Abstract
Background
Phenylketonuria (PKU) is a common, autosomal recessive inborn error of metabolism caused by PAH gene variants. After routine genetic analysis methods were applied, approximately 5% of PKU patients were still not diagnosed with a definite genotype.
Methods
In this study, for the first time, we identified PKU patients with unknown genotypes via single-gene full-length sequencing.
Results
The detection rate of PKU genotype increased from 94.6 to 99.4%, an increase of approximately 5%. The variants c.1199 + 502A > T and 1065 + 241C > A were found at a high frequency in Chinese PKU patients.
Conclusion
Our study suggest that single-gene full-length sequencing is a rapid, efficient and cost-effective tool to improve the genotype detection rate of PKU patients. Moreover, we provides additional case data to support pathogenicity of deep intronic variants in PAH.
Similar content being viewed by others
Introduction
Phenylketonuria (PKU) is the most common congenital disorder of amino acid metabolism, with a global prevalence of 1:10,000 newborns [1]. PKU is due to a deficiency in phenylalanine hydroxylase (PAH) activity caused by the PAH variant [2]. When this enzyme is deficient, elevated phenylalanine (Phe) can have toxic effects on the nervous system. In line with the European guidelines [3] and Chinese guidelines [4] for PKU, it is classified into mild PKU (mPKU, 360–1200 μmol/L) and classic PKU (cPKU, ≥ 1200 μmol/L), depending on the Phe concentration in peripheral blood at the time of diagnosis. Many countries have included PKU in neonatal screening programs. According to the latest screening data, the incidence of PKU was 6.28:100,000 newborns in China from 2013 to 2017[5].
Genetic analysis is an effective means for early etiological diagnosis, treatment guidance and prenatal diagnosis of PKU patients. Based on Chinese guidelines [4] gene diagnosis is the diagnostic method of the etiology of HPA patients, and it is recommended to carry out routine testing, especially for patients with atypical biochemical phenotypes. Through PAH gene detection, PKU patients can be identified more quickly and effectively.
The American College of Medical Genetics and Genomics (ACMG) [6] suggests that mutation analysis should be obtained for all infants with elevated Phe. Because of the high prevalence rate of PKU, PAH has been included in carrier screening by ACMG [7].
At present, routine molecular genetic analysis is commonly used in the clinical detection of PAH variants, including Sanger sequencing, next-generation sequencing (NGS) gene panels and multiplex ligation-dependent probe amplification (MLPA). Through the analysis of the PAH gene variant spectrum in different populations, 87–96% of PKU patients can be identified by sequencing all exons and flanking intron regions [8,9,10]. Exonic deletion/duplication identified by MLPA accounts for 2–3% of pathogenic PAH alleles [11, 12]. Approximately 5% of the remaining patients have typical clinical symptoms, but the genotype is unknown [11].
An analysis of the genetic landscape of PKU found that among pathogenic variants of PAH, 17.9% occur in introns or untranslated regions [1]. However, although conventional molecular genetic analysis can detect these regions, it only contains a small number of known variants and cannot cover all deep introns, 5′UTR and 3′UTR regions. In this study, we applied full-length sequencing of PAH single genes in PKU patients with unknown genotypes and with deletion/duplication of PAH. We examined the use of single-gene full-length sequencing for characterizing the molecular genetics of PKU patients and provide additional reference data for variant detection of deep introns of PAH.
Patients and methods
Subjects
Based on clinical features and newborn screening, a total of 687 patients were diagnosed with PKU at the Third Affiliated Hospital of Zhengzhou University from January 2016 to December 2021. All of them underwent PAH gene molecular genetic analysis through the gene panel (including PAH and DNAJC12) by NGS and MLPA.
We reanalyzed the clinical phenotypes and molecular genetic results of these PKU families to screen out patients with unknown genotypes. The inclusion criteria were as follows: (1) exhibiting PKU phenotypes or increased blood Phe concentrations (≥ 360 μmol/L); (2) having only a single deleterious heterozygous variant or no variants identified after PAH gene molecular genetic analysis; (3) having been excluded from tetrahydrobiopterin deficiency.
