Abstract
Background
Despite global efforts to reduce and eventually interrupt malaria transmission, the disease remains a pressing public health problem, especially in sub-Saharan Africa. This study presents a detailed spatio-temporal analysis of malaria transmission in Rwanda from 2012 to 2022. The main objective was to gain insights into the evolving patterns of malaria and to inform and tailor effective public health strategies.
Methods
The study used yearly aggregated data of malaria cases from the Rwanda health management information system. We employed a multifaceted analytical approach, including descriptive statistics and spatio-temporal analysis across three demographic groups: children under the age of 5 years, and males and females above 5 years. Bayesian spatially explicit models and spatio scan statistics were utilised to examine geographic and temporal patterns of relative risks and to identify clusters of malaria transmission.
Results
We observed a significant increase in malaria cases from 2014 to 2018, peaking in 2016 for males and females aged above 5 years with counts of 98,645 and 116,627, respectively and in 2018 for under 5-year-old children with 84,440 cases with notable geographic disparities. Districts like Kamonyi (Southern Province), Ngoma, Kayonza and Bugesera (Eastern Province) exhibited high burdens, possibly influenced by factors such as climate, vector control practices, and cross-border dynamics. Bayesian spatially explicit modeling revealed elevated relative risks in numerous districts, underscoring the heterogeneity of malaria transmission in these districts, and thus contributing to an overall rising trend in malaria cases until 2018, followed by a subsequent decline. Our findings emphasize that the heterogeneity of malaria transmission is potentially driven by ecologic, socioeconomic, and behavioural factors.
Conclusions
The study underscores the complexity of malaria transmission in Rwanda and calls for climate adaptive, gender-, age- and district-specific strategies in the national malaria control program. The emergence of both artemisinin and pyrethoids resistance and persistent high transmission in some districts necessitates continuous monitoring and innovative, data-driven approaches for effective and sustainable malaria control.
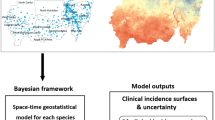
Graphical Abstract

Similar content being viewed by others
Background
Malaria is a life-threatening disease caused by Plasmodium parasites that are transmitted through the bites of infected female Anopheles mosquitoes. Malaria remains a public health challenge and is a major focus of the Sustainable Development Goals (SDGs) [1]. Concerted global efforts resulted in a decrease in malaria incidence and mortality rates by 37% and 60%, respectively, from 2000 to 2015; yet, malaria continues to pose a considerable burden, especially in sub-Saharan Africa [2].
The World Malaria Report 2023, put forth by the World Health Organization (WHO), reported an increase in malaria cases with up to 249 million cases estimated in 85 malaria endemic countries and territories [3]. Notably, over 95% of these cases were attributed to 29 countries, with Nigeria (27%), the Democratic Republic of the Congo (12%), Uganda (5%), and Mozambique (4%) contributing most importantly to the global burden of malaria [3]. Furthermore, the report estimated over 600,000 deaths related to malaria in 2023, with more than 75% of these deaths occurring among children under the age of 5 years [3]. The burden can be attributed to various factors, including limited access to healthcare services, inadequate infrastructure, poverty, political instability, and environmental conditions that favor malaria transmission [4,5,6]. Additionally, challenges such as parasites resistant to antimalarial drugs, mosquitoes resistant to insecticides, and limited resources for prevention, control, and elimination further contribute to the persistence of malaria in this region [7].
In Rwanda, the burden of malaria was particularly severe at the beginning of the new millennium, marking the country one of the most affected in the world. At the time, health facilities across Rwanda reported over 5 million malaria cases. However, from 2005 to 2012, there was a reduction of approximately 86% in malaria incidence and 74% in malaria mortality, indicating substantial progress in controlling the disease. Despite these achievements, the dynamics of malaria transmission in Rwanda continue to evolve, particularly with differences between provinces, influenced by various factors, including demographic changes, climate variability, and public health interventions [8].
Despite the significant strides made in malaria control and elimination in Rwanda, there remains a critical need for ongoing, evidence-based strategic planning and interventions tailored to the evolving dynamics of malaria transmission in districts. This study fills an important gap in the current research by employing an up-to-date spatio-temporal analysis that incorporates detailed demographic and district-specific insights. Unlike previous studies that may have provided broad overviews of malaria incidence, our research specifically identifies which demographic groups and districts are at highest risk, enhancing the precision of public health interventions. By focusing on these key areas, this study not only enhances understanding of the current malaria landscape in Rwanda but also contributes to improving health equity in healthcare service delivery. We pinpoint underserved or high-risk groups and districts, facilitating the development and implementation of cost-effective interventions that are precisely targeted to meet the needs of these vulnerable populations.
The purpose of the current study was to analyse the spatio-temporal dynamics of malaria in Rwanda from 2012 to 2022, placing particular emphasis on demography-specific variations. The study sought to provide a comprehensive picture of the malaria situation in Rwanda, contributing to the national and global efforts in malaria control and elimination. Understanding the demography specific aspects of malaria transmission is crucial for effective disease management, as different population groups such as children, pregnant women, and the elderly exhibit varied susceptibilities to malaria [9]. These demographic distinctions play an important role in the overall dynamics of malaria transmission and its control. The findings from this study are expected to guide resource allocation and implementation of tailored malaria control strategies.
