Abstract
Background
Intestinal inflammation is the main risk factor causing intestinal barrier dysfunction and lipopolysaccharide (LPS) can trigger inflammatory responses in various eukaryotic species. Yeast hydrolysate (YH) possesses multi-biological effects and is received remarkable attention as a functional ingredient for improving growth performance and promoting health in animals. However, there is still inconclusive on the protective effects of dietary YH supplementation on intestinal barrier of piglets. This study was conducted to investigate the attenuate effects of YH supplementation on inflammatory responses and intestinal barrier injury in piglets challenged with LPS.
Methods
Twenty-four piglets (with an average body weight of 7.42 ± 0.34 kg) weaned at 21 days of age were randomly assigned to one of two dietary treatments (12 replications with one pig per pen): a basal diet or a basal diet containing YH (5 g/kg). On the 22nd d, 6 piglets in each treatment were intraperitoneally injected with LPS at 150 μg/kg BW, and the others were injected with the same amount of sterile normal saline. Four hours later, blood samples of each piglet were collected and then piglets were euthanized.
Results
Dietary YH supplementation increased average daily feed intake and average daily gain (P < 0.01), decreased the ratio of feed intake to gain of piglets (P = 0.048). Lipopolysaccharide (LPS) injection induced systemic inflammatory response, evidenced by the increase of serum concentrations of haptoglobin (HP), adrenocorticotropic hormone (ACTH), cortisol, and interleukin-1β (IL-1β). Furthermore, LPS challenge resulted in inflammatory intestinal damage, by up-regulation of the protein or mRNA abundances of tumor necrosis factor-α (TNF-α), IL-1β, toll-like receptors 4 (TLR4) and phosphor-nuclear factor-κB-p65 (p-NFκB-p65) (P < 0.01), and down-regulation of the jejunal villus height, the protein and mRNA abundances of zonula occludens-1 (ZO-1) and occludin (OCC; P < 0.05) in jejunal mucosa. Dietary YH supplementation decreased the impaired effects of ACTH, cortisol, HP, IL-1β and diamine oxidase in serum (P < 0.05). Moreover, YH supplementation also up-regulated the jejunal villus height, protein and mRNA abundances of ZO-1 and OCC (P < 0.05), down-regulated the mRNA expressions of TNF-α and IL-1β and the protein abundances of TNF-α, IL-1β, TLR4 and p-NFκB-p65 in jejunal mucosa in LPS-challenged pigs (P < 0.01).
Conclusion
Yeast hydrolysate could attenuate inflammatory response and intestinal barrier injury in weaned piglets challenged with LPS, which was associated with the inhibition of TLR4/NF-κB signaling pathway activation.
Graphical Abstract

Similar content being viewed by others
Introduction
Intestinal epithelial barrier, a structure of continuous monolayer enterocytes, is dominated by intercellular tight junction [1]. Under a normal state, it acts as a selective filter that enables the absorption of nutrients and ensures an effective defense against exogenous pathogens, luminal antigens, etc. [2]. For early weaned mammals, however, the gastrointestinal tract is immature and vulnerable to multitudinous stresses [3], and intestinal epithelial barrier is frequently defective in various pathological status, especially in bacterial infections induced by pathogenic bacteria [4, 5]. The damaged intestinal epithelial barrier mainly causes the increase of intestinal permeability, promotes the transfer of antigens in lumen to the subepithelial tissues, and further exacerbates the mucosal and systemic inflammatory reactions [1, 6, 7]. The secretion of pro-inflammatory cytokines during the inflammatory response is a major factor in triggering the disruption of the intestinal barrier [8]. In piglets, intestinal barrier dysfunction and accompanied by the enhancement of intestinal permeability are often observed, with subsequent diarrhea and growth retardation [9, 10]. Therefore, effective and safe preventive approaches to maintenance of intestinal barrier function are urgently needed for piglets. Notably, lipopolysaccharide (LPS), an intrinsic component of the cell wall of gram-negative bacteria, has been shown to be a key molecule in inducing the production of pro-inflammatory cytokines [7]. It often contributes to inflammatory intestinal damage in piglets. The molecular mechanism is manifested by the activation of inflammatory signaling pathway by LPS, which induces the expression of key proteins of pro-inflammatory factors and thus leads to intestinal barrier damage [11]. Previous studies have shown that LPS can be used to construct a well-established model of inflammation in pigs [12, 13].
Yeast (Saccharomyces cerevisiae) is widely distributed in nature and has been inseparable from human life [14]. Yeast hydrolysate (YH), also known as yeast autolysate, is obtained from Saccharomyces cerevisiae via protein hydrolysis enzyme [15, 16]. Several researches suggested that the autolytic yeast fractions or peptides from autolyzed yeasts revealed physiological effects on anti-obesity [17, 18], anti-fatigue [19], anti-stress [20, 21] and immuno-promotional activities [22, 23]. For these reasons, YH has attracted much attention as a functional material supplement and it is generally recognized as non-toxic, effective and safe [24]. Recently, several studies were focused on improving intestinal health and immune-potentiating activities with YH. Specifically, YH has multiple roles on promoting digestion and absorption of nutrients [25], improving intestinal microflora structure [26] and decreasing diarrhea of young animals [19], while also acts as an immunomodifier to prevent gut inflammation [27]. However, the protective effects of dietary supplementation with YH on intestinal barrier are limited and inconclusive. It is widely known that hyperinflammation in intestine is one of the most factors causing intestinal barrier dysfunction [1, 2, 10]. Consequently, considering the above, we postulated that YH has the potential to prevent LPS-induced intestinal barrier dysfunction in piglets by alleviating inflammation via the related signaling pathways. This study tested these hypotheses by assessing the effects of YH on the systemic inflammatory response, intestinal morphology, expression of tight junction-related proteins and gut anti-inflammatory capacity in piglets.
