Abstract
Background
Recent studies suggested that genetic variants associated with monogenic bone disorders were involved in the pathogenesis of atypical femoral fractures (AFF). Here, we aim to identify rare genetic variants by whole exome sequencing in genes involved in monogenic rare skeletal diseases in 12 women with AFF and 4 controls without any fracture.
Results
Out of 33 genetic variants identified in women with AFF, eleven (33.3%) were found in genes belonging to the Wnt pathway (LRP5, LRP6, DAAM2, WNT1, and WNT3A). One of them was rated as pathogenic (p.Pro582His in DAAM2), while all others were rated as variants of uncertain significance according to ClinVar and ACMG criteria.
Conclusions
Osteoporosis, rare bone diseases, and AFFs may share the same genes, thus making it even more difficult to identify unique risk factors.
Similar content being viewed by others
Background
Atypical femoral fractures (AFF) are low-impact fractures that differ from classic osteoporotic femoral fractures in that they occur in the subtrochanteric region or femoral diaphysis, usually in the setting of prolonged treatment with bisphosphonates (BP).While its physiopathology has not been completely clarified, genetic predisposition appears to be key given that the incidence of AFF is very low in the general population (5.9 per 10,000 person-years) [1], and specific patient populations appear to be at an increased risk of sustaining them including people with Asian ancestry and patients affected with specific monogenic bone disorders [2]. A number of studies have tried to identify the genes involved in the AFF risk suggesting that AFF occur in the setting of a complex and heterogeneous genetic background where each affected individual could have their own genetic burden [3, 4]. In a recent study by Zhou et al. (2023) [5], the authors suggested that genetic variants associated with monogenic bone disorders might play a role in the pathogenesis of AFF. In their study, 37 candidate genes involved in monogenic bone disorders were analyzed from whole-exome sequencing (WES) data in 60 AFF patients, with 95% having received bisphosphonates. Fifteen (25%) of the 60 AFF patients had clinical features of a monogenic bone disorder. In total, nine patients in their AFF cohort (15%) had a (likely) pathogenic variant, eight of whom fulfilled clinical criteria suggestive of monogenic bone disorders.
In a prior study performed by our group [6], we selected genetic variants in genes shared by at least two AFF patients and absent in controls. Hence, those variants only present in one AFF patient were removed from the analysis.
In view of the recent studies [3, 4] where each individual could have their own genetic background and furthermore, genes involved in monogenic bone disorders can play an important role, we decided to contribute with new data on 12 women with AFF and 4 controls without any fracture, all of whom had received bisphosphonates for over 5 years due to a diagnosis of osteoporosis. In the present study, we aimed to recover all rare genetic variants present in our AFF patients and controls from a list of 37 candidate genes proposed by Zhou et al. [5] and other additional genes involved in rare monogenic diseases with bone impairment.
Methods
Participants were previously described in a work published by our group [6]. Briefly, twelve unrelated postmenopausal women with AFF (mean age ± SD of 74.5 ± 6.1) and four postmenopausal women without any fracture (controls) (mean age ± SD of 79 ± 7.2) were recruited in Hospital del Mar (Barcelona, Spain) and Hospital Universitario de La Princesa (Madrid, Spain). All of them received bisphosphonate (BP) treatment for > 5 years due to a diagnosis of osteoporosis. No patient had hypophosphatemia or suspicion of a monogenic disease. Half of the AFF patients had received corticosteroid therapy for more than one year due to polymyositis, rheumatoid arthritis, asthma or chronic bronchitis. None of the controls had receive glucocorticoids.
Whole exome sequencing (WES) was performed at the CNAG facilities (Barcelona, Spain). Capture was performed using Agilent Human All Exon 50 Mb v5 and samples were sequenced at a coverage of 140x on a HiSeq 2000 sequencer. Pipeline of the WES is detailed in Garcia-Giralt et al. (2022) [6].
We filtered for rare variants (MAF < 0.005) with CADD > 20 and the resulting variants were overlapped with our list of candidate genes (Supplemental Table 1).
Results and discussion
A total of 41 genetic variants were detected in genes belonging to the list of candidate genes (Table 1). Only one of the variants identified was rated as pathogenic according to ClinVar or ACMG guidelines (p.Pro582His in DAAM2 [7]), while all others were rated as variants of uncertain significance (VUS) according to ACMG criteria.
Interestingly, variants in COL1A1 and COL1A2 were detected in control individuals (with osteoporosis and long-term BP treatment, but without AFF), suggesting their putative involvement in the underlying osteoporosis phenotype. The same could be proposed for the FKBP10 and TNXB genes, which were found mutated in controls and AFF patients. Zhou et al. [5] found likely pathogenic variants and VUS in COL1A1 and COL1A2 genes related to a diagnosis of osteogenesis imperfecta or monogenic osteoporosis in 5 AFF patients, which could suggest a role of these genes in both bone tissue pathology and AFF.
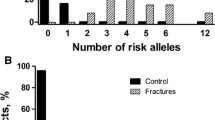
Out of 33 genetic variants identified in women with AFF, eleven (33.3%) were found in genes belonging to the Wnt pathway (LRP5, LRP6, DAAM2, WNT1, and WNT3A). Moreover, the AFF11 woman was homozygous for a mutation in DAAM2. It is difficult to discern whether these genes play a role in the pathophysiology of AFF in addition to their known role in low bone mass. Similarly, LRP5 was also found mutated in 2 AFF patients with a diagnosis of monogenic osteoporosis in the Zhou et al. study [5] suggesting this putative dual role. On the other hand, DAAM2 gene was not assessed in the AFF patients from that study and we cannot know its involvement in bone phenotypes.