Methods
In this study, a spatio-temporal analysis was conducted to investigate the patterns and dynamics of malaria transmission across Rwanda from January 2012 to December 2022. The analysis focused on identifying spatio-temporal trends and clusters of malaria transmission, providing insights into how these patterns have evolved over the years and contributing to a more nuanced public health strategy in Rwanda.
Study setting
Rwanda is located in East Africa just south of the Equator, occupying an area of 26,338 km2. It is bordered by Uganda in the north, Tanzania in the East, the Democratic Republic of the Congo in the west, and Burundi in the south. The country is a part of the eastern and central African highlands, featuring a varied landscape that ranges from the mountainous Congo-Nile divide and Virunga volcano range in the West and North-Central areas to rolling hills, earning it the nickname “Land of a Thousand Hills” The average elevation across the country varies from 1500 to 2000 m above mean sea level.
Rwanda experiences a temperate, sub-equatorial climate with an average annual temperature of 18.5 °C. The mean annual precipitation is 1250 mm, concentrated in two main rainy seasons (March to May and September to November), interspersed with both a long (June to August) and a short dry season (December to February). An extensive network of rivers, streams, and lakes, surrounded by wetlands, characterizes the landscape of Rwanda.
According to the 2022 census, Rwanda had a population of 13,246,394 individuals, with a high density of 503 people per km2. The country is administratively divided into four provinces and the City of Kigali collectively encompassing 30 districts. The majority (72%) of Rwandans reside in rural areas and nearly half of the urban population lives in the capital city, Kigali. The demographic profile is predominantly young, with 70.3% of the population being under the age of 30 years.
Malaria transmission in Rwanda occurs year-round, peaking typically after the rainy seasons, in May/June and November/December. The entire population is at risk of malaria, though its transmission and intensity vary across regions due to factors like climate variability, altitude, population density, level of urbanisation, and population movement [10]. Malaria control measures in Rwanda include the distribution of long-lasting insecticidal nets (LLINs), indoor residual spraying (IRS), and larval source management (LSM). Environmental and climate factors, along with aspects like irrigation practices and cross-border movement, significantly influence the dynamics of malaria transmission in Rwanda [11].
Data collection
This study utilized data from the Rwanda Health Management Information System (HMIS), which is not publicly available but can be accessed upon reasonable request. The dataset includes aggregated yearly data on malaria cases from 2012 to 2022, collected monthly for each of the 30 districts. through the national routine surveillance system from both community and health care facilities, and it are managed by the Rwanda Biomedical Center. Managed by the Rwanda Biomedical Center, the data are devoid of personal identifiers and categorize malaria cases into three demographic groups: children under the age of 5 years, males above 5 years, and females above 5 years.
Additionally, population data, crucial for calculating expected malaria cases and assessing relative risks (RRs), were obtained from the National Institute of Statistics of Rwanda. This information comes from the fourth (2012) and fifth (2022) Rwanda Population and Housing Census, thematic report on population size, structure, and distribution by district. These population figures were used to estimate the annual population for each district from 2013 to 2021, allowing for the analysis of malaria trends and demographic risks across districts [12, 13].
Statistical analysis
Initially, a descriptive statistics analysis encompassed bar plots for demographic groups; namely, children under the age of 5 years, males above 5 years, and females above 5 years. The bar plots in Fig. 1 provide a visual representation of the absolute number of reported malaria cases within the specified demographic groups from 2012 to 2022. Each bar color represents a different demographic group, illustrating the annual case counts and allowing for a comparative analysis over the years. This visualisation helps to identify trends and disparities in the incidence of malaria cases among these groups.
Subsequently, the analysis incorporated summary statistics, encompassing the median number of cases, standard deviation (SD), minimum and maximum for each demographic group across all districts. This step offered a quantitative insight into the variability and distribution of malaria occurrences.
For the spatio-temporal risk modeling and clusters of malaria in Rwanda, the first step focused on identifying and understanding the clusters of malaria cases across 30 districts of Rwanda, utilising SaTScan™ software version 10.1.2 (Martin Kulldorff, Information Management Services, Inc., Silver Spring, Maryland, USA). The analysis was performed using spatio scan statistics with the discrete Poisson model, a method particularly adept at identifying clusters with either significantly high or low rates of malaria incidence [14]. The discrete Poisson model was chosen to compare the observed number of cases against the expected distribution under the hypothesis of random spatiotemporal occurrence. This approach allowed for the identification of significant deviations from this expectation, thereby pinpointing areas and times of unusually high or low malaria prevalence. The spatially explicit analysis was conducted within defined circular windows, with the maximum spatio cluster size set at 50% of the population at risk. In the study, clusters were identified based on high or low rates. Additionally, the temporal window for the study ranged from a minimum of 1 year to a maximum of 5 years. A key aspect of the analysis was the rigorous statistical validation. There were 999 Monte Carlo replications to ascertain the statistical significance of the identified clusters, adhering strictly to a P-value threshold of 0.05 [15, 16].
In a second step, a spatio-temporal model was applied, using a Bayesian spatially explicit model, aiming to assess the RR of malaria infection across various districts and demographic groups in Rwanda from 2012 to 2022 [17, 18]. RR quantifies the likelihood of malaria occurrence in specific demographics (children under the age of 5 years, males above 5 years, and females above 5 years) across each district, compared to the national average.