Materials and methods
Chemical analysis of yeast hydrolysate
Yeast hydrolysate was provided by Jiangmen Thealth Bioengineering Co., Ltd. (Guangzhou, China). The contents of moisture, crude protein, crude fat and crude ash were measured with the reference of AOAC [28]. Gross energy was determined by an oxygen bomb calorimeter (Parr instruments, Moline, IL, USA). The soluble protein in yeast hydrolysate was extracted according to the method of Wang et al. [29] and fractionated by sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) system according to the previous study [30]. The gel was stained with Coomassie Brilliant Blue (Beyotime, Shanghai, China) for 40 min and de-stained with deionized water for 8 h.
Experimental animals, diet, and design
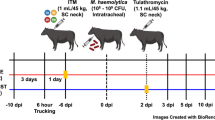
The animal procedures were reviewed and approved by the Animal Care and Use Committee at Sichuan Agricultural University with the approval number of SYXK (Sichuan)-2019–187. A total of twenty-four weaned piglets (21-day-old), with an average initial body weight (BW) of 7.42 ± 0.34 kg, were randomly allotted to two groups (12 replicates per treatment and one piglets per replicate) receiving either a basal diet or a basal diet with YH (5 g/kg) for 21 d. All piglets were fed individually in metabolic cages (1.5 m × 0.7 m × 1.0 m) and housed in an environmentally controlled room. Piglets were fed three times daily at 8:00, 14:00 and 20:00 and have free accessed to water and feed throughout the experiment. After 21-d feeding trial, immunological challenge was applied to the half of piglets in each treatment (Fig. 1A). That means 6 piglets in each treatment were intraperitoneally injected with LPS at 150 μg/kg BW, and the other 6 piglets were injected with an equal volume of sterile physiological saline. The basal diet (Table 1) was a corn-soybean meal-fish meal diet and was formulated to meet or exceed National Research Council (NRC 2012) [31] requirements for piglets from 7–11 kg and 11–25 kg stage. The YH diet was formulated by replacing soybean meal with 5 g/kg YH in equal amounts in the basal diet. The molecular weight of YH was less than 50 kDa and mostly clustered below 25 kDa (Fig. S1). YH mainly provided a rich source of crude protein (45.50%), and contributed less to crude ash (6.47%) and crude fat (2.17%) (Table S1).
Dietary yeast hydrolysate supplementation improved the growth performance of weaned piglets before LPS challenge. A Schematic of the feeding experiment and LPS challenge. B–D Effects of dietary YH supplementation on average daily feed intake (ADFI), average daily gain (ADG) and the ratio of feed intake to gain (F/G) of weaned piglets. Control, piglets were fed with a basal diet; YH, piglets were fed with a YH containing diet, 5 g/kg. *P < 0.05, **P < 0.01, compared with control group
LPS injection
The challenged piglets were intraperitoneally injected with Escherichia coli LPS (E. coli serotype O55:B5, Sigma Chemical Inc., St. Louis, MO, USA) at 150 μg/kg BW, and unchallenged piglets were administrated the same volume of sterile physiological saline. The dose and serotype of LPS used in this study was consistent with the previous reports [12, 13]. Previous experiments have presented that LPS injection particularly caused dramatic inflammatory response and intestinal barrier dysfunction in pigs, rats and mice. And these negative effects generally occurred within 3–6 h after LPS injection [7, 32]. Therefore, blood and intestinal samples in this study were collected 4 h following LPS or saline injection.
Growth performance
Yeast hydrolysate treatment was a main factor prior to the LPS challenge. Piglets were weighted individually on 1st d and 22nd d of the experiment. Daily feed consumption was recorded for each piglet. Average daily gain and the ratio of feed intake to gain were calculated as well.
Blood sample collection and analysis
Four hours following LPS and saline injection, blood samples were collected in 10 mL vacutainer tubes via anterior vena cava. Blood was centrifugated at 3500 × g for 10 min at 4 ℃. Serum samples were stored at −20 ℃ until subsequent analysis for inflammatory markers and diamine oxidase (DAO) concentrations. Commercially available porcine ELISA kits (Chenglin Biological Technology Co., Ltd., Beijing, China) were performed according to the manufacturer’s instructions for the following indicators: adrenocorticotropic hormone (ACTH), cortisol, C-reactive protein (CRP), serum amyloid A (SAA), haptoglobin (HP), tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β) and DAO in serum.
Intestinal samples collection and analysis
Piglets were euthanized with pentobarbital sodium (200 mg/kg) in a separate sampling room away from other animals. The intestine was immediately removed. A 2-cm segment was removed from mid-jejunum and fixed with 4% paraformaldehyde solution. Paraffin embedding was used to cut into cross sects (5 μm thick). The jejunal morphology was determined by hematoxylin and eosin (H&E) stain. Intestinal morphological images were photographed with a Nikon TS100 microscope (40 × and 100 ×). Villus height and crypt depth were analyzed and calculated by Image Pro Plus 6.0 software (Media Cybernetics, Bethesda, MD, USA). Other sections were stained using immunofluorescence for TLR4 protein. Briefly, mouse anti-TLR4 monoclonal antibody (1:100, sc-293072, Santa Cruz, Dallas, TX, USA) was incubated overnight at 4 ℃. Corresponding secondary antibody (Cy3 conjugated Goat Anti-mouse IgG, 1:300, GB21301 from Servicebio, Wuhan, China) was incubated for 50 min at room temperature. The slides were washed three times with PBS, and then incubated with DAPI solution at room temperature for 10 min and stored in the dark. After immunofluorescence, microphotographs were acquired with an inverted microscope (Leica DMI400B, Wetzlar, Germany). In addition, the inner wall of the middle jejunum was washed with ice-cold saline and the mucosal samples were then scraped into a sterile tube. Mucosal samples were immediately placed into liquid nitrogen and stored at −80℃ until the analysis of genes and proteins expressions. About 0.5 g of frozen jejunal mucosal scrapings were homogenized in ice-cold saline and prepared into a 10% homogenate, crushed using an ultrasonic cell crushing system at 4 °C and then centrifuged (3000 × g, 15 min, 4 °C). The collected supernatant was used to analyze TNF-α and IL-1β contents by ELISA kits according to the manufacturer’s instructions.
