Abstract
Background
Current soil-transmitted helminth (STH) control guidelines endorse the use of albendazole or mebendazole for school-based targeted preventive chemotherapy (PC), yet their reduced efficacy against Strongyloides stercoralis and Trichuris trichiura presents significant limitations. Emerging evidence indicates that community-wide PC [or mass drug administration (MDA)] using ivermectin, commonly used in other neglected tropical disease (NTD) control programs, may play an important role in controlling these parasites. We conducted a systematic review and meta-analysis to evaluate the effectiveness of ivermectin PC in reducing STH prevalence in endemic populations.
Methods
We searched Pubmed, EMBASE, and Web of Science on February 14, 2023, for studies that investigated the effectiveness of ivermectin PC, either alone or in combination with other anthelmintic drugs, on STH infections, and provided a measure of STH prevalence before and after PC. We calculated pooled prevalence reductions for each STH using random-effects meta-analyses. Our protocol is available on PROSPERO (registration number CRD42023401219).
Results
A total of 21 were eligible for the systematic review, of which 15 were eligible for meta-analysis. All studies delivered ivermectin through MDA. The pooled prevalence reduction of S. stercoralis following MDA with ivermectin alone was 84.49% (95% CI 54.96–94.66) across five studies and 81.37% (95% CI 61.62–90.96) across seven studies with or without albendazole. The prevalence reduction of T. trichiura was 49.93% (95% CI 18.23–69.34) across five studies with ivermectin alone, and 89.40% (95% CI 73.66–95.73) across three studies with the addition of albendazole. There was high heterogeneity for all syntheses (I2 > 65%).
Conclusions
This study underscores the key role of ivermectin-based MDA in addressing limitations in current global STH guidelines in terms of limited efficacy against S. stercoralis and T. trichiura. Based on these findings, revising international STH guidelines to include ivermectin is a promising option to progress the control and eventual elimination of STHs and other NTDs.
Similar content being viewed by others
Background
Soil-transmitted helminth (STH) infections are the most prevalent neglected tropical disease (NTD) worldwide, infecting an estimated 895 million people [1] and contributing 1.9 million disability-adjusted life years (DALYs) per annum [2]. STH infections are caused by a group of intestinal nematodes including Ascaris lumbricoides, Trichuris trichiura, hookworms (Necator americanus, Ancylostoma ceylanicum, Ancylostoma duodenale) and Strongyloides stercoralis. Of note, S. stercoralis is estimated to infect 600 million people annually [3], and is characterised by its unique auto-infective lifecycle capable of causing chronic and potentially fatal hyperinfection among immunosuppressed patients [4]. T. trichiura also contributes significantly to the global burden with an estimated 290 million annual infections, and is associated with a range of adverse health outcomes in the case of chronic and heavy intensity infections, including developmental delay, anaemia, gastrointestinal disease, and Trichuris dysentery syndrome [1].
The mainstay of public health control efforts against STH infections is school-based targeted preventive chemotherapy (PC). PC refers to the large-scale distribution of safe and efficacious drugs to specific risk groups (targeted PC) or to entire communities [mass drug administration (MDA)]. For STHs, the WHO recommended strategy is school based targeted PC, delivering benzimidazole anthelmintics, mebendazole or albendazole, to school-aged children [5]. While other risk groups have been identified, namely women of reproductive age and adults in high-risk occupations like miners, there are no defined distribution channels to target them. Furthermore, although these drugs are efficacious against A. lumbricoides and hookworm [6], they have no efficacy against S. stercoralis [7] and limited efficacy against T. trichiura [6]. Concerns have also been raised regarding the potential generation of anthelmintic resistance among humans [8], a phenomenon well documented in livestock [9]. Investigation into alternative therapeutic regimens for STH control is therefore a key priority.
Ivermectin is a broad-spectrum antiparasitic drug that has high efficacy against S. stercoralis and A. lumbricoides, moderate efficacy against T. trichiura, and poor efficacy against hookworms [6, 10,11,12,13]. While ivermectin alone has not been used in school-based targeted PC programs for STH, it has been used over the last two decades in highly effective community-wide MDA campaigns against onchocerciasis [14] and more recently against scabies [15, 16]. These programs demonstrated, to varying degrees, reductions in the prevalence and intensity of off-target STHs [17,18,19], providing preliminary evidence that ivermectin MDA may be a cost-effective strategy for the simultaneous control of multiple NTDs, including STH infections. While the combination of albendazole and ivermectin has significant therapeutic efficacy against all STH species [6, 7], their effectiveness at the population level in MDA programs has also been variable [20,21,22,23,24,25].
Addressing these gaps in knowledge will provide an important evidence base to inform policy decision-making and optimise the implementation of PC programs to progress STH control and elimination targets. This systematic review and meta-analysis aimed to evaluate the role of ivermectin-based PC in improving the control of STHs by describing the existing literature that documents the impact of ivermectin PC in endemic populations, and to quantify its effectiveness, both as a standalone regimen and in combination with albendazole, in reducing STH prevalence.
Methods
Search strategy and selection criteria
This systematic review and meta-analysis was completed in accordance with the 2020 PRSIMA guidelines [26]. Papers were eligible for inclusion if they investigated the effectiveness of ivermectin PC (including both targeted PC and MDA), either alone or in combination with other anthelmintic drugs, on STH infections, and provided a measure of STH prevalence before and after PC.