After screening, a total of 37 PKU patients with unknown genotypes and their family members were enrolled. Among them, thirty-six PKU patients had only a single deleterious heterozygous variant identified, and one patient did not have any variants detected. Samples from all of these probands underwent single-gene full-length sequencing. To test the detection efficiency of single-gene full-length sequencing, we selected 5 samples with different exon deletions or duplications in PAH detected by MLPA analysis for sequencing (Fig. 1). All PKU families signed informed consent, and the study passed the ethical approval of Third Affiliated Hospital of Zhengzhou University.
Single-gene full-length sequencing
Sequencing of residual DNA specimens from the probands was used for library preparation and target capture. Library preparation included end repair, adapter ligation and PCR enrichment and was carried out as recommended by Illumina protocols. The amplified DNA was captured using a GenCap Phenylketonuria capture kit (MyGenostics GenCap Enrichment Technologies). An Illumina HiSeq X Ten Sequencer (Illumina, San Diego, USA) with 150 bp paired-end sequencing mode was used for sequencing the genomic DNA. The mean sequencing coverage was > 1000 × , and > 99.0% of bases for every sample were sequenced to at least 20 × coverage.
Data analysis
The sequencing reads were aligned to the human reference genome (hg19/GRCh37) using BWA, and PCR duplicates were removed by using Picard v1.57 (http://picard.sourceforge.net/). The variants of single nucleotide variants (SNVs) and insertion-deletion (InDel) were detected by GATK (https://software.broadinstitute.org/gatk/). Variant annotation and interpretation were conducted by ANNOVAR [13] and associated with multiple databases. The annotation databases mainly included (1) human population databases, such as gnomAD (http://gnomad.broadinstitute.org/), the 1000 Genome Project (http://browser.1000genomes.org), “HUABIAO” whole-exome public database (https://www.biosino.org/wepd/index) and dbSNP (http://www.ncbi.nlm.nih.gov/snp); (2) in silico prediction algorithms, such as SIFT (http://sift.jcvi.org), FATHMM (http://fathmm.biocompute.org.uk), MutationAssessor (http://mutationassessor.org), and CADD (http://cadd.gs.washington.edu); and (3) disease and phenotype databases, such as ClinVar (http://www.ncbi.nlm.nih.gov/clinvar), HGMD (http://www.hgmd.org), and BIOPKU (http://www.biopku.org/home/home.asp). The impact of variants on the splice site was predicted by using Alamut® Visual Plus v1.1.
Large-scale deletion/duplication of PAH was identified using CNVkit [14]. Normal references used for CNV identification were obtained using sequencing data from 10 normal males and 10 females that had previously been validated without large deletions or duplications of PAH by MLPA.
Variant validation and classification
All putatively causal variants were sequenced by Sanger method to confirm the genotypes of the probands and parents. The variants were classified into five categories: pathogenic, likely pathogenic, uncertain significance, likely benign and benign, according to the ClinGen PAH Expert Panel Specifications to the ACMG/AMP Variant Interpretation Guidelines [15].
Analysis of nonbenign PAH variants in deep introns and untranslated regions
A total of 1282 variants were included in the PAHvdb database (as of June 18, 2021), and we screened the SNVs in deep introns and untranslated regions by manual screening. The screening criteria were as follows: (1) located on introns, 5′UTR or 3′UTR that distance exons > 20 bp; (2) having reliable supporting reports in PubMed (https://pubmed.ncbi.nlm.nih.gov/); (3) having no evidence of benign impact correlation in ClinVar and HGMD databases; (4) having an allele frequency no greater than 5% in the gnomAD database. We analyzed the variants screened manually and the deep intronic novel variants detected in patients in this study, including analyses of genome location and carrier population.
Results
SNV/indel detection
After screening, a total of 37 PKU patients with unknown genotypes were included. Their information, genotypic and phenotypic characteristics are summarized in Table 1.