mRNA abundance analysis
Total RNA was extracted from jejunal mucosa using the TRIZOL reagent (TaKaRa Biotechnology (Dalian) Co., Ltd., Dalian, China). RNA integrity was verified by agarose gel electrophoresis. cDNA was synthesized with PrimeScript RT kit (TaKaRa). Real-time PCR was performed using SYBR Premix Ex Taq reagents (TaKaRa) and CFX-96 RT-qPCR Detection System (Bio-Rad, Hercules, CA, USA). The genes of intestinal barrier and inflammatory markers related primer pairs were synthesized by Sangon Biotech (Shanghai) Co., Ltd. (Shanghai, China) and listed in Table 2. The mRNA expression of target gene relative to housekeeping gene (β-actin) was calculated by the method of Arce et al. [33].
Western blot analysis
Western blot analysis was performed as previously described [34]. Briefly, protein was extracted from jejunal mucosa using the lysis buffer (Beyotime, Shanghai, China). Protein concentration was measured with the BCA protein assay kit (Pierce, Rockford, IL, USA). Then, protein was transferred to polyvinylidene fluoride membranes using a wet Trans-Blot system (Bio-Rad). After blocking, membranes were incubated with primary antibodies: anti-TLR4 (sc-293072, Santa Cruz), anti-ZO-1 (61–7300, Invitrogen, MA, USA), anti-OCC (ab31721, abcam, Shanghai, China), anti-TNF-α (ab6671, abcam), anti-IL-1β (sc-12742, Santa Cruz), anti-NFκB-p65 (6956, CST, Cell signaling Technology, Beverly, USA), anti-p-NFκB-p65 (3033, CST), and anti-β-actin (sc-47778, Santa Cruz). After washing, the corresponding secondary antibodies, goat anti-rabbit/mouse IgG -HRP secondary antibody (sc-2030 and sc-2031, Santa Cruz), were incubated at room temperature for 1 h. Visualization of membranes was performed with the Clarity™ Western ECL substrate (Bio-Rad) and the ChemiDoc XRS imaging system (Bio-Rad). The β-actin was applied as a controller for the mean of protein load.
Statistical analysis
Statistical analysis was performed using SAS software package (Version 9.4; S.A.S, Institute Inc., Cary, NC, USA) [35]. All data were expressed as mean values with their standard error and checked for normal distribution using the Shapiro–Wilk test of SAS. Each piglet served as the statistical unit. Specifically, data on growth performance prior to LPS challenge were analyzed by two-tailed Student’s t-test. After LPS injection, data from serum and jejunum samples were statistically analyzed by two-way ANOVA using the PROC MIXED procedure of SAS with the following model:
where yij is an observed trait, μ is the overall mean, αi is the fixed effect of immunological challenge (i = saline or LPS), βj is the fixed effect of dietary YH (j = 0 or 5 g/kg YH), αi × βj is the interaction between LPS and YH and eijk is the random error. Differences between the different groups were analyzed by Duncan’s multiple comparison method. P < 0.05 was considered statistically significant, and 0.05 < P < 0.10 indicated a trend.
Results
Effects of YH on growth performance in piglets prior to LPS injection
As shown in Fig. 1, a 21-d feeding experiment was conducted to examine the effects of YH on growth performance of piglets under normal condition (Fig. 1A). Compared with control group, dietary YH supplementation increased ADFI (P < 0.01) and ADG (P < 0.01) (Fig. 1B and C), decreased F/G of piglets (P = 0.048) (Fig. 1D).
Effects of YH on systemic inflammatory response and serum DAO concentration in piglets challenged with LPS
Results of serum acute phase protein, stress hormone and inflammatory cytokines concentrations in piglets challenged with LPS were showed in Fig. 2 and Fig. 3. As expected, LPS injection enhanced HP (Fig. 2B), cortisol (Fig. 2D), ACTH (Fig. 2E) and IL-1β (Fig. 3B) concentrations in serum (P < 0.01). However, LPS + YH group significantly decreased the concentrations of HP, cortisol, ACTH and IL-1β in serum compared with the LPS group (P < 0.05).
Dietary yeast hydrolysate supplementation inhibited the over-production of acute phase protein and stress hormone in piglets challenged with LPS. A–C Effects of dietary YH supplementation on the serum concentrations of serum amyloid A (SAA), haptoglobin (HP) and C-reactive protein (CRP) in piglets challenged with LPS. D and E Effects of dietary YH supplementation on the serum levels of stress hormones (D) cortisol and (E) adrenocorticotropic hormone. Control, piglets were fed with a basal diet; YH, piglets were fed with a YH containing diet, 5 g/kg. a,b,cMeans with different superscript letters in a row were significantly different (P < 0.05)
Dietary yeast hydrolysate supplementation attenuated the enhancement of serum concentrations of (A) tumor necrosis factor-α (TNF-α) and (B) interleukin-1β (IL-1β) in piglets challenged with LPS. Control, piglets were fed with a basal diet; YH, piglets were fed with a YH containing diet, 5 g/kg. a,bMeans with different superscript letters in a row were significantly different (P < 0.05)
As shown in Fig. 4, compared with saline group, there was greater concentration of serum DAO in LPS group (P < 0.01), however, YH supplementation significantly inhibited the increase of the serum DAO concentration in LPS challenged piglets (P = 0.02).