Papers were excluded from the systematic review if PC was given only to positive cases or given only to a random sample of the population; if outcomes were only reported for positive cases; if PC was delivered in the context of randomised trials where randomisation occurred at individual level; or if data published were duplicate data from another paper.
Additional exclusion criteria were applied for the quantitative synthesis (meta-analysis) to remove significant sources of heterogeneity. Studies were excluded from the meta-analysis if they met any of the following three exclusion criteria: (1) time from the last round of ivermectin PC to the follow-up prevalence assessment was less than 1 month or greater than 24 months as studies with < 1 month follow-up periods will likely be measuring PC efficacy (intervention outcomes under ideal settings) rather than effectiveness (intervention outcomes under real-world settings), therefore overestimating the real-world impact of PC, while those with > 24 months follow-up will likely underestimate the effectiveness of PC; (2) if the time from the baseline assessment to the first round of PC was greater than 12 months; or (3) if the baseline prevalence was less than 5%.
We searched Pubmed, EMBASE, and Web of Science on February 14, 2023 with no limitations on year or language of publication. The following search terms were used for each of the three key concepts: (1) ivermectin: “ivermectin”; (2) PC: “preventive chemotherapy” or “chemotherapy” or “mass drug administration” or “mass administration” or “mass treatment” or “population” or “community” or “communities” or “village” or “villages” or “school” or “schools” or “prevalence” or “program” or “programme”; (3) soil-transmitted helminth infections: “soil-transmitted helminth” or “soil-transmitted helminths” or “STH” or “nematode” or “geohelminth” or “Ascaris” or “hookworm” or “Necator” or “Ancylostoma” or “Trichuris” or “Strongyloides”. The complete search strategy, including medical subject heading terms used, are provided in Additional file 1 (p. 1). We identified additional studies by manually searching reference lists of included papers and key systematic reviews [27, 28], and through personal knowledge.
All papers retrieved from databases were imported into EndNote version X9 (Clarivate, Philadelphia, USA) where they were first deduplicated. All paper titles, abstracts, and full-text papers were then screened by BL. For quality control, 20% of the papers subjected to full text screening were randomly selected and independently reviewed by NL to determine discrepancies in inclusion or exclusion. All papers were assessed for eligibility against the review protocol, available in PROSPERO (registration number CRD42023401219).
Data extraction and quality assessment
Data were extracted by BL using Covidence [29]. Where available, the following data were extracted from eligible papers: year and country of study; study population; drug(s) used; diagnostic technique; study design; primary disease target of PC; strategy of drug administration (mass or targeted); drug dosage and frequency; number of rounds of drug distribution; intervention coverage; additional interventions employed for STH control; prevalence of infection for each species before and after PC (including number of participants receiving treatment, number of participants infected, and proportion infected); time between baseline and each of the follow-up prevalence assessments; and follow-up time from last round (time between the last round of PC and follow-up prevalence assessments). For quality control, 20% of the papers subjected to data extraction were randomly selected and independently reviewed by NL, where any discrepancies were resolved through discussion. In the case of disagreements, it was escalated to NEC who made the final decision.
If a paper reported data for multiple arms, we extracted data from all arms separately provided they represented independent populations, herein referred to as “studies”. If a range of intervention coverage was reported, we extracted the median. In trials with a control group that was provided PC only and an intervention group that received an additional intervention [e.g., water, sanitation, and hygiene (WASH) improvements], only data from the control groups were extracted. Where multiple follow-up prevalence assessments were reported, we extracted data for all assessments.
We contacted five authors for additional data requesting a full manuscript or published paper for conference abstracts (n = 3) and intervention coverage data (n = 2). Three authors responded, of which one was unable to share a manuscript documenting the results of a conference abstract and two were unable to share coverage data.
Study quality was assessed using an approach from a previously published systematic review [27] that used a modified scale adapted from a validated scale [30] designed to assess risk of bias in prevalence studies. Modifications were made to account for most studies being quasi-experimental, pre-post prevalence surveys without a control group. We used quality assessment tools from the National Heart, Lung, and Blood Institute for observational and pre-post study designs [31, 32], and made modifications to ensure consistent participant selection and intervention coverage [27]. We evaluated studies based on nine safeguards to eliminate bias in measuring STH prevalence, including items that evaluated internal and external validity. Quality assessment was performed by BL and independently reviewed by NEC, with disagreements resolved through consensus.
Statistical analysis
All analyses were completed separately for each STH species and for each PC regimen. In the primary analysis, we conducted a random-effects weighted meta-analysis evaluating the effectiveness of PC against each STH species. The first timepoint at which prevalence data were available was considered the baseline (p1). For the purpose of the meta-analysis, we used one follow-up prevalence estimate (p2) per study, defined as the prevalence assessment that followed the last round of PC involving ivermectin. Although the primary outcome in the model was the pooled prevalence ratio (p2/p1), we converted and reported these results as pooled prevalence reduction [(1 − pooled prevalence ratio) × 100] for ease of interpretation. We report the pooled prevalence reduction for ivermectin PC as a monotherapy regimen and, separately, ivermectin and albendazole PC for A. lumbricoides, T. trichiura, and hookworm. Given that a single dose of albendazole is unlikely to have significant therapeutic activity against S. stercoralis [10], we pooled all studies using ivermectin for this species. Where sufficient data were available (n > 2 studies), we conducted sensitivity analyses based on the following restrictions: (1) follow-up time from last round (> 6 months; > 6 months and ≤ 18 months); (2) number of PC rounds administered (one round vs. multiple rounds); (3) diagnostic technique (stool-based methods for S. stercoralis; Kato-Katz for A. lumbricoides, T. trichiura, and hookworm); (4) PC coverage (< 75% vs ≥ 75% as recommended by the WHO for STH control); and (5) studies using ivermectin alone for S. stercoralis. Heterogeneity was assessed using Cochran’s Q test and Higgins’ I2 where an I2 of greater than 50% was considered to indicate significant heterogeneity. Publication bias and evidence of small-study effects were assessed through visual inspection of Doi plots and the Luis Furuya-Kanamori (LFK) index, which have greater sensitivity and power than the funnel plot and Egger’s regression method when there are fewer studies [33]. Visual asymmetry on the Doi plot refers to an imbalanced distribution of effect sizes, indicating potential publication bias where small or non-significant effect sizes may be missing from the analysis. An LFK index of ± 1 indicates no asymmetry on the Doi plot, between ± 1 and ± 2 indicates minor symmetry, and ± 2 indicates major asymmetry [33].