Subject AFF1 did not carry any mutations from our list of candidate genes while all other AFF patients were carriers of variants in more than one gene. For example, subject AFF11 accumulated up to 9 rare genetic variants, one of them in homozygosity (DAAM2). Unfortunately, there is no information about this latter variant in the ClinVar database. Interestingly, Daam2 KO mice showed a marked reduction in bone strength, despite minimal changes in bone morphology and mineral content, indicating an abnormal bone composition and structure explained in part by cortical impairment [8].
While none of our patients could be confidently diagnosed of any monogenic bone disorder, like most of the Dutch AFF cohort [5], all shared the common feature of severe postmenopausal osteoporosis that required long-term BP treatment and, in some cases, also denosumab. Noteworthy, 50% of the women with AFF in our cohort and none of the controls had been on long-term glucocorticoid treatment which is a recognized risk factor for AFF [9]. When comparing both cohorts according to the gene candidate list proposed by Zhou et al. [5] (see supplemental Table 1) and considering all AFF patients with or without a clinical suspicion of monogenic bone disorders, a similar number of carriers of variants in Mendelian bone disease genes was detected (46% in Zhou et al. vs. 50% in this cohort).
Conclusion
Encompassing all of our findings we conclude that in our cohort we did not detect a major gene involved in AFF pathophysiology. We speculate that AFF development is probably the result of the sum of genetic variants together with other structural, physiological and environmental factors. If osteoporosis, rare bone diseases, and AFFs share the same genes, identifying unique risk factors could be even more challenging.
These results warrant further studies of genes related to monogenic bone disorders in the setting of severe osteoporosis, in addition to their potential role in AFF pathogenesis.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due extensive genomic information but are available from the corresponding author on reasonable request.
References
Feldstein AC, Black D, Perrin N, Rosales AG, Friess D, Boardman D, et al. Incidence and demography of femur fractures with and without atypical features. J Bone Min Res. 2012;27(5):977–86.
Nguyen HH, van de Laarschot DM, Verkerk A, Milat F, Zillikens MC, Ebeling PR. Genetic risk factors for atypical femoral fractures (AFFs): a systematic review. JBMR Plus. 2018;2(1):1–11.
Zhou W, van Rooij JGJ, Ebeling PR, Verkerk A, Zillikens MC. The Genetics of atypical femur Fractures-a systematic review. Curr Osteoporos Rep. 2021;19(2):123–30.
Del Real A, Cruz R, Sanudo C, Perez-Castrillon JL, Perez-Nunez MI, Olmos JM et al. High Frequencies of Genetic Variants in patients with atypical femoral fractures. Int J Mol Sci. 2024;25(4).
Zhou W, van Rooij JG, van de Laarschot DM, Zervou Z, Bruggenwirth H, Appelman-Dijkstra NM, et al. Prevalence of monogenic bone disorders in a Dutch cohort of atypical femur fracture patients. J Bone Min Res. 2023;38(6):896–906.
Garcia-Giralt N, Roca-Ayats N, Abril JF, Martinez-Gil N, Ovejero D, Castaneda S et al. Gene Network of Susceptibility to atypical femoral fractures related to Bisphosphonate Treatment. Genes (Basel). 2022;13(1).
Schneider R, Deutsch K, Hoeprich GJ, Marquez J, Hermle T, Braun DA, et al. DAAM2 variants cause nephrotic syndrome via actin dysregulation. Am J Hum Genet. 2020;107(6):1113–28.
Morris JA, Kemp JP, Youlten SE, Laurent L, Logan JG, Chai RC, et al. An atlas of genetic influences on osteoporosis in humans and mice. Nat Genet. 2019;51(2):258–66.
Black DM, Eastell R, Adams AL. Atypical femur fracture risk versus Fragility Fracture Prevention with bisphosphonates. Reply. N Engl J Med. 2020;383(22):2189–90.
Acknowledgements
Not applicable.
Funding
This research was funded by Centro de Investigación Biomédica en Red de Fragilidad y Envejecimiento Saludable (grant number CB16/10/00245); Fundación Española de Investigación Ósea y del Metabolismo Mineral (FEIOMM); Fondo de Investigación en Salud (grant number PI19/00033) from Instituto de Salud Carlos III (ISCIII) and European Union Fund. The research was also supported by MCIN/AEI/https://doi.org/10.13039/501100011033, Project PID2019-107188RB-C21, and AGAUR. DO is recipient of a Miquel Servet grant from ISCIII.
Author information
Authors and Affiliations
Contributions
Conceptualization: N.G.G., D.G., S.B. and R.R.; Patient recruiting and phenotyping: D.O., S.C. and X.N.; Methodology: N.G.G., D.G., S.B., and R.R.; Validation: N.G.G. and R.R.; Formal Analysis: N.G.G. and R.R.; Investigation: N.G.G., D.G., S.B., and R.R.; Data Curation: all authors; Writing—Original Draft Preparation, N.G.G. and D.O.; Writing—Review & Editing: All authors; Supervision: S.B., D.G., X.N. and R.R.; Project Administration: N.G.G.; Funding Acquisition: N.G.G., X.N., S.C., S.B. and D.G. All authors have reviewed and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Clinical Research Ethics Committee of Parc de Salut Mar (CEIC; 2017/7717/I).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.

Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Garcia-Giralt, N., Ovejero, D., Grinberg, D. et al. Assessing the contribution of genes involved in monogenic bone disorders to the etiology of atypical femoral fractures. Hum Genomics 18, 87 (2024). https://doi.org/10.1186/s40246-024-00652-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40246-024-00652-2