Dietary yeast hydrolysate supplementation attenuated the effects of LPS-injection on jejunal permeability and morphology. A Representative picture of the appearance of the intestinal tract of a piglet. B Hematoxylin and eosin section of jejunum at 40 times magnification (up) and 100 times magnification (down). C The concentrations of diamine oxidase (DAO) in serum of piglets. D–F The villus height, crypt depth and the villus height:crypt depth ratio of jejunum of piglets. Control, piglets were fed with a basal diet; YH, piglets were fed with a YH containing diet, 5 g/kg. a,b,cMeans with different superscript letters in a row were significantly different (P < 0.05)
Effects of YH on intestinal morphology in LPS- challenged piglets
The effects of YH on intestinal morphology in LPS-challenged piglets were shown in Fig. 4. LPS challenge caused dramatic intestinal hyperemia (Fig. 4A), induced intestinal mucosal injury reflected by villous atrophy and mucosal detachment (Fig. 4B), and decreased the villus height (Fig. 4D) (P = 0.02). Compared with LPS group, LPS + YH group attenuated the state of intestinal hyperemia, improved the morphology and significantly increased the villus height (P = 0.03).
Effects of YH on the expression of intestinal barrier related genes in LPS-challenged piglets
Compared with saline treatment, LPS injection reduced the relative mRNA expressions of CLDN-1 (Fig. 5A), OCC (Fig. 5C) and MUC2 (Fig. 5D) (P < 0.05), as well as the protein expressions of OCC (Fig. 5E and 5F; P = 0.01) and ZO-1 (Fig. 5E and G; P < 0.01) in jejunal mucosa. In compared to LPS group, YH supplementation significantly inhibited the down-regulation of mRNA expression of OCC (P = 0.02) and MUC2 (P < 0.01) and protein abundances of OCC (P < 0.01) and ZO-1 (P = 0.04) in jejunal mucosa of LPS-challenged piglets.
Dietary yeast hydrolysate supplementation improved the barrier function of jejunal mucosa in piglets challenged with LPS. A–D The relative mRNA expression of Claudin-1 (CLDN-1), Zonula occludens-1 (ZO-1), Occludin (OCC) and mucin2 (MUC2) in the jejunal mucosa of piglets. E–G The protein abundance of OCC ZO-1 in the jejunal mucosa of piglets. Control, piglets were fed with a basal diet; YH, piglets were fed with a YH containing diet, 5 g/kg. a,b,cmeans with different superscript letters in a row were significantly different (P < 0.05)
Effects of YH on the expression of TNF-α and IL-1β of jejunum in piglets challenged with LPS
As shown in Fig. 6, LPS injection enhanced the concentrations of TNF-α (Fig. 6A; P = 0.01) in jejunal mucosa, however, YH significantly reversed this change (P < 0.01). A further analysis by RT-qPCR and western blot revealed that LPS challenge significantly increased the mRNA expressions of TNF-α (Fig. 6C) and IL-1β (Fig. 6D) and the corresponding protein abundances (Fig. 6E–G; P < 0.01). Conversely, a down-regulation was observed in the mRNA expressions of IL-1β and the protein abundance of TNF-α and IL-1β in LPS + YH group (P < 0.01).
Dietary yeast hydrolysate supplementation inhibited the inflammatory response of jejunal mucosa in piglets challenged with LPS. A and B The concentrations of tumor necrosis factor-α (TNF-α) and interleukin-1β (IL-1β) in the jejunal mucosa of piglets by ELISA method. C and D The mRNA expression of TNF-α and IL-1β in the jejunal mucosa of piglets. E–G The protein abundance of TNF-α and IL-1β in the jejunal mucosa of piglets. Control, piglets were fed with a basal diet; YH, piglets were fed with a YH containing diet, 5 g/kg. a,b,cMeans with different superscript letters in a row were significantly different (P < 0.05)
Effects of YH on the TLR4/NF-κB signaling pathway in LPS-challenged piglets
As shown in Fig. 7, we investigated the expression of TLR4, the major inflammation-associated receptor, by immunofluorescence analysis and discovered that the distribution of TLR4 in jejunum of piglets enhanced by LPS challenge (Fig. 7A). Nevertheless, the variability was reversed with YH supplementation when compared to LPS group. Moreover, we observed an up-regulation in the expressions of TLR4 protein (Fig. 7B and C) and p-NFκB-p65 protein (Fig. 7B and D) in LPS group compared with saline group (P < 0.01). LPS + YH group decreased the protein abundances of TLR4 (P < 0.01) and p-NFκB-p65 (P = 0.01) compared with LPS group.
Dietary yeast hydrolysate supplementation decreased the protein abundance of TLR4 and p-NFκB-p65 in jejunal mucosa in piglets challenged with LPS. A Immunofluorescence staining (100 times magnification) of toll-like receptors 4 (TLR4) in jejunum of piglets. B–D Relative protein abundance of B and C TLR4 and B and D phosphor-Nuclear factor-κB-p65 (p-NFκB-p65). Control, piglets were fed with a basal diet; YH, piglets were fed with a YH containing diet, 5 g/kg. a,b,cMeans with different superscript letters in a row were significantly different (P < 0.05)
Discussion
Yeast hydrolysate (YH), an autolysate of Saccharomyces cerevisiae, has attracted much attention as a nutritional additive, which involved in various biological activities including growth promotion and immune regulation. Throughout the 21-d feeding experiment (pre-LPS-challenge) in this study, we observed that dietary YH supplementation increased growth performance of piglets. This effect may be related to the molecular weight of YH. As shown in an animal model, the low molecular weight YH (below 30 kDa) exhibits a low toxicity for rats [24]. This hydrolysate is more accessible to animals due to its low molecular weight contributing to a higher solubility in aqueous media and a better digestibility and absorptivity [36]. Previous studies have found that YH (below 10 kDa) revealed physiological effects on anti-obesity [37, 38] and anti-stress [20, 21]. In this study, the molecular weight of YH was less than 50 kDa and mostly clustered below 25 kDa. Furthermore, the beneficial effects of YH on growth performance have been characterized in rats [39], piglets [40], growing-finishing pigs [25], chickens [41] and fish [27, 42]. Similar results have been found in our previous study that feeding YH significantly improved growth performance for piglets under the normal physiological condition and the reason might also be that YH could improve intestinal barrier function [22]. Nevertheless, it remains to be studied whether YH can improve intestinal health under pathological states. In the present study, we focused on whether dietary YH attenuated the intestinal barrier impairment through inhibiting the massive release of pro-inflammatory cytokines. Hence, we utilized an incontrovertible model for acute gut injure by injecting lipopolysaccharide (LPS). LPS is an intrinsic constituent of membranes in gram-negative bacteria and it is a powerful endotoxin [7]. It binds to TLR4 and subsequently activates downstream signaling pathways, triggering an inflammatory response [11].