In the secondary analysis we used random-effects weighted meta-regressions to quantify the effect of select covariates on PC effectiveness. This was due to the presence of heterogeneity across studies on variables likely to affect PC effectiveness, including baseline prevalence, number of rounds of PC, and follow-up time from last round. For the purposes of the meta-regression, we used data from all follow-up prevalence assessments if a study had multiple assessments, where prevalence reduction was defined as the relative difference between each follow-up assessment (p2, or p3, or p4 …) and the first timepoint at which data were available (p1), yielding multiple reduction estimates for these studies [(1 − p2/p1) × 100) and; (1 − p3/p1) × 100) and; (1 − p4/p1) × 100) …]. The outcome variable in the model was relative prevalence reduction, where it was winsorised at its lower boundary so that any prevalence increase was reset to zero, allowing the winsorised distribution to mirror that of a proportion and to be analysed with a logit link function [27]. This approach was considered appropriate as any increase in prevalence would be unrelated to PC, suggesting no effectiveness. We entered the following covariates in the model: (1) baseline prevalence (%), (2) number of rounds of PC between baseline and follow-up prevalence assessments, and (3) time from last round of PC to follow-up prevalence assessments (months). We obtained the weighted odds ratio by exponentiating the coefficients, and report this estimate with the associated 95% confidence intervals (CIs).
All meta-regression models were fitted with robust clustered standard errors to account for clustering at the study level and heteroscedasticity. We only had sufficient data to analyse the impact of these covariates on the effectiveness of ivermectin PC, with or without albendazole, against S. stercoralis, and ivermectin and albendazole against A. lumbricoides, T. trichiura, and hookworm. Meta-analyses were completed using MetaXL (version 5.3) and meta-regressions were completed using Stata (version 17.0).
Results
Systematic review
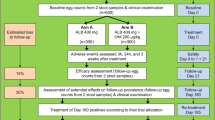
A total of 21 papers (reporting 25 studies) met the inclusion criteria for the systematic review [17,18,19,20,21,22,23,24,25, 34,35,36,37,38,39,40,41,42,43,44,45] and 15 of these papers (reporting 19 studies) were included in the meta-analysis [17,18,19,20,21,22, 24, 25, 35, 36, 39, 41,42,43, 45] (Fig. 1). Papers excluded at the full-text screening stage are provided in Additional file 1 (p. 2–4).
Table 1 lists individual studies included in the systematic review with their characteristics while Table 2 provides an aggregated summary of the study characteristics. Of the 25 studies included in the systematic review, 17 (68%) used ivermectin and albendazole as their PC regimen [20,21,22,23,24,25, 34, 36, 38,39,40,41, 43, 45] and 8 (32%) used ivermectin with no other anthelminthic drugs [17,18,19, 35, 37, 42, 44]. Nine studies used additional drugs in addition to ivermectin and/or albendazole [19, 34, 36, 38,39,40,41, 44]. There was no head-to-head comparison of ivermectin versus ivermectin and albendazole. Ivermectin was distributed to entire through community-wide MDA for all studies [17,18,19,20,21,22,23,24,25, 34,35,36,37,38,39,40,41,42,43,44,45]. Onchocerciasis (n = 3) (17, 34, 37) and scabies (n = 3) (18, 39, 43) were the primary diseases targeted for studies using ivermectin only. In studies using ivermectin and albendazole combined, albendazole was mostly distributed to entire communities through MDA together with ivermectin (n = 13) [21,22,23,24,25, 36, 39, 41, 43, 45], although four studies complemented MDA efforts with school-based targeted PC [20, 34, 38, 40] with albendazole only on alternating timelines. Lymphatic filariasis was the most commonly targeted primary disease, representing 64% of these studies (n = 16) (19, 21, 22, 33, 35, 36, 38, 40–42, 44, 46). Ivermectin dosages were within standard range (one dose, 150–200 μg/kg) for most studies (n = 18, 72%) where dosage was reported [17,18,19,20,21,22, 24, 25, 34,35,36,37, 40,41,42,43,44]. Two studies administered two doses given 7 to 14 days apart for scabies [17, 42] while one study [44] used a higher dosage (400 μg/kg) for lymphatic filariasis.
