Abstract
Background
Quick diagnosis of smear-negative pulmonary tuberculosis (TB) and extra-pulmonary TB are urgently needed in clinical diagnosis. Our research aims to investigate the usefulness of the interferon-γ release assay (IGRA) for the diagnosis of smear-negative pulmonary and extra-pulmonary TB.
Methods
We performed TB antibody and TB-IGRA tests on 389 pulmonary TB patients (including 120 smear-positive pulmonary TB patients and 269 smear-negative pulmonary TB patients), 113 extra-pulmonary TB patients, 81 patients with other pulmonary diseases and 100 healthy controls. Blood samples for the TB-Ab test and the TB-IGRA were collected, processed, and interpreted according to the manufacturer’s protocol.
Results
The detection ratio of smear-positive pulmonary TB patients and smear-negative pulmonary TB patients were 90.8% (109 of 120) and 89.6% (241 of 269), respectively. There was no statistically significant difference of its performance between these two sample sets (P > 0.05). The detection ratio of positive TB patients and extra-pulmonary TB patients were 90.0% (350 of 389) and 87.6% (99 of 113), respectively, which was not significantly different (P > 0.05).
Conclusions
In this work, the total detection ratio using TB-IGRA was 89.4%, therefore TB-IGRA has diagnostic values in smear-negative pulmonary TB and extra-pulmonary TB diagnosis.
Similar content being viewed by others
Multilingual abstracts
Please see Additional file 1 for translations of the abstract into five official languages of the United Nations.
Background
The World Health Organization’s (WHO) flagship Global TB Report 2016, released on Oct 12, considers Mycobacterium tuberculosis as one of the most significant human pathogens that are harmful to the global public health [1]. Over 550 million Chinese are infected with M. tuberculosis, including nearly 100 million extra-pulmonary tuberculosis (TB) patients and 300 million sputum smear-negative and/or culture-negative infections [1]. The clinical manifestations of TB are highly varied and unspecific; M. tuberculosis is able to infect various systems of the human body. The bacteriological examination method (smear microscopy) is still the gold standard for TB diagnosis in many countries, but the low smear-positive rate and long incubation period required to obtain positive cultures are problematic for the requirements in clinical diagnosis and treatment. Extra-pulmonary disease, like disseminated TB, brings great difficulties in clinical diagnosis [2, 3], since it is very hard to detect M. tuberculosis in patient’s sputum. Therefore, it results in a delay in the diagnostic process for pulmonary TB, especially in smear-negative cases [4]. Early detection and accurate diagnosis of TB could reduce the morbidity and spread of TB and it is also the key element in TB control [4]. Serological diagnosis of TB, such as the TB antibody (TB-Ab) test, is widely used in the laboratory in China, but the diagnostic yield is generally no more than 70%. Therefore, there is an urgent need for developing rapid and highly sensitive technology to change this situation [5, 6]. The interferon-γ release assay (IGRA) uses a special antigen as stimulus and follows Enzyme Linked Immunosorbent Assay (ELISA) procedures for detection has potentially high specificity and sensitivity. After being invented by Lalvani [5], this method is widely used in many counties and has become the most commonly used diagnostic method in TB detection [7,8,9,10].
IGRA is an ex vivo blood test of the T-cell immune response. It detects the T-cell release of interferon-gamma (IFN-γ), an inflammatory cytokine, following stimulation by antigens specific to the M. tuberculosis complex. These antigens include 6-kDa early secretory antigenic target (ESAT-6) and 10-kDa culture filtrate antigen (CFP-10), which are more specific for M. tuberculosis than the tuberculin skin test (TST) because they are not produced by Bacillus Calmette–Guérin (BCG) vaccine strains and non-tuberculosis mycobacteria (NTM) strains [11].
In order to verify the sensitivity and specificity of TB-IGRA in TB tests, we compared the diagnostic performance of TB-IGRA and TB-Ab tests in 389 pulmonary TB patients, 113 extra-pulmonary TB patients, 81 patients with other pulmonary diseases and 100 healthy individuals visiting the Center of Physical Examination for routine physical examination.
Methods
Subjects
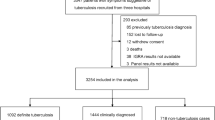
This work has obtained approval from the Research Ethics Committee of Hangzhou Medical College. All subjects signed the informed consent forms as approved. Demographic and clinical data were collected using a specific form and then transferred into a database. The examination for TB was usually completed within one week. Whole blood samples of 502 patients with TB were collected from Hangzhou Red Cross Hospital, Quzhou People’s Hospital, and Hospital of integrated traditional Chinese and Western medicine in Xiacheng District of Hangzhou and the Center for Disease Control and Prevention (CDC) of Zhejiang Province of China between September 2012 and June 2013. The demographic characteristics of the subjects in this study are shown in Table 1. The average age of the patients was 45 years and ranged from 13 to 82 years of age.
