Acknowledgements
The authors would like to thank and acknowledge the hard work of Healthcare Management Advisors (HMA) who were commissioned to undertake the Rapid Review. Additionally, the authors would like to thank all members of the consortium and consultation committees for their advice, input, and considerations during the development process. Further, a special thank you to the carers, consumers and lived experience consultants that provided input to the development of the Rapid Review and wider national Eating Disorders Research and Translation Strategy. Finally, thank you to the Australian Government—Department of Health for their support of the current project.
National Eating Disorder Research Consortium Members (alphabetical order of surname): * indicates named authors
Author | Primary affiliation |
|---|---|
Phillip Aouad | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Sarah Barakat | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Robert Boakes | School of Psychology, Faculty of Science, University of Sydney, NSW Australia |
Leah Brennan | School of Psychology and Public Health, La Trobe University, Victoria, Australia |
Emma Bryant* | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Susan Byrne | School of Psychology, Western Australia, Perth, Australia |
Belinda Caldwell | Eating Disorders Victoria, Victoria, Australia |
Shannon Calvert | Perth, Western Australia, Australia |
Bronny Carroll | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
David Castle | Medicine, Dentistry and Health Sciences, University of Melbourne, Victoria, Australia |
Ian Caterson | School of Life and Environmental Sciences, University of Sydney, Sydney, New South Wales, Australia |
Belinda Chelius | Eating Disorders Queensland, Brisbane, Queensland, Australia |
Lyn Chiem | Sydney Local Health District, New South Wales Health, Sydney, Australia |
Simon Clarke | Westmead Hospital, Sydney, New South Wales, Australia |
Janet Conti | Translational Health Research Institute, Western Sydney University, Sydney NSW Australia |
Lexi Crouch | Brisbane, Queensland, Australia |
Genevieve Dammery | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Natasha Dzajkovski | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Jasmine Fardouly | School of Psychology, University of New South Wales, Sydney, New South Wales, Australia |
John Feneley | New South Wales Health, New South Wales, Australia |
Nasim Foroughi | Translational Health Research Institute, Western Sydney University, Sydney NSW Australia |
Mathew Fuller-Tyszkiewicz | School of Psychology, Faculty of Health, Deakin University, Victoria, Australia |
Anthea Fursland | School of Population Health, Faculty of Health Sciences, Curtain University, Perth, Australia |
Veronica Gonzalez-Arce | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Bethanie Gouldthorp | Hollywood Clinic, Ramsay Health Care, Perth, Australia |
Kelly Griffin | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Scott Griffiths | Melbourne School of Psychological Sciences, University of Melbourne, Victoria, Australia |
Ashlea Hambleton | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Amy Hannigan | Queensland Eating Disorder Service, Brisbane, Queensland, Australia |
Mel Hart | Hunter New England Local Health District, New South Wales, Australia |
Susan Hart | St Vincent’s Hospital Network Local Health District, Sydney, New South Wales, Australia |
Phillipa Hay | Translational Health Research Institute, Western Sydney University, Sydney NSW Australia |
Ian Hickie | Brain and Mind Centre, University of Sydney, Sydney, Australia |
Francis Kay-Lambkin | School of Medicine and Public Health, University of Newcastle, New South Wales, Australia |
Ross King | School of Psychology, Faculty of Health, Deakin University, Victoria, Australia |
Michael Kohn | Westmead Hospital, University of Sydney, Australia |
Eyza Koreshe | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Isabel Krug | Melbourne School of Psychological Sciences, University of Melbourne, Victoria, Australia |
Jake Linardon | School of Psychology, Faculty of Health, Deakin University, Victoria, Australia |
Randall Long | College of Medicine and Public Health, Flinders University, South Australia, Australia |
Amanda Long | Exchange Consultancy, Redlynch, New South Wales, Australia |
Sloane Madden | Eating Disorders Service, Children’s Hospital at Westmead, Sydney, New South Wales, Australia |
Sarah Maguire* | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Danielle Maloney* | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Peta Marks | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Siân McLean | School of Psychology and Public Health, La Trobe University, Victoria, Australia |
Thy Meddick | Clinical Excellence Queensland, Mental Health Alcohol and Other Drugs Branch, Brisbane, Queensland, Australia |
Jane Miskovic-Wheatley* | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Deborah Mitchison | Translational Health Research Institute, Western Sydney University, Sydney NSW Australia |