In this context, the relative risk \(\:{\theta\:}_{i}\) quantifies whether an area \(\:i\) has higher \(\:\left({\theta\:}_{i}>\:1\right)\) or lower \(\:\left({\theta\:}_{i}<\:1\right)\) risk than the average risk in the whole population [19]. This measure helps identify high-risk zones, facilitating the implementation of targeted public health actions [20]. The observed malaria cases \(\:{Y}_{ij}\:\) for district \(\:i\:\) and year \(\:j\:\) were assumed to follow a Poisson distribution:
where \(\:{E}_{ij}\) represents the expected number of cases based on population data, and \(\:{\theta\:}_{ij}\:\) denotes the RR [21]. The natural logarithm of the RR, \(\:log\:\left({\theta\:}_{ij}\right)\:\) is expressed as a sum of an intercept and spatio-temporal effects, formulated as: \(\:log\:\left({\theta\:}_{ij}\right)\:=\alpha\:+{f}_{BYM}\left(i\right)+{f}_{iid}\left(i,{t}_{j}\right)+{f}_{iid}\left(i,{t}_{j}^{2}\right)+\beta\:\times\:{t}_{j}+\:\delta\:\times\:{t}_{j}^{2}\). In this expression, \(\:\alpha\:\) captures the baseline malaria risk, whilst \(\:\beta\:\) and \(\:\:\delta\:\) represent coefficients of the linear and quadratic terms of the temporal trend, \(\:{t}_{j}\:\)refers to the year index and ranges from 1 to the maximum number of years [18]. \(\:{f}_{BYM}\left(i\right)\:\) represents the Besag-York-Mollié model for spatio structured and unstructured effects for location\(\:\:i\); \(\:{f}_{iid}\left(i,{t}_{j}\right)\) denotes the interaction between location and linear effect of time, assuming independent and identically distributed random effects for location \(\:i\); \(\:{f}_{iid}\left(i,{t}_{j}^{2}\right)\) captures the interaction between location and quadratic effect of time trends for location \(\:\:i\). The spatio structure of the model was established by constructing a neighborhood matrix assuming as neighbors districts that share boundaries, effectively accounting for spatial dependencies [22]. This model’s capacity to handle the heterogeneity and variability in malaria risk due to geographic and temporal factors such as seasonal changes and shifts in public health strategies is enhanced by the integration of both spatial and temporal data. By capturing how malaria risk fluctuates over time in a particular district, the model aids in evaluating the effectiveness of interventions and supports evidence-based policy-making by delivering detailed insights into how risk varies among different demographics, districts, and over time, effectively guiding resource allocation and strategic public health planning [20]. Data segmentation into three demographic groups—children under 5 years of age, males above 5 years, and females above 5 years—was a critical step in the study. Post-model estimation, the estimated mean RRs and their 95% credible intervals were extracted. Inference was conducted using R-INLA methods [18]. Bayesian inference was conducted using integrated nested Laplace approximations (INLA) with the R-INLA package allowing for fast and accurate approximations of posterior distributions. To allow the empiric data to primarily influence the inference, vague priors were selected for our Bayesian analysis. These priors are intentionally non-informative, emphasizing the reliance on observed data to drive posterior distributions [23]. The statistical analyses and visualizations for this study were conducted using R version 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria). Geographic data management and the creation of maps depicting the geographical spread of malaria risk over time were effectively handled using the sf package [24]. The spdep package was instrumental in analyzing spatial dependence and computing statistics that illuminate the spatial dynamics of the data [25]. Furthermore, the ggplot2 package was utilized extensively to generate time plots, enabling a detailed observation of temporal trends in malaria risk from 2012 to 2022 [26,27,28,29].
Results
Descriptive analysis
From 2012 onwards, an increasing trend of malaria cases across all three demographic groups was observed. Cases among males and females older than 5 years peaked in 2016 with 98,645 and 116,627 cases, respectively (Fig. 1). Cases among children under the age of 5 years, kept increasing with an observed peak in 2018 with 84,440 cases.
For children under the age of 5 years, the median number of cases per district varied significantly, with some districts like Ngoma experiencing a median of 37,380 cases, illustrating a higher burden of malaria in these younger populations. The SD for this group indicates variability in case numbers, with districts like Kayonza and Ngoma (Eastern Province) showing a wide dispersion in the data (Table 1). The minimum and maximum for children under the age of 5 years further highlight the disparity between districts, ranging from as low as 23 in Nyabihu (Northern Province) to as high as 84,440 in Ngoma (Eastern Province) suggesting substantial heterogeneity in malaria burden among districts (Table 1).
For males above 5 years of age, the median cases also exhibited substantial variation, with districts like Nyabihu and Musanze (Northern Province) on the lower end, while others such as Kamonyi (Southern Province) and Bugesera (Eastern Province) showed higher medians (Table 1).
Similarly, for females above 5 years of age, the median cases by district revealed heterogeneity, with districts like Burera and Nyabihu on the lower spectrum, while others such as Kamonyi (Southern Province) and Bugesera (Eastern Province) had higher median numbers. The minimum and maximum in this demographic group underscore the heterogeneity in malaria burden across the country, with significant differences between districts’ lowest and highest recorded cases.