The number of rounds of MDA administered between baseline and last prevalence assessment ranged between 1 and 23 rounds, with 10 (40%) studies administering only 1 round [17, 19, 22,23,24, 41, 42, 44, 45]. The follow-up time from last round ranged between 1 week and 36 months, with 16 (64%) studies being 12 months or less [17,18,19,20, 22, 23, 25, 35, 37,38,39,40, 43, 44], 8 (32%) being between > 12 and ≤ 24 months [21, 24, 36, 41, 42, 45], and 1 (4%) being greater than 24 months [34]. Of the 17 studies that assessed ivermectin and albendazole, there were between 1 and 16 rounds administered, with a median of 3 rounds. Follow-up time ranged between 5 and 36 months, with a median of 12 months. Of the 8 studies that assessed ivermectin, there were between 1 and 23 rounds administered, with a median of 1 round. Follow-up time ranged between 1 week and 21 months, with a median of 10.5 months. There was considerable variability in MDA coverage. Of the 21 (84%) studies that reported coverage [17,18,19,20,21,22,23, 25, 34,35,36,37,38, 41,42,43, 45], the range was between 27 and 93%, with 13 studies [17,18,19,20, 22, 34, 35, 37, 38, 41, 42, 45] achieving ≥ 75% coverage as recommended by the WHO for STH control. For studies assessing ivermectin and albendazole, coverage ranged between 27 and 82%, with a median of 73%, while the coverage for ivermectin alone studies ranged between 81 and 91%, with a median of 88%. Additional information about the studies included in the review, including locations, surveyed populations, diagnostic methods, and primary disease targets are summarised in Table 1 (for individual studies) and 2 (aggregated summary).
Risk of bias
Results of the risk of bias assessment is summarised in Additional file 1 (p. 5). Notably, of the 15 papers included in the meta-analysis, there were 13 (87%) that had response (or participation) rates of < 75% or showed a difference in relevant demographic characteristics between responders (participants) and non-responders (non-participants) (or not reported). Additionally, there were 6 (40%) papers where the drug distribution strategy was not clearly described and/or not delivered to at least 75% of the target population (or not reported). There was no indication of major risk of bias among the remaining 7 items.
Meta-analysis
Meta-analysis results are presented in Fig. 2 (for S. stercoralis and T. trichiura) and 3 (for hookworm and A. lumbricoides). The pooled prevalence reduction of S. stercoralis following MDA with ivermectin alone was 84.49% (95% CI 54.96–94.66) across five studies (Fig. 2a), and 81.37% (95% CI 61.62–90.96) across seven studies with or without albendazole (Fig. 2b). The pooled prevalence reduction for T. trichiura was 49.93% (95% CI 18.23–69.34) across five studies with ivermectin (Fig. 2c), and 89.40% (95% CI 73.66–95.73) across three studies with ivermectin and albendazole (Fig. 2d). We did not observe a significant reduction in hookworm prevalence with ivermectin alone [Fig. 3a, prevalence reduction 23.38% (95% CI − 5.63–44.42) across four studies], but the pooled prevalence reduction was 78.99% (95% CI 67.57–86.39) when using ivermectin and albendazole across 13 studies (Fig. 3b). Although we observed an A. lumbricoides prevalence reduction of 35.30% (95% CI 4.07–56.36) across three studies with ivermectin alone (Fig. 3c), we did not detect a statistically significant reduction associated with ivermectin and albendazole MDA across five studies [Fig. 3d, prevalence reduction − 13.08% (95% CI − 56.88–18.49)].
Forest plot of prevalence reduction for studies assessing the effectiveness of a ivermectin alone against Strongyloides stercoralis, b ivermectin, with or without albendazole, against S. stercoralis, c ivermectin alone against Trichuris trichiura, and d ivermectin and albendazole against T. trichiura
Results of the sensitivity analyses are in Additional file 1 (p. 8). Of note, the pooled prevalence reduction was sensitive to variations in the number of MDA rounds and coverage for hookworm. A single round of MDA resulted in a hookworm prevalence reduction of 47.14% (95% CI 0.95–71.79) across four studies, compared to 85.70% (95% CI 73.35–91.70) across nine studies where multiple rounds were administered. Reduced MDA coverage (< 75%) was associated with a hookworm prevalence reduction of 88.95% (95% CI 79.07–94.16) across 7 studies, compared with 48.80% (95% CI 19.73–67.34) associated with higher coverage (≥ 75%) across 4 studies. We did not observe variations in pooled prevalence reduction for the remaining sensitivity analyses or there was insufficient data (Additional file 1, p. 8).
There was high heterogeneity among all syntheses. For studies assessing ivermectin alone, I2 was 78% for S. stercoralis, 89% for T. trichiura; 94% for hookworm; 86% for A. lumbricoides, with a similar pattern when albendazole was considered (Figs. 2 and 3).
Results of Doi plots and LFK indices showed evidence of major asymmetry for studies assessing ivermectin alone for S. stercoralis (LFK index -7.35) and hookworm (LFK index − 3.71), but less for A. lumbricoides (LFK index − 1.24) and T. trichiura (LFK index − 0.36) (Additional file 1, p. 7). For studies assessing ivermectin and albendazole, there was major asymmetry for S. stercoralis (LFK index − 4.33), hookworm (LFK index − 3.21), and T. trichiura (LFK index − 2.58), with no evidence of asymmetry for A. lumbricoides (LFK index − 0.78) (Additional file 1, p. 6).