After single-gene full-length sequencing, 74 potential disease-causing variant alleles were identified. A total of 33 patients were completely genotyped, of which 28 carried compound heterozygous variants and 5 harbored three separate variants. Compared with the previous results, the detection rate of PKU increased from 94.6% (650/687) to 99.4% (683/687), an increase of approximately 5%. However, there were still four patients with unclear genotypes. Although they have identified some variants of uncertain significance, the pathogenicity of these variants may need more evidence (Additional file 1: Table S1).
Among the results from 33 patients identified by full-length sequencing, all of the newly detected variant alleles were in the deep introns, including c.707-59C > G, c.1065 + 241C > A, c.1199 + 502A > T and a novel variant c.706 + 629A > C (Table 2). The most frequent variant was c.1199 + 502A > T (57.6%), followed by c.1065 + 241C > A (33.3%) and c.707-59C > G (6.1%). It indicated that full-length sequencing could effectively detect the variants both of exons and deep introns.
The novel variant c.706 + 629A > C was identified in a patient with cPKU. After family verification, it formed a compound heterozygous with c.526C > T (p.Arg176Ter). This variant is not present in population databases (gnomAD no frequency). In silico analysis by RESCUE-ESE and ESEfinder, it predicts this variant is probably damaging to the protein structure. But these predictions have not been confirmed by functional studies. Therefore, it has been classified as a uncertain significance (PM3, PP4_Moderate, PM2_Supporting).
Combined with the phenotypic analysis, 68.4% of the PKU patients with c.1199 + 502A > T were associated with cPKU, while those with c.1065 + 241C > A preferred mPKU. The variant c.707-59C > G was identified in two patients with mPKU. According to ClinGen PAH Expert Panel Specifications for interpretation of genetic variants, these deep intronic variants were classified as likely pathogenic or pathogenic.
Identification of the large-scale deletion/duplication of PAH
We selected five patients (in Table 3) and detected four kinds of deletion and duplication variants by MLPA, involving exons 4, 5, 6, 12, 1 and upstream (Additional file 1: Fig. S1). Full-length sequencing data showed the genomic regions of PAH gene deletions or duplicates in these samples. By comparison with the PAH reference sequence, we obtained the exons and introns contained in these regions. The results of analysis of the five samples were consistent with MLPA analysis. It shows that the single-gene full-length sequencing can analyze large-scale deletion/duplication within gene.
Distribution of PAH gene variant types
Through the supplementary detection of single-gene full-length sequencing, 683 of 687 PKU patients were completely genotyped. The variant types of the fully genotyped patients are summarized in Table 4. A total of 612 (89.6%) patients carried all variants in exons and flanking intron regions. We detected these variants by conventional sequence analysis, including Sanger sequencing and gene panels by NGS and whole-exome sequencing (WES). Thirty-three (4.8%) patients carried deep intronic variants that were identified by whole-genome sequencing (WGS) and single-gene full-length sequencing. In addition, 38 (5.6%) harbored the large-scale deletion/duplication that was detected by gene-targeted deletion/duplication analysis. Notably, among the molecular genetic testing used in PKU, only WGS and single-gene full-length sequencing detected all the above variants.
Characteristics of variants in deep introns and untranslated regions
After our manual screening, there were seven nonbenign variants of deep introns in the PAHvdb database. Three of them were also identified in our study. In addition, in our study, we found a novel variant c.706 + 629A > C that had not been reported previously. Therefore, we analyzed a total of eight variants listed in the Additional file 1: Table S2.
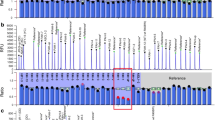
Among these variants, seven were detected in Asian populations, including Chinese and Iranian populations. In terms of the location of the variants, all variants were located in the catalytic domain (Fig. 2).
Discussion
PKU is a type of genetic disease with involvement of definite pathogenic genes and is treatable. Early, rapid and accurate genetic-based diagnosis is very important for subsequent patient treatment, genetic counseling and prenatal diagnosis. The previous diagnosis strategy suggested using sequencing analysis to detect variants in exons and flanking intron regions combined with MLPA to detect deletions and duplications [11].