According to sputum-smear, sputum-culture and X-ray tests, 120 patients were classified as smear-positive pulmonary TB patients, 269 patients were classified as smear-negative pulmonary TB patients and 113 patients were classified as extra-pulmonary TB patients (including tuberculous pleurisy, tuberculous peritonitis, spinal TB, renal TB, pelvic TB and intestinal TB). According to clinical manifestations, pathological diagnosis, sputum smear and culture, and X-ray diagnosis, 81 patients were classified as other lung disease patients (including pneumonia, lung cancer, lung tumors and bronchiectasis); the average age of these patients was 49 years and ranged from 17 to 82 years of age. One hundred cases of healthy individuals visiting the Center of Physical Examination for routine physical examination were collected from the above-mentioned hospitals. These healthy individuals had no prior history of TB and were sputum culture and X-ray negative. The average age of these subjects was 48 years and ranged from 31 to 60 years of age.
Reagents and instruments
TB-IGRA kits and TB-Ab kits were purchased from Beijing Wantai Biological Pharmacy Co., Ltd. and Nanjing Potomac Bio-Technology Co., Ltd., respectively. Multiskan MK-3 from Lab systems. Biosafety Cabinet from Heal Force. BD-TEK-ELX50 from Bio-Tek Company.
TB-Ab test
The TB-Ab test was used to detect serum samples. Assays and interpretation of results were strictly according to the manufacturers’ instructions. Simultaneously, sputum smear and sputum culture assays were performed.
Interferon-γ release assay
All subjects were tested with TB-IGRA according to the manufacturer’s instructions. Six milliliter fresh whole blood was collected using heparin vacutainer blood collection tubes. Briefly, 1 ml of peripheral venous blood samples collected from each participant were injected in three special culture tubes for the TB-IGRA: One test tube (T) coated with M. tuberculosis-specific antigens (a recombinant fusion protein of CFP-10 and ESAT-6), one positive control tube (P) containing phytohemagglutinin (PHA), and one negative control tube (N). Then the three tubes were incubated at 37 °C for 22 ± 2 h. Subsequently, the tubes were centrifuged at 3000 g for 10 min and the serum was stored at −20 °C until detection. The IFN-γ levels were detected using the ELISA method. Positive samples were identified following the criteria defined in Table 2 [12].
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics ver. 11.0 (IBM Co., Armonk, NY, USA). Statistical significance was defined as P < 0.05. Student’s t-tests were used to compare continuous variables of the study groups. To evaluate discrete variables, Pearson chi-square and Fisher exact tests were performed as appropriate. For the assessment of diagnostic agreement between tests, Cohen κ statistics were used.
Results
TB-IGRA test results of different patient groups
The total detection ratio of TB-IGRA tests for all groups combined was 89.4% (449 of 502), while the detection ratios of the TB group and extra-pulmonary TB group were 90.0% (350 of 389) and 87.6% (99 of 113), respectively. The detection ratios of sputum positive and smear-negative TB patient groups were 90.8% (109 of 120) and 89.6% (241 of 269), respectively, and the detection ratios between these two patient groups were not significant different (χ 2 = 0.52 and 0.14,P > 0.05). The detection ratios of TB-IGRA in other lung diseases and healthy controls was 11.6% (21 of 181), while the non-TB lung disease group TB-IGRA total detection ratio was 16.0% (13 of 81). Therefore, it was significantly lower than the detection ratio in TB patients, which was 90.0% (350 of 389) (χ 2 = 208.36, P < 0.01) (Tables 3 and 4).
Sensitivity comparison of TB-IGRA and TB-Ab test
The TB-IGRA and TB-Ab detection sensitivities of sputum positive TB patients were 90.8% (109 of 120) and 41.7% (50 of 120), respectively, the detection sensitivities of smear-negative TB patients were 89.6% (241 of 269) and 31.6% (85 of 269), respectively, and the overall detection sensitivities of TB patients were 90.0% (350 of 389) and 34.7% (135 of 389), respectively. The TB-IGRA and TB-Ab detection sensitivities of extra-pulmonary TB were 87.6% (99 of 113) and 31.0% (35 of 113), respectively, while the overall sensitivities of TB-IGRA and TB-Ab detection of TB were 89.4% (449 of 502) and 33.9% (170 of 502), respectively. Therefore, the sensitivity of the TB-IGRA test was significantly higher than the sensitivity of the TB-Ab test (χ 2 = 64.9–327.9, P < 0.01) (Table 3).