Meta-regression
As shown in Table 3, for each 1% increase in baseline prevalence, there was significantly reduced odds of prevalence reduction for T. trichiura (OR = 0.95, 95% CI 0.90–0.99, P = 0.041) and A. lumbricoides (OR = 0.82, 95% CI 0.70–0.96, P = 0.027). For each increase in the number of MDA rounds, there was an 82% increase in the odds of prevalence reduction for hookworm (OR = 1.82, 95% CI 1.21–1.73, P = 0.008).
Discussion
For the past three decades, WHO guidelines for STH control have endorsed specific therapeutic regimens that have been widely implemented in school-based targeted PC programs. However, these drugs have inadequate efficacy against S. stercoralis and T. trichiura and school-based targeted PC does not address adult reservoir of infections [46, 47]. This systematic review and meta-analysis is the first synthesis of existing evidence on the effectiveness of ivermectin PC, both as a standalone regimen and in combination with albendazole, in reducing STH prevalence in children and adults.
We observed a substantial reduction in S. stercoralis prevalence following ivermectin MDA. This is consistent with findings from a recent meta-analysis [28] and adds to the growing body of evidence supporting the inclusion of ivermectin in control guidelines for S. stercoralis. While the WHO has begun addressing gaps in current guidelines, a comprehensive strategy for S. stercoralis control is still under development. Our study highlights three important gaps in understanding that will need to be addressed to inform WHO recommendations. First, all studies delivered ivermectin through community-wide MDA, with impact observed in both children and adults, whereas current STH control is based on school-based targeted PC. Given that morbidity from S. stercoralis infections is concentrated in adults [47], guidelines may advocate for MDA. Second, the modest sample sizes and baseline prevalence of S. stercoralis infections (< 20%) means that it is unclear, based on the available evidence, how thresholds for MDA should be determined. Finally, there remain uncertainties regarding the added benefit of administering multiple rounds of MDA. Most existing studies assessed the impact of only 1 to 2 rounds, often with variable follow-up periods. Further research and mathematical modelling are needed to address these gaps.
While MDA with ivermectin alone resulted in a moderate reduction in T. trichiura prevalence, its co-administration with albendazole yielded a more substantial reduction, consistent with the efficacy and mathematical modelling literature [6, 48]. These findings support the inclusion of ivermectin for STH control in areas where this species is endemic.
We found a significant reduction in hookworm prevalence with ivermectin and albendazole, and no reduction with ivermectin alone, in agreement with an efficacy meta-analysis [6]. Surprisingly, reduced MDA coverage was associated with a greater hookworm prevalence reduction in our sensitivity analysis, potentially due to fewer MDA rounds in studies with ≥ 75% coverage and/or variations in unmeasured confounding, such as WASH access, socioeconomic status, or baseline infection intensity.
Although we observed a moderate reduction in A. lumbricoides prevalence with ivermectin alone, we did not detect a significant reduction with ivermectin and albendazole MDA. This was unexpected given that the efficacy of albendazole against A. lumbricoides infections is well documented [6]. We hypothesise that our finding may reflect low MDA coverage (with two of the five studies having less than 35% coverage [25, 36]) and/or the longer time period from the last round of MDA to the follow-up assessment in the albendazole and ivermectin studies (average 13.3 months across 5 studies) compared to ivermectin only studies (average 4.7 months across 3 studies). This could be especially impactful for A. lumbricoides due its high fecundity and egg survival rates, leading to increased environmental contamination and consequently rapid rates of reinfection and new infections after MDA [49,50,51].
Meta-regression findings showed that increased baseline prevalence predicted a reduction in MDA effectiveness against T. trichiura and A. lumbricoides, and more rounds of MDA predicted enhanced effectiveness against hookworm, in agreement with mathematical modelling [52].
The publication of the WHO’s 2010–2020 NTD roadmap and the signing of the 2012 London Declaration on NTDs represented a global commitment to treat 75% of children at risk of STH infections through school-based targeted PC programs in all endemic countries, largely relying on international health aid and pharmaceutical donations [53]. There was exceptional progress made towards this goal, where 69% of the 596 million at-risk school-aged children received a benzimidazole tablet by 2017 [54]. Notably, many countries continue to rely on such drug donations to maintain impact. However, these drugs are usually designated for specific risk populations and diseases, such as albendazole for STH control in school-aged children or ivermectin for onchocerciasis control, limiting their reach. Furthermore, there has been a strategic shift in the 2021–2030 roadmap, to move from reliance on international health aid to increased country ownership of control programs supported by domestic funding [53, 55]. Our findings provide evidence to support additional drug supply and funding mechanisms to procure ivermectin and albendazole to enable the implementation of community-wide STH control programs. This would be particularly impactful in areas endemic with S. stercoralis or T. trichiura, and where there is significant geographic overlap with other NTDs that rely on ivermectin, including onchocerciasis, lymphatic filariasis, and scabies.
There were limitations to our study. There were a small number of studies, many quasi-experimental or observational in nature, highlighting a need for more methodologically rigorous studies evaluating the effectiveness of ivermectin-based MDA for STH control. Although we made use of the available evidence, we had insufficient data to draw reliable conclusions for A. lumbricoides and to conduct a direct comparison of drug regimens. There was significant heterogeneity in prevalence reduction for all syntheses, likely due to programmatic and population variation between studies, including socioeconomic and environmental conditions and WASH access. There was evidence of potential publication bias, possibly leading to an overestimation of the true effectiveness of ivermectin PC. Finally, there was an insufficient number of studies reporting infection intensity to allow pooling of results. Measuring changes in prevalence alone fails to capture the full benefits of PC given that higher intensity infections are an important indicator of clinical morbidity [56]. Future studies should evaluate effectiveness using both infection prevalence and intensity outcomes, aligning with WHO targets [55].