In this study, we analyzed the genetic test results of 687 PKU patients and found that 5.4% of the patients could not be accurately diagnosed based on the previous strategy. Interestingly, full-length sequencing improved the diagnosis rate to more than 99% and can lead to rapid and efficient genetic-based diagnosis. To the best of our knowledge, this is the first time that single full-length sequencing of PAH has been used to identify PKU patients.
Full-length sequencing analysis suggested that deep intronic variants might be an important potential pathogenic mechanism of PKU. We found that nearly 90% of patients with previously undefined genotypes carried deep intron variants. Three deep intronic variants c.1199 + 502A > T, c.1065 + 241C > A and c.707-59C > G detected in our study were also reported in other variant spectrum studies of Chinese PKU patients [16, 17]. Our study provided additional patient data to support findings related to these three variants by sequencing a larger population. Notably, the c.1199 + 502A > T (2.8%, 19/687) and c.1065 + 241C > A (1.6%, 11/687) seemed to be found at a high frequency in our PKU patients. However, the pathogenicity of c.706 + 629A > C may need more experimental evidence or patient cases.
In the PAHvdb database, a total of 31 variants of deep introns are included. According to the previous criteria, we screened 8 nonbenign variants. Compared with other populations in the world, the frequency of deep intronic variants seems to be high in Asian, especially Chinese, PKU patients. We found that all of these deep intronic variants were distributed in the central domain, which includes Fe3+ ion binding sites involved in the binding of a cofactor [18]. The most commonly affected regions were introns 6 and 11. The distribution characteristics of deep intronic variants were consistent with the previous analysis of variants in the PAHvdb database and Chinese variant spectrum [11, 19].
Furthermore, we analyzed the genotypic-phenotypic correlation of these deep intronic variant carriers. Approximately 70% of patients with c.1199 + 502A > T had a severe cPKU phenotype. However, c.1065 + 241C > A and c.707-59C > G were associated with a lighter phenotype in PKU patients. Based on previous studies of genotype–phenotype correlation in PKU patients [16, 20], it is found that the variants of different positions will lead to different residual activities. Similarly, variations in different positions of the introns have different effects on protein expression. Martínez-Pizarro et al. [21] reported that c.1199 + 17G > A and c.1199 + 20G > C of PAH could cause a splicing defect by a novel mechanism involving U1snRNP binding downstream of the 5' splice site, resulting in exon 11 skipping and the formation of incomplete protein. Dericquebourg et al. [22] analyzed four hemophilia A patients with different clinical severity, who carried different deep intronic variants of F8. These variants lead to the creation of a de novo acceptor or donor splice site, and the formation of pseudoexon retention with different sequence lengths in the intron regions. For PKU patients, we speculate that the difference in phenotypic severity caused by deep intronic variants may be related to their location and impact on RNA splicing.
An increasing amount of studies have confirmed that deep intronic variants contribute to different diseases by affecting mRNA processing [23,24,25]. The splicing initiation of premRNA needs to be recognized by spliceosome and splice site (ss) sequences: the 5′ss (donor site), the 3′ss (acceptor site), and the branching point [26, 27]. Jin et al. [17] reported that the c.1199 + 502A > T variant of PAH acted to strengthen a cryptic branching point, and minigene expression showed that pseudoexon retention appeared in intron 11. The mechanism of pseudoexon inclusion caused by deep intronic variants may be due to activation of noncanonical splice sites, alterations to the splicing regulatory environment or loss of splice site competition [28, 29]. In addition, there are many other pathogenic mechanisms, such as disrupting transcription regulatory motifs or noncoding RNA [30]. Therefore, more experimental studies of the pathogenic mechanism of PAH deep intronic variants is required.
We analyzed data from 683 completely genotyped PKU patients, and deep intronic variants were carried in 4.8% of patients. Such variants cannot be detected by routine genetic analysis methods. WGS has been proven to be a powerful tool to identify causative variants residing outside coding regions in a variety of diseases [31, 32]. However, the cost of WGS sequencing is too high to be suitable for large-scale population screening. Similar to WGS, we designed a series of unique primers for PAH to amplify exons, deep introns and untranslated regions. And the time and cost of this single-gene full-length sequencing is similar to that of gene panel.