Aggregated malaria incidence rates per 1000 individuals for the period 2012–2022 are detailed across various districts, stratified by three demographic groups as shown in Table 2. The district of Ngoma recorded the highest incidence rate among children under the age of 5 years, with 670.5 cases per 1000 children. Conversely, the district of Nyabihu reported the lowest rate in this group, with 2.6 cases per 1000 children. Among males above 5 years of age, the highest incidence rate was observed in Ngoma with 273.7 cases per 1000, while Musanze had the lowest with 12.6 cases per 1000. Similarly, females above 5 years of age in Ngoma experienced the highest incidence rate of 313.9 cases per 1000 individuals, whereas Burera reported the lowest rate at 6.0 cases per 1000.
The spatio scan statistics highlighting the high-risk malaria clusters in Rwanda, stratified by demographic groups between 2012 and 2022 are depicted in Fig. 2. For children under the age of 5, the clusters identified during 2015–2019 include districts such as Bugesera, Gasabo, Gisagara among others, with an observed to expected case ratio of 2.29, indicating that the observed cases were over twice the expected number. This cluster also shows a significant log likelihood ratio of 584,362, strongly suggesting a higher-than-expected malaria incidence, with a P-value of less than 0.001, confirming the statistical significance of these findings. Similarly, for males above 5 years, the period 2014–2018 shows a cluster encompassing additional districts like Karongi and Nyamagabe, with an observed to expected ratio of 2.3 and a log likelihood ratio of 1,146,688, also significant at a P-value of less than 0.001. This indicates a similarly high risk compared to national averages, with significantly more cases observed than expected. The clusters for females above 5 years of age during the same period exhibit an observed to expected ratio of 2.39 and a log likelihood ratio of 1,469,933, with the clustering extending into districts such as Kirehe and Rulindo. The P-value of less than 0.001 for these clusters again supports the presence of a significantly higher incidence of malaria than expected based on the national average. These statistics substantiate the clusters shown in all maps, with districts marked in red indicating a number of observed malaria cases surpassing expected values.
Spatial distribution of high malaria risk clusters in Rwanda from 2012–2022, stratified by demographic groups and their corresponding cluster identification periods. The left map indicates clusters for children under the aged of 5 years during 2015–2019, the middle map denotes clusters for males above 5 years of age during 2014–2018, and the right map illustrates clusters for females above 5 years of age during 2014–2018. Districts coloured in red represent areas where the number of observed malaria cases was higher than expected, signalling a higher risk of reported malaria cases compared to the national average
A comprehensive summary of the spatio scan analysis from 2012 to 2022, depicted in Table 3 reveals malaria clusters across various demographic groups. The analysis indicates that for children under the age of 5 years, between 2015 and 2019, a total of 1,637,971 malaria cases were observed in districts including Bugesera, Gasabo, Gisagara among others. These cases notably surpassed the expected count of 713,780, based on the underlying population of 650,000. The expected number of cases is defined as the number of cases that would be expected based on the underlying population at risk in the absence of any spatial or temporal clustering. The high significance of this cluster is further emphasized by a log likelihood ratio of 584,362 and a P-value of less than 0.001. Similarly, for males aged above 5 years from 2014 to 2018, the observed cases totaled 3,032,237 across several districts, significantly exceeding the expected 1,318,150 cases derived from a population of 2,324,912. This discrepancy is highlighted by a log likelihood ratio of 1,146,688 and a P-value of less than 0.001. Additionally, the cluster for females aged above 5 years during the same timeframe involved 3,611,089 observed malaria cases, far exceeding the expected 1,510,183 cases from a population of 2,435,551. This clustering is confirmed as significant by a log likelihood ratio of 1,469,933 and a P-value of less than 0.001 (Table 3).
Throughout the 2012 to 2022 timeframe, the spatio-temporal analysis of malaria risk among children under the age of 5 years has revealed distinct patterns of elevated RR in certain districts (Fig. 3). Initially, the district of Ngoma was notable with the highest RR in 2014, reaching 3.24 (95% CI: 3.22–3.26). Over the subsequent years, districts such as Gisagara, Huye, Kayonza, and Ruhango were consistently highlighted for their high RRs. Notably, Gisagara district exhibited a significant increase in RR, with a peak at 2.13 (95% CI: 2.12–2.15) in 2013 and surging at 2.64 (95% CI: 2.63–2.65) in 2015. Similarly, Huye district showed an increase in RR to 3.39 (95% CI: 3.38–3.41) in 2015. Ngoma district displayed the most substantial RR during this period, with a peak of 7.00 (95% CI: 6.98–7.03) in 2016 (Fig. 3).
Over the decade-long study from 2012 to 2022, a discernible pattern of malaria risk among males aged above 5 years was observed, with significant variances across different districts. The investigation began with Kirehe district exhibiting a notable RR of 1.86 (95% CI: 1.84–1.87) in 2012 (Fig. 4). In subsequent years, several districts emerged as recurrent hotspots with elevated RR values. Ngoma district, for instance, showed elevated RRs throughout the study period, with a peak RR of 5.70 (95% CI: 5.68–5.72) in 2016. Similarly, Kayonza district displayed consistently high RRs, notably reaching 4.59 (95% CI: 4.57–4.60) in 2016. Ruhango district also demonstrated persistently high RRs, especially in 2017 with a RR of 4.67 (95% CI: 4.65–4.69). Despite a general trend of declining RRs by 2020, the districts of Ngoma, Kayonza, and Ruhango continued to report elevated risks.