Richard O’Kearney | College of Health & Medicine, Australian National University, Australian Capital Territory, Australia |
Shu Hwa Ong | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Roger Paterson | ADHD and BED Integrated Clinic, Melbourne, Victoria, Australia |
Susan Paxton | La Trobe University, Department of Psychology and Counselling, Victoria, Australia |
Melissa Pehlivan* | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Genevieve Pepin | School of Health & Social Development, Faculty of Health, Deakin University, Geelong, Victoria, Australia |
Andrea Phillipou | Swinburne Anorexia Nervosa (SWAN) Research Group, Centre for Mental Health, School of Health Sciences, Swinburne University, Victoria, Australia |
Judith Piccone | Children's Health Queensland Hospital and Health Service, Brisbane, Queensland, Australia |
Rebecca Pinkus | School of Psychology, Faculty of Science, University of Sydney, NSW Australia |
Bronwyn Raykos | Centre for Clinical Interventions, Western Australia Health, Perth, Western Australia, Australia |
Paul Rhodes | School of Psychology, Faculty of Science, University of Sydney, NSW Australia |
Elizabeth Rieger | College of Health and Medicine, Australian National University, Australian Capital Territory, Australia |
Karen Rockett | New South Wales Health, New South Wales, Australia |
Sarah Rodan | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Janice Russell | Central Clinical School Brain and Mind Research Institute, University of Sydney, New South Wales, Sydney |
Haley Russell | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Fiona Salter | Ramsay Health Care, Perth, Australia |
Susan Sawyer | Department of Paediatrics, The University of Melbourne, Australia |
Beth Shelton | National Eating Disorders Collaboration, Victoria, Australia |
Urvashnee Singh | The Hollywood Clinic Hollywood Private Hospital, Ramsey Health, Perth, Australia |
Sophie Smith | Sydney, New South Wales, Australia |
Evelyn Smith | Translational Health Research Institute, Western Sydney University, Sydney NSW Australia |
Karen Spielman | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Sarah Squire | The Butterfly Foundation, Sydney, Australia |
Juliette Thomson | The Butterfly Foundation, Sydney, Australia |
Marika Tiggemann | College of Education, Psychology and Social Work, Flinders University, South Australia, Australia |
Stephen Touyz* | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Ranjani Utpala | The Butterfly Foundation, Sydney, Australia |
Lenny Vartanian | School of Psychology, University of New South Wales, Sydney, New South Wales, Australia |
Sabina Vatter | InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia |
Andrew Wallis | Eating Disorder Service, The Sydney Children’s Hospital Network, Westmead Campus, Sydney, Australia |
Warren Ward | Department of Psychiatry, University of Queensland, Brisbane, Australia |
Sarah Wells | University of Tasmania, Tasmania, Australia |
Eleanor Wertheim | School of Psychology and Public Health, La Trobe University, Victoria, Australia |
Simon Wilksch | College of Education, Psychology and Social Work, Flinders University, South Australia, Australia |
Michelle Williams | Royal Hobart, Tasmanian Health Service, Tasmania, Australia |
Funding
The RR was in-part funded by the Australian Government Department of Health in partnership with other national and jurisdictional stakeholders. As the organisation responsible for overseeing the National Eating Disorder Research and Translation Strategy, InsideOut Institute commissioned Healthcare Management Advisors to undertake the RR as part of a larger, ongoing, project. Role of Funder: The funder was not directly involved in informing the development of the current review.
Author information
Authors and Affiliations
Consortia
Contributions
PM, ST and SM oversaw the Rapid Review process; AL carried out and wrote the initial HMA report; HR and PA wrote the current manuscript; all authors edited and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
ST receives royalties from Hogrefe and Huber, McGraw Hill and Taylor and Francis for published books/book chapters. He has received honoraria from the Takeda Group of Companies for consultative work, public speaking engagements and commissioned reports. He has chaired their Clinical Advisory Committee for Binge Eating Disorder. He is the Editor in Chief of the Journal of Eating Disorders. ST is a committee member of the National Eating Disorders Collaboration as well as the Technical Advisory Group for Eating Disorders. AL undertook work on this RR while employed by HMA. PA and SM are guest editors of the special issue “Improving the future by understanding the present: evidence reviews for the field of eating disorders”, in the Journal of Eating Disorders.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Russell, H., Aouad, P., Le, A. et al. Psychotherapies for eating disorders: findings from a rapid review. J Eat Disord 11, 175 (2023). https://doi.org/10.1186/s40337-023-00886-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40337-023-00886-w