Moreover, our results indicated that the high-depth sequencing data obtained by full-length sequencing could also be used to analyze large-scale deletions/duplications within PAH. Therefore, this method of single-gene full-length sequencing not only has a lower detection cost than WGS but can also cover more regions of the targeted gene than routine genetic analysis methods. And using this method, we can find more deep intronic variants and micro-structure variants.
Even with single-gene full-length sequencing, four PKU patients (0.6%) did not have a clear genetic diagnosis. At present, phenylalanine metabolism may also be related to epigenetic factors [33]. Li et al. [34] reported that long noncoding RNAs (lncRNAs) were associated with PAH and modulated enzymatic activities by facilitating PAH-substrate and PAH-cofactor interactions. Therefore, epigenetic modification may be a new pathogenic mechanism of PKU.
Conclusion
Our study offers proof that single-gene full-length sequencing can achieve rapid, efficient and cost-effective genetic-based diagnosis in PKU patients. We believe this sequencing technique can be implemented in medical practice to help with the diagnosis, genetic counseling, carrier screening and prenatal diagnosis of PKU patients.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PKU:
-
Phenylketonuria
- Phe:
-
Phenylalanine
- PAH:
-
Phenylalanine hydroxylase
- mPKU:
-
Mild PKU
- cPKU:
-
Classic PKU
- ACMG:
-
American College of Medical Genetics and Genomics
- NGS:
-
Next-generation sequencing
- MLPA:
-
Multiplex ligation-dependent probe amplification
- WES:
-
Whole-exome sequencing
- WGS:
-
Whole-genome sequencing
References
van Spronsen FJ, Blau N, Harding C, Burlina A, Longo N, Bosch AM. Phenylketonuria. Nat Rev Dis Primers. 2021;7(1):36.
Blau N, van Spronsen FJ, Levy HL. Phenylketonuria. Lancet (London, England). 2010;376(9750):1417–27.
van Spronsen FJ, van Wegberg AM, Ahring K, Bélanger-Quintana A, Blau N, Bosch AM, Burlina A, Campistol J, Feillet F, Giżewska M, et al. Key European guidelines for the diagnosis and management of patients with phenylketonuria. Lancet Diabetes Endocrinol. 2017;5(9):743–56.
Yang Y, Ye Y. Consensus about the diagnosis and treatment of hyperphenylalaninemia. Zhonghua er ke za zhi = Chin J Pediatr. 2014;52(6):420–5.
Xiang L, Tao J, Deng K, Li X, Li Q, Yuan X, Liang J, Yu E, Wang M, Wang H, et al. Phenylketonuria incidence in China between 2013 and 2017 based on data from the Chinese newborn screening information system: a descriptive study. BMJ Open. 2019;9(8):e031474.
Vockley J, Andersson HC, Antshel KM, Braverman NE, Burton BK, Frazier DM, Mitchell J, Smith WE, Thompson BH, Berry SA. Phenylalanine hydroxylase deficiency: diagnosis and management guideline. Genet Med: Off J Am Coll Med Genet. 2014;16(2):188–200.
Gregg AR, Aarabi M, Klugman S, Leach NT, Bashford MT, Goldwaser T, Chen E, Sparks TN, Reddi HV, Rajkovic A, et al. Screening for autosomal recessive and X-linked conditions during pregnancy and preconception: a practice resource of the American College of Medical Genetics and Genomics (ACMG). Genet Med: Off J Am Coll Med Genet. 2021;23(10):1793–806.
Li N, Jia H, Liu Z, Tao J, Chen S, Li X, Deng Y, Jin X, Song J, Zhang L, et al. Molecular characterisation of phenylketonuria in a Chinese mainland population using next-generation sequencing. Sci Rep. 2015;5:15769.
Rajabi F, Rohr F, Wessel A, Martell L, Dobrowolski SF, Guldberg P, Güttler F, Levy HL. Phenylalanine hydroxylase genotype-phenotype associations in the United States: a single center study. Mol Genet Metab. 2019;128(4):415–21.