In the comprehensive analysis conducted from 2012 to 2022, notable trends in malaria risk among females aged above 5 years were observed, highlighting significant geographic heterogeneity in risk levels across different districts (Fig. 5). The investigation began with districts of Kirehe and Nyagatare which demonstrated elevated RRs of 1.77 (95% CI: 1.76–1.79) and 1.76 (95% CI: 1.75–1.78), respectively, in 2012. However, it was from 2014 onwards that certain districts consistently emerged with particularly high RRs (Fig. 5). In 2014, Kirehe district reported a markedly high RR of 3.45 (95% CI: 3.43–3.46), and Huye district also showed a substantial increase to 3.32 (95% CI: 3.30–3.33). The year 2015 saw Ngoma district reaching the decade peak with a RR of 5.04 (95% CI: 5.02–5.05), with Huye and Kayonza districts following closely, peaking at 4.35 (95% CI: 4.34–4.36) and 3.92 (95% CI: 3.91–3.94), respectively. Ruhango emerged as a district with an elevated malaria risk, peaking at a RR of 4.62 in 2017. Kayonza, Nyanza, and Nyamasheke were also identified as high-risk districts, consistently reporting RRs above 2.5 from 2014 to 2018 (Fig. 5). Toward the end of the study period, there was a general decline in RRs. However, Ruhango and Gisagara districts continued to manifest elevated risks of around 1.10 in 2020.
The time plots delineate the malaria transmission risk across various districts in Rwanda, stratified by demographic groups and annotated for clarity (Fig. 6). Plot A illustrates the trend for children under the age of 5 years, where districts such as Ngoma, Huye, Kayonza, and Ruhango exhibit an ascending and descending trajectory in RR from 2012 to 2022. In contrast, Gisagara and Bugesera districts demonstrate a relatively stable RR (Fig. 6).
Plot B, representing males above 5 years of age, highlights that Ngoma, Ruhango, Kayonza, and Huye districts faced a consistent increase in RR. The peak of the risk was observed in Ngoma district in 2016 (Fig. 6).
In Plot C, focusing on females above 5 years of age, districts such as Ngoma, Kayonza, Nyanza, and Huye are depicted with RRs of 2 and above (Fig. 6). In these plots, colors indicate RR values above 1 for some years in the study period, signifying a higher risk of malaria transmission. In contrast, those areas without color or unhighlighted represent districts with a RR of 1 or below.
Combined time plots illustrating the relative risk (RR) of malaria infection for three demographic groups in districts with RR greater than 1 in Rwanda from 2012 to 2022. A Children under the age of 5 years; B males above 5 years of age; and C females above 5 years of age. Each colored line corresponds to a district that reported a RR greater than the national average during the study period. The color key denotes the specific districts
Interactive web application
An interactive web application has been created using Shiny (https://paulamoraga.shinyapps.io/malariarwandaapp/), The dashboard offers tools such as interactive maps, a database, heat maps, and risk analysis, enabling users to explore malaria data across Rwanda for various demographic groups from 2012 to 2022. It visualizes data like population, cases, and RR, providing insights into spatial and temporal trends to support public health planning and interventions [30].
Discussion
The comprehensive spatio-temporal analysis of malaria risk in Rwanda from 2012 to 2022 provided important insights into the disease dynamics. The study focused on identifying spatial and temporal trends, as well as clusters of cases, unveiling the evolving patterns of malaria over an 11-year period. A significant increase in malaria cases was observed from 2014 to 2018, particularly affecting three demographic groups: children below the age of 5 years, and males and females aged above 5 years, with a peak in 2016. This surge was notably impactful on under 5-year-old children and females aged above 5 years. These observations concur with the 2015 Rwanda DHS report, which indicated an increased malaria prevalence among children under the age of 5 years, reflecting a broader trend of escalating cases [31]. Potential contributing factors to this rise included climatic variations that might favor mosquito breeding, as well as issues with LLINs, such as delayed deliveries and insufficient insecticide content [32]. Additionally, the confirmed resistance of Anopheles gambiae to pyrethroids and a shift in vectors toward outdoor biting, thus reducing the effectiveness of LLINs [32,33,34]. Moreover, lack of access to healthcare might play a role, including limited availability of effective antimalarial medications, insufficient staffing and training for healthcare workers, which might impact the management and containment of malaria and other infectious diseases. Challenges in funding and implementing prevention and control programs exacerbated by socioeconomic factors, including poverty, lack of awareness about malaria prevention, and limited access to education might have contributed. The decline in cases post-2018 might be attributed to the Rwandan government efforts in training community health workers (CHWs), which led to effective home-based malaria treatment [35]. Additionally, community-based environmental management, robust supply chain management for antimalarial drugs, and a referral system from the community settings to health centers played a role in reducing malaria transmission [36]. Furthermore, the introduction and scaling up of more effective LLINs, particularly those treated with a combination of pyrethroids and piperonyl butoxide (PBO), might have significantly impacted malaria control efforts in Rwanda. Indeed, PBO enhances the efficacy of pyrethroids by inhibiting the enzymes that mosquitoes use to detoxify these insecticides, effectively managing resistance and increasing mosquito mortality. This combination has been shown to maintain effectiveness even in areas with high pyrethroid resistance [37]. Improvements in IRS might have contributed to these declines. The strategic use of new classes of insecticides and the rotation among them have helped overcome the challenges posed by insecticide resistance ensuring the continued effectiveness of IRS in reducing mosquito populations and interrupting malaria transmission [38, 39]. Additionally, innovative vector control tools, such as the use of drones for larvicide application, might have had a positive impact in reducing mosquito larvae. Despite the decline in cases post-2018, the emergence of artemisinin resistance in Rwanda calls for rigorous monitoring and adaptation of treatment protocols [10]. The study results further confirm the positive impact of these interventions, providing evidence that supports the effectiveness of the Rwandan government comprehensive approach in fighting malaria.