Acute phase proteins (APPs) such as C-reactive protein (CRP), haptoglobin (HP) and serum amyloid A (SAA) were secreted by hepatocytes and served as a crucial role in the etiopathogenesis of immune diseases [43]. In addition, some stress hormones (e.g., ACTH and cortisol) were frequently used in response to infectious status in the body [44]. With the infection and injury of the host (such as LPS injection), the expressions or serum concentrations of APPs and stress hormones will be dramatically enhanced [45, 46]. Indeed, our results found that serum concentrations of HP, SAA, ACTH and cortisol in piglets were increased 4 h after LPS-injection. However, supplementation of YH to the LPS-infected piglets reduced the levels of HP, ACTH and cortisol, suggesting that YH attenuated LPS-induced stress response. To our knowledge, TNF-α and IL-1β were the critical inducers of APPs [47]. And it is a highly significant correlation between serum APPs and TNF-α levels in some infectious agents [48]. In the present investigation, LPS challenge resulted in an increase of TNF-α and IL-1β in serum. Undoubtedly, LPS caused an excessive activation of immune system. Nevertheless, YH supplementation decreased the concentrations of TNF-α and IL-1β in LPS-challenged piglets, which indicated dietary YH supplementation could decrease the systemic inflammation after LPS infection. Over-production of proinflammatory cytokines manufactured intestinal damage, such as villous atrophy, mucosal swelling, submucosal hemorrhage and exfoliation, and led to an increase of intestinal permeability [7]. Several blood indictors have been used to evaluate the intestinal permeability. DAO, an enzyme found at high levels in the mammalian intestinal mucosa, is a marker of maturation and integrity in response to intestinal epithelium [49]. The levels of serum DAO are positively correlated with intestinal permeability. In this study, YH supplementation reduced DAO concentrations, indicating that YH had beneficial effects on attenuating the increase of intestinal permeability of piglets challenged with LPS. Meanwhile, intestinal permeability can usually be assessed with intestinal epithelial barrier function [6]. Therefore, it is possible that YH supplementation can mitigate systemic inflammatory associated with the improvement of intestinal barrier function.
Intestinal morphology is regarded as a visual reflection for the growth and development of gut and determined by villus height and crypt depth [50]. This study showed that LPS-injection induced intestinal damage including villous atrophy, mucosal detachment, and a decrease of villus height in jejunum of piglets. While dietary inclusion of YH could counteract the morphological changes of jejunum after LPS challenge, thereby maintaining the villus integrity and structure of intestinal mucosa. Considering the importance of intestinal epithelial barrier in intestinal function, the tight junctions between epithelial cells were analyzed in this study. Tight junctions are multi-protein complexes including claudins, occludin and ZOs, which defend against the passage of luminal antigens, pathogenic bacterium and their toxins [6]. Recently, the experimental results showed that YH inclusion markedly attenuated the down-regulation mRNA expressions of OCC, and the protein abundances of OCC and ZO-1 in jejunal mucosa of LPS-challenged piglets. Thus, dietary YH administration could maintain the integrity of intestinal barrier by inhibiting the decrease of tight junction protein expression under immunological stress, which might be the potential reasons that YH mitigated the impairments of intestinal permeability and morphology in LPS-injected piglets.
It is generally accepted that cytokines are the critical modulators of intestinal inflammation [47]. Over-production of pro-inflammatory cytokines (e.g., TNF-α and IL-1β) has been demonstrated to directly impair the tight junctional function of some epithelial and endocrine cells [51]. Previous studies have indicated that alleviating intestinal inflammation might effectively prevent pathogenic bacteria and their toxins from disrupting intestinal barrier function [2]. Consequently, the reduction of intestinal pro-inflammatory cytokine concentrations under stressful conditions is one of the major strategies to protect the intestinal barrier and mitigate intestinal inflammation. In the present study, YH supplementation significantly reduced the mRNA expressions of TNF-α and IL-1β, and the corresponding protein abundances in jejunal mucosa in LPS challenged-piglets. Similarly, Waititu et al. [52] reported that piglets receiving a YH riched in cell wall polysaccharides reduced TNF-α level in ileum challenged by LPS. Hence, the protected effect of YH on intestinal barrier appears to be achieved by suppressing the inflammatory response. This is also a possible reason that YH ameliorates the systemic inflammatory response.
With a further view to investigating the molecular mechanisms of YH in the alleviation of intestinal inflammation, we evaluated the activation of TLR4 signaling pathway. TLR4, a typical pattern recognition receptor in the TLR protein family, is widely distributed on the surface of various intestinal cells and plays an essential role in LPS-mediated signaling [11]. Mechanistically, TLR4 activation triggered by LPS can induce the increased expression of downstream molecules (such as NF-κB), and then enhance the expression of proinflammatory cytokines-related genes, resulting in intestinal barrier damage [7, 53]. Currently, we observed that YH supplementation significantly decreased the protein abundance and immunofluorescence intensity of TLR4 in jejunal mucosa of piglet challenged with LPS, as well as downregulated the protein levels of p-NF-κB. NF-κB, the master transcription factor for TLR4 signaling, is phosphorylated and translocated to the nucleus in the stimulated state, then promoting the release of pro-inflammatory cytokines [54]. Accordingly, YH supplementation inhibits the TLR4/NF-κB signaling pathway, which may represent a potential mechanism to decelerate the signaling of LPS, thereby enabling the inflammatory response to be dampened.