Vela-Amieva M, Alcántara-Ortigoza MA, Ibarra-González I, González-Del Angel A, Fernández-Hernández L, Guillén-López S, López-Mejía L, Carrillo-Nieto RI, Belmont-Martínez L, Fernández-Lainez C. An updated PAH mutational spectrum of phenylketonuria in Mexican patients attending a single center: biochemical, clinical-genotyping correlations. Genes. 2021;12(11):1676.
Liu N, Huang Q, Li Q, Zhao D, Li X, Cui L, Bai Y, Feng Y, Kong X. Spectrum of PAH gene variants among a population of Han Chinese patients with phenylketonuria from northern China. BMC Med Genet. 2017;18(1):108.
Yan YS, Yao FX, Hao SJ, Zhang C, Chen X, Feng X, Yang T, Huang SZ. Analysis of large deletion of phenylalanine hydroxylase gene in Chinese patients with phenylketonuria. Zhonghua yi xue za zhi. 2016;96(14):1097–102.
Wang K, Li M, Hakonarson H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucl Acids Res. 2010;38(16):e164.
Talevich E, Shain AH, Botton T, Bastian BC. CNVkit: genome-wide copy number detection and visualization from targeted DNA sequencing. PLoS Comput Biol. 2016;12(4):e1004873.
Zastrow DB, Baudet H, Shen W, Thomas A, Si Y, Weaver MA, Lager AM, Liu J, Mangels R, Dwight SS, et al. Unique aspects of sequence variant interpretation for inborn errors of metabolism (IEM): the ClinGen IEM working group and the phenylalanine hydroxylase gene. Hum Mutat. 2018;39(11):1569–80.
Zhang X, Ye J, Shen N, Tao Y, Han L, Qiu W, Zhang H, Liang L, Fan Y, Wang J, et al. In vitro residual activities in 20 variants of phenylalanine hydroxylase and genotype-phenotype correlation in phenylketonuria patients. Gene. 2019;707:239–45.
Jin X, Yan Y, Zhang C, Tai Y, An L, Yu X, Zhang L, Hao S, Cao X, Yin C, et al. Identification of novel deep intronic PAH gene variants in patients diagnosed with phenylketonuria. Hum Mutat. 2022;43(1):56–66.
Li N, He C, Li J, Tao J, Liu Z, Zhang C, Yuan Y, Jiang H, Zhu J, Deng Y, et al. Analysis of the genotype-phenotype correlation in patients with phenylketonuria in mainland China. Sci Rep. 2018;8(1):11251.
Hillert A, Anikster Y, Belanger-Quintana A, Burlina A, Burton BK, Carducci C, Chiesa AE, Christodoulou J, Đorđević M, Desviat LR, et al. The genetic landscape and epidemiology of phenylketonuria. Am J Hum Genet. 2020;107(2):234–50.
Waters PJ, Parniak MA, Nowacki P, Scriver CR. In vitro expression analysis of mutations in phenylalanine hydroxylase: linking genotype to phenotype and structure to function. Hum Mutat. 1998;11(1):4–17.
Martínez-Pizarro A, Dembic M, Pérez B, Andresen BS, Desviat LR. Intronic PAH gene mutations cause a splicing defect by a novel mechanism involving U1snRNP binding downstream of the 5′ splice site. PLoS Genet. 2018;14(4):e1007360.
Dericquebourg A, Jourdy Y, Fretigny M, Lienhart A, Claeyssens S, Ternisien C, Boisseau P, Rohrlich PS, Négrier C, Vinciguerra C. Identification of new F8 deep intronic variations in patients with haemophilia A. Haemoph: Off J World Fed Hemoph. 2020;26(5):847–54.
Minnerop M, Kurzwelly D, Wagner H, Soehn AS, Reichbauer J, Tao F, Rattay TW, Peitz M, Rehbach K, Giorgetti A, et al. Hypomorphic mutations in POLR3A are a frequent cause of sporadic and recessive spastic ataxia. Brain: J Neurol. 2017;140(6):1561–78.
Hujová P, Souček P, Grodecká L, Grombiříková H, Ravčuková B, Kuklínek P, Hakl R, Litzman J, Freiberger T. Deep Intronic mutation in SERPING1 caused hereditary angioedema through pseudoexon activation. J Clin Immunol. 2020;40(3):435–46.