Spatially explicit analysis highlighted the heterogeneity of malaria burdens across Rwanda [40]. The high burden in districts like Ngoma, contrasted by significantly lower burdens in districts such as Nyabihu, suggests that local factors like ecologic conditions, vector control practices, healthcare access, and socioeconomic status influence malaria transmission [41]. The cluster analysis was critical in understanding the spatial distribution and demographic segmentation of malaria risk, which is essential for tailored public health interventions. For children under the age of 5 years, significant malaria risk clusters in districts such as Bugesera, Gasabo, and Gisagara call for focused intervention strategies. Females aged above 5 years shared overlapping risk areas with younger children, pointing to similar exposure risks in household and community environments [42].
The Bayesian analysis provided a nuanced understanding of the spatio-temporal dynamics and heterogeneity of malaria risk. Elevated RRs in specific districts over the 11-year study period highlighted the evolving nature of malaria transmission, influenced by ecological, occupational, and behavioral factors and land use patterns [43,44,45]. The results indicated periods and districts with heightened malaria transmission, emphasizing the need for tailored malaria control strategies based on local risk profiles and demographic vulnerabilities [46].
This analysis does more than just illuminate demographic disparities; it also uncovers district-specific malaria risk. By targeting high-risk populations and adapting interventions to meet the unique needs of these districts, we enhance public health strategy efficiency and effectiveness. This tailored approach maximizes healthcare resource utilisation and responds precisely to the specific demographic and geographic patterns of malaria transmission. Moreover, such strategic alignment addresses the fundamental causes of health inequities, underscoring the importance of improving health equity through focused interventions. Ultimately, this strategy leads to more effective malaria management and reduces disparities across different demographic groups.
This study has important ramifications for Rwanda’s national malaria control program. The findings advocate for a dynamic, adaptive approach to malaria control, integrating socioeconomic, ecological, and behavioural factors. Enhanced surveillance and spatial targeting of interventions, particularly in regions with persistently high RRs, are crucial. Understanding risk profiles across different districts and demographic groups allows for more effective resource allocation and tailored interventions, including the distribution of LLINs, IRS, and community education programs. Additionally, the study highlights the necessity of adaptive management and district-specific strategies, informed by local transmission patterns and demographic vulnerabilities.
The strength of this study lies in its comprehensive approach, utilising advanced statistical methods such as Bayesian spatially explicit models and spatio scan statistics to analyze an 11-year dataset, providing a detailed understanding of the spatio-temporal dynamics of malaria transmission across different demographic groups.
However, the study’s focus on spatio-temporal dynamics does not address the underlying causal pathways. For instance, it has been suggested that climate change might have a broad impact on vector ecology and malaria transmission. In addition, the behavioral aspects of the human population and mosquito vectors, such as changes in human movement patterns or mosquito biting behavior, were not extensively explored. Future research should focus on the long-term sustainability and effectiveness of control measures in the face of changing environmental and demographic conditions and delve deeper into socioeconomic factors influencing malaria prevalence and control effectiveness.
Conclusions
The current study’s spatio-temporal analysis of malaria in Rwanda from 2012 to 2022 provides new insights into the evolving patterns of malaria transmission, underlining not only the surge in malaria cases from 2014 to 2018, but also the potential underlying factors contributing to these trends. Our findings reveal significant demographic vulnerabilities, particularly among females above 5 years of age and under 5-year-old children, stressing the need for targeted interventions in these groups. The observed increase in malaria cases during this 11-year period can be attributed to a combination of climatic variations, ineffective use of LLINs, resistance of Anopheles gambiae mosquitoes to pyrethroids, and changes in mosquito behavior favoring outdoor biting. Importantly, the study has identified distinct malaria ecozones in Rwanda, suggesting that a one-size-fits-all approach to malaria control is not be feasible. Instead, district-specific strategies considering local ecological, biological, and socio-economic conditions are essential. The decline in malaria cases post-2018, most likely attributed to government-led initiatives such as training CHWs, underscores the potential of localised strategies. Furthermore, the new challenge of artemisinin resistance calls for a robust surveillance system to monitor drug efficacy and vector resistance patterns continually. The persistent high transmission rates in some districts call for a refined focus within the national malaria control program, to address these micro-epidemiological variances effectively.
Availability of data and materials
All data generated or analyzed during this study are included within the manuscript. Additionally, an interactive web application for further exploration and visualization of the data is available at https://paulamoraga.shinyapps.io/malariarwandaapp/.