Conclusion
Dietary YH supplementation improves the growth performance and attenuates LPS-induced intestinal inflammation and barrier injury. The underlying molecular mechanism is YH supplementation inhibits the activation of TLR4/NF-κB signaling pathway induced by LPS, to prevent the over-production of inflammatory cytokines, and thus improved the intestinal barrier function.
Abbreviations
- ACTH:
-
Adrenocorticotropic hormone
- ADFI:
-
Average daily feed intake
- ADG:
-
Average daily gain
- CLDN-1:
-
Claudin-1
- CRP:
-
C-reactive protein
- DAO:
-
Diamine oxidase
- F/G:
-
The ratio of feed intake to gain
- HP:
-
Haptoglobin
- IL-1β:
-
Interleukin-1β
- LPS:
-
Lipopolysaccharide
- MUC2:
-
Mucin2
- NF-κB:
-
Nuclear factor-κB
- OCC:
-
Occludin
- SAA:
-
Serum amyloid A
- TLR4:
-
Toll-like receptors 4
- TNF-α:
-
Tumor necrosis factor-α
- YH:
-
Yeast hydrolysate
- ZO-1:
-
Zonula occludens-1
References
Rana AS, Michel B, Thomas M. Mechanism of cytokine modulation of epithelial tight junction barrier. Front Biosci. 2009;14:2765. https://doi.org/10.2741/3413.
Croschwitz KP, Hogan SP. Intestinal barrier function: Molecular regulation and disease pathogenesis. J Allergy Clin Immun. 2009;124(1):3–20. https://doi.org/10.1016/j.jaci.2009.05.038.
Weström B, Arévalo-Sureda E, Pierzynowska K, Pierzynowski SG, Pérez-Cano FJ. The immature gut barrier and its importance in establishing immunity in newborn mammals. Front Immun. 2020;11:1153. https://doi.org/10.3389/fimmu.2020.01153.
Ng QX, Soh AYS, Loke W, Lim DY, Yeo WS. The role of inflammation in irritable bowel syndrome (IBS). J Inflamm Res. 2018;11:345. https://doi.org/10.2147/JIR.S174982.
Barani M, Rahdar A, Sargazi S, Amiri MS, Sharma PK, Bhalla N. Nanotechnology for inflammatory bowel disease management: Detection, imaging and treatment. Sensing Bio-Sensing Res. 2021;32:100417. https://doi.org/10.1016/j.sbsr.2021.100417.
Anderson R, Dalziel J, Gopal P, Bassett S, Ellis A, Roy N. Colitis: The role of intestinal barrier function in early life in the development of colitis. In: Fukata M, editor. New Zealand: Institute; 2012;Chapter 1:1-30.
Williams JM, Duckworth CA, Watson AJ, Frey MR, Miguel JC, Burkitt MD, et al. A mouse model of pathological small intestinal epithelial cell apoptosis and shedding induced by systemic administration of lipopolysaccharide. Dis Model Mech. 2013;6(6):1388–99. https://doi.org/10.1242/dmm.013284.
Hiippala K, Jouhten H, Ronkainen A, Hartikainen A, Kainulainen V, Jalanka J, et al. The potential of gut commensals in reinforcing intestinal barrier function and alleviating inflammation. Nutrients. 2018;10(8):988. https://doi.org/10.3390/nu10080988.
Moeser AJ, Pohl CS, Rajput M. Weaning stress and gastrointestinal barrier development: Implications for lifelong gut health in pigs. Anim Nutr. 2017;3(4):313–21. https://doi.org/10.1016/j.aninu.2017.06.003.
Mao J, Qi S, Cui Y, Dou X, Luo XM, Liu J, et al. Lactobacillus rhamnosus GG attenuates lipopolysaccharide-induced inflammation and barrier dysfunction by regulating MAPK/NF-κB signaling and modulating metabolome in the piglet intestine. J Nutr. 2020;150(5):1313–23. https://doi.org/10.1093/jn/nxaa009.
Ciesielska A, Matyjek M, Kwiatkowaska K. TLR4 and CD14 trafficking and its influence on LPS-induced pro-inflammatory signaling. Cell Mol Life Sci. 2021;78(4):1233–61.
Liu YL, Wang XY, Leng WB, Pi DG, Tu ZX, Zhu HL, et al. Aspartate inhibits LPS-induced MAFbx and MuRF1 expression in skeletal muscle in weaned pigs by regulating Akt, AMPKα and FOXO1. Innate Immun. 2017;23(1):34–43. https://doi.org/10.1177/1753425916673443.
Touchette KJ, Carroll JA, Allee GL, Matteri RL, Zannelli ME. Effect of spray-dried plasma and lipopolysaccharide exposure on weaned pigs: I. Effects on the immune axis of weaned pigs. J Anim Sci. 2002;80(2):494–501. https://doi.org/10.2527/2002.802494x.
Parapouli M, Vasileiadis A, Afendra AS, Hatziloukas E. Saccharomyces cerevisiae and its industrial applications. AIMS Microbiol. 2020;6(1):1. https://doi.org/10.3934/microbiol.2020001.
Jung EY, Hong YH, Kim JH, Park Y, Bae SH, Chang UJ, et al. Effects of yeast hydrolysate on hepatic lipid metabolism in high-fat-diet-induced obese mice: Yeast hydrolysate suppresses body fat accumulation by attenuating fatty acid synthesis. Ann Nutr Metab. 2012;61(2):89–94. https://doi.org/10.1159/00033844.
Mosser M, Chevalot I, Olmos E, Blanchard F, Kapel R, Oriol E, et al. Combination of yeast hydrolysates to improve CHO cell growth and IgG production. Cytotechnology. 2013;65(4):629–41. https://doi.org/10.1007/s10616-012-9519-1.
Jung EY, Lee JW, Hong YH, Chang UJ, Suh HJ. Low dose yeast hydrolysate in treatment of obesity and weight loss. Prev Nutr Food Sci. 2017;22(1):45. https://doi.org/10.3746/pnf.2017.22.1.45.