Schulz HL, Grassmann F, Kellner U, Spital G, Rüther K, Jägle H, Hufendiek K, Rating P, Huchzermeyer C, Baier MJ, et al. Mutation spectrum of the ABCA4 gene in 335 stargardt disease patients from a multicenter german cohort-impact of selected deep intronic variants and common SNPs. Invest Ophthalmol Vis Sci. 2017;58(1):394–403.
Papasaikas P, Valcárcel J. The spliceosome: the ultimate RNA chaperone and sculptor. Trends Biochem Sci. 2016;41(1):33–45.
Caminsky N, Mucaki EJ, Rogan PK. Interpretation of mRNA splicing mutations in genetic disease: review of the literature and guidelines for information-theoretical analysis. F1000Research. 2014;3:282.
Petersen USS, Doktor TK, Andresen BS. Pseudoexon activation in disease by non-splice site deep intronic sequence variation: wild type pseudoexons constitute high-risk sites in the human genome. Hum Mutat. 2022;43(2):103–27.
Grodecká L, Kováčová T, Kramárek M, Seneca S, Stouffs K, De Laet C, Majer F, Kršjaková T, Hujová P, Hrnčířová K, et al. Detailed molecular characterization of a novel IDS exonic mutation associated with multiple pseudoexon activation. J Mol Med (Berl). 2017;95(3):299–309.
Vaz-Drago R, Custódio N, Carmo-Fonseca M. Deep intronic mutations and human disease. Hum Genet. 2017;136(9):1093–111.
Fadaie Z, Whelan L, Ben-Yosef T, Dockery A, Corradi Z, Gilissen C, Haer-Wigman L, Corominas J, Astuti GDN, de Rooij L, et al. Whole genome sequencing and in vitro splice assays reveal genetic causes for inherited retinal diseases. NPJ Genom Med. 2021;6(1):97.
Larrue R, Chamley P, Bardyn T, Lionet A, Gnemmi V, Cauffiez C, Glowacki F, Pottier N, Broly F. Diagnostic utility of whole-genome sequencing for nephronophthisis. NPJ Genom Med. 2020;5:38.
Cederbaum S. Phenylketonuria: an update. Curr Opin Pediatr. 2002;14(6):702–6.
Li Y, Tan Z, Zhang Y, Zhang Z, Hu Q, Liang K, Jun Y, Ye Y, Li YC, Li C, et al. A noncoding RNA modulator potentiates phenylalanine metabolism in mice. Science (New York, NY). 2021;373(6555):662–73.
Acknowledgements
Not available.
Funding
This research was funded by Joint Open Research Fund of Henan Key Laboratory of Child Brain Injury and Henan Pediatric Clinical Research Center (KFKT2021002) and Medical Science and Technique Foundation of Henan Province (LHGJ20200453, LHGJ20190357).
Author information
Authors and Affiliations
Contributions
All authors have materially participated in the study and manuscript preparation. JG and XL collected all clinical data, performed the clinical and genetic analyses and drafted the manuscript; YG was responsible for revising the manuscript. HY, YG and LS analyzed the genetic data and performed laboratory experiments; FY, EY and QS conducted the in silico prediction of the impact of variants and participated in conceiving the work; DZ collected and reviewed the data. EY participated in the design of some experiments. LZ designed the whole study and drafted and revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of The Third Affiliated Hospital of Zhengzhou University (Approval No. 2022-065-01).
Consent for publication
The authors declares that there are no financial or other relationships that might lead to a conflict of interest of the present article. The manuscript is approved by all authors for publication.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Table S1: Other variants information of patients with unclear genotypes; Figure S1: MLPA results of patient 38-42; Table S2: Summary of nonbenign PAH variants in deep introns.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gao, J., Li, X., Guo, Y. et al. Identification of phenylketonuria patient genotypes using single-gene full-length sequencing. Hum Genomics 16, 23 (2022). https://doi.org/10.1186/s40246-022-00397-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40246-022-00397-w