Abbreviations
- HMIS:
-
Health management information system
- IRS:
-
Indoor residual spraying
- LLINs:
-
Long-lasting insecticidal nets
- LSM:
-
Larval source management
- RR:
-
Relative risk
- SDGs:
-
Sustainable development goals
- WHO:
-
World Health Organization
References
Sarpong E, Acheampong DO, Fordjour GNR, Anyanful A, Aninagyei E, Tuoyire DA, et al. Zero malaria: a mirage or reality for populations of sub-saharan Africa in health transition. Malar J. 2022;21:314.
Okunlola OA, Oyeyemi OT. Spatio-temporal analysis of association between incidence of malaria and environmental predictors of malaria transmission in Nigeria. Sci Rep. 2019;9(1):17500.
WHO. World malaria report 2023. Geneva: World Health Organization; 2023.
Patz JA, Patz SS. Malaria risk and temperature: influences from global climate change and local land use practices. Proc Natl Acad Sci USA. 2006. https://doi.org/10.1073/pnas.0601493103.
Keiser J, Maltese M, Bos R, Tanner M, Singer B, Utzinger J. Effect of irrigation and large dams on the burden of malaria on a global and regional scale. Am J Trop Med Hyg. 2005;72:392–406.
Stern DI, Gething PW, Kabaria CW, Temperley WH, Noor AM, Okiro EA, et al. Temperature and malaria trends in Highland East Africa. PLoS ONE. 2011;6(9):e24524.
Suh PF, Elanga-Ndille E, Tchouakui M, Sandeu MM, Tagne D, Wondji C, et al. Impact of insecticide resistance on malaria vector competence: a literature review. Malar J. 2023;22(1):19.
Kubana E, Munyaneza A, Sande S, Nduhuye F, Karangwa JB, Mwesigye D, et al. A comparative analysis of risk factors of malaria, case study Gisagara and Bugesera District of Rwanda. RDHS 2014/2015. A retrospective study. BMC Public Health. 2023;23:168.
Kohara Melchior LA, Chiaravalloti Neto F. Spatial and spatio-temporal analysis of malaria in the state of Acre, western Amazon, Brazil. Geospat Health. 2016;11:443.
Rwanda Biomedical Center. Rwanda Malaria Programme Mid Term Review. Rwanda: Kigali; 2023.
Nzabakiriraho JD, Gayawan E. Geostatistical modeling of malaria prevalence among under-five children in Rwanda. BMC Public Health. 2021;21:369.
National Institute of Statistics of Rwanda (NISR). Fifth Rwanda Population and Housing Census, Thematic Report: Population size, structure, and spatial distribution. Report. Kigali,Rwanda; 2023.
National Institute of Statistics of Rwanda (NISR). Rwanda Fourth Population and Housing Census. Thematic report: Population size, structure and distribution. Report. Rwanda: National Institute of Statistics of Rwanda (NISR),Ministry of Finance and Economic Planning (MINECOFIN); 2012.
Coleman M, Coleman M, Mabuza AM, Kok G, Coetzee M, Durrheim DN. Using the SaTScan method to detect local malaria clusters for guiding malaria control programmes. Malar J. 2009;8:68.
Colborn KL, Giorgi E, Monaghan AJ, Gudo E, Candrinho B, Marrufo TJ, et al. Spatio-temporal modelling of weekly malaria incidence in children under 5 for early epidemic detection in Mozambique. Sci Rep. 2018;8:9238.
Moraga P. Spatial statistics for data science: theory and practice with. Boca Raton: Chapman & Hall/CRC Data Science Series; 2023.
Adegboye O, Gayawan E, James A, Adegboye A, Elfaki F. Bayesian spatial modelling of Ebola outbreaks in Democratic Republic of Congo through the INLA-SPDE approach. Zoonoses Public Health. 2021;68:443–51.
Moraga P. Geospatial Health data: modeling and visualization with R-INLA and Shiny. Boca Raton: Chapman & Hall/CRC Biostatistics Series; 2019.
McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157(10):940–3.
Librero J, Ibanez B, Martinez-Lizaga N, Peiro S, Bernal-Delgado E, Spanish Atlas of Medical Practice Variation Research G. Applying spatio-temporal models to assess variations across health care areas and regions: lessons from the decentralized Spanish National Health System. PLoS ONE. 2017;12(2):e0170480.
Moraga P. Small area disease risk estimation and visualization using R. R J. 2018;10(1):495–506.
Lawson AB, Rotejanaprasert C, Moraga P, Choi J. A shared neighbor conditional autoregressive model for small area spatial data. Environmetrics. 2015;26(6):383–92.
Håvard Rue SM, Chopin N. Approximate bayesian inference for latent gaussian models by using integrated nested Laplace approximations. J Royal StatSociety. 2009;71:319.
Pebesma E. Simple features for R: standardized support for spatial vector data. R J. 2018;10(1):439–46.
Roger S, Bivand EP, Gómez-Rubio V. Applied spatial data analysis with R. 2nd ed. New York: Springer-Verlag; 2013.
Giorgi E, Diggle PJ, Snow RW, Noor AM. Geostatistical methods for disease mapping and visualisation using data from spatio-temporally referenced prevalence surveys. Int Stat Rev. 2018;86(3):571–97.
Wickham H. ggplot2: elegant graphics for data analysis. New York: Springer-Verlag; 2016.