Conclusions
Overall, our study underscores the key role of ivermectin-based MDA in addressing the shortcomings of the current global guidelines for STH control. Based on the findings of our study, revising international guidelines to include ivermectin in STH control programs is a promising option for the integrated control and eventual elimination of STHs and other NTDs as public health problems. Achieving this requires a well-coordinated effort that leverages international health aid and mobilises domestic resources effectively.
Availability of data and materials
The data supporting the conclusions of this article are included in the article and its additional file. The raw data used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- LFK index:
-
Luis Furuya-Kanamori index
- MDA:
-
Mass drug administration
- NTD:
-
Neglected tropical disease
- PC:
-
Preventive chemotherapy
- STH:
-
Soil-transmitted helminth
- WASH:
-
Water, sanitation and hygiene
- WHO:
-
World Health Organization
- CI :
-
Confidence interval
- OR :
-
Odds ratio
References
James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–858.
Kyu HH, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1859–922.
Buonfrate D, Bisanzio D, Giorli G, Odermatt P, Furst T, Greenaway C, et al. The global prevalence of Strongyloides stercoralis infection. Pathogens. 2020;9(6):468.
Tamarozzi F, Martello E, Giorli G, Fittipaldo A, Staffolani S, Montresor A, et al. Morbidity associated with chronic Strongyloides stercoralis infection: a systematic review and meta-analysis. Am J Trop Med Hyg. 2019;100(6):1305–11.
World Health Organisation (WHO). Preventive chemotherapy to control STH infection in at risk population groups. 2017.
Clarke NE, Doi SAR, Wangdi K, Chen Y, Clements ACA, Nery SV. Efficacy of anthelminthic drugs and drug combinations against soil-transmitted helminths: a systematic review and network meta-analysis. Clin Infect Dis. 2019;68(1):96–105.
Henriquez-Camacho C, Gotuzzo E, Echevarria J, White AC Jr, Terashima A, Samalvides F, et al. Ivermectin versus albendazole or thiabendazole for Strongyloides stercoralis infection. Cochrane Database Syst Rev. 2016;1:CD007745.
Vercruysse J, Albonico M, Behnke JM, Kotze AC, Prichard RK, McCarthy JS, et al. Is anthelmintic resistance a concern for the control of human soil-transmitted helminths? Int J Parasitol Drugs Drug Resist. 2011;1(1):14–27.
Wolstenholme AJ, Fairweather I, Prichard R, von Samson-Himmelstjerna G, Sangster NC. Drug resistance in veterinary helminths. Trends Parasitol. 2004;20(10):469–76.
Marti H, Haji HJ, Savioli L, Chwaya HM, Mgeni AF, Ameir JS, et al. A comparative trial of a single-dose ivermectin versus three days of albendazole for treatment of Strongyloides stercoralis and other soil-transmitted helminth infections in children. Am J Trop Med Hyg. 1996;55(5):477–81.
Adenusi AA, Oke AO, Adenusi AO. Comparison of ivermectin and thiabendazole in the treatment of uncomplicated human Strongyloides stercoralis infection. Afr J Biotechnol. 2003;2(11):465–9.
Belizario VY, Amraillo ME, de Leon WU, de los Reyes AE, Bugayong MG, Macatangay BJC. A comparison of the efficacy of single doses of ALB, IVM, and DBMZ alone or in combinations against Ascaris and Trichuris spp. Bull World Health Organ. 2003;81(1):35–42.
Wimmersberger D, Coulibaly JT, Schulz JD, Puchkow M, Huwyler J, N’Gbesso Y, et al. Efficacy and safety of ivermectin against Trichuris trichiura in preschool-aged and school-aged children: a randomized controlled dose-finding trial. Clin Infect Dis. 2018;67(8):1247–55.
Omura S, Crump A. Ivermectin: panacea for resource-poor communities? Trends Parasitol. 2014;30(9):445–55.
Romani L, Whitfeld MJ, Koroivueta J, Kama M, Wand H, Tikoduadua L, et al. Mass drug administration for scabies control in a population with endemic disease. N Engl J Med. 2015;373(24):2305–13.
Hardy M, Samuela J, Kama M, Tuicakau M, Romani L, Whitfeld MJ, et al. Community control strategies for scabies: a cluster randomised noninferiority trial. PLoS Med. 2021;18(11): e1003849.
Heukelbach J, Winter B, Wilcke T, Muehlen M, Albrecht S, de Oliveira FA, et al. Selective mass treatment with ivermectin to control intestinal helminthiases and parasitic skin diseases in a severely affected population. Bull World Health Organ. 2004;82(8):563–71.
Knudson A, Ariza Y, Lopez MC, Fejardo OS, Reyes P, Moncada LI, et al. Impacto de la ivermectina sobre sobre las geohelmintiasis en el foco de oncocercosis en Colombia (The effect of ivermectin on geohelminth frequency i.e. as used in the onchocerciasis control program in Colomia). Rev Salud publica. 2012;14(4):681–94. (in Spanish)
Marks M, Gwyn S, Toloka H, Kositz C, Asugeni J, Asugeni R, et al. Impact of community treatment with ivermectin for the control of scabies on the prevalence of antibodies to Strongyloides stercoralis in children. Clin Infect Dis. 2020;71(12):3226–8.