Specificity comparison of TB-IGRA and TB-Ab test
The specificity of the TB-IGRA tests for the healthy control group and the other lung diseases group were 92.0% (92 of 100) and 83.9% (68 of 81), respectively, while the specificity of the TB-Ab tests for the healthy controls group and the lung diseases group were 93.0% (93 of 100) and 86.4% (70 of 81), respectively. The overall specificity of the TB-IGRA tests and the TB-Ab tests were 88.4% (160 of 181) and 90.1% (163 of 181), respectively, which were not significantly different (χ 2 = 0.2, P > 0.05) (Table 4).
Discussion
Currently, rapid diagnosis of TB is depending on observation of clinical symptoms, radiographic examination, smears and culture of clinical samples [4]. Because the negative rate of smears and culture of clinical samples is too high and the pathological samples for testing are hard to obtain, it is difficult to diagnose smear-negative and extra-pulmonary TB. Although the TST test is widely used to detect TB, NTM and BCG vaccination is known to introduce false-positive results [5]. Furthermore, in the TST test, patients with advanced HIV disease could give rise to false negative results [6]. In China, the BCG vaccination program has been widely implemented and causes a highly false-positive detection ratio in TST test [13]. Therefore, immunological methods with high sensitivity and specificity to detect smear-negative and extra-pulmonary TB are urgently needed.
In this work, the total detection ratio of TB-IGRA tests was 89.4%, which was higher than the widely used TB-Ab test that showed a detection ratio of 33.9% (P < 0.01). Furthermore, these ratios were also higher than results reported by Wang JY (87%) [14] and Kobashi Y (86%) [15], but slightly lower than Kim SH’s result (95%) [16]. Overall, TB-IGRA showed a higher detection ratio of TB than other serological methods. In addition, the detection ratio of this method in smear-negative TB patients and positive pulmonary TB patients showed no significant difference (89.6% vs 90.8%, P > 0.05). Given that the TB-IGRA test has a high sensitivity, is able to detect smear-negative patients effectively, and can be used for latent TB detection, we used TB-IGRA for the diagnosis of TB and extra-pulmonary TB. The sensitivity of these tests were 90.0 and 87.6%, which was not significantly different (P > 0.05). The sensitivity of the TB-Ab test that is used in TB and extra-pulmonary TB detection was 34.7 and 31%, which was significantly lower than the sensitivity of TB-IGRA (P < 0.01). Furthermore, the TB-IGRA and TB-Ab specific detection ratios of healthy controls were 92.0 and 93.0%, while specific detection ratios in the lung disease group were 83.9 and 86.4%. Therefore, no significant difference in specificity was observed (P > 0.05). Although the detection ratio of the TB-IGRA was very high, still 8 positive samples in the healthy controls group were detected. Therefore, we need to confirm whether these positive samples are real false positives or latent TB.
Conclusions
In this work, we showed that the total detection ratio of the TB-IGRA tests was 89.4%, confirming that the TB-IGRA test has high sensitivity and specificity and diagnostic values in smear-negative pulmonary TB and extra-pulmonary TB diagnosis. The use of the TB-IGRA test may help in the early detection and accurate diagnosis of TB.
Abbreviations
- BCG:
-
Bacillus Calmette–Guérin
- CDC:
-
Centers for disease control and prevention
- CFP-10:
-
10 kDa culture filtrate antigen
- ELISA:
-
Enzyme linked immunosorbent assay
- ESAT-6:
-
6-kDa early secretory antigenic target
- IFN-γ:
-
Interferon-γ
- IGRA:
-
Interferon-γ release assay
- NTM:
-
Non-tuberculosis mycobacteria
- PHA:
-
Phytohemagglutinin
- TB:
-
Tuberculosis
- TB-Ab:
-
TB antibody
- TST:
-
Tuberculin skin test
- WHO:
-
World Health Organization
References
WHO. Global tuberculosis report 2016. Geneva: World Health Organization; 2016. http://www.who.int/tb/publications/global_report/en/. Accessed 15 Nov 2016.
Fry DE. Extra-pulmonary tuberculosis and its surgical treatment. Surg Infect. 2016;17(4):394–401.
Ali Chaudhry L, Al-Solaiman S. Multifocal tuberculosis: many faces of an old menace. Int J Mycobacteriol. 2013;2(1):58–69.
Park MY, Kim YJ, Hwang SH, Kim HH, Lee EY, Jeong SH, et al. Evaluation of an immunochromatographic assay kit for rapid identification of Mycobacterium tuberculosis complex in clinical isolates. J Clin Microbiol. 2009;47(2):481–4.