Park Y, Kim JH, Lee HS, Jung EY, Lee H, Noh DO, et al. Thermal stability of yeast hydrolysate as a novel anti-obesity material. Food Chem. 2013;136(2):316–21. https://doi.org/10.1016/j.foodchem.2012.08.047.
Hu J, Park JW, Kim IH. Effect of dietary supplementation with brewer’s yeast hydrolysate on growth performance, faecal microbial counts, diarrhoea score, blood profile, rectal temperature in weanling pigs challenged with lipopolysaccharide. J Anim Physiol Anim Nutr. 2020;104(2):629–36. https://doi.org/10.1111/jpn.13301.
Kim JM, Lee SW, Kim KM, Chang UJ, Song JC, Suh HJ. Anti-stress effect and functionality of yeast hydrolysate SCP-20. Eur Food Res Technol. 2003;217(2):168–72. https://doi.org/10.1007/s00217-003-0723-2.
Lee HS, Jung EY, Suh HJ. Chemical composition and anti-stress effects of yeast hydrolysate. J Med Food. 2009;12(6):1281–5. https://doi.org/10.1089/jmf.2009.0098.
Fu RQ, Liang C, Chen DW, Yan H, Tian G, Zheng P, et al. Effects of dietary Bacillus coagulans and yeast hydrolysate supplementation on growth performance, immune response and intestinal barrier function in weaned piglets. J Anim Physiol Anim Nutr. 2021;105(5):898–907. https://doi.org/10.1111/jpn.13529.
Gong Y, Yang F, Hu J, Liu C, Liu H, Han D, et al. Effects of dietary yeast hydrolysate on the growth, antioxidant response, immune response and disease resistance of largemouth bass (Micropterus salmoides). Fish Shellfish Immun. 2019;94:548–57. https://doi.org/10.1016/j.fsi.2019.09.044.
Jung EY, Lee HS, Chang UJ, Bae SH, Kwon KH, Suh HJ. Acute and subacute toxicity of yeast hydrolysate from Saccharomyces cerevisiae. Food Chem Toxicol. 2010;48(6):1677–81. https://doi.org/10.1016/j.fct.2010.03.044.
Zhang JY, Park JW, Kim IH. Effect of supplementation with brewer’s yeast hydrolysate on growth performance, nutrients digestibility, blood profiles and meat quality in growing to finishing pigs. Asian-Austral J Anim Sci. 2019;32(10):1565. https://doi.org/10.5713/ajas.18.0837.
Fu RQ, Chen DW, Tian G, Zheng P, Mao XB, Yu J, et al. Effect of dietary supplementation of Bacillus coagulans or yeast hydrolysates on growth performance, antioxidant activity, cytokines and intestinal microflora of growing-finishing pigs. Anim Nutr. 2019;5(4):366–72. https://doi.org/10.1016/j.aninu.2019.06.003.
Andriamialinirina HJT, Irm M, Taj S, Lou JH, Jin M, Zhou Q. The effects of dietary yeast hydrolysate on growth, hematology, antioxidant enzyme activities and non-specific immunity of juvenile Nile tilapia, Oreochromis niloticus. Fish Shellfish Immun. 2020;101:168–75. https://doi.org/10.1016/j.fsi.2020.03.037.
Latimer Junior G. Official methods of analysis of AOAC International. Gaithersburg: AOAC International; 2016.
Wang Y, Liu J, Wei F, Liu X, Yi C, Zhang Y. Improvement of the nutritional value, sensory properties and bioavailability of rapeseed meal fermented with mixed microorganisms. LWT. 2019;112:108238. https://doi.org/10.1016/j.lwt.2019.06.005.
Shi C, He J, Yu J, Yu B, Mao X, Zheng P, et al. Physicochemical properties analysis and secretome of Aspergillus niger in fermented rapeseed meal. PLoS One. 2016;11(4):e0153230. https://doi.org/10.1371/journal.pone.0153230.
NRC (National Academy of Sciences-National Research Council). Nutrient requirements of swine. 11th ed. Washington, DC: National Academies Press; 2012.
Liu Y, Huang J, Hou Y, Zhu H, Zhao S, Ding B, et al. Dietary arginine supplementation alleviates intestinal mucosal disruption induced by Escherichia coli lipopolysaccharide in weaned pigs. Brit J Nutr. 2008;100(3):552–60. https://doi.org/10.1017/S0007114508911612.
Arce R, Barros S, Wacker B, Peters B, Moss K, Offenbacher S. Increased TLR4 expression in murine placentas after oral infection with periodontal pathogens. Placenta. 2009;30(2):156–62. https://doi.org/10.1016/j.placenta.2008.11.017.
Pu JN, Chen DW, Tian G, He J, Huang ZQ, Zheng P, et al. All-trans retinoic acid attenuates transmissible gastroenteritis virus-induced inflammation in IPEC-J2 cells via suppressing the RLRs/NF-κB signaling pathway. Front Immun. 2022;31:13. https://doi.org/10.3389/fimmu.2022.734171.
SAS. Statistical Analysis System Version 9.4. NC, USA: SAS Institute Inc; 2013.
Kim KW, Thomas R. Antioxidative activity of chitosans with varying molecular weights. Food Chem. 2007;101(1):308–13. https://doi.org/10.1016/j.foodchem.2006.01.038.
Jung EY, Kim SY, Bae SH, Chang UJ, Choi JW, Suh HJ. Weight reduction effects of yeast hydrolysate below 10 kDa on obese young women. J Food Biochem. 2011;35(2):337–50. https://doi.org/10.1111/j.1745-4514.2010.00385.x.
Jung EY, Cho MK, Hong YH, Kim JH, Park Y, Chang UJ, et al. Yeast hydrolysate can reduce body weight and abdominal fat accumulation in obese adults. Nutrition. 2014;30(1):25–32. https://doi.org/10.1016/j.nut.2013.02.009.