Bah YM, Bah MS, Paye J, Conteh A, Saffa S, Tia A, et al. Soil-transmitted helminth infection in school age children in Sierra Leone after a decade of preventive chemotherapy interventions. Infect Dis Poverty. 2019;8(1):41.
Echazu A, Juarez M, Vargas PA, Cajal SP, Cimino RO, Heredia V, et al. Albendazole and ivermectin for the control of soil-transmitted helminths in an area with high prevalence of Strongyloides stercoralis and hookworm in northwestern Argentina: a community-based pragmatic study. PLoS Negl Trop Dis. 2017;11(10): e0006003.
Massa K, Magnussen P, Sheshe A, Ntakamulenga R, Ndawi B, Olsen A. The combined effect of the lymphatic filariasis elimination programme and the schistosomiasis and soil-transmitted helminthiasis control programme on soil-transmitted helminthiasis in schoolchildren in Tanzania. Trans R Soc Trop Med Hyg. 2009;103(1):25–30.
Ziem JB, Olsen A, Magnussen P, Horton J, Spannbrucker N, Yelifari L, et al. Annual mass treatment with albendazole might eliminate human oesophagostomiasis from the endemic focus in northern Ghana. Trop Med Int Health. 2006;11(11):1759–63.
Vargas P, Krolewiecki AJ, Echazú A, Juarez M, Cajal P, Gil JF, et al. Serologic monitoring of public health interventions against Strongyloides stercoralis. Am J Trop Med Hyg. 2017;97(1):166–72.
Eneanya OA, Gankpala L, Goss CW, Bolay FK, Weil GJ, Fischer PU. Impact of annual versus semiannual mass drug administration with ivermectin and albendazole on helminth infections in Southeastern Liberia. Am J Trop Med Hyg. 2022;106(2):700–9.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Rev Esp Cardiol. 2021;74(9):790–9.
Clarke NE, Clements ACA, Doi SA, Wang D, Campbell SJ, Gray D, et al. Differential effect of mass deworming and targeted deworming for soil-transmitted helminth control in children: a systematic review and meta-analysis. Lancet. 2017;389(10066):287–97.
Stroffolini G, Tamarozzi F, Fittipaldo A, Mazzi C, Le B, Vaz Nery S, et al. Impact of preventive chemotherapy on Strongyloides stercoralis: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2023;17(7): e0011473.
Veritas Health Innovation. Covidence systematic review software. Melbourne, Australia 2023. www.covidence.org. Accessed 20 Mar 2023.
Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–9.
National Heart Lung and Blood Institute. Quality assessment tool for observational cohort and cross-sectional studies. 2014. http://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort. Accessed 20 Mar 2023.
National Heart Lung and Blood Institute. Quality assessment tool for before-after (pre–post) studies with no control group. 2014. http://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-riskreduction/tools/before-after. Accessed 20 Mar 2023.
Furuya-Kanamori L, Barendregt JJ, Doi SAR. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int J Evid Based Healthc. 2018;16(4):195–203.
Ame S, Kabole F, Nanai AM, Mwinzi P, Mupfasoni D, Ali SM, et al. Impact of preventive chemotherapy on transmission of soil-transmitted helminth infections in Pemba Island, United Republic of Tanzania, 1994–2021. PLoS Negl Trop Dis. 2022;16(6): e0010477.
Anselmi M, Buonfrate D, Espinoza AG, Prandi R, Marquez M, Gobbo M, et al. Mass administration of ivermectin for the elimination of onchocerciasis significantly reduced and maintained low the prevalence of Strongyloides stercoralis in Esmeraldas, Ecuador. PLoS Negl Trop Dis. 2015;9(11): e0004150.
Eneanya OA, Gankpala L, Goss CW, Momolu AT, Nyan ES, Gray EB, et al. Community-based trial assessing the impact of annual versus semiannual mass drug administration with ivermectin plus albendazole and praziquantel on helminth infections in northwestern Liberia. Acta Trop. 2022;231: 106437.
Gebrezgabiher G, Yewhalaw D, Ayana M, Hailu A, Mekonnen Z. Impact of ivermectin mass drug administration on burden of soil-transmitted helminths in onchocerciasis control and elimination programs, Yeki district, southwest Ethiopia. PLoS ONE. 2022;17(2): e0263625.
Griswold E, Eigege A, Adelamo S, Mancha B, Kenrick N, Sambo Y, et al. Impact of three to five rounds of mass drug administration on schistosomiasis and soil-transmitted helminths in school-aged children in North-Central Nigeria. Am J Trop Med Hyg. 2022;107(1):132–42.
Hurlimann E, Silue KD, Zouzou F, Ouattara M, Schmidlin T, Yapi RB, et al. Effect of an integrated intervention package of preventive chemotherapy, community-led total sanitation and health education on the prevalence of helminth and intestinal protozoa infections in Cote d’Ivoire. Parasit Vectors. 2018;11(1):1–20.
Knopp S, Mohammed KA, Rollinson D, Stothard JR, Khamis IS, Utzinger J, et al. Changing patterns of soil-transmitted helminthiases in Zanzibar in the context of national helminth control programs. Am J Trop Med Hyg. 2009;81(6):1071–8.