Elena N, Ieno AFZ. A beginner’s guide to data exploration and visualisation with R. Newburgh: Highland Statistics Ltd; 2015.
Wikle CK, Zammit-Mangion A, Cressie N. Spatio-temporal statistics with. R. Boca Raton: Chapman & Hall/CRC; 2019.
Moraga P, SpatialEpiApp. A Shiny web application for the analysis of spatial and spatio-temporal disease data. Spat Spatiotemporal Epidemiol. 2017;23:47–57.
Bizimana JP, Nduwayezu G. Spatio-temporal patterns of malaria incidence in Rwanda. Trans GIS. 2020;25:751–67.
Karema C, Wen S, Sidibe A, Smith JL, Gosling R, Hakizimana E, et al. History of malaria control in Rwanda: implications for future elimination in Rwanda and other malaria-endemic countries. Malar J. 2020;19(1):356.
Hakizimana E, Karema C, Munyakanage D, Iranzi G, Githure J, Tongren J. Monitoring long-lasting insecticidal net (LLIN) durability to validate net serviceable life assumptions, in Rwanda. Malar J. 2014. https://doi.org/10.1186/1475-2875-13-344.
Hakizimana E, Karema C, Munyakanage D, Iranzi G, Githure J, Tongren JE, et al. Susceptibility of Anopheles gambiae to insecticides used for malaria vector control in Rwanda. Malar J. 2016;15:582.
Rwanda Biomedical Center. Malaria Matchbox Assessment in Rwanda. Kigali,Rwanda; 2021.
WHO. World Malaria Report 2022. Geneva: World Health Organization. Report. Geneva;; 2022.
Kabera M, Mangala JN, Soebiyanto R, Mukarugwiro B, Munguti K, Mbituyumuremyi A, et al. Impact of pyrethroid plus piperonyl butoxide synergist-treated nets on malaria incidence 24 months after a National Distribution Campaign in Rwanda. Am J Trop Med Hyg. 2023;109(6):1356–62.
Govoetchan R, Fongnikin A, Syme T, Small G, Gbegbo M, Todjinou D, et al. VECTRON T500, a new broflanilide insecticide for indoor residual spraying, provides prolonged control of pyrethroid-resistant malaria vectors. Malar J. 2022;21(1):324.
Ngufor C, Fongnikin A, Hobbs N, Gbegbo M, Kiki L, Odjo A, et al. Indoor spraying with chlorfenapyr (a pyrrole insecticide) provides residual control of pyrethroid-resistant malaria vectors in southern Benin. Malar J. 2020;19(1):249.
Hakizimana E, Karema C, Munyakanage D, Githure J, Mazarati JB, Tongren JE, et al. Spatio-temporal distribution of mosquitoes and risk of malaria infection in Rwanda. Acta Trop. 2018;182:149–57.
Ingabire CM, Kateera F, Hakizimana E, Rulisa A, Muvunyi C, Mens P, et al. Determinants of prompt and adequate care among presumed malaria cases in a community in eastern Rwanda: a cross sectional study. Malar J. 2016;15:227.
Ostovar ARA, Raeisi A, Majdzadeh R. Time series analysis of meteorological factors influencing malaria in Iran. J Arthropod Borne Dis. 2016;10:222.
Asingizwe D, Poortvliet PM, Koenraadt CJM, van Vliet AJH, Ingabire CM, Mutesa L, et al. Role of individual perceptions in the consistent use of malaria preventive measures: mixed methods evidence from rural Rwanda. Malar J. 2019;18:270.
Aubourg MA, Al-Amin HM, Sunkara A, Chetan S, Monroe A, Phru CS, et al. Human behaviour directs household-level exposure to malaria vectors in Bandarban, Bangladesh. Malar J. 2022;21(1):355.
Paul P, Kangalawe RYM, Mboera LEG. Land-use patterns and their implication on malaria transmission in Kilosa District, Tanzania. Trop Dis Travel Med Vaccines. 2018;4:6.
Yankson R, Anto EA, Chipeta MG. Geostatistical analysis and mapping of malaria risk in children under 5 using point-referenced prevalence data in Ghana. Malar J. 2019;18:67.
Acknowledgements
We extend our deepest gratitude to the Rwanda Biomedical Center for their generous and invaluable support in providing essential malaria secondary data. This contribution was crucial not only for the successful completion of this study but also for enabling a deeper understanding of the impact and dynamics of malaria in Rwanda. Their collaboration has significantly enriched our research and findings.
Funding
Open access funding provided by University of Basel. This research was supported by the Letten Prize, which awarded a personal prize to Paula Moraga. Rubuga F. Kitema received a PhD scholarship from the canton of Basel-Stadt. We extend our thanks to both for their essential support.
Author information
Authors and Affiliations
Contributions
The methodology and formal analysis were developed and performed by F.K.R. and P.M. The original draft was written by F.K.R The manuscript underwent review and editing by P.M., A.A., E.S., E.R., G.M., G.C, J.U.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rubuga, F.K., Moraga, P., Ahmed, A. et al. Spatio-temporal dynamics of malaria in Rwanda between 2012 and 2022: a demography-specific analysis. Infect Dis Poverty 13, 67 (2024). https://doi.org/10.1186/s40249-024-01237-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40249-024-01237-w