Kim JM, Kim SK, Jung EY, Bae SH, Suh HJ. Yeast hydrolysate induces longitudinal bone growth and growth hormone release in rats. Phytother Res. 2009;23(5):731–6. https://doi.org/10.1002/ptr.2720.
Molist F, van Eerden E, Parmentier H, Vuorenmaa J. Effects of inclusion of hydrolyzed yeast on the immune response and performance of piglets after weaning. Anim Feed Sci Tech. 2004;195:136–41. https://doi.org/10.1016/j.anifeedsci.2014.04.020.
Wang T, Cheng K, Yu C, Tong Y, Yang Z, Wang T. Effects of yeast hydrolysate on growth performance, serum parameters, carcass traits, meat quality and antioxidant status of broiler chickens. J Sci Food Agric. 2021;102(2):575–83. https://doi.org/10.1002/jsfa.11386.
Jin M, Xiong J, Zhou QC, Yuan Y, Wang XX, Sun P. Dietary yeast hydrolysate and brewer’s yeast supplementation could enhance growth performance, innate immunity capacity and ammonia nitrogen stress resistance ability of Pacific white shrimp (Litopenaeus vannamei). Fish Shellfish Immun. 2018;82:121–9. https://doi.org/10.1016/j.fsi.2018.08.020.
Perez L. Acute phase protein response to viral infection and vaccination. Arch Biochem Biophys. 2019;671:196–202. https://doi.org/10.1016/j.abb.2019.07.013.
Chami R, Monteleone AM, Treasure J, Monteleone P. Stress hormones and eating disorders. Mol Cell Endocrinol. 2019;497:110349. https://doi.org/10.1016/j.mce.2018.12.009.
Sánchez-Lemus E, Benicky J, Pavel J, Saavedra JM. In vivo Angiotensin II AT1 receptor blockade selectively inhibits LPS-induced innate immune response and ACTH release in rat pituitary gland. Brain Behav Immun. 2009;23(7):945–57. https://doi.org/10.1016/j.bbi.2009.04.012.
Hou X, Wang T, Ahmad H, Xu Z. Ameliorative effect of ampelopsin on LPS-induced acute phase response in piglets. J Funct Foods. 2017;35:489–98. https://doi.org/10.1016/j.jff.2017.05.044.
Luan YY, Yao YM. The clinical significance and potential role of C-reactive protein in chronic inflammatory and neurodegenerative diseases. Front Immun. 2018;9:1302. https://doi.org/10.3389/fimmu.2018.01302.
Moya SL, Boyle L, Lynch PB, Arkins S. Pro-inflammatory cytokine and acute phase protein responses to low-dose lipopolysaccharide (LPS) challenge in pigs. Anim Sci. 2006;82(4):527–34. https://doi.org/10.1079/ASC200665.
Luk GD, Bayless TM, Baylin SB. Diamine oxidase (histaminase). A circulating marker for rat intestinal mucosal maturation and integrity. J Clin Invest. 1980;66(1):66–70. https://doi.org/10.1172/JCI109836.
Chelakkot C, Ghim J, Ryu SH. Mechanisms regulating intestinal barrier integrity and its pathological implications. Exp Mol Med. 2018;50(8):1–9. https://doi.org/10.1038/s12276-018-0126-x.
Capaldo CT, Nusrat A. Cytokine regulation of tight junctions. Biochim Biophys Acta. 2009;1788:864–71. https://doi.org/10.1016/j.bbamem.2008.08.027.
Waititu SM, Yin F, Patterson R, Rodriguez-Lecompte JC, Nyachoti CM. Short-term effect of supplemental yeast extract without or with feed enzymes on growth performance, immune status and gut structure of weaned pigs challenged with Escherichia coli lipopolysaccharide. J Anim Sci Biotechn. 2016;7:64. https://doi.org/10.1186/s40104-016-0125-5.
Guo S, Al-Sadi R, Said HM, Ma TY. Lipopolysaccharide causes an increase in intestinal tight junction permeability in vitro and in vivo by inducing enterocyte membrane expression and localization of TLR-4 and CD14. Am J Pathol. 2013;182(2):375–87. https://doi.org/10.1016/j.ajpath.2012.10.014.
Tang J, Xu L, Zeng Y, Gong F. Effect of gut microbiota on LPS-induced acute lung injury by regulating the TLR4/NF-kB signaling pathway. Int Immunopharmacol. 2021;91:107272. https://doi.org/10.1016/j.intimp.2020.107272.
Acknowledgements
We gratefully acknowledge our debt to the generous donation from Jiangmen Thealth Bioengineering Co., Ltd., and the help of Huifen Wang and Zhemin Gu in animal experiment and sample collection.
Funding
This work was supported by the National Key Research and Development Program of China (2018YFD0500605), the Key Research and Development Program of Sichuan Province (2021YFYZ0008), and the Sichuan Pig Innovation Team of National Modern Agricultural Industry Technology System of China (scsztd-2020–08-11).
Author information
Authors and Affiliations
Contributions
BY conceived and designed the experiment. RF and CL participated in the animal experiment, data analysis and drafting of the manuscript. DC, GT, PZ and JH were responsible for animal care and sampling. JY and XM contributed technical support. YL and JL performed biochemical analysis. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures described in this study were approved by the Institutional Animal Care and Use Committee of Sichuan Agricultural University (No.20190129).
Consent for publication
Not applicable.
Competing interests
Authors declare there are no competing interests.
Supplementary Information
Additional file 1: Fig. S1.
SDS-PAGE analysis of yeast hydrolysate.
Additional file 2: Table S1.
Chemical component of yeast hydrolysate.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fu, R., Liang, C., Chen, D. et al. Yeast hydrolysate attenuates lipopolysaccharide-induced inflammatory responses and intestinal barrier damage in weaned piglets. J Animal Sci Biotechnol 14, 44 (2023). https://doi.org/10.1186/s40104-023-00835-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40104-023-00835-2