Le B, Monteiro MAAM, Amaral S, Wand H, Matthews A, Hii SF, et al. The impact of ivermectin, diethylcarbamazine, and albendazole mass drug administration on the prevalence of scabies and soil-transmitted helminths in school-aged children in Timor-Leste: a beforeafter assessment. Lancet Glob Health. 2023;11:e924–32.
Le B, Clarke N, Hii SF, Byrne A, Wand H, et al. Effectiveness of one and two doses of ivermectin mass drug administration in reducing the prevalence and intensity of soil-transmitted helminth (STH) infections in Western Province, Solomon Islands: a cluster-randomised, before-after analysis. Lancet Reg Health West Pac. 2023;42: 100942.
Loukouri A, Meite A, Koudou BG, Goss CW, Lew D, Weil GJ, et al. Impact of annual and semi-annual mass drug administration for lymphatic filariasis and onchocerciasis on hookworm infection in Cote d’Ivoire. PLoS Negl Trop Dis. 2020;14(9):1–15.
Moulia-Pelat JP, Nguyen LN, Hasocet H, Luquiaud P, Nicolas L. Advantages of an annual single dose of ivermectin 400 mcg/kg plus diethylcarbamazine for community treatment of bancroftian filariasis. Trans R Soc Trop Med Hyg. 1995;89:682–5.
Ziem JB, Magnussen P, Olsen A, Horton J, Asigri VL, Polderman AM. Impact of repeated mass treatment on human Oesophagostomum and hookworm infections in northern Ghana. Trop Med Int Health. 2006;11(11):1764–72.
Hotez PJ, Bundy AP, Beegle K, Brooker S, Drake L, de Silva N, et al. Helminth infections: soil-transmitted helminth infections and schistosomiasis. In: Disease control priorities in developing countries. New York: Oxford University Press; 2005. p. 467–82.
Schar F, Trostdorf U, Giardina F, Khieu V, Muth S, Marti H, et al. Strongyloides stercoralis: global distribution and risk factors. PLoS Negl Trop Dis. 2013;7(7): e2288.
Turner HC, Truscott JE, Bettis AA, Hollingsworth TD, Brooker SJ, Anderson RM. Analysis of the population-level impact of co-administering ivermectin with albendazole or mebendazole for the control and elimination of Trichuris trichiura. Parasite Epidemiol Control. 2016;1(2):177–87.
Asaolu S, Ofoezie IE. Ascaris spp. In: Rose J, Jiménez-Cisneros B, editors. Water and sanitation for the 21st century: health and microbiological aspects of excreta and wastewater management (global water pathogen project). East Lansing: Michigan State University, UNESCO; 2018.
Izurieta R, Reina-Ortiz M, Ochoa-Capello T. Trichuris trichiura. In: Rose J, Jiménez-Cisneros B, editors. Water and sanitation for the 21st century: health and microbiological aspects of excreta and wastewater management (global water pathogen project). East Lansing: Michigan State University, UNESCO; 2018.
Jia TW, Melville S, Utzinger J, King CH, Zhou XN. Soil-transmitted helminth reinfection after drug treatment: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2012;6(5): e1621.
Coffeng LE, Bakker R, Montresor A, de Vlas SJ. Feasibility of controlling hookworm infection through preventive chemotherapy: a simulation study using the individual-based WORMSIM modelling framework. Parasit Vectors. 2015;8:541.
Huang XX, Toure H, Biswas G. Resource tracking for neglected tropical disease programmes: the first step for developing a sustainable financing strategy. Trans R Soc Trop Med Hyg. 2021;115(2):179–81.
World Health Organization (WHO). Schistosomiasis and soil-transmitted helminthiases: numbers of people treated in 2017. World Health Organization; 2018.
World Health Organisation (WHO). 2030 targets for soil-transmitted helminthiases control programmes: WHO; 2019.
Anderson R, May RM. Infectious diseases of humans: dynamics and control. New York: Oxford Science Publications; 1991.
Acknowledgements
We would like to thank Samantha Bowen from UNSW Library for providing guidance in conducting the literature search.
Funding
SVN is funded by a NHMRC Investigator Grant. The corresponding author (BL) and senior authors (NEC and SVN) had full access to all the data and had final responsibility for the decision to submit for publication.
Author information
Authors and Affiliations
Contributions
SVN conceived the study. SVN, BL, and NEC designed the study and statistical analysis strategy. BL drafted the review protocol, completed the database searches, study screening, data extraction, quality assessment, and statistical analysis, and drafted the manuscript, with support and guidance from NEC and SVN. NL completed the quality control checks. All authors reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to declare.
Supplementary Information
Additional file 1: Appendix S1.
Search strategy (PubMed). Table S1. List of studies excluded at full-text screening stage. Table S2. Quality assessment of studies included in meta-analysis. Figure S1. Doi plots and LFK index for ivermectin preventive chemotherapy studies for A. lumbricoides (a), T. trichiura (b), Hookworm (c), and S. stercoralis (d). Figure S2. Doi plots and LFK index for ivermectin and albendazole preventive chemotherapy studies for Ascaris lumbricoides (a), Trichuris trichiura (b), Hookworm (c), and for all studies for Strongyloides stercoralis (d). Table S3. Pooled prevalence reduction in sensitivity analyses.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Le, B., Clarke, N.E., Legrand, N. et al. Effectiveness of ivermectin mass drug administration in the control of soil-transmitted helminth infections in endemic populations: a systematic review and meta-analysis. Infect Dis Poverty 13, 16 (2024). https://doi.org/10.1186/s40249-024-01185-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40249-024-01185-5