Lalvani A. Diagnosing tuberculosis infection in the 21st century: new tools to tackle an old enemy. Chest. 2007;131(6):1898–906.
Mandalakas AM, van Wyk S, Kirchner HL, Walzl G, Cotton M, Rabie H, et al. Detecting tuberculosis infection in HIV-infected children: a study of diagnostic accuracy, confounding and interaction. Pediatr Infect Dis J. 2013;32(3):e111–8.
Wang MS, Wang JL, Wang XF. The performance of interferon-gamma release assay in nontuberculous mycobacterial diseases: a retrospective study in China. BMC Pulm Med. 2016;16(1):163.
Huo ZY, Peng L. Accuracy of the interferon-γ release assay for the diagnosis of active tuberculosis among HIV-seropositive individuals: a systematic review and meta-analysis. BMC Infect Dis. 2016;16:350.
Clifford V, He Y, Zufferey C, Connell T, Curtis N. Interferon gamma release assays for monitoring the response to treatment for tuberculosis: a systematic review. Tuberculosis. 2015;95(6):639–50.
Sun L, Yan HM, Hu YH, Jiao WW, Gu Y, Xiao J, et al. IFN-γ release assay: a diagnostic assistance tool of tuberculin skin test in pediatric tuberculosis in China. Chin Med J. 2010;123(20):2786–91.
Pai M, Behr M. Latent Mycobacterium tuberculosis infection and interferon-gamma release assays. Microbiol Spectr. 2016;4(5). doi:10.1128/microbiolspec.TBTB2-0023-2016.
Wantai. Wantai quantitative diagnostic kit for Mycobacterium tuberculosis IFN-γ release assay (WT-IGRA) [package insert]. Beijing: Beijing Wantai Biological Pharmacy Co., Ltd; 2012.
Ruan Q, Zhang S, Ai J, Shao L, Zhang W. Screening of latent tuberculosis infection by interferon-γ release assays in rheumatic patients: a systemic review and meta-analysis. Clin Rheumatol. 2016;35(2):417–25.
Wang JY, Chou CH, Lee LN, Hsu HL, Jan IS, Hsueh PR, et al. Diagnosis of tuberculosis by an enzyme-linked immunospot assay for interferon-gamma. Emerg Infect Dis. 2007;13(4):553–8.
Kobashi Y, Obase Y, Fukuda M, Yoshida K, Miyashita N, Oka M. Clinical reevaluation of the QuantiFERON TB-2G test as a diagnostic method for differentiating active tuberculosis from nontuberculous mycobacteriosis. Clin Infect Dis. 2006;43(12):1540–6.
Kim SH, Choi SJ, Kim HB, Kim NJ, Oh MD, Choe KW. Diagnostic usefulness of a T-cell based assay for extrapulmonary tuberculosis. Arch Intern Med. 2007;167(20):2255–9.
Acknowledgements
The authors would like to thank Prof. Stijn van der Veen for critical reading of the manuscript. We gratefully acknowledge the contribution of all health staff.
Funding
This work was supported by Grants from the National Natural Sciences Foundation of China (81271893), the Natural Science Foundation of Zhejiang Province (LY12H19002), and Zhejiang Provincial Program for the Cultivation of High-level Innovative Health Talents, the Scientific Research Foundation of the Education Department of Zhejiang Province (Y201534356), the Natural Science Foundation of Zhejiang Medical College (2014B01) and Visiting Engineer Program of the Education Department of Zhejiang Province (FG2014011).
Availability of data and materials
The datasets supporting the findings of this paper are included in the paper.
Author information
Authors and Affiliations
Contributions
JL and LY were responsible for the initial study concept. YJ and SA all contributed to the study design. WZ carried out the data collection. JJ conducted the thematic analysis. FX drafted the initial paper with input from all authors. WL edited the initial paper. The remaining authors critically reviewed it and made revisions. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This work has obtained the approval from the Research Ethics Committee of Hangzhou Medical College. The approval numbers are 2013–002 and 2011–011. The serum specimens used in this study have been allowed to collect from TB patients. Written informed consents have been obtained from the participants. We also have obtained the written informed consents from the guardians on behalf of the minors/children enrolled in our study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional file
Additional file 1:
Multilingual Abstracts in the five official working languages of the United Nations. (PDF 869 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ji, L., Lou, YL., Wu, ZX. et al. Usefulness of interferon-γ release assay for the diagnosis of sputum smear-negative pulmonary and extra-pulmonary TB in Zhejiang Province, China. Infect Dis Poverty 6, 121 (2017). https://doi.org/10.1186/s40249-017-0331-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40249-017-0331-1